Abstract
Objective
Cognitive training offers a promising way to mitigate cognitive deterioration in individuals with mild cognitive impairment (MCI). This randomized control pilot trial examined the effects of Gist Reasoning Training on cognition as compared with a training involving New Learning in a well‐characterized MCI group.
Methods
Fifty participants with amnestic MCI were randomly assigned to the experimental Gist Training group or an active control New Learning group. Both groups received 8 h of training over a 4‐week period. We compared pre‐training with post‐training changes in cognitive functions between the two training groups.
Results
The Gist Training group showed higher performance in executive function (strategic control and concept abstraction) and memory span compared with the New Learning group. Conversely, the New Learning group showed gains in memory for details.
Conclusion
These findings suggest that cognitive training in general yields benefits, and more specifically, training programs that target top–down cognitive functions such as gist reasoning may have a broad impact on improving cognition in MCI. © 2016 The Authors. International Journal of Geriatric Psychiatry Published by John Wiley & Sons Ltd.
Keywords: MCI, cognitive training, gist reasoning, executive function, memory, RCT
The burden of cognitive impairment caused by Alzheimer's disease (AD) has escalated over the years because of increased longevity. Recent advances in our knowledge make it possible to detect AD in the early stages when individuals experience subtle cognitive deterioration with no significant functional impairment referred to as mild cognitive impairment (MCI) (Weiner et al., 2013; Cohen and Klunk, 2014). Steps taken to improve early detection of MCI will be most beneficial when interventions can mitigate cognitive deterioration (Petersen et al., 2014) because annual conversion rate to dementia varies from 5–7% and is especially higher in those with the amnestic subtype (e.g., Manly et al., 2008; Roberts et al., 2013). Available pharmacological treatments for AD have offered limited benefits in improving cognition or slowing progression from MCI to dementia (Thal et al., 2005; Feldman and Lane, 2007). With 200 failed AD drug candidates (Becker and Greig, 2013), the need to explore additional approaches that slow cognitive decline is urgent.
Cognitive training is one avenue to harness the residual brain capacity in MCI. Several studies have examined cognitive training effects in MCI, mostly in the amnestic subtype, but the findings have been contentious. While a Cochrane review of randomized control trials (RCT) found no benefits of cognitive training in MCI relative to controls (Martin et al., 2011), several other reviews (Jean et al., 2010; Stott and Spector, 2011; Cotelli et al., 2012; Simon et al., 2012; Huckans et al., 2013; Reijnders et al., 2013) and a meta‐analysis (Li et al., 2011) have found positive outcomes. A number of factors, such as poorly defined study‐populations, limited RCT, and lack of active control groups make it challenging to establish training benefits (Hampstead et al., 2014). Another potential limitation is that cognitive training studies have largely targeted memory functions, known to be most vulnerable and perhaps less modifiable in MCI. The training formats (individual vs. group; computer‐based vs. low technology vs. mixed), the dose, and the outcome measurements have varied widely (e.g., Greenaway et al., 2008; Hampstead et al., 2008; Belleville et al., 2011) with inconsistent generalization beyond the trained domain and limited improvements in functional outcomes (Gates et al., 2011; Hampstead et al., 2012; Simon et al., 2012).
Cognitive training that targets non‐memory domains in MCI would allow us to harness the neuroplastic potential of brain regions and networks that are relatively unaffected in the early stages of AD. Supporting this view, one of the largest RCT to date, the advanced cognitive training for independent and vital elderly (ACTIVE) trial, reported that individuals with low memory showed gains with abstract reasoning training, which targeted the ability to solve problems involving serial patterns of letter or number sequences, in contrast to memory training (Unverzagt et al., 2007). This reported benefit was revealed in a subgroup analysis of individuals whose memory scores were 1.5 standard deviations below the population mean. Although these individuals were not clinically diagnosed with MCI, the findings suggest a potential benefit of targeting reasoning skills in a lowered‐memory population. Additionally, empirical findings involving various forms of reasoning training in cognitively normal adults have shown generalized cognitive gains (Willis et al., 2006; Anand et al., 2011; Chapman et al., 2015) and lasting benefits in self‐reported independent activities of daily living (Rebok et al., 2014). Research from our group offers further motivation to examine reasoning training that focuses on gist abstraction abilities in MCI (Chapman and Mudar, 2014).
Gist abstraction is defined as the ability to synthesize and derive diverse interpretations from complex information (e.g., written documents and verbal information). Gist represents the preferential propensity to glean global meaning rather than details from complex information as described in van Dijk and Kintsch's (1983) discourse framework and gist representation in Reyna and Brainerd's (1995) fuzzy trace theory. Evidence suggests that advanced reasoning engages gist processing (Reyna and Brainerd, 1995, 2011; Reyna and Lloyd, 2006), and such gist reasoning skills are integral to successful academic, occupational, and functional performance (Reyna and Brainerd, 1995, 2011; Reyna and Lloyd, 2006; Chapman et al., 2012). A series of gist reasoning training (henceforth referenced to as Gist Training) trials (Chapman and Mudar, 2014), which targeted gist abstraction abilities in normally aging seniors (Anand et al., 2011; Chapman et al., 2015) and adults with traumatic brain injury (Vas and Chapman, 2012; Vas et al., 2015) have shown cognitive and neural benefits.
Studies on Gist Training involving normal older adults, in particular, have demonstrated not only gains in abstraction but also generalized benefits in untrained measures of cognitive control including cognitive switching, fluency, and concept abstraction (Anand et al., 2011; Chapman et al., 2015). Furthermore, normal older adults who underwent Gist Training showed increases in global and regional cerebral blood flow in the default mode network and the central executive network compared with waitlisted controls. Increased functional connectivity in the same brain networks was noted in addition to increased structural connectivity in the left uncinate fasciculus (Chapman et al., 2015). These brain gains were significantly linked to cognitive improvement. This convergent pattern suggests the brain's residual neuroplastic potential could be tapped by training top–down cognitive functions such as gist reasoning, to achieve cognitive and neural benefits.
The purpose of this randomized control pilot study was to examine the effects of Gist Training on cognition in individuals with MCI as compared with an active control training consisting of New Learning. We hypothesized significant gains in the Gist Training group compared with the New Learning group in executive functions whereas we predicted the New Learning group would show gains in memory. We expected both groups to self‐report gains on real life memory performance due to engagement/stimulation offered by the training programs.
Method
Fifty community‐dwelling seniors (see Table 1 for Demographics) participated in this study after providing informed consent according to the guidelines of The University of Texas at Dallas Human Protection Program and in accordance with the Helsinki Declaration of 1975, as revised in 1983. All participants were native English speakers, had a minimum of high school education, and 46 were right‐handed. Individuals of both genders were included with no exclusions made based on racial or ethnic factors. All participants completed the mini‐mental state examination (MMSE, Folstein et al., 1975), the Wide Range Achievement Test 4 (WRAT4, Wilkinson and Robertson, 2006), and either the Geriatric Depression Scale (GDS, Yesavage et al., 1982) or Beck Depression Inventory (BDI, Beck et al., 1996). Only participants with scores of 25–30 on the MMSE, ability to read at a 12th grade reading level, a score of 4 or below on the GDS or a score below 13 on BDI were included. All participants showed adequate visual and auditory acuity by being able to read 12 point font‐type and following conversation in a quiet environment, respectively.
Table 1.
Demographics and performance on screening measures
| Gist Reasoning | New Learning | |
|---|---|---|
| (n = 23; females = 11) | (n = 27; females = 16) | |
| Years of Education | 16.22 | 17.26 |
| (2.26) | (1.48) | |
| Age at test | 75.65 | 69.78 |
| (8.51) | (8.01) | |
| MMSE | 27.74 | 28.11 |
| (1.36) | (1.60) | |
| GDS | 1.27 | 1.91 |
| (1.19) | (1.35) | |
| BDI | 7.67 | 5.75 |
| (3.17) | (2.06) |
GDS Gist group n = 11, New Learning group n = 23; BDI Gist group n = 12, New Learning group n = 4. BDI, Beck Depression Inventory; GDS, Geriatric Depression Scale; MMSE, mini‐mental state examination.
Participants met Petersen criteria for MCI (Petersen et al., 2001) and were of the amnestic subtype. They had (i) subjective memory concerns; (ii) objective memory loss (e.g., a Wechsler Memory Scale‐III (WMS III, Wechsler, 1997b) logical memory subtest delayed recall score of 5–9 (8–15 year of education) and 9–12 (≥16 years of education) for early MCI (EMCI); ≤4 (8–15 year of education) and ≤8 (≥16 years of education) for late MCI (LMCI)) (Aisen et al., 2010); (iii) a Clinical Dementia Rating (CDR, Morris, 1993) of 0.5; (iv) preserved activities of daily living determined by instrumental activities of daily living scores; and (v) an absence of dementia. Diagnosis of MCI was made by a research team of neurologists, neuropsychologist, cognitive neuroscientists, and speech‐language pathologists. Four (two in each group) of the 50 patients were taking cholinesterase inhibitors when tested and were on stabilized doses of donepezil for at least 3 months. Participants with history of other neurologic disease, medical illnesses, major psychiatric disturbance, substance abuse, or taking psychoactive medications were excluded.
In the pre‐training phase, participants' baseline performance was established using cognitive measures of executive function and memory as well as a validated, self‐rating memory measure; after which, they were randomized into one of the two training groups (Gist Training n = 23 [14 EMCI, 9 LMCI]; New Learning Training n = 27 [17 EMCI, 10 LMCI]). The same measures were used in the post‐training phase to examine outcomes. The pre‐training and post‐training assessments were done by three experienced clinicians per manualized protocol. Scoring was done by two clinicians independently, one of whom was unaware of the group assignment and time of testing (pre or post), and no significant differences were observed between scores of the two raters (p < 0.05).
Measures
Executive function measures included similarities subtest from the Weschler Adult Intelligence Scale III (Wechsler, 1997a), strategic attention score from a list learning task (Hanten et al., 2007), and complex abstraction from an experimental text processing task (Anand et al., 2011). Memory measures included the logical memory subtest from WMS III, memory span from the list learning task, and memory for details from the text processing task. Participants rated their memory on the metamemory questionnaire (MMQ, Troyer and Rich, 2002). See Table 2 for details of experimental measures.
Table 2.
Description of experimental outcome measures
| Neurocognitive measure | Description | Administration and scoring |
|---|---|---|
| List learning | Three different lists of 16 words adapted from Hanten et al. (2007) were used. For each list, the words were divided into two similar sets of 8 words (one set spoken by a female voice and the other by a male voice, randomized within the list). The words within a list were designated by voice (male or female) as either high‐value (10 points) or low‐value (1 point). | Words were presented one at a time auditorily. Recall elicited at the end of each list. |
| Scoring | ||
| Strategic Attention: Number of high value words recalled on each trial. | ||
| Memory Span: Total number of words recalled on each trial | ||
| Text processing | Narrative of 550 words about a man's life and the eight jobshe attempted throughout his life in an effort to make life better for others. | Participant asked to read the narrative, generate lessons, and recall details. |
| Scoring | ||
| Adopted from previous studies by Ulatowska et al. (1998) and Chapman et al. (2002). | ||
| Abstraction: Scored on a pre‐established scale of 0–6. Scores fall on a continuum, representing qualitative differences in the nature of response, with lower scores indicating problems in abstracting meaning and higher scores indicating greater ability to abstract meaning across the text content. | ||
| Detail memory: Number of details recalled out of a possible 24 details. |
Gist Training and New Learning Training programs were delivered in small groups of 3–5 individuals over 4 weeks with two 1‐h sessions per week. The cognitive training was led by a clinician who had previously completed a 3‐stage process prior to study implementation consisting of reading about the programs, observing a trained clinician deliver a 4‐week program, and leading training sessions under supervision to ensure treatment fidelity. The training dose was determined based on a previous study involving normal controls (Anand et al., 2011). Training equity was based on similar group size, same number of sessions, similar opportunity for interaction and social contact, and comparable home assignments (reading an article or watching a short video estimated to take about 20 min a day). While compliance was not formally tracked, the majority of participants were observed to complete their assignments during the homework discussion period at the beginning of each session.
Cognitive training programs
Gist reasoning training
Gist Training is a strategy—rather than content‐based program. The primary objectives are to promote utilization of three core strategies: strategic attention, integrated reasoning, and innovation summarized in Table 3 (Chapman et al., 2012; Chapman and Mudar, 2014). The strategy instruction is hierarchical and dynamically interdependent, with each strategy building on previous strategies. A wide variety of information sources such as articles, short stories, and audio clips were used to provide intense practice with these strategies. Participants were encouraged to utilize the three strategies as often as possible within the context of their own life activities and goals throughout their day (e.g., listening to a lecture, reading a newspaper/book, watching television, or engaging in conversation).
Table 3.
Training protocols
| Training | Description |
|---|---|
| Gist Reasoning Training | Hierarchical strategies |
| Strategic attention: Consciously blocking distractions/less relevant information (e.g., reducing multitasking; turning off TV/email notifications) and focusing on important information (e.g., highlighting text). | |
| Integrated reasoning: Binding explicit facts with world knowledge to construct generalized meanings. | |
| Innovation: Deriving multiple interpretations and generalized applications beyond the concrete content reflecting fluency and fluidity of thinking. | |
| New Learning Training | New Learning about brain functions and influences on cognition. Example topics covered: Brain structures and functions; Neuroplasticity and neurogenesis; Memory and the brain; Social bonds and the brain |
New learning training
This training uses an educational approach to teach and discuss interesting facts about how the brain works and what factors influence its health. This program was originally developed at the Rotman Institute, Canada (Binder et al., 2008) and has been used by others in cognitive training studies (Chen et al., 2011; Levine et al., 2011; Novakovic‐Agopian et al., 2011). For this study, an adapted curriculum to approximate the general structure of Gist Training matching the number of sessions, duration, discussions, and homework assignments, was used. Topics outlined in Table 3, among others were covered. Information across a multitude of sources was presented to facilitate socially engaged discussion and New Learning. Individuals were encouraged to share with others what they were learning in the program as often as possible.
Statistical analysis
Each cognitive measure was entered in a general statistical linear model that included a training effect (pre‐assessment and post‐assessment) and a group effect from the two cognitive training therapies (Gist Training and New Learning), and the interaction between them. The interaction term (group × time) was of primary interest; therefore, we restricted inference to mean change over the assessment periods between the two training groups. Covariates, such as age and education, were included in the model as simple additive terms, but any effect of age and education was differenced out of the interaction contrasts. Also included in the model were three variance components from random effects due to variability within subjects, across subjects, and between stages of MCI (EMCI and LMCI). For each outcome measure the interaction contrast of means were obtained, which were transformed to student's t‐statistics. The corresponding p‐values are reported in Table 4.
Table 4.
Pre‐training to post‐training changes in cognitive functions in the two training programs
| Neurocognitive measures | Gist Reasoning | New Learning | Interaction p‐value | ||
|---|---|---|---|---|---|
| Pre | Post | Pre | Post | ||
| Executive function | |||||
| WAIS‐III Similarities (SS) | 13.32 (0.56) | 14.27 (0.56) | 13.89 (0.50) | 13.96 (0.51) | 0.066 |
| List learning strategic attention—trial 3 | 2.95 (0.39) | 4.34 (0.40) | 4.30 (0.37) | 4.39 (0.38) | 0.011 |
| Text processing complex abstraction | 2.96 (0.36) | 3.37 (0.38) | 3.04 (0.33) | 3.45 (0.35) | 0.498 |
| Memory | |||||
| WMS‐III Logical | 10.45 (1.31) | 12.67 (1.32) | 10.11 (1.30) | 11.00 (1.30) | 0.075 |
| List learning memory span | 3.31 (0.42) | 4.62 (0.43) | 4.98 (0.40) | 5.18 (0.41) | 0.016 |
| Text processing detail memory | 4.61 (0.26) | 5.04 (0.26) | 4.89 (0.24) | 6.00 (0.24) | 0.045 |
| Self‐evaluation memory | |||||
| MMQ Feelings | 33.14 (4.58) | 38.27 (4.58) | 31.28 (4.08) | 34.13 (3.94) | 0.278 |
| MMQ Mistakes | 41.83 (3.93) | 44.20 (3.93) | 42.32 (3.54) | 41.32 (3.39) | 0.188 |
| MMQ Strategies | 32.13 (4.22) | 36.38 (4.22) | 40.98 (3.88) | 40.22 (3.66) | 0.168 |
WAIS‐III, Weschler adult intelligence scale III; MMQ, metamemory questionnaire.
Results
Overall, we observed three significant two‐way interactions between training effect and training types. Gist Training showed increased post‐assessment means from baseline relative to New Learning training on executive function and memory measures, specifically strategic attention (high value points) (p = 0.011) and memory span (total number of words) (p = 0.016) on trial 3 of the list learning task. In each case, the New Learning group showed no mean change from baseline (Figure 1). Conversely, Gist Training showed a smaller increase in post‐assessment means from baseline relative to the New Learning training for detail memory (p = 0.045). Additionally, we observed two important trends wherein Gist Training showed improvements in concept abstraction on the similarities subtest (p = 0.066) and memory on the logical memory subtest (p = 0.075) relative to the New Learning group (Figure 2). We also observed a larger mean reduction in subjective memory mistakes with Gist Training, although not significant (p = 0.188).
Figure 1.
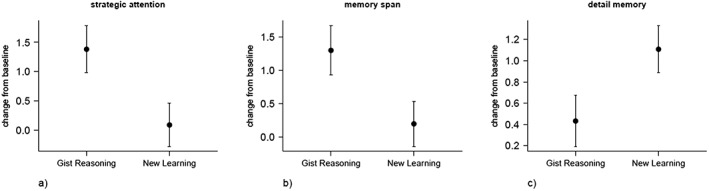
Gist Training showed increased post‐assessment means from baseline relative to New Learning Training for (a) third trial of strategic attention, and (b) memory span. New Learning training showed increased post‐assessment means from baseline relative to Gist Training for (c) detail memory.
Figure 2.
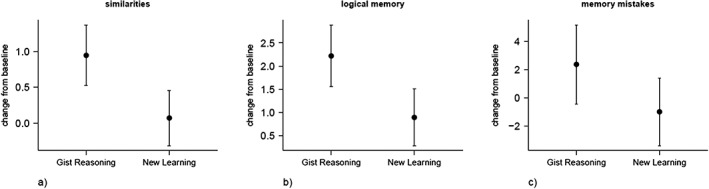
Gist Training showed (i) trends towards increased post‐assessment means from baseline relative to New Learning training for (a) similarities scaled score (b) logical memory raw score, and (ii) a reduction in number of subjective memory mistakes.
Discussion
This study is one of the first pilot RCT to investigate the impact of Gist Training in individuals with amnestic MCI as compared with an active control training program that targeted New Learning. Individuals who received Gist Training strategically recalled more high value items compared with low value items on the trial of interest (trial 3) during list learning compared with the New Learning group. Strategic processing is achieved when individuals are able to attend to the most important/relevant information while ignoring the less relevant details (Dayan et al., 2000). Such strategic processing is related to cognitive efficiency (Castel et al., 2007) and may serve to improve diminishing memory capacities in individuals with MCI. Gains in strategic attention with Gist Training are relevant to mitigating cognitive losses in MCI because previous research has shown that AD impairs cognitive control in early disease stages (Castel et al., 2009). Our finding suggests that a residual capacity to select important information and inhibit less important information and exert better top–down control may be improved in MCI through Gist Training.
The Gist Training group also showed a trend towards gains in concept abstraction on similarities subtest similar to our previous findings involving normal aging individuals (Anand et al., 2011; Chapman et al., 2015). The similarities subtest captures an individual's ability to process and abstract relationships (e.g., how are a car and train alike). Our findings suggest that training focused on abstracting meaning from complex information showed transfer benefits to untrained concept abstraction. However, unlike other cognitive training trials involving Gist Training in normal aging (Anand et al., 2011; Chapman et al., 2015), we did not find gains in complex gist abstraction during text processing. It is possible that the MCI group may have needed a higher training dose than 8 h to experience gains in complex abstraction.
With regard to memory benefits, both groups showed significant gains on different immediate memory measures. The Gist Training group improved significantly pre‐test to post‐test on memory span for items during list learning. Thus, not only did they strategically remember more high value items, but by using this strategy, they were able to improve their memory span (i.e., number of items recalled), a gain that was not observed in the New Learning group. Furthermore, the Gist Training group also showed a trend towards improvement on logical memory scores, a more complex memory measure, although not significant probably because of small subject numbers and variability contributed by EMCI and LMCI stages. Moro et al. (2015) reported similar improvements in memory in individuals with MCI following executive function training and attributed those gains to enhanced memory efficiency. One key gain observed in the New Learning group was a significant pre to post increase in memory for facts. The ability to remember more factual information is an important gain and was directly related to the nature of New Learning Training that mainly targeted memory for facts and is consistent with the findings of other training studies that have targeted memory functions in MCI (Li et al., 2011; Martin et al., 2011; Simon et al., 2012; Reijnders et al., 2013).
Few studies have reported quantitative data related to perceived gains/benefits following cognitive training. In the present study, participants in the Gist Reasoning group more often reported reduced frequency of memory mistakes on MMQ in everyday memory situations, such as remembering appointments, names, and telephone numbers. MMQ was incorporated into the study design after we completed a few waves of training; thus, we had data on only a subset of participants. Nonetheless, a similar number of MMQ measures were collected for both groups. Implication of improved daily memory may suggest a potential generalization to real life benefits; however, a no‐contact control group is needed to determine the true influence of the subjective changes on memory. Future studies are warranted to examine whether an increased training dose would achieve larger gains and whether perceived memory gains are associated with objective memory gains.
This pilot study should be interpreted within the context of its limitations. First, our sample size was relatively small to derive conclusive patterns. However, the positive cognitive gains support verification in a larger study. With the promising evidence of benefits from relatively brief Gist Training dose, future trials would be improved if different training dose effects were tested. The addition of neural markers measuring the brain's response to cognitive training would also be informative in light of prior evidence of brain and cognitive gains following Gist Training in other populations. Also, the small sample size did not allow us to examine individual factors that contribute to response to training such as stage of MCI. Because the classification of EMCI and LMCI is not universally accepted, our goal for staging was to account for variability caused by such differences during analysis. Future studies with larger samples should explore treatment response between these stages. Also, longitudinal studies are necessary to determine maintained effects and to determine whether cognitive interventions early in the disease are able to slow the rate of decline or conversion to dementia. Only a handful of studies have shown that training effects are maintained from 2 weeks to 6 months (Rapp et al., 2002; Kinsella et al., 2009; Greenaway et al., 2012); however, few have examined conversion rates subsequent to training (Huckans et al., 2013).
To summarize, rapid advances in early identification of AD necessitate development of multi‐dimensional treatment options to halt or slow cognitive deterioration in this population. This study offers preliminary evidence that Gist Training offers a promising protocol to engage and build cognitive capacity in individuals with MCI. More work is needed to establish long term benefits of such approaches in slowing cognitive deterioration and in extending years of functional competency in this population.
Conflict of interest
None declared
Key points.
This represents one of the first randomized pilot training trials to compare the cognitive benefits of a Gist Reasoning Training versus New Learning in Mild Cognitive Impairment (MCI).
The reasoning trained MCI group improved in measures of executive function and memory.
The New Learning MCI group improved on detail memory.
Findings support the potential for Gist Reasoning Training to harness and strengthen the latent cognitive capacities in MCI.
Acknowledgements
This work was supported by grants from the RGK Foundation, and BvB Dallas.
Mudar, R. A. , Chapman, S. B. , Rackley, A. , Eroh, J. , Chiang, H.‐S. , Perez, A. , Venza, E. , and Spence, J. S. (2017) Enhancing latent cognitive capacity in mild cognitive impairment with gist reasoning training: a pilot study. Int J Geriatr Psychiatry, 32: 548–555. doi: 10.1002/gps.4492.
References
- Aisen PS, Petersen RC, Donohue MC, et al. 2010. Clinical core of the Alzheimer's disease neuroimaging initiative: progress and plans. Alzheimers Dement 6: 239–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anand R, Chapman SB, Rackley A, et al. 2011. Gist reasoning training in cognitively normal seniors. Int J Geriat Psychiatry 26: 961–968. [DOI] [PubMed] [Google Scholar]
- Beck A, Steer RA, Brown GK. 1996. Manual for Beck Depression Inventory‐II. The Psychological Corporation: San Antonio, TX. [Google Scholar]
- Becker RE, Greig NH. 2013. Fire in the ashes: can failed Alzheimer's disease drugs succeed with second chances? Alzheimers Dement 9: 50–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belleville S, Clement F, Mellah S, et al. 2011. Training‐related brain plasticity in subjects at risk of developing Alzheimer's disease. Brain 134: 1623–1634. [DOI] [PubMed] [Google Scholar]
- Binder DTG, O' Connor C, Levine B. 2008. Brain health workshop: rotman research institute, Baycrest, Toronto, ON, Canada; University of California, Berkeley, CA.
- Castel AD, Balota DA, McCabe DP. 2009. Memory efficiency and the strategic control of attention at encoding: impairments of value‐directed remembering in Alzheimer's disease. Neuropsychology 23: 297–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castel AD, Farb NAS, Craik FIM. 2007. Memory for general and specific value information in younger and older adults: measuring the limits of strategic control. Mem Cognit 35: 689–700. [DOI] [PubMed] [Google Scholar]
- Chapman SB, Aslan S, Spence JS, et al. 2015. Neural mechanisms of brain plasticity with complex cognitive training in healthy seniors. Cereb Cortex 25: 396–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman SB, Gamino JF, Mudar RA. 2012. Higher order strategic gist reasoning in adolescence In The adolescent brain: learning, reasoning, and decision making. American Psychological Association (APA): Washington, DC: 123–151. [Google Scholar]
- Chapman SB, Mudar RA. 2014. Enhancement of cognitive and neural functions through complex reasoning training: evidence from normal and clinical populations. Front Syst Neurosci 8: . DOI:10.3389/fnsys.2014.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman SB, Zientz J, Weiner M, et al. 2002. Discourse changes in early Alzheimer disease, mild cognitive impairment, and normal aging. Alzheimer Dis Assoc Disord 16: 177–186. [DOI] [PubMed] [Google Scholar]
- Chen AJW, Novakovic‐Agopian T, Nycum TJ, et al. 2011. Training of goal‐directed attention regulation enhances control over neural processing for individuals with brain injury. Brain 134: 1541–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen AD, Klunk WE. 2014. Early detection of Alzheimer's disease using PiB and FDG PET. Neurobiol Dis 72: 117–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotelli M, Manenti R, Zanetti O, Miniussi C. 2012. Non‐pharmacological intervention for memory decline. Front Hum Neurosci 6 DOI:10.3389/fnhum.2012.00046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dayan P, Kakade S, Montague PR. 2000. Learning and selective attention. Nat Neurosci 3: 1218–1223. [DOI] [PubMed] [Google Scholar]
- Feldman HH, Lane R. 2007. Rivastigmine: a placebo controlled trial of twice daily and three times daily regimens in patients with Alzheimer's disease. J Neurol Neurosurg Psychiatry 78: 1056–1063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. 1975. “Mini‐mental state”. a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12: 189–198. [DOI] [PubMed] [Google Scholar]
- Gates NJ, Sachdev PS, Fiatarone Singh MA, Valenzuela M. 2011. Cognitive and memory training in adults at risk of dementia: a systematic review. BMC Geriatr 11: 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenaway MC, Duncan NL, Smith GE. 2012. The memory support system for mild cognitive impairment: randomized trial of a cognitive rehabilitation intervention. Int J Geriatr Psychiatry 28: 402–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenaway MC, Hanna SM, Lepore SW, Smith GE. 2008. A behavioral rehabilitation intervention for amnestic mild cognitive impairment. Am J Alzheimers Dis Other Demen 23: 451–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampstead BM, Gillis MM, Stringer AY. 2014. Cognitive rehabilitation of memory for mild cognitive impairment: a methodological review and model for future research. J Int Neuropsychol Soc 20: 135–51. [DOI] [PubMed] [Google Scholar]
- Hampstead BM, Sathian K, Moore AB, Nalisnick C, Stringer AY. 2008. Explicit memory training leads to improved memory for face–name pairs in patients with mild cognitive impairment: results of a pilot investigation. J Int Neuropsychol Soc 14: 883–889. [DOI] [PubMed] [Google Scholar]
- Hampstead BM, Sathian K, Phillips PA, et al. 2012. Mnemonic strategy training improves memory for object location associations in both healthy elderly and patients with amnestic mild cognitive impairment: a randomized, single‐blind study. Neuropsychology 26: 385–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanten G, Li X, Chapman SB, et al. 2007. Development of verbal selective learning. Dev Neuropsychol 32: 585–596. [DOI] [PubMed] [Google Scholar]
- Huckans M, Hutson L, Twamley E, et al. 2013. Efficacy of cognitive rehabilitation therapies for mild cognitive impairment (MCI) in older adults: working toward a theoretical model and evidence‐based interventions. Neuropsychol Rev 23: 63–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jean L, Bergeron M‐È, Thivierge S, Simard M. 2010. Cognitive intervention programs for individuals with mild cognitive impairment: systematic review of the literature. Am J Geriatr Psychiatry 18: 281–296. [DOI] [PubMed] [Google Scholar]
- Kinsella GJ, Mullaly E, Rand E, et a l. 2009. Early intervention for mild cognitive impairment: a randomised controlled trial. J Neurol Neurosurg Psychiatry 80: 730–736. [DOI] [PubMed] [Google Scholar]
- Levine B, Schweizer TA, O'Connor C, et al. 2011. Rehabilitation of executive functioning in patients with frontal lobe brain damage with goal management training. Front Hum Neurosci 5: . DOI:10.3389/fnhum.2011.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H, Li J, Li N, et al. 2011. Cognitive intervention for persons with mild cognitive impairment: a meta‐analysis. Ageing Res Rev 10: 285–296. [DOI] [PubMed] [Google Scholar]
- Manly JJ, Tang M‐X, Schupf N, et al. 2008. Frequency and course of mild cognitive impairment in a multiethnic community. Ann Neurol 63: 494–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin M, Clare L, Altgassen AM, Cameron MH, Zehnder F. 2011. Cognition‐based interventions for healthy older people and people with mild cognitive impairment In Cochrane Database of Systematic Reviews. Wiley‐Blackwell. [DOI] [PubMed] [Google Scholar]
- Moro V, Condoleo MT, Valbusa V, et al. 2015. Cognitive stimulation of executive functions in mild cognitive impairment: specific efficacy and impact in memory. Am J Alzheimers Dis Other Demen 30: 153–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris JC. 1993. The clinical dementia rating (CDR): current version and scoring rules. Neurology 43: 2412–2412. [DOI] [PubMed] [Google Scholar]
- Novakovic‐Agopian T, Chen AJW, Rome S, et al. 2011. Rehabilitation of executive functioning with training in attention regulation applied to individually defined goals. J Head Trauma Rehabil 26: 325–338. [DOI] [PubMed] [Google Scholar]
- Petersen RC, Caracciolo B, Brayne C, et al. 2014. Mild cognitive impairment: a concept in evolution. J Intern Med 275: 214–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen RC, Doody R, Kurz A, et al. 2001. Current concepts in mild cognitive impairment. Arch Neurol 58: 1985. [DOI] [PubMed] [Google Scholar]
- Rapp S, Brenes G, Marsh AP. 2002. Memory enhancement training for older adults with mild cognitive impairment: a preliminary study. Aging Ment Health 6: 5–11. [DOI] [PubMed] [Google Scholar]
- Rebok GW, Ball K, Guey LT, et al. 2014. Ten‐year effects of the advanced cognitive training for independent and vital elderly cognitive training trial on cognition and everyday functioning in older adults. J Am Geriatr Soc 62: 16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reijnders J, van Heugten C, van Boxtel M. 2013. Cognitive interventions in healthy older adults and people with mild cognitive impairment: a systematic review. Ageing Res Rev 12: 263–275. [DOI] [PubMed] [Google Scholar]
- Reyna VF, Brainerd CJ. 1995. Fuzzy‐trace theory: an interim synthesis. Learning and Individual Differences 7: 1–75. [Google Scholar]
- Reyna VF, Brainerd CJ. 2011. Dual processes in decision making and developmental neuroscience: a fuzzy‐trace model. Dev Rev 31: 180–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyna VF, Lloyd FJ. 2006. Physician decision making and cardiac risk: effects of knowledge, risk perception, risk tolerance, and fuzzy processing. J Exp Psychol Appl 12: 179–195. [DOI] [PubMed] [Google Scholar]
- Roberts RO, Knopman DS, Mielke MM, et al. 2013. Higher risk of progression to dementia in mild cognitive impairment cases who revert to normal. Neurology 82: 317–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon SS, Yokomizo JE, Bottino CMC. 2012. Cognitive intervention in amnestic mild cognitive impairment: a systematic review. Neurosci Biobehav Rev 36: 1163–1178. [DOI] [PubMed] [Google Scholar]
- Stott J, Spector A. 2011. A review of the effectiveness of memory interventions in mild cognitive impairment (MCI). Int Psychogeriatr 23: 526–538. [DOI] [PubMed] [Google Scholar]
- Thal LJ, Ferris SH, Kirby L, et al. 2005. A randomized, double‐blind, study of rofecoxib in patients with mild cognitive impairment. Neuropsychopharmacology 30: 1204–1215. [DOI] [PubMed] [Google Scholar]
- Troyer AK, Rich JB. 2002. Psychometric Properties of a New Metamemory Questionnaire for Older Adults. J Gerontol B Psychol Sci Soc Sci 57: P19–P27. [DOI] [PubMed] [Google Scholar]
- Ulatowska HK, Chapman SB, Highley AP, Prince J. 1998. Discourse in healthy old‐elderly adults: a longitudinal study. Aphasiology 12: 619–633. [Google Scholar]
- Unverzagt FW, Kasten L, Johnson KE, et al. 2007. Effect of memory impairment on training outcomes in ACTIVE. J Int Neuropsychol Soc 13: 953–960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Dijk TA, Kintsch W. 1983. Strategies of Discourse Comprehension. Academic Press: New York, NY. [Google Scholar]
- Vas AK, Chapman SB. 2012. Gist reasoning in adults with traumatic brain injury. International NeuroTrauma Letter 1: 1–12. [Google Scholar]
- Vas AK, Spence J, Chapman SB. 2015. Abstracting meaning from complex information (gist reasoning) in adult traumatic brain injury. J Clin Exp Neuropsychol 37: 152–161. [DOI] [PubMed] [Google Scholar]
- Wechsler D. 1997b. Wechsler Memory Scale ‐. Third edn. San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Wechsler D. 1997a. Wechsler Adult Intelligence Scale III. San Antonio: Harcourt Assessment. [Google Scholar]
- Weiner MW, Veitch DP, Aisen PS, et al. 2013. The Alzheimer's disease neuroimaging initiative: a review of papers published since its inception. Alzheimers Dement 9: e111–e194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson GS, Robertson GJ. 2006. WRAT4 Wide Range Achievement Test: Professional Manual. PAR: Lutz, FL. [Google Scholar]
- Willis SL, Tennstedt SL, Marsiske M, et al. 2006. Long‐term effects of cognitive training on everyday functional outcomes in older adults. JAMA 296: 2805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, et al. 1982. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17: 37–49. [DOI] [PubMed] [Google Scholar]


