Abstract
Choledochal cyst is a rare and often benign congenital cystic dilation throughout the biliary tree. Due to the benign nature of choledochal cyst among early-diagnosed patients, the clinical assumption and diagnosis seem to be of utmost significance. Therefore, we sought to assess different clinical manifestations of choledochal cyst and relevant laboratory findings in infants and older children.
Retrospectively, medical records of all patients with the diagnosis of choledochal cyst between 2005 and 2015 were reviewed. Demographic data, initial clinical presentation, positive findings on physical examination, history of any remarkable behavior such as persistent and unexplained crying and poor feeding, and diagnostic imaging modalities were listed. In addition, laboratory values for total and direct bilirubin, alkaline phosphatase, alanine transaminase, aspartate transaminase, prothrombin time, and partial thromboplastin time (PTT) were recorded for each patient. Patients were divided into 2 groups; younger than 1-year-old (infants), and 1 year to 18 years old (older children). Demographic data, clinical data, and laboratory values were compared between the infants and older children.
Thirty-two patients with a diagnosis of choledochal cyst were included in the study: 9 patients (28.12%) were infants and 23 patients (71.87%) were older children. Abdominal pain was the most common presenting symptom (62.5%), followed by nausea/vomiting (59.4%) and jaundice (28.1%). None of the patients presented with the classic triad of abdominal pain, jaundice, and right upper quadrant mass. Seventeen older children (73.91%) presented with nausea and vomiting, while 2 subjects (22.22%) in the infantile group presented with this feature (P = .01). Similarly, abdominal pain was found in 20 older children (86.95%); however, none of the infants presented with abdominal pain at diagnosis (P < .001). By contrast, the abdominal mass was more detected in infants than the older children (33.33% vs. 0%, P = .01). In terms of laboratory values, the median PTT was 44 and 36 s in infants and older children, respectively (P = .04).
Infants were more likely to present with abdominal mass and older children were more likely to have nausea, vomiting, and abdominal pain. Furthermore, infants had more prolonged PTT than older children, implying a potential bleeding tendency.
Keywords: children, choledochal cyst, infant, symptoms
1. Introduction
Choledochal cyst is a rare and often benign congenital cystic dilation throughout the biliary tree.[1] The incidence of choledochal cyst has been estimated to be 1 in 100,000 to 1 in 150,000 individuals in Western countries with an even higher incidence in some Asian countries (e.g., 1 in 13,000 in Japan). Some authors speculate that different mechanisms contribute to the formation of the disease. However, the exact etiology still remains unclear.[1,2] The most widely used classification of choledochal cyst is based on the site of cystic changes in the biliary tree. Type 1 (most common type) is characterized by a cystic or fusiform dilatation of common biliary duct (CBD). Type 2 is associated with a true CBD diverticulum. Type 3 presents as an intraduodenal choledochocele. Type 4 consists of 2 other subtypes; type 4A is characterized by multiple intra- and extrahepatic cysts, whereas type 4B is quite rare and it is associated with multiple extrahepatic cysts. Type 5, also known as Caroli disease, is associated with single or multiple intrahepatic cysts in combination with simultaneous extrahepatic diseases.[3]
Choledochal cysts are considered benign disorders. However, sometimes their varying clinical presentations among different age groups and delay in diagnosis lead to severe late complications such as malignant transformations, cholangitis, pancreatitis, and cholelithiasis. The classic triad of jaundice, abdominal pain, and abdominal right upper quadrant mass in a female neonate is found only in minority of patients.[4,5] Due to the benign nature of choledochal cyst among early-diagnosed patients, the clinical assumption and diagnosis seem to be of utmost significance. Therefore, we sought to assess different clinical manifestations of choledochal cyst and relevant laboratory findings in infants and older children.
2. Methods
The study was approved by the Medical Ethics Committee of Tabriz University of Medical Sciences. Retrospectively, medical records of all patients with the diagnosis of choledochal cyst between 2005 and 2015 in the university-affiliated Tabriz Children's Hospital were reviewed. Demographic data including age, gender, and date of admission were collected. In addition, initial clinical presentation, positive findings on physical examination, history of any remarkable behavior such as persistent and unexplained crying and poor feeding, and diagnostic imaging modalities were listed. In addition, laboratory values for total and direct bilirubin, alkaline phosphatase (ALP), alanine transaminase (ALT), aspartate transaminase (AST), prothrombin time (PT), and partial thromboplastin time (PTT) were recorded for each patient. Patients were divided into 2 groups; younger than 1-year-old (infants), and 1 year to 18 years old (older children). Demographic data, clinical data, and laboratory values were compared between the infants and older children.
Categorical variables were reported as count and proportion; continuous variables were reported as median and interquartile range. Statistical comparisons were made using Fisher exact test for proportions and the Mann–Whitney test for continuous variables, as determined prior to analysis. A P < .05 was considered statistically significant. Statistical analysis was performed using SPSS for windows (v 19.0, Chicago, IL).
3. Results
Thirty-two patients with a diagnosis of choledochal cyst were included in the study: 9 patients (28.12%) were infants, and 23 patients (71.87%) were older children. The diagnosis of choledochal cyst was established in both infants and older children with a combination of ultrasonography (25 patients), computerized tomography (15 patients), and cholangiography (11 patients). We found type 1 and 4 cysts in 23 (71.87%) and 6 patients (18.75%), respectively. However, cyst type was not determined in the remaining patients (9.37%). Abdominal pain was the most common presenting symptom (20 patients [62.5%]), followed by nausea/vomiting (19 [59.4%]) and jaundice (9 [28.1%]). None of the patients presented with the classic triad of abdominal pain, jaundice, and right upper quadrant mass.
Seventeen older children (73.91%) presented with nausea and vomiting, while 2 subjects (22.22%) in the infantile group presented with this feature (P = .01, Table 1). Similarly, abdominal pain was found in 20 older children (86.95%); however, none of the infants presented with abdominal pain at diagnosis (P < .001, Table 1). By contrast, the abdominal mass was more detected in infants than the older children (33.33% vs. 0%, P = .01, Table 1). There were no significant differences in abdominal distension, jaundice, clay-colored stool, and dark urine between the infants and older children (P > .05, Table 1). Furthermore, 5 older children had 2 of the classic triad symptoms (21.73%), while none of the infants had 2 of the 3 symptoms (P = .28).
Table 1.
Demographic data, clinical features, and laboratory findings for infants and older children with choledochal cyst.
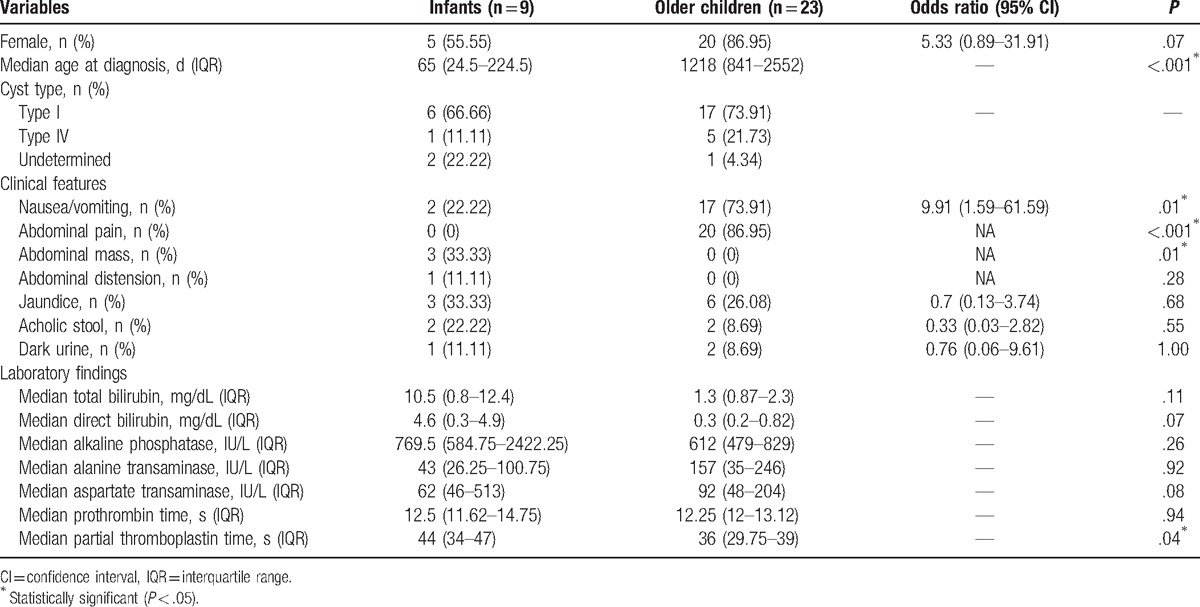
In terms of laboratory values, the median PTT was 44 and 36 s in infants and older children, respectively (P = .04, Table 1). Other laboratory parameters including total and direct bilirubin, ALP, AST, ALT, and PT did not significantly differ between infants and older children (P > .05, Table 1).
4. Discussion
The current study revealed that nausea, vomiting, and abdominal pain were the most common presenting symptoms in older children (1–18 years of age at presentation), while abdominal mass was predominant in infants (<1 year of age at presentation). Our finding on nausea and vomiting (as signs of the biliary tract irritation) is in contrast to that of the study by Hung et al[6] disclosing no difference in vomiting between the infants and classical pediatric group (1–18 years of age at presentation). In addition, Lipsett et al[7] and Edil et al[8] found that nausea and vomiting were similar between the children (<16 years old) and adults.
In the present study, we also found that abdominal pain was more common among older children than infants. Similar to our study, Hung et al[6] and Fumino et al[9] failed to find any abdominal pain in infants, while children had significantly more pain at presentation. Likewise, Tsai et al described a statistically different proportion of abdominal pain presentation between infants and older children (3.8% vs. 50%).[10] In addition, majority of the previous studies reported that adults, compared with children, were more likely to present with abdominal pain.[7,8,10–13] By contrast, a recent multicenter study by Ouaissi et al[14] observed similar proportions of abdominal pain presentation in children and adults. Furthermore, our study demonstrated that the proportion of patients presented with right upper quadrant mass was greater in infants compared with the older children. Consistently, Tsai et al[10] concluded that infants more commonly had abdominal mass in comparison with the children and adults. However, other 2 studies carried out in the setting of infants versus older children with choledochal cyst did not find any significant difference with regard to abdominal mass.[6,9]
The classic triad of abdominal pain, jaundice, and right upper quadrant mass has been reported in 0% to 22% of the patients.[5–8,10,11,13,15,16] In the present study, none of the patients showed the classic triad. Although Tsai et al reported the classic triad in 8/107 (7.47% of their total study population), they noted no difference in proportions of the classic triad among their study groups (infants, children, and adults).[10] Nevertheless, an earlier study by Shah et al[5] concluded that children were more likely to present with the classic triad. Among 42 children and adults with choledochal cyst, Lipsett et al[7] showed that 2 of the 3 classic symptoms were more commonly seen in children; however, our analysis did not result in similar significant difference. Lack of the classic triad in patients with choledochal cyst has been attributed to having access to and seeking medical care at the onset of symptoms.[13]
The present study yielded no evidence to suggest a difference between the infants and older children in terms of abdominal distension, jaundice, clay-colored stool, and dark urine. By contrast, the majority of previous investigations of choledochal cyst in infants and children revealed that jaundice was more commonly seen in infants.[6,9–11] In addition, our observation about the clay-colored stool is in contrast to that previously reported by Hung et al[6]: infants displayed acholic stool more commonly than the children.
Indeed, a few previous reports have indicated changing pattern of laboratory values in the setting of infants and older children. Notably, reports are indicative of bleeding tendency (prolonged PT and PTT) with manifestations such as intracranial hemorrhage, subcutaneous bleeding, bloody stools, or hematuria in infants compared with older children.[9,17–20] This rare finding is consistent with our study, in which we observed prolonged PTT in infants than older children. In addition, Tsai et al[10] showed that compared with children, infants had higher total and direct bilirubin levels, and lower liver function markers (ALP, AST, and ALT). Our study failed to detect any difference in these laboratory values between infants and older children.
This study had certain limitations. First, relatively small number of patients in our study could be increased by a multi-institutional design or a longer study period. The latter, however, might be challenging due to the less advanced imaging and detection modalities. Second, the study population only included type 1 and 4 cysts, while types of the remaining cysts were undetermined. Third, the present study did not consider operative and postoperative information for determining potential predictive factors for postoperative outcomes and complications. Fourth, we did not include laboratory values for biliary amylase, lipase, and gamma-glutamyl transpeptidase. However, one notable strength of the present study is the evaluation of different clinical presentations in the setting of infants and older children. Our observations on the symptoms and laboratory findings of choledochal cyst in infants could be useful in early diagnosis of the disease and minimizing late complications.
In conclusion, there is a changing pattern of choledochal cyst presentation between infancy and older childhood. Infants were more likely to present with abdominal mass and older children were more likely to have nausea, vomiting, and abdominal pain. Furthermore, infants had more prolonged PTT than older children, implying a potential bleeding tendency.
Acknowledgment
The authors wish to thank Taybe Deyhim, PhD (Faculty of Foreign Languages, Sciences and Researches Branch, Islamic Azad University, Tehran, Iran) for her language editing.
Footnotes
Abbreviations: ALP = alkaline phosphatase, ALT = alanine transaminase, AST = aspartate transaminase, CBD = common biliary duct, PT = prothrombin time, PTT = partial thromboplastin time.
The present study was financially supported by the Tabriz University of Medical Sciences, Tabriz, Iran.
The authors have no conflicts of interest to disclose.
References
- [1].Soares KC, Arnaoutakis DJ, Kamel I, et al. Choledochal cysts: presentation, clinical differentiation, and management. J Am Coll Surg 2014;219:1167–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Sato M, Ishida H, Konno K, et al. Choledochal cyst due to anomalous pancreatobiliary junction in the adult: sonographic findings. Abdom Imaging 2001;26:395–400. [DOI] [PubMed] [Google Scholar]
- [3].Ohashi T, Wakai T, Kubota M, et al. Risk of subsequent biliary malignancy in patients undergoing cyst excision for congenital choledochal cysts. J Gastroenterol Hepatol 2013;28:243–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Nicholl M, Pitt HA, Wolf P, et al. Choledochal cysts in western adults: complexities compared to children. J Gastrointest Surg 2004;8:245–52. [DOI] [PubMed] [Google Scholar]
- [5].Shah OJ, Shera AH, Zargar SA, et al. Choledochal cysts in children and adults with contrasting profiles: 11-year experience at a tertiary care center in Kashmir. World J Surg 2009;33:2403–11. [DOI] [PubMed] [Google Scholar]
- [6].Hung MH, Lin LH, Chen DF, et al. Choledochal cysts in infants and children: experiences over a 20-year period at a single institution. Eur J Pediatr 2011;170:1179–85. [DOI] [PubMed] [Google Scholar]
- [7].Lipsett PA, Pitt HA, Colombani PM, et al. Choledochal cyst disease. A changing pattern of presentation. Ann Surg 1994;220:644–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Edil BH, Cameron JL, Reddy S, et al. Choledochal cyst disease in children and adults: a 30-year single-institution experience. J Am Coll Surg 2008;206:1000–5. [DOI] [PubMed] [Google Scholar]
- [9].Fumino S, Ono S, Shimadera S, et al. Impact of age at diagnosis on clinical features in children with anomalous arrangement of the pancreaticobiliary duct. Eur J Pediatr Surg 2010;20:325–9. [DOI] [PubMed] [Google Scholar]
- [10].Tsai MS, Lin WH, Hsu WM, et al. Clinicopathological feature and surgical outcome of choledochal cyst in different age groups: the implication of surgical timing. J Gastrointest Surg 2008;12:2191–5. [DOI] [PubMed] [Google Scholar]
- [11].de Vries JS, de Vries S, Aronson DC, et al. Choledochal cysts: age of presentation, symptoms, and late complications related to Todani's classification. J Pediatr Surg 2002;37:1568–73. [DOI] [PubMed] [Google Scholar]
- [12].Huang CS, Huang CC, Chen DF. Choledochal cysts: differences between pediatric and adult patients. J Gastrointest Surg 2010;14:1105–10. [DOI] [PubMed] [Google Scholar]
- [13].Soares KC, Kim Y, Spolverato G, et al. Presentation and clinical outcomes of choledochal cysts in children and adults: a multi-institutional analysis. JAMA Surg 2015;150:577–84. [DOI] [PubMed] [Google Scholar]
- [14].Ouaissi M, Kianmanesh R, Ragot E, et al. Congenital bile duct cyst (BDC) is a more indolent disease in children compared to adults, except for Todani type IV-A BDC: results of the European multicenter study of the French Surgical Association. HPB (Oxford) 2016;18:529–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Stringer MD, Dhawan A, Davenport M, et al. Choledochal cysts: lessons from a 20 year experience. Arch Dis Child 1995;73:528–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Liem NT, Pham HD, Dung Le A, et al. Early and intermediate outcomes of laparoscopic surgery for choledochal cysts with 400 patients. J Laparoendosc Adv Surg Tech A 2012;22:599–603. [DOI] [PubMed] [Google Scholar]
- [17].Chen TY, Wang HK, Yeh ML, et al. Subdural hemorrhage as a first symptom in an infant with a choledochal cyst: case report. J Neurosurg Pediatr 2012;9:414–6. [DOI] [PubMed] [Google Scholar]
- [18].Ono S, Tokiwa K, Aoi S, et al. A bleeding tendency as the first symptom of a choledochal cyst. Pediatr Surg Int 2000;16:111–2. [DOI] [PubMed] [Google Scholar]
- [19].Fumino S, Iwai N, Deguchi E, et al. Bleeding tendency as a first symptom in children with congenital biliary dilatation. Eur J Pediatr Surg 2007;17:2–5. [DOI] [PubMed] [Google Scholar]
- [20].Krstovski N, Janic D, Dokmanovic L, et al. Late vitamin K deficiency bleeding in an infant with choledochal cyst. Turk J Pediatr 2010;52:652–4. [PubMed] [Google Scholar]


