Abstract
Background
The benefits of noninvasive positive pressure ventilation (NPPV) in patients with hypercapnic COPD are controversial. It is presumed that methodology and appropriate use of NIV ventilator might be crucial for the outcomes. With the new built-in software, the performance of NIV can be monitored at home, which can guarantee the compliance and appropriate use. This study investigated effects of home use of NIV in hypercapnia in COPD patients using the NIV ventilator with built-in software for monitoring.
Methods
The current multicenter prospective, randomized, controlled trial enrolled patients with stable GOLD stages III and IV hypercapnic COPD. Patients were randomly assigned via a computer-generated randomization sequence, with a block size of four patients, to continue optimized treatment (control group) or to receive additional NPPV (intervention group) for 3 months. The primary outcome was arterial carbon dioxide pressure (PaCO2). Data were derived from built-in software and analyzed every 4 weeks. Analysis was carried out with the intention to treat. This study is registered with ClinicalTrials.gov, number NCT02499718.
Results
Patients were recruited from 20 respiratory units in China from October 1, 2015, and recruitment was terminated with a record of the vital statistics on May 31, 2016. A total of 115 patients were randomly assigned to the NPPV group (n=57) or the control group (n=58). Patients complied well with NPPV therapy (mean [± standard deviation] day use 5.6±1.4 h). The mean estimation of leaks was 37.99±13.71 L/min. The changes in PaCO2 (−10.41±0.97 vs −4.32±0.68 mmHg, P=0.03) and 6-min walk distance (6MWD) (38.2% vs 18.2%, P=0.02) were statistically significant in the NPPV group versus the control group. COPD assessment test (CAT) showed a positive trend (P=0.06) in favor of the NPPV group. Pulmonary function and dyspnea were not different between groups.
Conclusion
Ventilators equipped with built-in software provided methodology for monitoring NIV use at home, which could facilitate the improvement of compliance and quality control of NIV use. It was shown that three months use of NIV at home could reduce the PaCO2 and improve exercise tolerance (6MWD) in chronic hypercapnic COPD patients.
Keywords: COPD, noninvasive positive pressure ventilation, long-term oxygen therapy, chronic respiratory failure, built-in software
Introduction
COPD is an increasing important cause of morbidity and mortality worldwide and leads to a significant economic and social burden.1,2 Advanced-stage COPD is characterized by irreversible severe flow limitation and chronic hypercapnia. The mechanisms related to chronic hypercapnia in COPD include the imbalance of respiratory impedance and reduced respiratory muscle function. Chronic hypercapnia could result in respiratory acidosis and desensitization of respiratory central drive in response to hypercapnia. Noninvasive ventilation (NIV) is possible to unload the respiratory muscles, reduce hypercapnia and restore the sensitivity of respiratory center.3
Physiological studies in literature had shown that NIV could improve ventilation as well as important physiological variables such as lung hyperinflation and blood gases4 in COPD patients with hypercapnia. Results from several clinical studies showed improvements in survival, exercise capacity, health-related quality of life (HRQL) and sleep quality.5–8 In addition, NIV use at home might be associated with lower overall treatment costs and fewer hospital admissions.9 On the other hand, there were also reports showing that NIV provided no additional benefits than long-term oxygen therapy alone in patient’s survival rate, hospital admission rate, arterial blood gases and quality of life. The reasons for these controversial results are unclear. Patient selection, methodology and quality control of NIV were supposed to be the main reasons for explanation of discrepancy of different studies results. Respiratory events occur during home NIV, such as asynchrony and leakage, are common and not readily detectable at home use setting. Compliance and ventilator parameters settings are another important factors attributable to the outcomes of NIV. NIV ventilator with built-in software for monitoring and recording can provided the possibility to check the compliance of use and respiratory events during NIV treatment,10,11 so that clinician can find out and fix the problem.
This study thus aims to investigate the effects of home NIV on stable COPD patients with chronic hypercapnic respiratory failure by using NIV ventilator equipped with built-in software.
Methods
Ethics statement
The study was approved by The First Affiliated Hospital of Guangzhou Medical University Ethics Committee, China. Informed consent was obtained from COPD patients or surrogates (the next of kin who had the authority to sign on behalf of the inclusive patients in case patients were illiterate) before participating in this study. The trial was registered with ClinicalTrials.gov, number NCT02499718.
Study design and patients
Our study was a multicenter prospective, randomized, controlled clinical trial using a prospective, randomized, open, blinded endpoint (PROBE) design.12 Patients were recruited from 20 respiratory units from October 1, 2015, and recruitment was terminated with a record of the vital statistics on May 31, 2016. Patients with clinically stable, GOLD stages III and IV flow limitation and chronic hypercapnic (prolonged hypercapnia during daytime at rest without oxygen or ventilatory support for at least 3 months), aged ≥40 years, were eligible for this study. Patients were judged as clinically stable if they had no acute exacerbation, which was defined as an increase in or new onset of more than one respiratory symptom (cough, sputum production, sputum purulence, dyspnea, and wheezing) lasting ≥2 days and requiring any change of pharmacological treatment during the 4-week run-in period before randomization.
Patients were ineligible if they had abnormalities of the lung or thorax other than COPD. Additional exclusion criteria were previously initiated NPPV (NPPV was used as a routine therapy in home before inclusion), obstructive sleep apnea, COPD with obstructive sleep apnea overlap syndrome, severe heart failure (New York Heart Association stage IV), severe arrhythmias, unstable angina, and malignant comorbidities. We also did not include the COPD patients in impaired general condition that could preclude follow-up visit. We did not include highly selected patients to maintain the generalizability of the results. COPD patients were recorded the screening procedure (including eligible, not eligible, and randomized) in a screening log.
Randomization and masking
After a 4-week run-in period, patients were admitted to hospital and randomly distributed to one of the following two groups: NPPV group and control group (LTOT). Randomization was via a computer-generated block randomization lists with a block size of four patients. When a patient was included, the peripheral investigators contacted an independent study coordinator, who would register patient’s baseline data and disclosed the group allocation for this patient. The intervention was unblinded as an effective sham noninvasive ventilator is not available; however, outcome assessors were blinded to treatment assignment throughout the trial.
Study procedure and ventilator setting
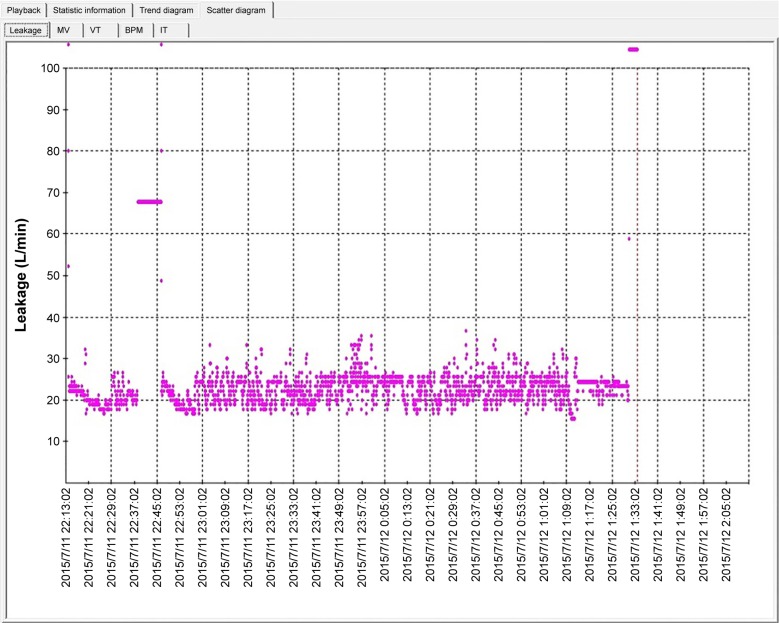
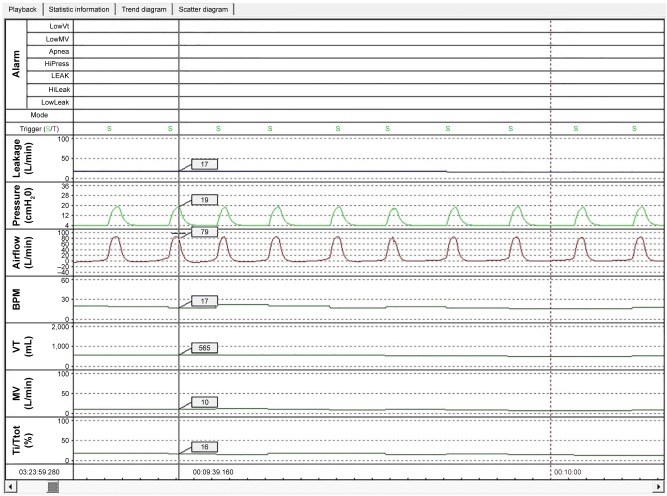
All included patients received regular maintenance pharmacologic treatments as well as home long term oxygen therapy (LTOT) according to the recommendation of GOLD 2014 at least since the run-in period. All patients received LTOT via nasal cannula at a flow rate of 1–3 L/min to achieve oxygen saturation ≥90% and the cumulative time was at least 15 hrs daily.13 In the NIV group, NIV was used at home setting, at least 5 hrs daily. The built-in software installed in the ventilator could record the parameters (including estimation of leaks, inspiratory positive airway pressure [IPAP], expiratory positive airway pressure [EPAP], tidal volume, minute ventilation, respiratory rate, back-up frequency, and percentage of inspirations triggered by the patient) (Figures 1 and 2). The time of using NIV depended on patient’s preference, although we recommend the patients to use NIV during sleep as the first choice.
Figure 1.
Scatter plot of leak recorded in built-in software.
Abbreviations: MV, minute volume; Vt, tidal volume; BPM, breath per minuter; IT, inspiratory time.
Figure 2.
Parameters recorded in built-in software.
Abbreviations: MV, minute volume; Vt, tidal volume; BPM, breath per minuter; IT, inspiratory time.
Flexo ST 30 NIV ventilator (Curative Co. SuZhou, People’s Republic of China) was used for the study. The parameter settings were as following. S/T mode, EPAP set at 4 cmH2O and backup frequency at 16 breaths/min. The IPAP was titrated by gradually increasing IPAP to the maximally tolerated level and IPAP–EPAP difference (pressure support level) more than 10 cmH2O7. The Face masks or nasal masks were used according to the patients’ comfort and preference. After randomization, all patients in NIV group receive at least one hour NIV treatment in hospital setting in order to get used to NIV treatment under the observation of study staff who were trained to provide NIV treatment. Furthermore, education of patients and patient’s family members was provided for ventilator use, mask fitting, etc.
Our primary endpoint was PaCO2. We did all blood gas measurements from arterialized capillary blood during spontaneous breathing, at least 1 h after the patients in the intervention group had switched from NPPV to spontaneous breathing. We assessed HRQL using the Severe Respiratory Insufficiency (SRI) Questionnaire14,15 and the COPD assessment test (CAT) as tools. We estimated pulmonary function, 6-min walk distance (6MWD), blood oxygen saturation, baseline dyspnea index (BDI), and transition dyspnea index (TDI) as previously specified.16–18 The estimators who took these measurements were blinded to treatment assignment and not involved in the study.
Statistical analysis
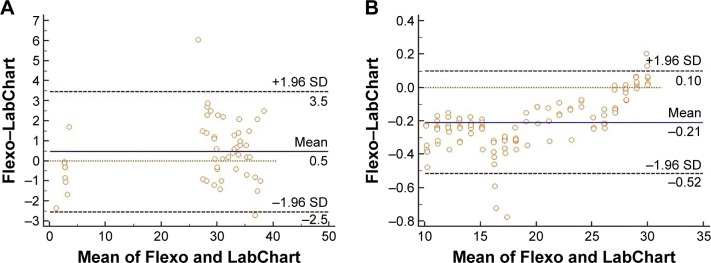
Statistical analyses were performed using SPSS 17.0 for Windows (SPSS Inc, Chicago, IL, USA). All primary analyses, as well as the primary endpoint analysis, were conducted on an intention to treat analysis (ITT). One-way analysis of variance was used to analyze the effect of NPPV on changes from baseline to follow-up of endpoints (forced vital capacity [FVC], forced expiratory volume in 1 s [FEV1], arterial oxygen pressure [PaO2], PaCO2, arterial oxygen saturation [SaO2], pH, TDI, and HRQL summary measures [SRI and CAT]). Chi-square test was used for comparing the differences between the two groups. P<0.05 was considered as statistically significant. Bland–Altman plots were used to evaluate the differences of ventilator parameters between the data from the built-in software and the PowerLab system. The range of agreement was shown with 95% limits of agreement (LoA) that stands for the mean difference ±1.96 SD. Narrower 95% LoA indicated better agreement.
Results
Among the 174 patients, 115 patients met the criteria and were enrolled in this study (Figure 3). Among them, 57 and 58 patients were in the intervention and control groups, respectively. The baseline characteristics were similar in these two groups (Table 1). As expected, approximately two-thirds of the subjects were male, with a mean age in the late 65 years. Patients had severe airflow obstruction and very low carbon monoxide gas transfer consistent with significant awake hypoxemia and hypercapnia while breathing room air. A total of 55 patients in the intervention group completed the study, and two patients (3.5%) discontinued NPPV treatment: the reasons were mask intolerance in one patient and patients’ impression of uselessness of NPPV in one patient. A total of 55 patients in the control arm successfully completed the study. One patient’s death and two patients’ drop-off were recorded, whereas the rate of loss was 5.1%.
Figure 3.
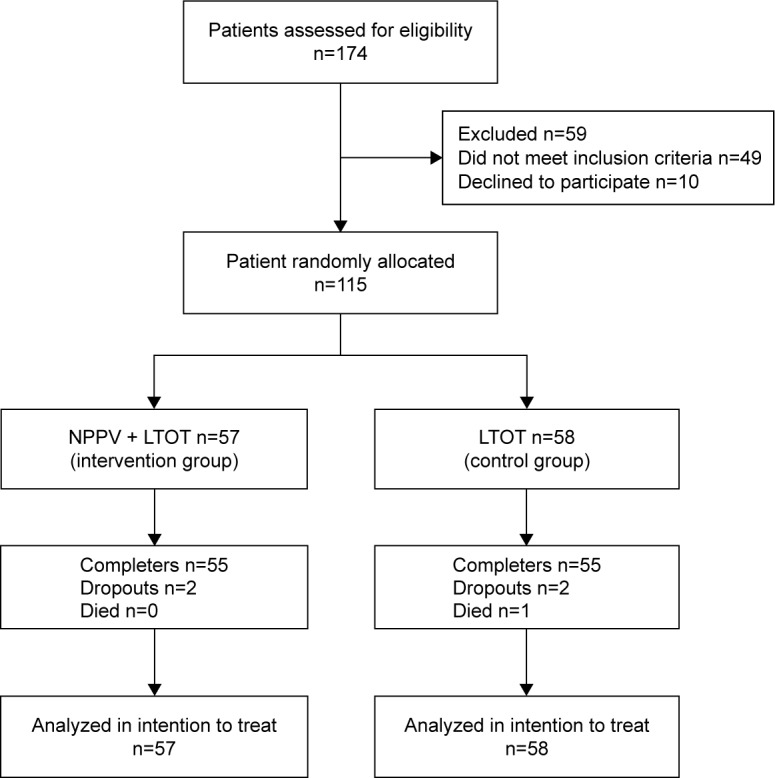
CONSORT flow diagram.
Abbreviations: CONSORT, consolidated standards of reporting trials; LTOT, long-term oxygen therapy; NPPV, noninvasive positive pressure ventilation.
Table 1.
Baseline demographic and clinical characteristics of patients
| NPPV + LTOT | LTOT | |
|---|---|---|
| Male, n (%) | 36 (80) | 35 (77.78) |
| Age, years | 66.91±7.10 | 68.47±6.57 |
| BMI, kg/m2 | 19.43±3.10 | 20.56±3.36 |
| SaO2, % | 90.80±4.61 | 92.44±3.11 |
| IPAP, mmH2O | 17.8±2.08 | – |
| EPAP, mmH2O | 4.2±0.1 | – |
| ΔPS, mmH2O | 12.29±2.08 | – |
| pH | 7.37±0.04 | 7.36±0.05 |
| PaCO2, mmHg | 57.78±2.88 | 58.07±3.50 |
| PaO2, mmHg | 69.76±15.83 | 73.99±27.85 |
| FVC, L | 1.60±0.65 | 1.48±0.53 |
| FVC, % predicted | 51.16±16.45 | 50.26±17.28 |
| FEV1, L | 0.55±0.19 | 0.62±0.22 |
| FEV1, % predicted | 23.34±7.48 | 28.02±11.97 |
| FEV1/FVC, % | 37.56±9.66 | 38.05±17.36 |
Notes: Data are mean ± SD, unless otherwise stated. ΔPS= IPAP-EPAP.
Abbreviations: BMI, body mass index; EPAP, expiratory positive airway pressure; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; IPAP, inspiratory positive airway pressure; LTOT, long-term oxygen therapy; NPPV, noninvasive positive pressure ventilation; PaO2, arterial oxygen pressure; PaCO2, arterial carbon dioxide pressure; SaO2, arterial oxygen saturation.
The mean inspiratory pressure was 17.8±2.08 cmH2O, and the mean expiratory pressure was 4.2±0.1 cmH2O. Patients on NPPV adhered well to the therapy. The overall compliance to NIV treatment was well. Mean time of NIV usage was 5.6±1.4h per day. A total of 48 patients (84%) exceeded the prescribed usage time of >5 h/day. The usage time was <4 h in 8.7% of patients. The mean estimation of leak was 37.99±13.71 L/min, among whom 87% of the patients displayed with leak <40 L/min. The mean estimation of leak recorded in the ventilator was 37.99±13.71 L/min. In the LTOT treatment arm, the mean LTOT usage was 16.8 h/day and 52 patients (90%) exceeded the prescribed usage time of >15 h/day.
Bland–Altman plots showed a low mean bias value between two measurements (PowerLab system and ventilator), as shown in Figure 4. In comparing the estimation of leak, we observed the lowest bias values (0.5 L/min) and the lowest LoA values (−2.5 to 3.5 L/min). In the estimation of pressure, the lowest bias value was −0.21 cmH2O and the lowest LoA value was −0.52 to 0.1 cmH2O. All the above results supported that the built-in software could provide accurate monitoring of the performance of the ventilator.
Figure 4.
Bland-Altman plots for absolute reliability of parameters estimation between the Flexo and LabChart.
Notes: (A) Bland–Altman plots for absolute reliability (means vs differences) of leak estimation between the Flexo and LabChart. (B) Bland–Altman plots for absolute reliability (means vs differences) of pressure estimation between the Flexo and LabChart.
Abbreviation: SD, standard deviation.
For the primary endpoint, 55 (96%) of the 57 patients in the intervention group and 55 (95%) of the 58 patients in the control group finished the follow-up visit. Comparing with the baseline, the decrease in PaCO2 was evident in the intervention group than in the control group (−10.41±0.97 vs −4.32±0.68 mmHg, P=0.03). Furthermore, the rate of subjects with more than the minimum clinical improvement of 6MWT was higher in NIV group than in the control group (21 [38.2%] vs 10 [18.2%], P=0.02) (Table 2). The change in CAT scores had a positive trend in the intervention arm than in the control arm (−4.98±6.25 vs −3.31±4.28, P=0.06). However, no significant between-group differences were noted for changes in SRI scores, SaO2, pH, PaO2, BE, FVC, FEV1, FEV1/FVC, and TDI (all P>0.05) (Table 3). Seven patients (12%) reported skin rash at the facial skin, which could be managed by changing mask. We did not judge this as a relevant adverse event as minor skin lesions can often happen during noninvasive ventilation.
Table 2.
6MWD
| Group | 6MWD change, n
|
Total | |
|---|---|---|---|
| Improved (Δd ≥54 min) | Unimproved (Δd <54 min) | ||
| LTOT | 10 | 48 | 58 |
| NPPV + LTOT* | 21 | 36 | 57 |
| Total | 31 | 84 | 115 |
Note:
Chi-square test, P=0.02.
Abbreviations: LTOT, long-term oxygen therapy; 6MWD, 6-min walk distance; NPPV, noninvasive positive pressure ventilation.
Table 3.
Treatment period effect between two groups
| 90 days change from baseline (95% confidence interval)
|
Difference | P-value | ||
|---|---|---|---|---|
| NPPV + LTOT | LTOT | |||
| SaO2 | 1.2% (−0.8% to 3.2%) | 0.3% (−0.8% to 1.5%) | 0.9% (−0.6% to 2.4%) | 0.15 |
| FVC | 6.6% (−6.4% to 18.6%) | 6.7% (0.6% to 12.8%) | −0.1% (−5.6% to 23.1%) | 0.20 |
| FEV1 | 17.3% (−8.5% to 43.2%) | −1.4% (−7.7% to 5.0%) | 18.7% (−5.4% to 33.6%) | 0.10 |
| pH | 0.002 (0 to 0.003) | 0.002 (0 to 0.004) | −0.001 (0.001 to 0.002) | 0.56 |
| PaCO2 | −17.7% (−21.5% to −13.9%) | −7.2% (−9.7% to −5.7%) | −10.5% (−4.7% to −12.3%) | 0.03 |
| PaO2 | 4.3% (−4.6% to 13.2%) | −3.1% (−9.6% to 3.5%) | 7.4% (−5.4% to 4.1%) | 0.58 |
| SRI | 24.7% (15.3% to 34.1%) | 5.5% (−0.9% to 11.9%) | 19.2% (2.1% to 17.6%) | 0.21 |
| CAT | −14.7% (−21.3% to −10.2%) | −11.9% (−18.3% to −5.5%) | 6.8% (−20.3% to −4.2%) | 0.06 |
| TDI | −6.9% (9.6% to −4.2%) | −9.4% (−11.9% to −6.9%) | 2.5% (5.3% to −3.2%) | 0.79 |
Abbreviations: CAT, COPD assessment test; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; LTOT, long-term oxygen therapy; NPPV, noninvasive positive pressure ventilation; PaO2, arterial oxygen pressure; PaCO2, arterial carbon dioxide pressure; SaO2, arterial oxygen saturation; SRI, Severe Respiratory Insufficiency; TDI, Transitional Dyspnea Index.
Discussion
This is the first randomized controlled trial report to date of using NIV ventilator equipped with built-in software to monitor the ventilator parameters in home setting in stable hypercapnic COPD patients. In order to estimate the accuracy of built-in software in ventilators, data downloaded from software were compared using the PowerLab system. The finding showed that the estimation of leak and pressure was a low mean bias value between built-in software and PowerLab system. Previous study showed that the rate of abnormalities was 66% and leak was the most common abnormality (34.2%) followed by desaturation dips (23.8%) in home NPPV.19 In addition, studies have further reported that leak increases ineffective trigger, patient–ventilator asynchrony, and hypoventilation in patients.20–22 In our study, the mean estimation of leak was 37.99 L/min and 87% of the leaks were <40 L/min, which was greatly lower than the threshold leak influencing the effects of NPPV as reported by previous study,23 which could ensure the appropriateness of NIV use and reliability of the results.
By using built-in software, ventilators, respiratory events were occurring in 12 patients (21%) during NPPV, which were corrected by study staff to ensure the proper use of NPPV. Also, this trial provided evidence that three months use of NPPV at home could improve PaCO2 and 6MWD in chronic stable COPD with hypercapnia as compared with LTOT alone. Quality of life (CAT scores) was shown to have tendency of improvement, but the improvement did not reach the level of statistical significance (P=0.06) probably due to the small sample size. Additionally, NPPV treatment was not associated with significant improvements in pulmonary function and dyspnea.
Struik et al24 found that the level of PaCO2 in hypercapnic COPD patients, who received NPPV for >5 h, decreased remarkably after 3 months. The findings of our study similarly confirmed that NPPV plus LTOT could significantly reduce PaCO2 than LTOT alone, which may be associated with noninvasive ventilation that could unload respiratory muscles fatigue and reset central respiratory drive. Another important finding was that NPPV significantly improved the exercise endurance of the hypercapnic COPD patients (the mechanisms related to this improvement are not clear and were not studied in this trial). We hypothesized that NIV might be able to improve quality of life if NPPV were used for longer time in a larger population. The minimal clinical improvement in the 6MWD of 54 min25 was reached in 21 (36.8%) patients in the NPPV group versus 10 (17.2%) patients in the control group (P=0.02). Although we did not observe statistical significance in the scores of SRI and CAT between the two groups, our findings suggested that NPPV tended to improve the quality of life of COPD patients and the negative outcomes could be associated with the short follow-up visit (3 months). Additionally, no significant improvements in pulmonary function were found in the present study at 3 months after intervention, which was in agreement with the results reported in previous studies.6,24
Nevertheless, the current study presents several limitations. First, the average IPAP was only 17.8 cmH2O. In recent years, some researchers stressed the importance of high-intensity noninvasive ventilation.26–28 However, patients included in those studies were European and American who were different from Asian patients. Although the mean pressure was low in the present study, we demonstrated that NPPV also decreased the PaCO2 and improved the exercise endurance and had a positive trend in improving the quality of life. Second, the follow-up time was short (3 months) in this study. In our future studies, ventilators equipped with built-in software will be used for the evaluation of the long-term effects of NPPV (including the survival, the frequency of acute exacerbation of COPD, and economic evaluation of the cost of COPD) in stable hypercapnic COPD patients.
Conclusion
Ventilators equipped with built-in software provided methodology for monitoring NPPV use at home, which could facilitate the improvement of compliance and quality control of NPPV use. It was shown that three months use of NPPV at home could reduce the PaCO2 and improve exercise tolerance (6MWD) in chronic hypercapnic COPD patients.
Acknowledgments
The authors wish to thank the Curative for providing the ventilators. The study was supported by the Natural Science Foundation of China (NSFC; 813111129) and the Science and Technology Project of Guangdong Province (2014A020215033).
Footnotes
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors received financial support from Curative Medical Co. China for the research. The authors report no other conflicts of interests in this work.
References
- 1.Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2016. [Accessed January 6, 2016]. Available from: http://goldcopd.org.
- 2.Narsingam S, Bozarth AL, Abdeljalil A. Updates in the management of stable chronic obstructive pulmonary disease. Postgrad Med. 2015;127(7):758–770. doi: 10.1080/00325481.2015.1084212. [DOI] [PubMed] [Google Scholar]
- 3.Gea J, Agusti A, Roca J. Pathophysiology of muscle dysfunction in COPD. J Appl Physiol. 2013;114(9):1222–1234. doi: 10.1152/japplphysiol.00981.2012. [DOI] [PubMed] [Google Scholar]
- 4.Windisch W, Kostic S, Dreher M, Virchow JC, Jr, Sorichter S. Outcome of patients with stable COPD receiving controlled noninvasive positive pressure ventilation aimed at a maximal reduction of Pa(CO2) Chest. 2005;128(2):657–662. doi: 10.1378/chest.128.2.657. [DOI] [PubMed] [Google Scholar]
- 5.Bhatt SP, Peterson MW, Wilson JS, Durairaj L. Noninvasive positive pressure ventilation in subjects with stable COPD: a randomized trial. Int J Chron Obstruct Pulmon Dis. 2013;8:581–589. doi: 10.2147/COPD.S53619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kohnlein T, Windisch W, Kohler D, et al. Non-invasive positive pressure ventilation for the treatment of severe stable chronic obstructive pulmonary disease: a prospective, multicentre, randomised, controlled clinical trial. Lancet Respir Med. 2014;2(9):698–705. doi: 10.1016/S2213-2600(14)70153-5. [DOI] [PubMed] [Google Scholar]
- 7.McEvoy RD, Pierce RJ, Hillman D, et al. Australian trial of non-invasive Ventilation in Chronic Airflow Limitation (AVCAL) Study Group Nocturnal non-invasive nasal ventilation in stable hypercapnic COPD: a randomised controlled trial. Thorax. 2009;64(7):561–566. doi: 10.1136/thx.2008.108274. [DOI] [PubMed] [Google Scholar]
- 8.Casanova C, Celli BR, Tost L, et al. Long-term controlled trial of nocturnal nasal positive pressure ventilation in patients with severe COPD. Chest. 2000;118(6):1582–1590. doi: 10.1378/chest.118.6.1582. [DOI] [PubMed] [Google Scholar]
- 9.Tuggey JM, Plant PK, Elliott MW. Domiciliary non-invasive ventilation for recurrent acidotic exacerbations of COPD: an economic analysis. Thorax. 2003;58(10):867–871. doi: 10.1136/thorax.58.10.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pasquina P, Adler D, Farr P, Bourqui P, Bridevaux PO, Janssens JP. What does built-in software of home ventilators tell us? An observational study of 150 patients on home ventilation. Respiration. 2012;83(4):293–299. doi: 10.1159/000330598. [DOI] [PubMed] [Google Scholar]
- 11.Janssens JP, Borel JC, Pepin JL, groupe SomnoVNI Nocturnal monitoring of home non-invasive ventilation: the contribution of simple tools such as pulse oximetry, capnography, built-in ventilator software and autonomic markers of sleep fragmentation. Thorax. 2011;66(5):438–445. doi: 10.1136/thx.2010.139782. [DOI] [PubMed] [Google Scholar]
- 12.Hansson L, Hedner T, Dahlof B. Prospective randomized open blinded end-point (PROBE) study. A novel design for intervention trials. Prospective randomized open blinded end-point. Blood Press. 1992;1(2):113–119. doi: 10.3109/08037059209077502. [DOI] [PubMed] [Google Scholar]
- 13.Hardinge M, Suntharalingam J, Wilkinson T, British Thoracic Society Guideline update: The British Thoracic Society Guidelines on home oxygen use in adults. Thorax. 2015;70(6):589–591. doi: 10.1136/thoraxjnl-2015-206918. [DOI] [PubMed] [Google Scholar]
- 14.Windisch W, Budweiser S, Heinemann F, Pfeifer M, Rzehak P. The Severe Respiratory Insufficiency Questionnaire was valid for COPD patients with severe chronic respiratory failure. J Clin Epidemiol. 2008;61(8):848–853. doi: 10.1016/j.jclinepi.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 15.Walterspacher S, July J, Kohlhaufl M, Rzehak P, Windisch W. The Severe Respiratory Insufficiency Questionnaire for subjects with COPD with long-term oxygen therapy. Respir Care. 2016;61(9):1186–1191. doi: 10.4187/respcare.04574. [DOI] [PubMed] [Google Scholar]
- 16.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 17.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 18.Wanger J, Clausen JL, Coates A, et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26(3):511–522. doi: 10.1183/09031936.05.00035005. [DOI] [PubMed] [Google Scholar]
- 19.Rabec C, Georges M, Kabeya NK, et al. Evaluating noninvasive ventilation using a monitoring system coupled to a ventilator: a bench-to-bedside study. Eur Respir J. 2009;34(4):902–913. doi: 10.1183/09031936.00170508. [DOI] [PubMed] [Google Scholar]
- 20.Ueno Y, Nakanishi N, Oto J, Imanaka H, Nishimura M. A bench study of the effects of leak on ventilator performance during noninvasive ventilation. Respir Care. 2011;56(11):1758–1764. doi: 10.4187/respcare.01145. [DOI] [PubMed] [Google Scholar]
- 21.Branson RD, Blakeman TC, Robinson BR. Asynchrony and dyspnea. Respir Care. 2013;58(6):973–989. doi: 10.4187/respcare.02507. [DOI] [PubMed] [Google Scholar]
- 22.Carteaux G, Lyazidi A, Cordoba-Izquierdo A, et al. Patient-ventilator asynchrony during noninvasive ventilation: a bench and clinical study. Chest. 2012;142(2):367–376. doi: 10.1378/chest.11-2279. [DOI] [PubMed] [Google Scholar]
- 23.Borel JC, Sabil A, Janssens JP, et al. Intentional leaks in industrial masks have a significant impact on efficacy of bilevel noninvasive ventilation: a bench test study. Chest. 2009;135(3):669–677. doi: 10.1378/chest.08-1340. [DOI] [PubMed] [Google Scholar]
- 24.Struik FM, Sprooten RT, Kerstjens HA, et al. Nocturnal non-invasive ventilation in COPD patients with prolonged hypercapnia after ventilatory support for acute respiratory failure: a randomised, controlled, parallel-group study. Thorax. 2014;69(9):826–834. doi: 10.1136/thoraxjnl-2014-205126. [DOI] [PubMed] [Google Scholar]
- 25.Singh SJ, Puhan MA, Andrianopoulos V, et al. An official systematic review of the European Respiratory Society/American Thoracic Society: measurement properties of field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1447–1478. doi: 10.1183/09031936.00150414. [DOI] [PubMed] [Google Scholar]
- 26.Windisch W, Storre JH, Kohnlein T. Nocturnal non-invasive positive pressure ventilation for COPD. Expert Rev Respir Med. 2015;9(3):295–308. doi: 10.1586/17476348.2015.1035260. [DOI] [PubMed] [Google Scholar]
- 27.Dreher M, Storre JH, Schmoor C, Windisch W. High-intensity versus low-intensity non-invasive ventilation in patients with stable hypercapnic COPD: a randomised crossover trial. Thorax. 2010;65(4):303–308. doi: 10.1136/thx.2009.124263. [DOI] [PubMed] [Google Scholar]
- 28.Windisch W, Haenel M, Storre JH, Dreher M. High-intensity noninvasive positive pressure ventilation for stable hypercapnic COPD. Int J Med Sci. 2009;6(2):72–76. doi: 10.7150/ijms.6.72. [DOI] [PMC free article] [PubMed] [Google Scholar]