Abstract
Introduction
An estimated 2.6 million stillbirths occur worldwide each year. A standardized classification system setting out possible cause of death and contributing factors is useful to help obtain comparative data across different settings. We undertook a systematic review of stillbirth classification systems to highlight their strengths and weaknesses for practitioners and policymakers.
Material and methods
We conducted a systematic search and review of the literature to identify the classification systems used to aggregate information for stillbirth and perinatal deaths. Narrative synthesis was used to compare the range and depth of information required to apply the systems, and the different categories provided for cause of and factors contributing to stillbirth.
Results
A total of 118 documents were screened; 31 classification systems were included, of which six were designed specifically for stillbirth, 14 for perinatal death, three systems included neonatal deaths and two included infant deaths. Most (27/31) were developed in and first tested using data obtained from high‐income settings. All systems required information from clinical records. One‐third of the classification systems (11/31) included information obtained from histology or autopsy. The percentage where cause of death remained unknown ranged from 0.39% using the Nordic‐Baltic classification to 46.4% using the Keeling system.
Conclusion
Over time, classification systems have become more complex. The success of application is dependent on the availability of detailed clinical information and laboratory investigations. Systems that adopt a layered approach allow for classification of cause of death to a broad as well as to a more detailed level.
Keywords: Cause of death, classification, pregnancy outcome, stillbirth, systematic review
Abbreviations
- ICD
International Classification of Diseases
- MM
deaths during pregnancy, childbirth and the puerperium
- PM
perinatal mortality
Key Message.
Classification systems for cause of and factors contributing to stillbirth need to be applicable in settings in which the majority of stillbirths occur.
Introduction
For international comparison, the World Health Organization defines stillbirth as a baby born dead at 28 weeks of gestation or more, or with a birthweight of ≥1000 g, or a body length of ≥35 cm 1, 2. Annually, an estimated 2.6 million stillbirths occur worldwide, most of which are thought to result from preventable causes 3. About 98% of all stillbirths occur in low‐ and middle‐income countries. Apart from the immediate distress of losing a baby, stillbirth has been reported to have severe psychosocial consequences for parents, including anxiety, long‐term depression, post‐traumatic stress disorder and stigmatization 2, 4. Sadly, the risk of stillbirth is higher for women with a previous history of stillbirth compared with women who have not had a stillbirth 5, 6, 7, 8, 9, 10.
Reduction in the global burden of stillbirths is dependent on strategic interventions that, to be effective, require a clear understanding of the cause of and factors associated with stillbirth. Perinatal audit (or review) is the recommended practice for establishing cause of and factors contributing to death. It is also used to identify what went well, and what could have been done better, with regard to care provided 11.
In order to systematically and comprehensively extract relevant information from clinical records and/or verbal autopsy data to assign cause of death and contributing factors for each case of stillbirth reviewed, the use of standardized classification systems is very helpful. The use of agreed and comprehensive systems should also allow for uniform use of terminology and comparison within and between settings. It would be helpful to have an agreed classification system that can be applied across multiple settings to allow for comparability of findings.
Presently, there are a variety of classification systems that are used to assign cause of perinatal death. Most of these classification systems show poor comparability 12 and consistently report about two‐thirds of stillbirths as “unexplained” or “cause unknown” 13. Some of the systems cannot be recommended for classification of cause of death in case of stillbirth because they were not designed for this purpose, and others are considered difficult to apply and have been reported to have high inter‐observer variability 14.
In some countries with a high stillbirth rate, perinatal death audit has been introduced, but classification systems are rarely used during this process 7. This is, in part at least, because it is difficult to know which of the classification systems is best suited to the local or national setting or healthcare level and partly because of lack of knowledge and understanding of often complex classification systems. Given that diagnostic and management pathways in most low‐resource settings are different to those in high‐income countries, it is also important to understand the minimum information required to be able to apply any of the systems.
We undertook a systematic review to identify and describe existing classification systems used to identify cause of and/or conditions associated with stillbirth. We evaluated the advantages and limitations of each classification system to provide healthcare providers and policy makers with information to be able to choose which classification system would be most appropriate in their setting, maternity unit, region or country.
Material and methods
Search strategy
We developed a review protocol to guide our search and defined our inclusion and exclusion criteria.
Electronic databases (MEDLINE, CINAHL Plus, Global Health, Science Direct and Scopus) were searched for existing stillbirth or perinatal death classification systems published in English between 1950 (the period just before the first recorded classification system) and 2015 (inclusive).
The following search terms were used: (stillbirth OR “perinatal mortality”) AND classification AND (system OR framework) to identify publications on classification systems and/or publications on cause of stillbirth and perinatal death that documented the use of a classification system. We hand‐searched the references of all identified relevant publications to find additional papers or documents.
Inclusion and exclusion criteria
We defined a classification system as any method of categorizing cause of stillbirth. All published classification systems for stillbirth or perinatal death were included. We excluded systems that were designed exclusively for neonatal, infant or general mortality. Inclusion or exclusion of papers was determined after review by all authors. Disagreements were settled through consensus.
Data extraction and analysis
All identified classification systems that met the inclusion criteria were obtained in their full electronic or print versions and reviewed. One author (MA) extracted relevant information using a predesigned summary table, which was cross‐checked by the other reviewers (SBZ and NvdB). Information captured included: where and how the classification systems were first developed and used, the major categories used in the classification system, type and range of information required for application and proportion of deaths reported as unknown. Where known, the number and distribution of identified cause of stillbirths documented with the first application of the system were noted (see Table S1).
We assessed the applicability and ease of use of each system based on information requirements, proportion of unknown cause of stillbirth and overall complexity determined by exploring the structure of and terminology used in the systems.
Three criteria were used for the assessment of classification systems: (i) information requirements – Depth of clinical information required to apply the system, including any special tests required for certain diagnoses; (ii) proportion of stillbirths reported as unknown (or unclassified) by the authors of the system and (iii) complexity – number of categories and subcategories and their hierarchical relationships within each system, use of terminology in the categories and subcategories.
We categorized studies by year of publication, their scope (stillbirths only and perinatal mortality) and level of complexity (as defined above). We used narrative synthesis to report our findings.
Results
A total of 118 documents were identified and screened, out of which 31 unique classification systems were included (Figure 1).
Figure 1.
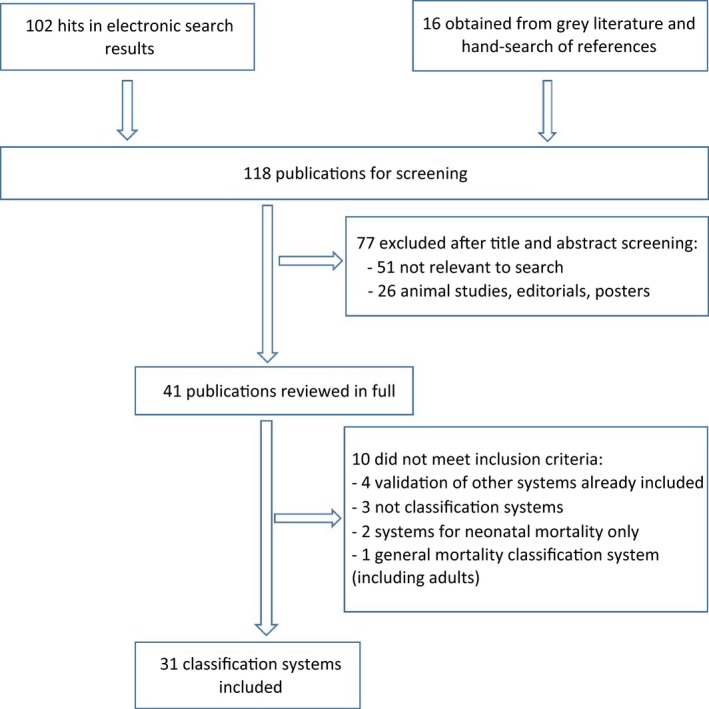
Flow chart showing process for selection of included studies. [Color figure can be viewed at wileyonlinelibrary.com].
Development of classification systems for stillbirth
The included classification systems were published between 1954 and 2016. Only six of these were designed specifically for stillbirth 13, 15, 16, 17, 18, 19. Fourteen of the classification systems were designed to include perinatal mortality, three included neonatal death, two included infant mortality and one included “late abortions” 20.
The systems were developed and first applied using data on stillbirth in a variety of settings: Europe [16], Australasia [3], Scandinavia [3], North America [4], Africa [1], mixed locations [2] and from consensus [2].
Of the 31 systems included, 17 were developed using hospital data; six systems [International Classification of Diseases (ICD)‐10, 2004; Chan et al., 2004; PSANZ‐PDC, 2009; Frøen, 2009; Reddy et al., 2009; ICD‐ (Perinatal Mortality) PM, 2015] were developed through conference or expert consensus 19, 21, 22, 23, 24, 25; five were modifications of previously developed systems (Amended Aberdeen, 1969; Extended Wigglesworth, 1986; Hey et al., 1986; Cole et al., 1986; Keeling et al., 1989) 26, 27, 28, 29, 30 and; three used data from surveys (Butler & Bonham, 1963; Cole et al., 1989; Alberman et al., 1994) 31, 32, 33.
The number of deaths included in the studies describing development of the system and/or first application varied and ranged from 239 21 to 15 251 34. Generally, the sample size of the studies was much higher in earlier studies than more recent studies.
Information required for application of classification systems
Table 1 summarizes the type of information required to be able to apply each of the classification systems. In general, the vast majority of systems require information that would need to be obtained from fairly comprehensive clinical records in order to assign the cause of death and identify factors associated with death or contributing conditions (but which are not the underlying cause of death).
Table 1.
Classification systems and the type of information required to assign cause of death and contributing factors
| Classification system | Complexity | Source and type of information required to use classification system | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Name/publication title | Authors | Year of development first publication or use | Scope | No. of main categories | No. of levels | Clinical records | Full autopsy | Histological autopsy | Other requirement(s) |
| Aberdeen classification | Baird | 1954 | Perinatal | 8 | 1 | √ | Accurate gestational age or birthweight | ||
| Classification of causes of perinatal mortality | Bound et al. | 1956 | Perinatal | 11 | 1 | √ | √ | √ | |
| British Perinatal Mortality Survey ‐ First Report | Butler and Bonham | 1963 | Perinatal | 9 | 1 | √ | √ | ||
| Amended Aberdeen | Baird and Thomson | 1969 | Perinatal | 10 | 2 | √ | √ | ||
| A clinical classification of the mechanisms of perinatal wastage | Low et al. | 1970 | Perinatal | 8 | 1 | √ | |||
| Clinical classification of perinatal deaths | Knutzen et al. | 1975 | Perinatal | 8 | 1 | √ | |||
| Perinatal death: audit and classification | Chang et al. | 1979 | Perinatal | 15 | 3 | √ | |||
| Wigglesworth | Wigglesworth | 1980 | Perinatal | 5 | 1 | √ | |||
| Causes of stillbirth: a clinicopathological study of 243 patients | Hovatta et al. | 1983 | Stillbirth | 10 | 2 | √ | √ | Serum enzymes assay; oral glucose tolerance test | |
| Classifying perinatal death: fetal and neonatal factors | Hey, Lloyd and Wigglesworth | 1986 | Perinatal | 11 | 2 | √ | √ | ||
| Extended Wigglesworth | CESDI | 2001 | √ | ||||||
| Perinatally related waste – a proposed classification of primary obstetric factors | Whitfield et al. | 1986 | Perinatal | 12 | 1 | √ | √ | ||
| Classifying perinatal death: an obstetric approach | Cole et al. | 1986 | Perinatal | 10 | 2 | √ | Rhesus compatibility test | ||
| International Collaborative Effort (ICE) | Cole et al. | 1989 | Perinatal | 8 | 1 | √ | |||
| Classification of perinatal death | Keeling et al. | 1989 | Perinatal | 5 | 1 | √ | √ | √ | Chromosomal assay |
| Classification of Primary Cause of Fetal Death | Fretts et al. | 1992 | Stillbirth | 10 | 1 | √ | √ | √ | |
| A new hierarchical classification of causes of infant deaths in England and Wales | Alberman et al. | 1994 | Perinatal | 9 | 1 | √ | |||
| Nordic‐Baltic | Langhoff‐Roos et al. | 1996 | Perinatal | 13 | 1 | √ | Accurate gestational age | ||
| A computer‐based method of cause of death classification in stillbirths and neonatal deaths | Winbo et al. | 1997 | Perinatal | 6 | 1 | √ | Computerized record system | ||
| Neonatal and Intrauterine Death Classification according to Etiology (NICE) | Winbo et al. | 1998 | Perinatal | 13 | 1 | √ | Computerized record system | ||
| Evaluation of 239 cases of perinatal death using a fundamental classification system | de Galan‐Roosen et al. | 2002 | Perinatal | 7 | 2 | √ | |||
| ICD‐10 | WHO | 2004 | √ | ||||||
| Perinatal Society of Australia and New Zealand – Perinatal Death Classification (PSANZ‐PDC) | Chan et al. | 2004 | Perinatal | 11 | 1 | √ | |||
| Relevant Condition at Death (ReCoDe) | Gardosi et al. | 2005 | Stillbirth | 9 | 1 | √ | √ | ||
| Tulip | Korteweg et al. | 2006 | Perinatal | 6 | 2 | √ | √ | √ | Chromosomal assay |
| Stockholm classification of stillbirth | Varli et al. | 2008 | Stillbirth | 17 | 2 | √ | |||
| National Institute of Child Health and Human Development (NICHHD) | Reddy et al. | 2009 | Stillbirth | 15 | 2 | √ | |||
| Causes of death and associated conditions (CODAC)/Simplified CODAC | Frøen et al. | 2009 | Perinatal | 10 | 1 | √ | |||
| Perinatal Society of Australia and New Zealand – Perinatal Death Classification (PSANZ‐PDC) – Version 2.2 | PSANZ | 2009 | Perinatal | 11 | 3 | √ | |||
| Initial Causes of Fetal Death (INCODE) | Dudley et al. | 2010 | Stillbirth | 6 | 1 | √ | √ | √ | Interview with mother/parents |
| ICD‐PM | WHO | 2016 | Perinatal | 3 | 3 | √ | |||
ICD, International Classification of Diseases; MM, deaths during pregnancy, childbirth and the puerperium; PM, perinatal mortality.
A number of systems reviewed, including ReCoDe, INCODE and TULIP 13, 17, 35, have categories that may require histological evidence to support certain diagnoses. INCODE has subcategories for congenital abnormalities for various body systems – diagnosis of which may require a post mortem. In addition, some systems may require chromosomal assays to enable a final diagnosis to be made 30, 35. In two of the systems, a specific, computerized system and program for recording patient information was used in the development of the system and such a system may also be required for the application of the system 36, 37. The new ICD‐PM 25 was developed to allow for minimal data requirement and requires fewer clinical details compared with some other recently developed classification systems.
However, some systems such as Keeling et al. (1989), Langhoff‐Roos et al. (1996) and Korteweg et al. (2006) require a lot of detail for their application 30, 35, 38.
Proportion of deaths that remain unclassified
Table 2 summarizes the proportion of deaths reported as unknown and/or unclassified for each classification system at the time of the development and first application of the system. Only classification systems that reported the proportion of unknown and/or unclassified causes of death were summarized (16 of 31). The lowest reported percentage of unknown cause of death was reported by Langhoff‐Roos et al. (1996) 38. Using the Nordic‐Baltic classification, they reported 0.39% of deaths as cause unknown. The highest reported proportion of unknown cause of death was noted with application of the system by Keeling et al. (1989), which reported 46.4% of stillbirths analyzed as cause of death unknown 30.
Table 2.
Proportion of deaths reported as unknown or unclassified
| Publication | Proportion unknown/unclassified (%) |
|---|---|
| Langhoff‐Roos et al. (1996) | <1 |
| Whitfield et al. (1986), Cole et al. (1986), Alberman (1994), Winbo et al. (1997) | <5 |
| Hovatta et al. (1983), de Galan‐Roosen et al. (2002) | 5–10 |
| Gardosi et al. (2005), Korteweg et al. (2006), Varli et al. (2008) | 11–20 |
| Chang et al. (1979), Fretts et al. (1992) | 21–30 |
| Baird et al. (1954) | 31–40 |
| Knutzen et al. (1975), Winbo et al. (1998), Keeling et al. (1989) | 41–50 |
Structural and terminological complexity
The more recently developed classification systems, such as the Stockholm classification (Varli et al. 2008), PSANZ‐PDC (2009) and NICHHD (Reddy et al. 2009) have a comprehensive provision for a wide range of categories, covering most of the possible causes of death 18, 19, 23 (Table 1). There were a few earlier systems, such as Chang et al. (1979), with a wide range of categories 39.
The category for unexplained deaths was absent in some of the systems, such as in Low et al. (1970) 40, whereas some have too many sublevels for each category (Chang et al., 1979).
Other key points
Many classification systems were developed using data from a large number, and proportion, of all recorded stillbirths in the populations studied, so ensuring that the results are representative of the population and are, therefore, likely to be more generalizable in the settings for which these systems were developed 13, 17, 20, 24, 31, 36, 39, 41, 42.
One system (Whitfield et al., 1986) was developed to be used for all “perinatally‐related wastages”, including late abortions 20. This has the advantage of presenting an opportunity to use a single system across many stages of pregnancy, although it is also complex to use and the terminology is no longer correct.
The use of highly inclusive definitions of stillbirth, such as “fetal losses from 16 completed weeks of gestation” (Tulip) 35, or inclusion of “late abortions” in the case definition 20, may make application of systems more difficult where there is a lack of information about gestational age at time of death and/or birth.
Discussion
We conducted a review of existing classification systems used to assign cause of, and factors contributing to, stillbirth. Our focus on papers published in the English language may have limited the number of papers included in this review. However, we may have been able to partly compensate for this by specifically searching for papers found in references in other papers that may otherwise have been missed through keyword searches.
Recently, some publications exploring classification of stillbirth have been published, but none focused on reviewing previous classification systems with a view to understanding how the systems have changed over the years, which could guide discussions on how best to approach classification of stillbirth. However, a recent systematic review was conducted to summarize key features of classification systems for both stillbirths and neonatal deaths, but it was limited to the 5‐year period of 2009 to 2014 43. Even though they reported an overall higher number of classification systems, only 55 classification systems included stillbirth 43, which is less than the 118 we found in our review. Another study used the Delphi method to establish a consensus on the important characteristics of ICD‐PM 44.
Although our study focused on classification systems for stillbirth only, it offers a comprehensive summary of classification systems and their characteristics. We hope the study will help to inform discussion on how best to approach the often difficult task of assigning cause of, and factors contributing to, stillbirth during perinatal death reviews. In addition, we sought to provide clarity on which classification systems could be used in a standardized manner to provide comparable data across a variety of settings. Our findings highlight that the type and range of information required to apply any of the existing systems may not be available in low‐ and middle‐income countries where the majority of stillbirths occur. This will require increased efforts to improve data collection and use as well as the strengthening of perinatal death audit processes in these settings.
“Cause of death” and “contributing factors” are different. While “cause” refers to conditions that have a clear causal relation to death, contributing factors refer to factors that are unlikely to have caused death directly but may have contributed to death 45. The new application of the International Classification of Death to deaths during pregnancy, childbirth and the puerperium (ICD‐MM) was used to clarify this relationship for maternal death and a similar approach was taken in cases of perinatal deaths 45, 46. In this review, we found that both terminologies were still used erroneously and interchangeably by many authors.
Traditionally, classification systems were developed to address the specific disease pattern and practice in a particular population. However, only Knutzen et al. (1975) was developed using data from a middle‐income country (South Africa) 34. Cause of death and associated conditions (CODAC) was developed with data from two middle‐income countries (Malaysia and South Africa) out of the seven countries included in the study 24. ICD‐PM was developed with data from a middle‐income country (South Africa) representing less than 10% of the overall data, whereas a high‐income country (UK) represented >90% of the data used to develop this system 25. All other classification systems were developed using information pertaining to stillbirth data from high‐income settings. There is likely to be a difference in distribution and range of causes of and factors contributing to stillbirth in low‐income countries compared with high‐income countries. Although a large proportion of stillbirths in low‐resource settings is associated with challenges in providing care for obstetric emergencies, maternal infections and fetal growth restriction 7, 12, stillbirths in high‐income countries are more often related to congenital abnormalities and factors such as obesity, smoking and advanced maternal age 47.
Earlier systems usually included a category for stillbirth due to isoimmunization. The absence of this category in more recent systems may be due to improvements in antenatal care, particularly in high‐income countries, where such cases are detected early and preventive measures are taken to avoid adverse outcomes.
The proportion of deaths for which a clear cause of death cannot be determined is important in any classification system. Generally, the proportion of stillbirths that remain unexplained or unknown has decreased as new classification systems were developed over time. This has been attributed mainly to improvement in the availability, range and use of diagnostic tests in countries where these classification systems were developed and used, as well as improvements in record keeping and in the amount and detail of clinical information available in cases of stillbirths. Furthermore, the change in the structure of classification systems, particularly the provision of more categories to accommodate more diagnoses, may have contributed to the reduction in the proportion of stillbirths categorized as unknown cause of death in more recent classification systems. The proportion of unexplained stillbirths also depends on the population to which a classification system is applied, as cause of death is more likely to be found in populations with generally high disease burden.
The structure and level of complexity of classification systems is potentially a limiting factor with regard to feasibility of application of the systems. In many low‐resource settings, mortality reviews are conducted by healthcare providers and managers with basic midwifery knowledge and skills 48. The success of a system in such settings will, therefore, be dependent on how easy it is to understand and apply.
The simplicity of earlier systems, such as the Aberdeen classification, made these easy to use 26, but this is often at the expense of accurate assignment of a cause of death or may provide limited or no information on contributing factors. This would not support in‐depth review and may not optimally allow healthcare providers to identify preventable factors or cause of death. Systems with less technical, simpler terminology, such as the Nordic‐Baltic 38 and ReCoDe 13 classifications, are easier to apply and more likely to be used consistently across settings, resulting in lower inter‐observer variability.
Systems requiring a lot of detail 30, 35, 38 may in theory have the advantage of being more accurate, but the feasibility of applying them in low‐resource settings, where the required level of detail is rarely available, may be a major limitation with regard to recommendation for more global use.
The range of causes of stillbirth that are recognized and can be assigned has expanded over the years. More recently proposed systems tend to be more specific, with many more potential causes of stillbirth included. However, this has also led to the introduction of more subcategories, making classification systems more complex, potentially increasing inter‐observer variability. The application of such systems may be particularly difficult in low‐ and middle‐income countries where non‐specialist healthcare providers provide the majority of maternal and newborn health care 48, 49. If these more complex systems are to be applied this will require healthcare providers to be trained to understand how to apply such systems. In addition, patient records will need to be improved to ensure information required to apply classification systems is documented and available at time of review.
Classification systems without a category for unexplained stillbirth present a challenge as it must be assumed that there will always be a proportion of deaths where cause of death cannot be ascertained and it is not clear how such cases could be included in aggregated information on stillbirths (i.e. those cases would presumably be unaccounted for or treated as “missing data”) 40. Having too many subcategories as in Chang et al. (1979) makes a system cumbersome to use and subject to higher inter‐observer variability 39.
Different terms have been used to describe the group of stillbirths whose cause could not be determined, including “unknown”, “unclassified” and “unexplained”. Most classification systems have not defined these terms. For the few that have, there may be slight differences in meaning. However, generally, the terms are used to represent categories in which cause of death could not be determined either due to lack of sufficient information or simply because the cause cannot be determined at the current level of diagnostic ability. Sometimes the term “unclassified” is used to describe a group of stillbirths with a known cause that does not belong to any category in the classification used.
Although a broader, comprehensive system including all or most of the possible causes of death may be expected to result in a smaller proportion of deaths that are classified as unexplained or unknown, in practice, this is not always so. For example, despite the many categories and subcategories of the system by Chang et al. 39, 26.3% of stillbirths remained as unexplained. Similarly, the NICE classification has detailed provisions for almost all possible causes of perinatal death imaginable, but has reported up to 43.6% of perinatal deaths as unexplained 37. We suggest that the availability of detailed clinical information and records is most likely the most important factor determining ability to assign a clear cause of death and apply any classification system, and that a broad and complex system in itself is insufficient.
About a third (11/31) of classification systems include information that can only be obtained through histological examination of tissue and/or autopsy. Although such information is not a requirement per se, the availability of this information provides more clarity on cause of death and contributing factors. This is more often included in more recent systems that tend to move towards more accurate diagnoses involving histological and chromosomal examinations. However, autopsies are rarely conducted in low‐ and middle‐income countries and pathology services are not usually available. For these settings, there should be a strong focus on obtaining as much clinical information as possible to help identify cause of death related to obstetric and maternal complications. Since perinatal (including stillbirth) audits are conducted to identify potentially avoidable priority areas for intervention and improvement in quality of care 20, it should be possible to at least identify factors contributing to, or associated with, stillbirth, even if a clear underlying cause of death cannot be assigned with certainty.
Recently developed systems rely on very specific patient details and laboratory investigations to enable increasingly accurate diagnoses to be made. This means that, in addition to ensuring that detailed case notes are kept and are available and used for review, there is a need to improve healthcare providers’ knowledge and understanding regarding causal pathways and aetiology of stillbirth. Information obtained via perinatal death or stillbirth review should also inform the care pathway for women and their partners who have had a stillbirth. This should include debriefing, support services (where available) and counseling for future pregnancies. Such support is still not available to most women who have had a stillbirth.
Conclusion
The current stillbirth classification systems were designed to suit specific populations, disease patterns and needs, and this, at least in part, explains the variation in approach. There is currently no single agreed system that will suit every purpose and setting. If a classification system is to be applied successfully in low‐resource settings during stillbirth or perinatal death audit or review, it should strike a balance between the level of detail required, proportion of deaths for which a cause of death can be assigned and ease of use.
A layered classification system that allows classification to a broad as well as more detailed level in a systematic manner is probably the most useful as it will allow for comparison within and between settings at least with regard to the main types and causes of stillbirth.
Funding
This study was conducted under the ‘Making it Happen’ Program funded by DFID/UKAid, Contract number 202945‐101.
Supporting information
Table S1. Summary table of included studies.
Acknowledgments
We would like to thank Caroline Hercod for her help in editing the manuscript.
Aminu M, Bar‐Zeev S, van den Broek N. Cause of and factors associated with stillbirth: a systematic review of classification systems. Acta Obstet Gynecol Scand 2017; 96:519–528.
Conflict of interest
All authors have stated explicitly that there are no conflicts of interest in connection with this article.
References
- 1. World Health Organization . Stillbirths. Geneva: WHO, 2015. Available online at: http://www.who.int/maternal_child_adolescent/epidemiology/stillbirth/en/ (accessed January 03, 2016). [Google Scholar]
- 2. Frøen JF, Cacciatore J, McClure EM, Kuti O, Jokhio AH, Islam M, et al. Stillbirths: why they matter. Lancet. 2011;377:1353–66. [DOI] [PubMed] [Google Scholar]
- 3. Lawn JE, Blencowe H, Waiswa P, Amouzou A, Mathers C, Hogan D, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. Lancet. 2016;387:587–603. [DOI] [PubMed] [Google Scholar]
- 4. Heazell AEP, Siassakos D, Blencowe H, Burden C, Bhutta ZA, Cacciatore J, et al. Stillbirths: economic and psychosocial consequences. Lancet. 2016;387:604–16. [DOI] [PubMed] [Google Scholar]
- 5. Kupka R, Kassaye T, Saathoff E, Hertzmark E, Msamanga G, Fawzi W. Predictors of stillbirth among HIV‐infected Tanzanian women. Acta Obstet Gynecol Scand. 2009;88:584–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ouyang F, Zhang J, Betrán AP, Yang Z, Souza JP, Merialdi M. Recurrence of adverse perinatal outcomes in developing countries. Bull World Health Organ. 2013;91:357–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Aminu M, Unkels R, Mdegela M, Utz B, Adaji S, van den Broek N. Causes of and factors associated with stillbirth in low‐ and middle‐income countries: a systematic literature review. BJOG. 2014;121:141–53. [DOI] [PubMed] [Google Scholar]
- 8. Stringer EM, Vwalika B, Killam WP, Giganti MJ, Mbewe R, Chi BH, et al. Determinants of stillbirth in Zambia. Obstet Gynecol. 2011;117:1151–9. [DOI] [PubMed] [Google Scholar]
- 9. Watson‐Jones D, Weiss HA, Changalucha JM, Todd J, Gumodoka B, Bulmer J, et al. Adverse birth outcomes in United Republic of Tanzania‐impact and prevention of maternal risk factors. Bull World Health Organ. 2007;85:9–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yatich NJ, Funkhouser E, Ehiri JE, Agbenyega T, Stiles JK, Rayner JC, et al. Malaria, intestinal helminths and other risk factors for stillbirth in Ghana. Infect Dis Obstet Gynecol. 2010;2010:350763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. World Health Organization, Department of Reproductive Health and Research . Beyond the numbers: reviewing maternal deaths and complications to make pregnancy safer. Geneva: World Health Organization, 2004. Available online at: http://www.who.int/maternal_child_adolescent/documents/9241591838/en/ (accessed December 03, 2015). [Google Scholar]
- 12. Lawn JE, Blencowe H, Pattinson R, Cousens S, Kumar R, Ibiebele I, et al. Stillbirths: Where? When? Why? How to make the data count? Lancet. 2011;377:1448–63. [DOI] [PubMed] [Google Scholar]
- 13. Gardosi J, Kady SM, McGeowr P, Francis A, Tonks A. Classification of stillbirth by relevant condition at death (ReCoDe): population based cohort study. BMJ. 2005;331:1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Flenady V, Frøen JF, Pinar H, Torabi R, Saastad E, Guyon G, et al. An evaluation of classification systems for stillbirth. BMC Pregnancy Childbirth. 2009;9:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hovatta O, Lipasti A, Rapola J, Karjalainen O. Causes of stillbirth: a clinicopathological study of 243 patients. Br J Obstet Gynaecol. 1983;90:691–6. [DOI] [PubMed] [Google Scholar]
- 16. Fretts RC, Boyd ME, Usher RH, Usher HA. The changing pattern of fetal death, 1961–1988. Obstet Gynecol. 1992;79:35–9. [PubMed] [Google Scholar]
- 17. Dudley DJ, Goldenberg R, Conway D, Silver RM, Saade GR, Varner MW, et al. A new system for determining the causes of stillbirth. Obstet Gynecol. 2010;116:254–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Varli IHN, Petersson K, Bottinga R, Bremme K, Hofsjo A, Holm M, et al. The Stockholm classification of stillbirth. Acta Obstet Gynecol Scand. 2008;87:1202–12. [DOI] [PubMed] [Google Scholar]
- 19. Reddy UM, Goldenberg R, Silver R, Smith GCS, Pauli RM, Wapner RJ, et al. Stillbirth classification – developing an international consensus for research. Obstet Gynecol. 2009;114:901–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Whitfield CR, Smith NC, Cockburn F, Gibson AAM. Perinatally related wastage – proposed classification of primary obstetric factors. Br J Obstet Gynaecol. 1986;93:694–703. [PubMed] [Google Scholar]
- 21. World Health Organization . ICD‐10 International statistical classification of diseases and related health problems. Geneva: World Health Organization, 2004. [Google Scholar]
- 22. Chan A, King JF, Flenady V, Haslam RH, Tudehope DI. Review Article: classification of perinatal deaths: development of the Australian and New Zealand classifications. J Paediatr Child Health. 2004;40:340–7. [DOI] [PubMed] [Google Scholar]
- 23. Perinatal Society of Australia and New Zealand (PSANZ) . Perinatal Death Classification (PSANZ‐PDC) Version 2.2 2009. Available online at: http://www.stillbirthalliance.org.au/doc/Section_7_Version_2.2_April_2009.pdf (accessed August 30, 2013).
- 24. Frøen JF, Pinar H, Flenady V, Bahrin S, Charles A, Chauke L, et al. Causes of death and associated conditions (Codac) – a utilitarian approach to the classification of perinatal deaths. BMC Pregnancy Childbirth. 2009;9:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. WHO . International Classification of Diseases – Perinatal Mortality (ICD‐PM). 2016. Available online at: http://www.who.int/reproductivehealth/projects/02-ICD-PM.pdf (accessed August 16, 2016).
- 26. Baird D, Walker J, Thomson AM. The causes and prevention of stillbirths and first week deaths. III. A classification of deaths by clinical cause; the effect of age, parity and length of gestation on death rates by cause. Br Med J. 1954;61:433–48. [DOI] [PubMed] [Google Scholar]
- 27. CESDI – Confidential Enquiry into Stillbirths and Deaths in Infancy: 8th Annual Report. London: Maternal and Child Health Research Consortium, 2001. [Google Scholar]
- 28. Hey EN, Lloyd DJ, Wigglesworth JS. Classifying perinatal death: fetal and neonatal factors. Br J Obstet Gynaecol. 1986;93:1213–23. [DOI] [PubMed] [Google Scholar]
- 29. Cole SK, Hey EN, Thomson AM. Classifying perinatal death: an obstetric approach. Br J Obstet Gynaecol. 1986;93:1204–12. [DOI] [PubMed] [Google Scholar]
- 30. Keeling JW, MacGillivray I, Golding J, Wigglesworth J, Berry J, Dunn PM. Classification of perinatal death. Arch Dis Child. 1989;64:1345–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Butler NR, Bonham DG, British Perinatal Mortality Survey . Perinatal mortality; the first report of the 1958 British Perinatal Mortality Survey. Edinburgh: Livingstone, 1963. [Google Scholar]
- 32. Alberman E, Botting B, Blatchley N, Twidell A. A new hierarchical classification of causes of infant deaths in England and Wales. Arch Dis Child. 1994;70:403–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cole SK. Accuracy of death certificates in neonatal deaths. Community Med. 1989;11:1–8. [DOI] [PubMed] [Google Scholar]
- 34. Knutzen VK, Baillie P, Malan AF. Clinical classification of perinatal deaths. S Afr Med J. 1975;49:1434–6. [PubMed] [Google Scholar]
- 35. Korteweg FJ, Gordijn SJ, Timmer A, Erwich J, Bergman KA, Bouman K, et al. The Tulip classification of perinatal mortality: introduction and multidisciplinary inter‐rater agreement. BJOG. 2006;113:393–401. [DOI] [PubMed] [Google Scholar]
- 36. Winbo IG, Serenius FH, Dahlquist GG, Källen BA. A computer‐based method for cause of death classification in stillbirths and neonatal deaths. Int J Epidemiol. 1997;26:1298–306. [DOI] [PubMed] [Google Scholar]
- 37. Winbo IG, Serenius FH, Dahlquist GG, Källén BA. NICE, a new cause of death classification for stillbirths and neonatal deaths. Neonatal and Intrauterine Death Classification according to Etiology. Int J Epidemiol. 1998;27:499–504. [DOI] [PubMed] [Google Scholar]
- 38. Langhoff‐Roos J, Borch‐Christensen H, Larsen S, Lindberg B, Wennergren M. Potentially avoidable perinatal deaths in Denmark and Sweden 1991. Acta Obstet Gynecol Scand. 1996;75:820–5. [DOI] [PubMed] [Google Scholar]
- 39. Chang A, Keeping JD, Morrison J, Esler EJ. Perinatal death: audit and classification. Aust N Z J Obstet Gynaecol. 1979;19:207–11. [DOI] [PubMed] [Google Scholar]
- 40. Low JA, Boston RW, Cervenko FW. A clinical classification of the mechanisms of perinatal wastage. Can Med Assoc J. 1970;102:365–8. [PMC free article] [PubMed] [Google Scholar]
- 41. Bound JP, Butler NR, Spector WG. Classification and causes of perinatal mortality. BMJ. 1956;2:1191–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Bound JP, Butler NR, Spector WG. Classification and causes of perinatal mortality II. BMJ. 1956;2:1260–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Leisher SH, Teoh Z, Reinebrant H, Allanson E, Blencowe H, Erwich JJ, et al. Seeking order amidst chaos: a systematic review of classification systems for causes of stillbirth and neonatal death, 2009–2014. BMC Pregnancy Childbirth. 2016;16:295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wojcieszek AM, Reinebrant HE, Leisher SH, Allanson E, Coory M, Erwich JJ, et al. Characteristics of a global classification system for perinatal deaths: a Delphi consensus study. BMC Pregnancy Childbirth. 2016;16:223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. McClure EM, Saleem S, Pasha O, Goldenberg RL. Stillbirth in developing countries: a review of causes, risk factors and prevention strategies. J Matern Fetal Neonatal Med. 2009;22:183–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. World Health Organization . The WHO application of ICD‐10 to deaths during pregnancy, childbirth and the puerperium: ICD‐MM. Geneva: World Health Organization, 2012. Available online at: http://www.who.int/reproductivehealth/publications/monitoring/9789241548458/en/ (accessed September 02, 2015). [Google Scholar]
- 47. Flenady V, Koopmans L, Middleton P, Smith GC, Duke W, Erwich JJ, et al. Stillbirths: the way forward in high‐income countries. Lancet. 2011;377:1703–17. [DOI] [PubMed] [Google Scholar]
- 48. Ameh CA, Adegoke A, Pattinson R, van den Broek N. Using the new ICD‐MM classification system for attribution of cause of maternal death – a pilot study. BJOG. 2014;121:32–40. [DOI] [PubMed] [Google Scholar]
- 49. Owolabi H, Ameh C, Bar‐Zeev S, Adaji S, Kachale F, van den Broek N. Establishing cause of maternal death in Malawi via facility‐based review and application of the ICD‐MM classification. BJOG. 2014;121:95–101. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Summary table of included studies.


