Abstract
Background
Although regional socioeconomic (SE) factors have been associated with worse health outcomes, prior studies have not addressed important confounders or work disability.
Methods
A national sample of 59 360 workers’ compensation (WC) cases to evaluate impact of regional SE factors on medical costs and length of disability (LOD) in occupational low back pain (LBP).
Results
Lower neighborhood median household incomes (MHI) and higher state unemployment rates were associated with longer LOD. Medical costs were lower in states with more workers receiving Social Security Disability, and in areas with lower MHI, but this varied in magnitude and direction among neighborhoods. Medical costs were higher in more urban, more racially diverse, and lower education neighborhoods.
Conclusions
Regional SE disparities in medical costs and LOD occur even when health insurance, health care availability, and indemnity benefits are similar. Results suggest opportunities to improve care and disability outcomes through targeted health care and disability interventions.
Keywords: disability duration, medical costs, occupational low back pain, socioeconomic factors, workers’ compensation
1. INTRODUCTION
In recent years, there has been increasing public health awareness of regional disparities in health outcomes. Using mortality data between 1985 and 2010 from the National Center for Health Statistics, one recent study found that zip code of residence is predictive of mortality or length of life.1 One possible explanation is that worse health outcomes for lower socioeconomic (SE) status neighborhoods are due to poor health care access or lack of health insurance.2, 3, 4 However, studies in different economically developed countries observed significant associations between neighborhood SE status and health outcomes, such as mortality and poor health status, despite universal health care coverage in those countries.5, 6, 7, 8, 9
There have been several other studies in the United States which found a link between neighborhood‐level SE disadvantages and morbidity and mortality independent of individual SE status.10, 11, 12 None of these studies, however, accounted for level of insurance coverage or cost‐sharing amount (eg, deductible amounts), which are important predictors of health care utilization and adverse health outcomes.13 Prior research on adverse health outcomes and associated SE factors has been confounded by unmeasured differences in health insurance coverage, which can be associated with individual and local SE factors.14, 15 For example, the RAND Health Insurance Experiment demonstrated that an increased co‐insurance amount was associated with a sizeable reduction in health care utilization reflected in physician visits, outpatient visits, prescription drug spending, dental care, and preventative health care, especially in low‐income patients.14
In this study, we were able to look at differences in outcomes associated with occupational low back pain (LBP) by assessing the benefits provided by Workers Compensation (WC) for one large insurer. WC benefits have the advantage of total and uniform coverage for all health care services for accepted claims for work‐related conditions, without cost‐sharing. Thus, we were able to eliminate the influence of the type of health insurance coverage. WC also compensates for lost work time, providing 60‐70% of lost wages depending on specific state laws, another outcome to evaluate in relation to SE factors.
Occupational LBP is an important public health problem which accounts for one third of all occupational musculoskeletal injuries and illnesses resulting in work disability. In the United States, the direct costs associated with work‐related overexertion events (dominated by LBP) in 2013 were estimated to be $15 billion.16 Uncomplicated LBP is a common condition in working‐age populations where intensive interventions are rarely required and treatment guidelines are quite clear about the recommended course of care and expected recovery.17 However, the vast majority of working‐age LBP patients in the U.S. receive too much testing and treatment for their LBP as compared to guideline recommendations.18, 19 The objective of this study was to determine if SE characteristics of claimants’ geographic context were associated with WC benefits including intensity of medical care (as reflected by medical expenses) and length of time absent from work for acute uncomplicated LBP, after controlling for individual and state characteristics.
2. METHODS
2.1. Study design and population
This study used a large WC administrative database from a single private insurer that represents about 10% of the U.S. private WC market.20 The database has complete capture of individual medical and indemnity services provided to injured workers, and has been used for a number of national health services research studies.21, 22, 23 The distribution of occupational injuries/disorders and overall medical costs is comparable to national occupational injury datasets, such as the Bureau of Labor Statistics (BLS) and the National Council on Compensation Insurance.24 We selected cases that were injured over a period of 7 years 2002‐2008 (inclusive) and were compensated for at least 1 day away from work. The study was approved by the New England Institutional Review Board.
To identify cases treated primarily for uncomplicated LBP, diagnoses associated with bills for medical services received in the first 15 days of seeking medical treatment were evaluated using diagnostic codes from the International Classification of Diseases, Ninth Edition (ICD‐9) referring to LBP or non‐specific back pain (Supplemental Table S1). The case identification and selection process utilized the primary (most common) diagnosis during this initial period of care, as well as the presence of any specific diagnoses inconsistent with uncomplicated LBP (indicating multiple trauma, severe injuries, and non‐injury diagnoses such as infection, cancer, and autoimmune disease) for exclusions. The process and list of diagnosis described in detail elsewhere.25
2.2. Measures
2.2.1. Outcome variables
The outcome variables were total medical costs summarized from paid medical bills and length of time absent from work or length of disability (LOD). Medical costs were a surrogate measure for the intensity of medical care. As the data included medical costs during the years 2002‐2008, inclusive, we accounted for average price change for medical care by adjusting the medical costs to 2008 dollars using the medical care component of the Consumer Price Index.26 Medical costs (pricing) for certain medical services may vary according to presence of state WC medical fee schedules, medical provider type, or area, and as such were controlled for in the model.27 We censored the data at 1 year from LBP onset since most cases (93%) return to work within a year, and we wanted to avoid the impact of highly variable state polices that affect closure of long‐term claims with lump sum settlements for work disability that often occur after 1 year.28 LOD, calculated as the total number of lost work days represented by disability payments, was obtained using data on sequential payments for lost wage replacement (temporary total or temporary partial lost days) where each payment compensates a claimant for a defined period of time.
2.2.2. Independent individual‐level variables
Individual‐level variables previously associated with medical costs and LOD (described in Table 1) were included.25
Table 1.
Cohort characteristics according to individual, neighborhood, and state characteristics (2002‐2008, inclusive)
| Variable | Number | Percentage | Grand mean (minimum, maximum) | SD a |
|---|---|---|---|---|
| Gender | ||||
| Female | 18 352 | 30.9 | ||
| Male | 41 008 | 69.1 | ||
| Age (years) | 39.4 (18, 65) | 10.8 | ||
| Tenure (years) | 5.8 (0, 47) | 7.7 | ||
| Average weekly wage ($) | 403.0 (1, 1311) | 187.5 | ||
| Injury severity | ||||
| Less severe | 47 805 | 80.5 | ||
| More severe | 11 555 | 19.5 | ||
| Early opioid prescribing (MEA b per 100 mg) | ||||
| No | 43 013 | 72.5 | 3.9 (0, 29.4) | 3.8 |
| Yes | 16 347 | 27.5 | ||
| Early lumbar MRI c scan | ||||
| No | 41 805 | 70.4 | ||
| Yes | 17 555 | 29.6 | ||
| Lumbar spine surgery | ||||
| No | 53 869 | 90.7 | ||
| Yes | 5491 | 9.3 | ||
| Industry type | ||||
| Mining | 1071 | 1.8 | ||
| Construction | 2087 | 3.5 | ||
| Transportation, communications, electric, gas, and sanitary services | 16 305 | 27.5 | ||
| Agriculture, forestry, and fishing | 588 | 1.0 | ||
| Manufacturing | 10 887 | 18.3 | ||
| Wholesale trade | 4515 | 7.6 | ||
| Retail trade | 6626 | 11.2 | ||
| Services | 14 782 | 24.9 | ||
| Public administration | 1990 | 3.4 | ||
| Finance, insurance, and real estate | 509 | 0.9 | ||
| Litigation status | ||||
| No | 40 178 | 67.7 | ||
| Yes | 19 182 | 32.3 | ||
| Median household income (10 000 $) | 5.3 (0.6, 25.0) | 2.1 | ||
| Rural population (%) | 21.2 (0, 100) | 35.8 | ||
| White population (%) | 73.7 (0, 100) | 25.4 | ||
| Educational attainment < some college (%) | 48.7 (0, 100) | 16.1 | ||
| Wage replacement rate (%) | 68 (60, 80) | 3 | ||
| Waiting period (days) | 5.3 (3, 7) | 1.9 | ||
| Retroactive period (days) | 15.7 (0, 42) | 7.0 | ||
| State medical fee schedule | ||||
| No | 10 498 | 17.7 | ||
| Yes | 48 862 | 82.3 | ||
| Initial treating provider choice | ||||
| Allowed | 22 516 | 37.9 | ||
| Not allowed | 36 844 | 62.1 | ||
| Treating provider change | ||||
| Allowed | 8282 | 14.0 | ||
| Allowed once | 14 241 | 24.0 | ||
| Not Allowed | 36 837 | 62.1 | ||
| Annual population below 100% poverty (%) | 12.3 (5.4, 22.6) | 2.7 | ||
| Annual unemployment rate | 5.3 (2.5, 8.3) | 1.0 | ||
| Annual Gini coefficient | 45.4 (38.0, 54.0) | 2.2 | ||
| Annual rate of disabled workers receiving SSDI d | 3.4 (1.7, 7.8) | 0.9 |
Standard deviation.
Morphine equivalent amount.
Magnetic resonance imaging.
Social security disability insurance.
2.2.3. Independent neighborhood SE variables
U.S. Census tracts are defined as small geographic areas that have 2500‐8000 residents and are relatively homogeneous regarding population SE characteristics.29 Residential addresses of cases were geocoded using ArcGIS software program30 and were linked to information corresponding to later specified census tract SE variables based on unique census tract numbers. The following SE status components,2 measured at census‐tract level (which we will refer to as “neighborhood”), and previously associated with health outcomes31, 32, 33, 34, 35, 36 were included: percentage of population who indicated their race as white; median household income (MHI) as inflation adjusted dollars; percentage of population classified as rural; and percentage of population aged 25 years and over without some college education (Table 1).
2.2.4. Independent state‐level variables
The state‐level variables previously associated with health outcomes were: (i) annual state poverty rate for each year 2002‐2008, measured as percentage of state population with income below 100% poverty; (ii) household income inequality (Gini coefficient), a ratio ranging between 0 (complete income equality) and 1 (complete income inequality)37, 38; (iii) unemployment rate39, 40; and (iv) the rate of disabled workers receiving Social Security Disability Insurance (SSDI). We included state WC policies on wage replacement and medical benefits (2002‐2008, see Table 1) known to impact medical cost and LOD.25 Sources of data about neighborhood‐level and state‐level variables are presented in Table 2.
Table 2.
Sources of neighborhood and state socioeconomic characteristics data
| Variable | Level | Source | Link |
|---|---|---|---|
| Percentage of population classified as rural in 2010 census | Census tract | U.S. census through NHGIS | https://www.nhgis.org |
| Percentage of population who indicated their race as white 2006‐2010 | Census tract | ACS through NHGIS | https://www.nhgis.org |
| Median household income 2006‐2010 | Census tract | ACS through NHGIS | https://www.nhgis.org |
| Percentage of persons (aged ≥25 years) with educational attainment less than some college 2006‐2010 | Census tract | ACS through NHGIS | https://www.nhgis.org |
| Annual household income inequality (Gini coefficient) 2002‐2008 | State | U.S. census | http://factfinder2.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh = t#none |
| Annual rate of unemployment 2002‐2008 | State | U.S. BLS | http://www.bls.gov/lau/#data |
| Annual rate of disabled workers receiving SSDI 2002‐2008 | State | U.S. SSA | http://www.ssa.gov/policy/docs/statcomps/di_asr/2008/index.html |
| Percentage of population below 100% poverty 2002‐2008 | State | U.S. census | http://www.census.gov/hhes/www/poverty/data/incpovhlth/index.html |
ACS, American Community Survey (published every 5 years during study period); BLS, U.S. Bureau of Labor Statistics; NHGIS, The National Historical Geographic Information System, University of Minnesota; SSA, Social Security Administration; SSDI, Social Security Disability Insurance.
2.3. Statistical analysis
Descriptive statistics for LBP cases were calculated for individual level, related neighborhood‐level and state‐level SE variables. Because of the hierarchical structure of the data (LBP cases [level‐1] nested within states [level‐2]), multivariable multilevel regression was conducted using the PROC MIXED procedure in Statistical Analysis System (SAS) 9.2.41 Neighborhood‐level variables were treated as individual‐level variables because 96% of census tracts (31 836/33 142) had fewer than five cases per tract (average 1.8 cases per tract). This small cluster size implies that a multilevel analysis would have less efficient estimate of variance parameters, and that these variables can be evaluated at an individual level.42
The analysis was performed in three modeling steps for each outcome. The total variance of the outcome variable was partitioned in between‐state variability and within‐state variability. Model 1, the unconditional model, provides the average values of the outcome variables and whether they vary significantly between states (measured using the intraclass correlation (ICC) as the proportion of between‐state variance over the total variance). In model 2, state‐level variables were added and each outcome variable was modeled as a linear function of state‐level variables, each effect or association was represented by a regression coefficient, which quantified variation in the outcome variable as a function of the variation in each independent state‐level variable. Model 3 incorporated variables from model 2 and individual‐level variables, first as fixed effects and then as random effects, to examine if effects of neighborhood‐level variables on the outcome variables vary significantly between states. To determine the proportional reduction in ICC after including state‐level variables while controlling for individual‐level variables, 1 minus (between‐state variance in model 3/between‐state variance model 1) was computed.43 The resulting percentage is the amount of between‐state variability in the outcome variable attributed to each state‐level variable. All continuous individual‐level and state‐level variables were centered at the grand mean by subtracting the sample grand mean for each continuous variable. The distributions of the outcome variables were positively skewed and, thus, were transformed using the natural logarithm and log‐linear models.
3. RESULTS
The cohort included 59 360 LBP cases residing in 33 142 neighborhoods from 49 states. The mean medical cost per case was $8296, with a median of $3786. The mean LOD per case (in the first 12 months) was 98 days, with a median of 42 days. Supplemental Table S2 presents the distribution of LBP cases by state with summary statistics for medical costs and LOD. The characteristics for the cohort are shown in Table 1. About two thirds of cases were male (69.1%), with an average age and tenure of 39.4 and 5.8 years, respectively. This is a representative cohort of LBP with respect to distributions of demographic variables of other occupational LBP studies.44, 45, 46
3.1. Principal findings
Parameter estimates from the three multilevel regression models examining the associations of medical costs and LOD that individual‐level variables, including neighborhood‐level, and state‐level variables are presented in Table 3. The unconditional models (models 1, no predictors) showed significant variability between states in mean medical costs and LOD. For medical costs, the ICC indicated that 5% of the total variability in both mean medical costs and mean LOD can be explained by state‐level factors. We note here the numerical magnitude of 5% of variation in the state outcome variables (represents a mean differential medical cost of $1211‐$4514 and a mean differential range of 19‐69 disability days). In the final models (models 3, Table 3), included state‐level (WC policy and SE) variables accounted for 26% and 43% reduction in between‐state variability in medical costs and LOD, respectively. Including only significant state‐level SE variables (unemployment rate and rate of disabled workers receiving SSDI) as a group in model 3 were associated with 7% and 28% reduction in between‐state variability in medical costs and LOD, respectively.
Table 3.
Parameter estimates from the three multilevel regression models examining associations of medical expenses and length of disability with neighborhood and state socioeconomic characteristics
| Medical expenses | Length of disability | |||||
|---|---|---|---|---|---|---|
| Fixed parameter estimates | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 |
| Intercept | 8.288*** | 8.373*** | 7.659*** | 3.835*** | 3.848*** | 3.252*** |
| Neighborhood‐level variables | ||||||
| Median household income (10 000 $) | 0.025*** (RS e < 0.001*) | −0.006** (RS < 0.001) | ||||
| Rural population (%) | −0.001*** (RS < 0.001) | <0.001 (RS < 0.001) | ||||
| White population (%) | −0.001*** (RS < 0.001) | <−0.001 (RS < 0.001) | ||||
| Educational attainment (% < some college) | 0.003*** (RS < 0.001) | <0.001 (RS < 0.001) | ||||
| State‐level variables | ||||||
| Population below 100% poverty (%) | −0.004 | −0.006 | −0.002 | −0.005 | ||
| Unemployment rate | 0.045*** | 0.038*** | 0.018* | 0.016** | ||
| Gini coefficient (%) | 0.002 | −0.007 | 0.005 | −0.001 | ||
| Disabled workers receiving SSDI a (%) | −0.092*** | −0.130*** | 0.012 | −0.012 | ||
| Variance components | ||||||
| Within‐state variability | 1.823*** | 1.819*** | 0.965*** | 1.393*** | 1.390*** | 0.899*** |
| Between‐state variability | 0.087*** | 0.092*** | 0.064*** | 0.072*** | 0.054*** | 0.041*** |
| ICC b | 5% | 5% | ||||
| Proportional reduction in between‐state variability in outcome measure | 26% | 43% | ||||
| Model fit statistic | ||||||
| −2LL c | 204 200 | 204 109*** | 167 140*** | 188 306 | 188 208*** | 162 865*** |
| BIC d | 204 208 | 204 116*** | 167 178*** | 188 310 | 188 215*** | 162 904*** |
Social Security Disability Insurance.
Intra‐class Correlation (percentage of total variability in medical expenses or work disability length that is explained by between‐state variability).
−2 log likelihood ratio.
Bayesian Information Criterion; *P < 0.05; **P < 0.01; ***P < 0.001. Parameter estimates in model 2 are also adjusted for state Workers’ Compensation policy variables (wage replacement rate, waiting period, retroactive period, medical fee schedule, treating provider choice, and treating provider change). Parameter estimates in model 3 are adjusted for age, gender, tenure, average weekly wage, industry type, injury severity, early opioid prescribing, early magnetic resonance imaging prescribing, lumbar spine surgery, and claim litigation status.
Random slope (examine if the relationship between each neighborhood‐level variable and the outcome measure vary significantly between states).
3.2. Associations of SE factors with LOD and medical costs
As shown in Table 4, after adjusting for all statistically significant individual‐level and state‐level variables, state unemployment rate and neighborhood MHI were the only two neighborhood SE variables significantly associated with differences in LOD. Each 1% increase in the state unemployment rate was associated with an average of 0.4 day increase (95% CI 0.1, 0.7) in LOD. Figure 1 shows the average state unemployment rate in the U.S. (2002‐2008). Figure 2 shows the adjusted association between state unemployment rate and LOD. Overall, a decrease in neighborhood MHI by $10 000 was also associated with an average of 0.2 day increase (95% CI 0.1, 0.3) in LOD.
Table 4.
Adjusted* associations of neighborhood and state socioeconomic characteristics with medical expenses and length of disability estimated by multivariable multilevel regression (model no.3)
| Medical expenses ($) | Length of disability (days) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Parameter estimate of association | S.E. a | Difference in the geometric mean of medical expenses | 95% CI b | P‐value | Parameter estimate of association | S.E. a | Difference in the geometric mean of WD length c | 95% CI b | P‐value |
| Intercept | 7.633 | 0.071 | 2065 | 1789, 2384 | <0.001 | 3.196 | 0.067 | 24.4 | 21.4, 28.0 | <0.001 |
| Neighborhood‐level variables | ||||||||||
| Median household income (10 000 $) | 0.025 | 0.003 | 48 | 33, 63 | <0.001 | −0.006 | 0.002 | −0.2 | −0.3, −0.1 | <0.001 |
| Rural population (%) | −0.001 | <0.001 | −2 | −2, −1 | <0.001 | <0.001 | <0.001 | 0.0 | 0.0,0.0 | 0.060 |
| White population (%) | −0.001 | <0.001 | −3 | −3, −2 | <0.001 | −<0.001 | <0.001 | 0.0 | 0.0,0.0 | 0.073 |
| Educational attainment (% < some college) | 0.002 | <0.001 | 5 | 3, 6 | <0.001 | <0.001 | <0.001 | 0.0 | 0.0,0.0 | 0.458 |
| State‐level variables | ||||||||||
| Population below 100% poverty (%) | −0.006 | 0.005 | −14 | −34, 7 | 0.185 | −0.005 | 0.005 | −0.1 | −0.4, 0.1 | 0.266 |
| Unemployment rate | 0.036 | 0.007 | 75 | 48, 104 | <.001 | 0.015 | 0.006 | 0.4 | 0.1, 0.7 | 0.011 |
| Gini coefficient (%) | −0.007 | 0.008 | −14 | −45, 17 | 0.363 | −0.001 | 0.007 | 0.0 | −0.4, 0.3 | 0.836 |
| Disabled workers receiving SSDI d (%) | −0.122 | 0.019 | −237 | −303, −168 | <0.001 | −0.012 | 0.017 | −0.3 | −1.1, 0.6 | 0.503 |
Standard Error of parameter estimate of association.
Confidence intervals.
Work Disability.
Social Security Disability Insurance.
*Parameter estimates are also adjusted for age, gender, tenure, average weekly wage, industry type, injury severity, early opioid prescribing, early MRI prescribing, lumbar spine surgery, claim litigation status, state Workers’ Compensation policy variables (wage replacement rate, waiting period, retroactive period, medical fee schedule, treating provider choice, and treating provider change).
Figure 1.
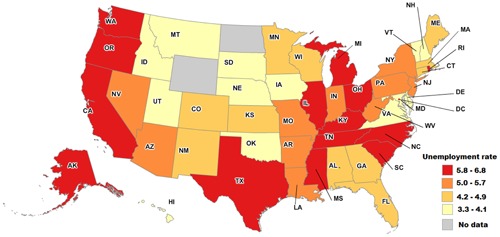
Average state unemployment rate in the U.S. (2002‐2008, inclusive)
Figure 2.
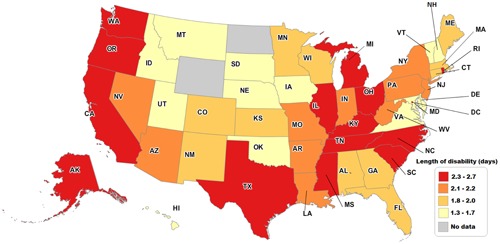
Adjusted association between state unemployment rate and length of disability in occupational low back pain in the U.S. (2002‐2008, inclusive)
Controlling for all statistically significant individual‐level and state‐level variables, state unemployment rate and rate of disabled workers receiving SSDI had significant associations with medical costs. An increase in state unemployment rate by 1% was associated with a $75 increase in mean of medical costs per case (95% CI $48, $104). Figure 3 shows the adjusted association between state unemployment rate and medical expenses. However, there was a decrease in mean medical costs per case by $237 (95% CI $168, $303) for each 1% increase in the rate of disabled workers receiving SSDI. There were also significant but smaller associations between neighborhood SE variables and mean medical costs (Table 4). An increase in neighborhood MHI by $10 000 and increase in population with less than some college educational attainment by 1% were associated with an increase in mean medical costs per case by $48 (95% CI $33, $63) and $5 (95% CI $3, $6), respectively. Additionally, each 1% increase in neighborhood population classified as rural and “white” was associated with a decrease in mean medical costs per case by $2 (95% CI $1, $2) and $3 (95% CI $2, $3), respectively. As shown in Table 3, examining randomness of neighborhood‐level variables’ effects on the outcomes showed that only MHI effects on LOD and medical costs varied significantly between states.
Figure 3.
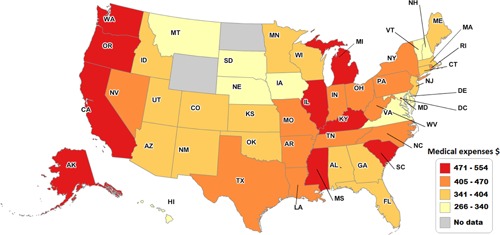
Adjusted association between state unemployment rate and medical expenses in occupational low back pain in the U.S. (2002‐2008, inclusive)
4. DISCUSSION
This study has shown significant regional socioeconomic disparities in medical costs and LOD due to occupational LBP, even when multiple potential confounders are addressed, and health insurance type and access are mostly uniform. Living in a state with a higher unemployment rate and lower neighborhood MHI were associated with increased LOD. Living in a state with a higher unemployment rate and lower percentage of disabled workers on SSDI were related to higher medical costs (reflected by higher utilization of medical services). Additionally, living in a neighborhood with a higher MHI, higher percentage of residents with less than some college educational attainment, with an urban setting, or with minority status were all associated with higher medical costs. However, the observed effects of MHI on LOD and medical costs varied in magnitude and direction between states. Overall, the observed associations of LOD and medical costs with neighborhood SE characteristics may seem modest, but, in fact, their effects on LOD and medical costs become more important when considering the entire national neighborhood‐level SE spectrum included in our sample (see Table 1). For example, when all independent variables have their grand mean values, the LOD for a person living in a neighborhood with the highest MHI is shorter by 3.9 days (95% CI 2.0, 5.9) and 4.9 days (95% CI 2.4, 7.3) than if the same person was living in neighborhoods with the average and the lowest MHIs, respectively. Similarly, the medical costs for a person living in a neighborhood with the highest MHI is higher by $1293 (95% CI $1000, $1586) and $1044 (95% CI $808, $1281) than if the same person were living in neighborhoods with average and the lowest MHIs, respectively. These findings may actually underestimate the full magnitude of the neighborhood SE effects on LOD and medical costs. Area‐level SE conditions may generally determine an individual's SE status (eg, income and education level). Thus, adjusting for an individual's SE characteristics could essentially eliminate a significant portion of the neighborhood effect by over‐adjusting.34
The observed associations of state and neighborhood SE characteristics with medical costs may suggest either regional differences in pricing of medical services or overutilization of potentially unnecessary medical services. Therefore, we conducted a sensitivity analysis using the total number of medical visits to any provider as an outcome variable, which showed similar associations in magnitude and direction to those presented in our original analysis (sensitivity analysis data are available on request).
Our findings of positive associations of state unemployment rate with medical costs and LOD are consistent with previous studies.39, 40 An increase in the U.S. unemployment rate was associated with higher national averages for LOD across multiple conditions,39 and higher medical costs.47 Injured workers living in areas with poor economic conditions may find it difficult to get alternative suitable employment or obtain modified and less physically demanding duties; employers have less incentive to offer accommodations and, thus, have longer disability duration which in turn drives more health care utilization.40, 47 Low area education may also be a surrogate for limited job and economic opportunities. Also, LBP might become more disabling due to higher levels of distress accompanying job insecurity in a context of high unemployment.48
Medical costs were slightly higher in cases residing in neighborhoods characterized by higher percentages of racial and ethnic minorities and lower educational attainment without significant differences in LOD, suggesting potentially unnecessary services for these persons and less incentive to return to work. In medical care for occupational LBP, there is ample evidence that over‐treatment, reflected by unnecessary services without additional improvement in LOD outcomes, is the main manifestation of poor quality care.21, 49, 50 For example, one study showed that patients with occupational LBP had higher medical costs and similar LOD outcomes when they were managed by primary care providers than those patients without a primary care provider involvement.49 Certain forms of care (such as chiropractic) associated with overtreatment are more common in populations with lower education and lower SES, and thus may account for the association with higher medical costs. More expensive and potentially unnecessary care is closely related to a higher occurrence of diagnostic testing and treatments that are not recommended by accepted evidence‐based guidelines,51, 52 which suggests lower quality care.19, 53 Thus, total medical expenses served as a suitable proxy for quality of care in our study.
Living in a state with a higher percentage of disabled workers on SSDI was related to lower medical costs. A plausible explanation for this is that some workers with complicated LBP substitute WC benefits with SSDI when they develop permanent disability or their eligibility for WC benefits is declined.54, 55
Overall, increased neighborhood MHI was associated with significantly lower LOD despite higher medical costs. This finding is consistent with other studies demonstrating that more affluent neighborhoods experience more favorable health outcomes4—and that this effect of affluence was greater than the negative effect of more intensive and potentially unnecessary medical care.
Medical costs for people living in more rural neighborhoods were slightly lower than medical costs for those living in more urban neighborhoods, with no significant difference in LOD. This suggests that, on average, rural populations might use fewer medical services without any negative impact on outcomes—consistent with results in other studies.23 Another potential explanation for this is that rural populations may be more resilient and have more active lifestyles.56 For example, one study of workers with occupational bone fractures showed that workers living in more rural zip codes had lower LOD than workers from urban zip codes.36
4.1. Implications
After accounting for multiple potential confounders, this study has shown significant regional socioeconomic disparities in medical costs and LOD due to occupational LBP despite a mostly uniform health insurance type and access to medical care. These results suggest that even after implementation of “health care for all” important regional disparities in quality of care and outcomes in LOD may persist, unless the underlying economic and structural factors that affect quality of medical care and non‐medical factors that affect recovery can be addressed. The combined influences of neighborhood and state SE characteristics on medical costs and LOD at a state and national levels are likely to remain high and not negligible as occupational LBP is highly prevalent.57 This highlights the need for further research to uncover and understand causal pathways underlying these associations.
4.2. Strengths and limitations
A primary strength of this study is the ability to evaluate the contribution of neighborhood and state SE factors to medical cost and LOD in a common and important condition affecting a working population, independent of the influence of health insurance access and coverage while controlling for several important individual‐level and state‐level factors. The results are highly generalizable as over 90% of the private workforce in the U.S. is covered by WC insurance. Also, our findings were based on a large longitudinal sample of LBP cases, identified using standardized and precise medical diagnosis codes (ICD‐9 codes), from 49 states over a period of 7 years. Additionally, the dataset has complete coverage of medical services provided to injured workers and is of comparable size in terms of the number and distribution of occupational injuries/disorders and overall medical costs to multiple occupational health datasets, such as BLS and the National Council on Compensation Insurance.24 Another unique strength is that the associations found in this study were independent of several very important individual‐level (eg, opioid prescribing) and state‐level WC policy (eg, medical fee schedules) characteristics.
This study also has some limitations. Our administrative dataset had no information on clinically observed injury severity measured by, for example, functional limitations. However, using ICD‐9 code to define injury severity, we found a significant relationship between “more severe” LBP and LOD. This result is consistent with the findings of a prior study that obtained more precise clinical information about injury severity using medical reports, and found that the ICD‐9 severity designation correlated well with those found in medical reports in a similar dataset.58 Additionally, there was no information on several important predictors of disability duration, such as occupation, job physical demand levels, social support at work, worker's recovery expectations and employer/supervisor‐employee relationship.59, 60 Ideally, we would have access to patient self‐report to address these important variables, but this type of information is not readily available or collected in administrative WC data. However, these factors would not have a significant impact on the magnitude and direction of the associations observed in this study, unless there were significant differences between states or between neighborhoods in these variables. Another limitation is that the measure of LOD was based on paid indemnity services, yet termination of indemnity benefits does not necessarily imply that workers experienced a sustained return to work. Additionally, estimates of medical costs might have been influenced by medical cost differences between and within states, and not all differences in medical costs reflect differences in quality of care. But, it is unlikely that this affected findings significantly, because the presence of state medical fee schedules was an adjustment factor. Also, the direction and magnitude of associations of state and neighborhood SE characteristics were consistent in sensitivity analysis using the number of medical visits to any provider as an outcome. Another potential limitation is the slight differences between dates of collection of individual‐level data (2002‐2008) and neighborhood SE characteristics (2005‐2009). Additionally, neighborhood SE characteristics were measured at a census tract‐level rather than census block‐level due to insufficient number of cases at these two neighborhood levels. However, prior studies showed that lag‐times up to several years61 and whether census tract or census block aggregate data are used are unlikely to affect observed relationships, because socioeconomic conditions tend to be generally stable over several years, and block‐level SE measures are quite similar within tracts.34, 61
5. CONCLUSIONS
This study showed that state and neighborhood SE conditions are associated with medical cost and LOD in the context of universal health insurance coverage and wage compensation, even after controlling for several important individual and state characteristics. The findings suggest that state and neighborhood SE conditions are significant and independent contributors to healthcare costs and work disability outcomes, primarily for people living in disadvantaged neighborhoods. For clinicians, results suggest that local environmental context should be considered when evaluating risk for delayed return to work.
Supporting information
Additional Supporting Information may be found online in the supporting information tab for this article.
Supporting Table S1.
Supporting Table S2.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the planning of the study and drafting of the manuscript. Mujahed Shraim, Manuel Cifuentes, and Joanna L. Willetts planned and conducted the analyses. All authors have approved this version of the manuscript.
ACKNOWLEDGMENTS
The authors would like to thank YoonSun Choi for invaluable assistance with statistical analyses, Elyssa Besen and Tin‐Chi Lin for editorial reviews, and Peg Rothwell for editorial assistance.
FUNDING
The Liberty Mutual Research Institute for Safety sponsored the study. The parent company, Liberty Mutual Insurance, had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
ETHICS APPROVAL AND INFORMED CONSENT
The study was approved by the New England Institutional Review Board.
DISCLOSURE (AUTHORS)
The authors declare no conflicts of interest.
DISCLOSURE BY AJIM EDITOR OF RECORD
Steven Markowitz declares that he has no competing or conflicts of interest in the review and publication decision regarding this article.
DISCLAIMER
None.
Shraim M, Cifuentes M, Willetts JL, Marucci‐Wellman HR, Pransky G. Regional socioeconomic disparities in outcomes for workers with low back pain in the United States. Am J Ind Med. 2017; 60: 472–483. https://doi.org/10.1002/ajim.22712
Institution at which the work was performed: Liberty Mutual Research Institute for Safety, Hopkinton, MA.
REFERENCES
- 1. Kulkarni SC, Levin‐Rector A, Ezzati M, Murray CJ. Falling behind: life expectancy in US counties from 2000 to 2007 in an international context. Popul Health Metr. 2011; 9:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood). 2002; 21:60–76. [DOI] [PubMed] [Google Scholar]
- 3. Gatrell AC. Structures of geographical and social space and their consequences for human health. Geografiska Annaler. 1997; 79:141–154. [Google Scholar]
- 4. Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Commun Health. 2001; 55:111–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gusmano MK, Weisz D, Rodwin VG, et al. Disparities in access to health care in three French regions. Health Policy. 2014; 114:31–40. [DOI] [PubMed] [Google Scholar]
- 6. Kapral MK, Wang H, Mamdani M, Tu JV. Effect of socioeconomic status on treatment and mortality after stroke. Stroke. 2002; 33:268–273. [DOI] [PubMed] [Google Scholar]
- 7. Luo ZC, Kierans WJ, Wilkins R, Liston RM, Mohamed J, Kramer MS. Disparities in birth outcomes by neighborhood income: temporal trends in rural and urban areas, british columbia. Epidemiology. 2004; 15:679–686. [DOI] [PubMed] [Google Scholar]
- 8. Stafford M, Marmot M. Neighbourhood deprivation and health: does it affect us all equally? Int J Epidemiol. 2003; 32:357–366. [DOI] [PubMed] [Google Scholar]
- 9. Wang JY, Wang CY, Juang SY, et al. Low socioeconomic status increases short‐term mortality of acute myocardial infarction despite universal health coverage. Int J Cardiol. 2014; 172:82–87. [DOI] [PubMed] [Google Scholar]
- 10. Epstein D, Reibel M, Unger JB, et al. The effect of neighborhood and individual characteristics on pediatric critical illness. J Community Health. 2014; 39:753–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Robbins AS, Chen AY, Stewart AK, Staley CA, Virgo KS, Ward EM. Insurance status and survival disparities among nonelderly rectal cancer patients in the National Cancer Data Base. Cancer. 2010; 116:4178–4186. [DOI] [PubMed] [Google Scholar]
- 12. Signorello LB, Cohen SS, Williams DR, Munro HM, Hargreaves MK, Blot WJ. Socioeconomic status, race, and mortality: a prospective cohort study. Am J Public Health. 2014; 104:e98–e107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Eaddy MT, Cook CL, O'Day K, Burch SP, Cantrell CR. How patient cost‐sharing trends affect adherence and outcomes: a literature review. P T. 2012; 37:45–55. [PMC free article] [PubMed] [Google Scholar]
- 14. Manning WG, Newhouse JP, Duan N, et al. Health Insurance and the Demand for Medical Care: evidence From a Randomized Experiment. Santa Monica, CA: RAND Corporation; 1988. [PubMed] [Google Scholar]
- 15. Tamblyn R, Laprise R, Hanley JA, et al. Adverse events associated with prescription drug cost‐sharing among poor and elderly persons. JAMA. 2001; 285:421–429. [DOI] [PubMed] [Google Scholar]
- 16.Liberty Mutual Research Institute for Safety. Annual Report of Scientific Activity. Hopkinton, MA: Liberty Mutual Research Institute for Safety; 2014. [Google Scholar]
- 17. Staal JB, Hlobil H, van Tulder MW, et al. Occupational health guidelines for the management of low back pain: an international comparison. Occup Environ Med. 2003; 60:618–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dagenais S, Caro J, Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. Spine J. 2008; 8:8–20. [DOI] [PubMed] [Google Scholar]
- 19. Deyo RA, Mirza SK, Turner JA, Martin BI. Overtreating chronic back pain: time to back off? J Am Board Fam Med. 2009; 22:62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Paduda J. 2013. Workers' comp rates are up, but still no profit. Available at: http://www.joepaduda.com/2013/06/workers‐comp‐rates‐up‐still‐profit/. Last accessed January 4, 2016.
- 21. Cifuentes M, Willetts J, Wasiak R. Health maintenance care in work‐related low back pain and its association with disability recurrence. J Occup Environ Med. 2011; 53:396–404. [DOI] [PubMed] [Google Scholar]
- 22. Webster BS, Choi Y, Bauer AZ, Cifuentes M, Pransky G. The cascade of medical services and associated longitudinal costs due to nonadherent magnetic resonance imaging for low back pain. Spine. 2014; 39:1433–1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Young AE, Cifuentes M, Wasiak R, Webster BS. Urban‐rural differences in work disability following occupational injury: are they related to differences in healthcare utilization? J Occup Environ Med. 2009; 51:204–212. [DOI] [PubMed] [Google Scholar]
- 24. Murphy PL, Sorock GS, Courtney TK, Webster BS, Leamon TB. Injury and illness in the, American workplace: a comparison of data sources. Am J Ind Med. 1996; 30:130–141. [DOI] [PubMed] [Google Scholar]
- 25. Shraim M, Cifuentes M, Willetts JL, Marucci‐Wellman HR, Pransky G. Length of disability and medical costs in low back pain: do state workers' compensation policies make a difference? J Occup Environ Med. 2015; 57:1275–1283. [DOI] [PubMed] [Google Scholar]
- 26.U.S. Bureau of Labor Statistics. 2010. Measuring Price Chnage for Medical Care in the CPI. Available at: http://www.bls.gov/cpi/cpifact4.htm. Last accessed December 28, 2015.
- 27. Eccleston SM. WCRI Medical Price Index for Workers’ Compensation. 2nd ed Cambridge, MA: Workers Compensation Research Institute; 2008. [Google Scholar]
- 28. Hashemi L, Webster BS, Clancy EA, Volinn E. Length of disability and cost of workers' compensation low back pain claims. J Occup Environ Med. 1997; 39:937–945. [DOI] [PubMed] [Google Scholar]
- 29.United States Census Bureau. 2013. Census Tracts and Block Numbering Areas. Available at: http://www2.census.gov/geo/pdfs/reference/GARM/Ch10GARM.pdf. Last accessed December 5, 2015.
- 30.Esri. ArcGIS Desktop: release 10. Redlands, CA: Environmental Systems Research Institute; 2013. [Google Scholar]
- 31. Doubeni CA, Schootman M, Major JM, et al. Health status, neighborhood socioeconomic context, and premature mortality in the United States: the National Institutes of Health‐AARP Diet and Health Study. Am J Public Health. 2012; 102:680–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fuentes M, Hart‐Johnson T, Green CR. The association among neighborhood socioeconomic status, race and chronic pain in black and white older adults. J Natl Med Assoc. 2007; 99:1160–1169. [PMC free article] [PubMed] [Google Scholar]
- 33. Martens PJ, Chateau DG, Burland EM, et al. The effect of neighborhood socioeconomic status on education and health outcomes for children living in social housing. Am J Public Health. 2014; 104:2103–2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pearl M, Braveman P, Abrams B. The relationship of neighborhood socioeconomic characteristics to birthweight among 5 ethnic groups in California. Am J Public Health. 2001; 91:1808–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992; 82:816–820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Young AE, Wasiak R, Webster BS, Shayne RG. Urban‐rural differences in work disability after an occupational injury. Scand J Work Environ Health. 2008; 34:158–164. [DOI] [PubMed] [Google Scholar]
- 37. Adler NE, Stewart J. Health disparities across the lifespan: meaning, methods, and mechanisms. Ann NY Acad Sci. 2010; 1186:5–23. [DOI] [PubMed] [Google Scholar]
- 38. Kennedy BP, Kawachi I, Glass R, Prothrow‐Stith D. Income distribution, socioeconomic status, and self rated health in the United States: multilevel analysis. BMJ. 1998; 317:917–921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lipton B, Robertson J, Porter K. 2015. Workers Compensation Temporary Total Disability Indemnity Benefit Duration: 2013 Update. NCCI Research Brief. Available at: https://www.ncci.com/Articles/Documents/II_TTD_Duration_final.pdf. Last accessed May 26, 2015.
- 40. Victor RA, Fleischman C. How Choice of Provider and Recessions Affect Medical Costs in Workers' Compensation. Cambridge, MA: Workers Compensation Research Institute; 1990. [Google Scholar]
- 41.SAS Institute I. 2008. SAS/STAT® 9.2 User's Guide. Cary, NC: SAS Institute, Inc. [Google Scholar]
- 42. Snijders TAB. Power and sample size in multilevel linear models In: Everitt BS, Howell DC, eds. Encyclopedia of Statistics in Behavioral Science. Chicester: Wiley; 2005:1570–1573. [Google Scholar]
- 43. Wang J, Xie H, Fisher JH. Multilevel Models, Applications Using SAS. Germany: Higher Education Press and Walter De Gruyter; 2012. [Google Scholar]
- 44. Krause N, Dasinger LK, Deegan LJ, Brand RJ, Rudolph L. Alternative approaches for measuring duration of work disability after low back injury based on administrative workers' compensation data. Am J Ind Med. 1999; 35:604–618. [DOI] [PubMed] [Google Scholar]
- 45.NOISH. Worker Nealth Charterbook, 2004. Cincinnati, OH: Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, DHHS (NIOSH) Publication No. 2004–149; 2004. [Google Scholar]
- 46. Shaw WS, Pransky G, Patterson W, Winters T. Early disability risk factors for low back pain assessed at outpatient occupational health clinics. Spine. 2005; 30:572–580. [DOI] [PubMed] [Google Scholar]
- 47. Boden LB, Fleischman CA. Medical Costs in Workers' Compensation: trends and Interstate Comparisons. Cambridge, MA: Workers Compensation Research Institute; 1989. [Google Scholar]
- 48. Volinn E, Nishikitani M, Volinn W, Nakamura Y, Yano E. Back pain claim rates in Japan and the United States: framing the puzzle. Spine. 2005; 30:697–704. [DOI] [PubMed] [Google Scholar]
- 49. Atlas SJ, Wasiak R, van den Ancker M, Webster B, Pransky G. Primary care involvement and outcomes of care in patients with a workers' compensation claim for back pain. Spine (Phila Pa 1976). 2004; 29:1041–1048. [DOI] [PubMed] [Google Scholar]
- 50. Webster BS, Verma S, Willetts J, Hopcia K, Wasiak R. Association of disability duration with physical therapy services provided after meniscal surgery in a workers' compensation population. Arch Phys Med Rehabi. 2011; 92:1542–1551. [DOI] [PubMed] [Google Scholar]
- 51. Dagenais S, Roffey DM, Wai EK, Haldeman S, Caro J. Can cost utility evaluations inform decision making about interventions for low back pain? Spine J. 2009; 9:944–957. [DOI] [PubMed] [Google Scholar]
- 52. Waddell G, Burton AK. Occupational health guidelines for the management of low back pain at work: evidence review. Occup Med (Lond). 2001; 51:124–135. [DOI] [PubMed] [Google Scholar]
- 53. Haldeman S, Dagenais S. What have we learned about the evidence‐informed management of chronic low back pain? Spine J. 2008; 8:266–277. [DOI] [PubMed] [Google Scholar]
- 54. Guo X, Burton JF. The growth in applications for Social Security Disability Insurance: a spillover effect from workers' compensation. Soc Secur Bull. 2012; 72:69–88. [PubMed] [Google Scholar]
- 55. O'Leary P, Boden LI, Seabury SA, Ozonoff A, Scherer E. Workplace injuries and the take‐up of Social Security disability benefits. Soc Secur Bull. 2012; 72:1–17. [PubMed] [Google Scholar]
- 56. Martoz‐Baden R, Colvin PL. Coping strategies: a rural‐urban comparison. Family Relations. 1986; 25:281–288. [Google Scholar]
- 57.U.S. Bureau of Labor Statistics. 2014. Nonfatal occupational injuries and illnesses requiring days away from work, 2013. Available at: http://www.bls.gov/news.release/pdf/osh2.pdf. Last accessed January 4, 2016.
- 58. Webster BS, Bauer AZ, Choi Y, Cifuentes M, Pransky GS. Iatrogenic consequences of early magnetic resonance imaging in acute, work‐related, disabling low back pain. Spine. 2013; 38:1939–1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Shaw WS, Pransky G, Fitzgerald TE. Early prognosis for low back disability: intervention strategies for health care providers. Disabil Rehabil. 2001; 23:815–828. [DOI] [PubMed] [Google Scholar]
- 60. Steenstra IA, Busse JW, Tolusso D, et al. Predicting time on prolonged benefits for injured workers with acute back pain. J Occup Rehabil. 2014; 25:267–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Geronimus AT, Bound J. Use of census‐based aggregate variables to proxy for socioeconomic group: evidence from national samples. Am J Epidemiol. 1998; 148:475–486. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional Supporting Information may be found online in the supporting information tab for this article.
Supporting Table S1.
Supporting Table S2.


