Neuromyelitis optica spectrum disorder (NMOSD) associated with aquaporin-4 antibody (AQP4-Ab) predominantly targets the optic nerve and spinal cord and is characterized by frequent relapses and accrual of irreversible disability.1 Variations in clinical course may include an initial or predominant involvement in extra spinal/optic nerve locations and a benign course marked by mild attacks and minimal residual deficits.2,3 However, spontaneous remissions are rare. We are reporting 2 patients who satisfied the 2015 criteria for NMOSD4 and had a unique disease course highlighted by periods of spontaneous remission lasting 19 and 23 years.
Methods.
Patient 1.
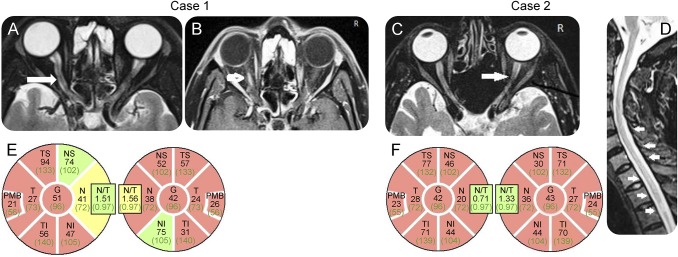
In 1995, a then 31-year-old woman developed severe unexplained vomiting for nearly a month, followed by a brief period of ataxia, diplopia, and dysarthria. The following year, she had urinary retention for a week without any limb weakness. In the third year of her illness, she had sequential optic neuritis staring in the left eye for which she received a short course of oral steroids. Her vision remained poor ever since. In subsequent years, she had no other medication except treatment for hypothyroidism. Nineteen years later, at the age of 51 years, she presented to us with optic neuritis in the right eye. Review of her medical records revealed that brain MRI (1995–1997) documented an initially enhancing lesion in the medulla extending into the high cervical cord. Visual evoked potentials were abnormal and oligoclonal bands were negative. During her current admission, her corrected visual acuity was 20/200 in both eyes. The rest of neurologic examination was normal. Her recent MRI (figure, A and B) was consistent with the diagnosis of NMOSD, and optical coherence tomography demonstrated the extent of visual loss (figure, E). Cell-based assay for AQP4-Ab was positive (EUROIMMUN, Lübeck, Germany).
Figure. MRI and OCT data of patients.
(A and B) Hyperintensity (FATSAT axial) and enhancement of the right optic nerve. (C) Resolving LETM (T2W sagittal) in the cervicodorsal spinal cord. (D) Bilateral long segment atrophy of optic nerves. (E and F) OCT images (ring scan data) from both eyes of each patient showing severe retinal nerve fiber layer thinning compared with normative device data (red areas indicate thickness below first percentile). G = global; FATSAT = fat saturated; LETM = longitudinally extensive transverse myelitis; N = nasal; NI = nasal-inferior; NT = nasal-superior; OCT = optical coherence tomography; PMB = peripapillary macular bundle; T = temporal; TI = temporal-inferior; TS = temporal-superior.
Patient 2.
In 1983, at the age of 28 years, this male patient had acute onset weakness of lower limbs with urinary retention. As reported by the patient, he underwent a myelogram for the same and was thought to have a tumor in the cervical spinal cord. He was empirically given a course of steroids for 3 weeks following which he gradually regained power in his limbs and remained well for the next 22 years. In 2001, at the age of 36 years, he had left optic neuritis which recovered poorly with steroids. Since then, he had myelitis averaging 1 attack every 2 years, mostly in the form of a “partial cord syndrome.” He presented to our center in 2011 where MRI (figure, C and D) and AQP4-Ab testing were confirmatory for NMOSD. At present, visual acuity in his right eye is 20/200 and in the left eye counting fingers at 1 foot distance. He remains attack free after starting immunosuppressants.
Discussion.
The 2 patients described in our report had a unique clinical course characterized by long periods of spontaneous remission, 19 and 23 years. Our first patient had in retrospect an area postrema syndrome followed by severe bilateral optic neuritis. Evaluation of later events in patient 2 suggests that the first attack was likely to have been a tumefactive myelitis which responded to steroids. Both patients had chronic disease spanning decades, with severe visual loss and minimal spinal cord dysfunction.
Wingerchuck et al.5 have highlighted the varied clinical course of NMO. While 90% of patients relapse within 5 years after the index event, some may have a much longer disease-free period.5 We were unable to find published cases in the literature that highlighted extended periods of spontaneous remission similar to our patients. A recent case report identified an AQP4-Ab–positive oriental woman who had 11 episodes of recurrent unilateral optic neuritis over a period of 22 years.6 Localization to the optic nerve and the lengthy disease course were similar to our patients. There has been a phenomenal expansion of our knowledge of the clinical spectrum of NMOSD in recent years. Our report contributes additional information that spontaneous and lengthy remissions may occur and particularly in the early phase of AQP4-Ab–mediated NMOSD. A review of history going well beyond the conventional period may unearth similar cases in other large NMOSD registries and provide a valuable cohort of patients for future studies.
Footnotes
Authors contributions: Lekha Pandit: drafting/revising the manuscript, study concept or design, and analysis or interpretation of data, accepts responsibility for conduct of research and will give final approval, acquisition of data, study supervision, responsible for listing contributors who do not qualify for authorship, and responsible for assuring that all authors submit disclosure forms. Sharik Mustafa: drafting/revising the manuscript.
Study funding: No targeted funding reported.
Disclosure: The authors report no disclosures. Go to Neurology.org/nn for full disclosure forms. The Article Processing Charge was funded by the authors.
References
- 1.Jarius S, Ruprecht K, Wildemann B, et al. Contrasting disease patterns in seropositive and seronegative neuromyelitis optica: a multicentre study of 175 patients. J Neuroinflammation 2012;9:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collangues N, Cabre P, Marignier R, et al. A benign form of neuromyelitis optica: does it exist? Arch Neurol 2011;68:918–924. [DOI] [PubMed] [Google Scholar]
- 3.Bergamaschi R, Jarius S, Robotti M, et al. Two cases of benign neuromyelitis optica in patients with celiac disease. J Neurol 2009;256:2097–2099. [DOI] [PubMed] [Google Scholar]
- 4.Wingerchuck DM, Banwell B, Bennett J, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 2015;85:177–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wingerchuk DM, Hogancamp WF, O'Brien PC, et al. The clinical course of neuromyelitis optica (Devic's syndrome). Neurology 1999;53:1107–1114. [DOI] [PubMed] [Google Scholar]
- 6.Yew CY, Hor YJ, Lim TT, et al. Eleven episodes of recurrent optic neuritis of the same eye for 22 years eventually diagnosed as neuromyelitis optica spectrum disorder. Mult Scler Relat Disord 2016;10:22–25. [DOI] [PubMed] [Google Scholar]