Abstract
Background
Hospital-acquired respiratory viral infections can result in morbidity and mortality of hospitalized patients. This study was undertaken to better understand the magnitude of the problem of nosocomial respiratory viral infections in adult and pediatric patients.
Methods
This was a retrospective study at a tertiary care adult and pediatric teaching hospital. Study patients met a priori criteria for definite or possible nosocomial respiratory viral infection.
Results
From April 1, 2015 to April 1, 2016, we identified 40 nosocomial respiratory viral infections in 38 patients involving 14 definite and 3 possible cases in our adult hospital and 18 definite and 5 possible cases in our pediatric hospital. The incidence was 5 cases/10 000 admissions and 44 cases/10 000 admissions to our adult and pediatric hospitals, respectively. Only 6.8% of cases were due to influenza. Although 63% of cases occurred during the fall and winter, such infections were identified throughout the year. Five (13%) nosocomial respiratory viral infections occurred in 2 adult and 3 pediatric patients who died during the hospitalization.
Conclusions
Nosocomial respiratory viral infections are an underappreciated cause of morbidity and mortality in hospitalized adult and pediatric patients. The incidence was nearly 10-fold higher in our pediatric hospital. We estimate there are approximately 18 955 pediatric and adult cases of nosocomial respiratory viral infections in US acute care hospitals each year.
Keywords: hospital-acquired, nosocomial, pneumonia, respiratory tract infection, viral
Respiratory viruses are transmitted in the hospital setting from direct contact with infected visitors and family, infected healthcare workers, other infected patients, indirectly through contact with contaminated fomites, or from patient-to-patient spread due to poor hand hygiene practices among healthcare providers. The frequency of specific respiratory viruses causing nosocomial infections reflects their activity in the community [1]. Few studies have assessed the outcomes of nosocomial respiratory viral infections in noncritically ill, non-immunocompromised adult and pediatric patients. In one study, 1 in 5 children admitted to a pediatric intensive care unit (ICU) due to a respiratory viral infection had acquired the infection in the hospital. These children had an approximately 6-fold increased likelihood of mortality compared with those who had community-acquired respiratory viral infections [2]. In another pediatric study, 49% of nosocomial respiratory viral infections occurred in premature infants [3]. One study in adult patients noted that 24% of nonventilated hospital-acquired pneumonias were caused by viruses [4]. These publications suggest that nosocomial respiratory viral infections can lead to significant morbidity and mortality. We investigated such cases in our adult and pediatric hospitals to better understand the magnitude of the problem and the outcomes of such infections.
METHODS
This was a retrospective, Institutional Review Board-approved study of patients who developed laboratory-confirmed respiratory viral infections and whose symptoms began during hospitalization at Rhode Island Hospital and Hasbro Children’s Hospital (HCH) between April 1, 2015 and April 1, 2016. Rhode Island Hospital is licensed for 719 beds, 87 of which are licensed for HCH. The two hospitals are located in adjoining buildings on the same campus as part of the Lifespan Hospital System.
A nosocomial respiratory viral infection was defined as a hospitalized patient who had a positive respiratory viral panel ([RVP] Luminex, Austin, TX), rapid influenza test (Xpert; Cepheid, Sunnyvale, CA), or rapid respiratory syncytial virus (RSV) test (Xpert; Cepheid) of a nasopharyngeal or bronchoscopic lavage specimen. The RVP assay included testing for influenza A and B, RSV A and B, coronavirus, parainfluenza, human metapneumovirus, adenovirus, as well as rhinovirus and enterovirus; however, the assay did not distinguish the latter 2 viruses, which heretofore will be noted as rhino/enterovirus. Hospitalized patients with a positive result in one of these tests during the study period were identified using our institutional infection control software system (TheraDoc; Premier, Charlotte, NC). A definite nosocomial respiratory viral infection was defined as a patient whose number of days from hospital admission to symptom onset exceeded the upper range for the incubation period of the identified virus (Table 1). A possible nosocomial respiratory viral infection case was defined as a patient in whom the number of days from hospital admission to symptom onset was within the range of the incubation period for the identified virus who were admitted without clinical signs or symptoms of a respiratory infection. A patient could be included more than once during the hospitalization if they had complete resolution of symptoms ascribed to the respiratory viral infection, recurrence of symptoms compatible with such an infection, and the time interval was greater than the above-noted incubation period. If the second such episode was due to a different virus, it was considered a definite case, and if it was due to the same virus, it was considered a possible case. Cases were assigned to a season based on the date when the symptoms of a respiratory viral infection were first documented in the medical record. Estimates of the incidence of nosocomial viral infections yearly in US acute care adult and pediatric hospitals were based on the number of such infections identified in the current study and the number of admissions to these hospitals during the 2014 fiscal reporting year based on data from the American Hospital Association.
Table 1.
Viral Incubation Periodsa
| Virus | Median (Range) Incubation Period |
|---|---|
| Adenovirus [23] | 5.6 days (4.8–6.3 days) |
| Coronavirus [23] | 3.2 days (2.8–3.7 days) |
| Influenza A [23] | 1.4 days (1.3–1.5 days) |
| Influenza B [23] | 0.6 days (0.5–0.6 days) |
| Parainfluenza [23] | 2.6 days (2.1–3.1 days) |
| Respiratory syncytial virus A and B [23] | 4.4 days (3.9–4.9 days) |
| Rhino/enterovirus [23] | 1.9 days (1.4–2.4 days) |
| Metapneumovirus [23, 24] | Not available (3–6 days) |
aViral incubation included in this table correlate with the viruses detected on the laboratory respiratory viral panel, rapid influenza, and rapid respiratory syncytial virus tests used in this study. There has been no established incubation period for metapneumovirus in the literature, and the range is based on reported cases.
A literature review was performed using the following PubMed search terms: nosocomial; hospital-acquired; and respiratory viral infections. Only studies written in the English language were included. Studies were excluded in our comparative analysis of the incidence of respiratory viral infections if the study was an outbreak investigation or if the reported incidence included nonrespiratory viral infections.
RESULTS
We identified 40 (32 definite and 8 possible) nosocomial viral respiratory tract infections in 38 patients during the study period, including 17 patients admitted to the adult hospital and 23 patients admitted to the pediatric hospital (5 and 44 cases per 10 000 admissions to the adult and pediatric hospital, respectively) (Table 2). The median age of cases in the adult and pediatric hospitals was 56 and 1 year of age, respectively. Eleven (28%) of the cases were immunocompromised. In 6 cases, patients were in an ICU when they developed symptoms. In 5 other cases, after the nosocomial respiratory viral infection was identified, the patient was transferred to an ICU. The mean interval from symptom onset to ICU admission was 1.8 days. Two of these 5 cases, and 4 of the 10 cases already in an ICU, required mechanical ventilation after a mean interval of 5 and 0 days after symptom onset, respectively. In 17 of the 40 cases (43%), antibiotics were initiated at the time of symptom onset, and in 82% of the cases, the antibiotics were continued despite positive test results for the respiratory viral infection. It is unclear how many of these cases had bacterial coinfection. Fever (defined as temperature >38°C) and/or cough were the initial symptoms in over half of the cases (78% and 60%, respectively). Fever was the most common symptom among the pediatric patients (83%), whereas cough was the most common symptom among adult patients (77%). Congestion and rhinorrhea were present in 48% and 38% of patients, respectively. No adult patients had documented symptoms of vomiting or conjunctivitis associated with their viral infection; however, both were documented in pediatric patients (15% and 2.5%, respectively). No adult patients had a single isolated symptom at presentation, but fever was the only presenting symptom in 3 of the 23 pediatric cases.
Table 2.
Patient Demographics, Medical History, and Hospital Interventions
| All Patients | Adult Hospital | Pediatric Hospital | |
|---|---|---|---|
| 40 | 17 | 23 | |
| Years of age [mean (interquartile range)/median] | 26 (54)/8 | 56 (27)/56 | 3.3 (12)/1.1 |
| Female sex (%) | 17 (43) | 6 (35) | 11 (48) |
| Definite case (%) | 32 (80) | 14 (82) | 18 (78) |
| Past Medical History | |||
| Asthma (%) | 5 (13) | 2 (12) | 3 (13) |
| COPD (%) | 2 (5) | 2 (12) | 0 |
| Other chronic lung diseases (%) | 4 (10) | 0 | 4 (17) |
| Past neonatal intensive care unit admission (%) | N/A | Unknown | 12 (57)a |
| Immunocompromised (%)a | 11 (28) | 4 (24) | 7 (30) |
| Admission Diagnosis | |||
| Pneumonia (%) | 3 (7.5) | 3 (18) | 0 |
| Other infection (%) | 11 (28) | 6 (35) | 5 (22) |
| Noninfectious (%) | 26 (65) | 8 (47) | 18 (78) |
| Malignancy/scheduled chemotherapy (%) | 5 (13) | 1 (5.9) | 4 (17) |
| Intervention After Onset of Respiratory Viral Infection Symptoms | |||
| Transfer to intensive care unit (%) | 5 (13) | 2 (12) | 3 (13) |
| Intubation (%) | 6 (15) | 1 (5.8) | 5 (22) |
| Started on antibiotics (%) | 17 (43) | 7 (41) | 10 (44) |
| Died during same hospitalization (%) | 5 (13) | 2 (12) | 3 (13) |
Abbreviations: COPD, chronic obstructive pulmonary disease; HIV, human immunodeficiency virus; N/A, not applicable.
aSubjects were considered immunocompromised if they had any of the following: positive HIV test, report of HIV infection; receiving a prolonged course of steroids or other immunomodulatory medications; neutropenia during the hospitalization; or undergoing active chemotherapy during the hospitalization.
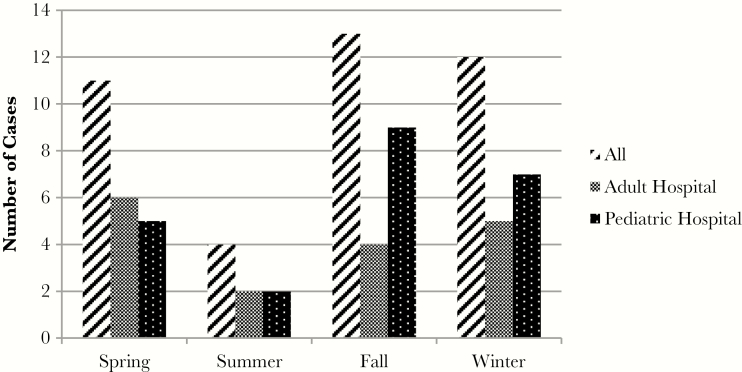
Forty-four viruses were identified in the 40 cases, including 4 cases of viral coinfection (Table 3). The most common viruses identified were rhino/enterovirus in both adults (61%) and pediatric cases (54%). Influenza A only accounted for 3 cases (6.8%); no nosocomial influenza B cases were identified. During the study period, influenza activity was widespread in Rhode Island March 2, 2015 through April 1, 2016 per data from the Rhode Island Department of Health. Although 63% of cases occurred in the fall and winter, they were identified throughout the year (Figure 1).
Table 3.
Types of Viruses Causing Nosocomial Respiratory Viral Infectionsa
| All Viruses No. (%) | Adult Hospital No. (%) | Pediatric Hospital No. (%) | Seasons No. | |
|---|---|---|---|---|
| 44 | 18 | 26 | 44 | |
| Adenovirus | 3 (6.8) | 2 (11) | 1 (3.8) | Sp 1; Su 0; F 1; W 1 |
| Coronavirus | 2 (4.5) | 0 (0) | 2 (7.7) | Sp 0; Su 0; F 1; W 1 |
| Influenza A | 3 (6.8) | 1 (5.6) | 2 (7.7) | Sp 0; Su 0; F 0; W 3 |
| Influenza B | 0 (0) | 0 (0) | 0 (0) | N/A |
| Parainfluenza | 1 (2.3) | 0 (0) | 1 (3.8) | Sp 1; Su 0; F 0; W 0 |
| Respiratory syncytial virus A and B |
6 (14) | 2 (11) | 4 (15) | Sp 3; Su 0; F 0; W 3 |
| Rhino/enterovirus | 25 (57) | 11 (61) | 14 (54) | Sp 6; Su 5; F 9; W 5 |
| Metapneumovirus | 4 (9) | 2 (11) | 2 (7.7) | Sp 2; Su 0; F 0; W 2 |
Abbreviations: F, fall; N/A, not applicable; Sp, spring; Su, summer; W, winter.
aThree patients had viral coinfection: 1 pediatric patient was infected with rhino/enterovirus and parainfluenza, another pediatric patient was infected with rhino/enterovirus, metapneumovirus, and influenza A. One adult patient was infected with both adenovirus and respiratory syncytial virus.
Figure 1.
Seasonality of nosocomial respiratory viral infections. Seasons were determined by the date that symptoms onset was first documented in the medical record. Spring, March 19–June 20; Summer, June 21–September 23; Fall, September 23–December 20; and Winter, December 21–March 18. The results shown in this graphic reflect the time period of the study (April 1, 2015–April 1, 2016).
Two adult and 3 pediatric patients (13%) died during the hospitalization involving rhino/enterovirus (2 adults, 1 pediatric patient), metapneumovirus (1 pediatric patient), and RSV (1 pediatric patient). The 3 pediatric patients were under 2 years of age. It is difficult to ascribe mortality to such infections in patients with multiple comorbidities; however, 1 pediatric patient with multiple congenital abnormalities decompensated shortly after the viral infection was diagnosed leading to intubation and extracorporeal membrane oxygenation (ECMO). The patient died 1 month after the respiratory virus testing was positive. Another pediatric patient with a hematologic malignancy decompensated shortly after the viral infection was diagnosed leading to intubation and ECMO. The patient died 11 days after respiratory virus testing was positive.
DISCUSSION
Forty nosocomial respiratory viral infections were diagnosed in 38 patients during 1 year, predominantly involving rhino/enterovirus in both pediatric and adult patients. Our data are strikingly similar to a study done nearly 40 years ago [5]. These authors found an incidence of 55 nosocomial respiratory viral infections per 10 000 pediatric hospital admissions, and 4 such infections per 10 000 adult medical admissions. Overall, 1 in 229 admissions to our pediatric hospital developed a nosocomial respiratory viral infection. However, at its peak in the fall, 1 in 139 admissions to our pediatric hospital developed such an infection. Based on our data and the number of US hospital admissions during fiscal year 2014, we estimate that there are approximately 15 834 adult and 3121 pediatric cases of nosocomial respiratory viral infections in US acute care hospitals yearly.
Fever and/or cough were the most common presenting symptoms often leading to initiation of antibacterial therapy. Approximately half of the pediatric cases were under 1 year of age, and these patients appear to be at greater risk of acquiring such infections [6]. Twelve percent of cases were associated with ICU admission, and 15% required intubation a mean of 1.8 days after symptom onset. One fatal case involved a nosocomial RSV infection, and another involved nosocomial metapneumovirus infection; however, both cases were associated with deterioration requiring intubation and ECMO. Autopsy data have confirmed that nosocomial respiratory viral infections can cause or contribute to mortality [7].
Respiratory viruses are clearly important pathogens causing hospital-acquired infections [8, 9]. In one study, 23% of severe nosocomial pneumonia in adults were due to respiratory viruses [10]. For decades, it has been known that nosocomial respiratory viral infections are a particular problem in pediatric patients [11]. In one study, 1 in 6 children under the age of 4 hospitalized for 1 week or more during winter or spring developed a nosocomial respiratory viral infection [12]. However, detailed studies of noninfluenza nosocomial respiratory viral infections are limited, and, to our knowledge, our study is the only one that broadly assessed the incidence of these infections in both adult and pediatric patients in a nonepidemic setting in approximately 40 years (Table 4). We found that rhinovirus and/or enterovirus were the predominant viruses identified among nosocomial respiratory viral infections. A previous prospective cohort study demonstrated that rhinovirus was the most commonly detected virus among children with viral respiratory infections, and approximately 20% of these infections were hospital acquired [13]. Similar to our findings, a pediatric study found that 73% of nosocomial respiratory infections were due to rhinovirus [14]. However, another pediatric study found that RSV and influenza were associated with 51% and 19% of such cases, respectively [2]. This may reflect differences in virologic diagnostic testing performed as well as the recognition of RSV in patients diagnosed with bronchiolitis at admission.
Table 4.
Published Studies of Nonendemic Nosocomial Respiratory Viral Infections
| Authors | Year | Patient Population | Study Design | Viruses Identified | Study Findings |
|---|---|---|---|---|---|
| Mufson et al [25] | 1973 | Pediatric | Prospective surveillance | Parainfluenza 3 | 36 of 197 uninfected contacts acquired infection with parainfluenza 3 during hospital stay |
| Wenzel et al [12] | 1977 | Pediatric | Prospective surveillance | RSV, Parainfluenza type 3, Influenza A/B | 17 nosocomial respiratory viral infections per 100 admissions |
| Valenti et al [5] | 1980 | Adult and Pediatric Patients | Prospective surveillance | RSV, Influenza A, Adenovirus, Parainfluenza, Rhinovirus | 4 and 55 nosocomial respiratory viral infections/10 000 admissions to the adult and pediatric care units, respectively |
| Sims [26] | 1981 | Pediatric | Prospective surveillance | RSV, Influenza A/B, Parainfluenza, Adenovirus, Rhinovirus, Enterovirus | 73 nosocomial respiratory viral infections/10 000 admissions |
| Gagneur et al [27] | 2002 | Pediatric | Prospective surveillance | Human Coronavirus | 11% of patients admitted to the neonatal and pediatric intensive care units developed a nosocomial respiratory viral infection |
| Simon et al [3] | 2006 | Pediatric | Prospective surveillance | RSV | 1 nosocomial respiratory viral infection/1000 patient days |
| Sidler et al [14] | 2012 | Pediatric | Retrospective observation | Adenovirus, Coronoavirus, Human Metapneumovirus, Influenza A/B, Parainfluenza, RSV, Rhinovirus | 1.3 nosocomial respiratory viral infections/1000 patient days |
Abbreviations: RSV, respiratory syncytial virus.
Seventy-nine percent and 81% of our hospital rooms are single occupancy for our adult and pediatric patients, respectively. During the study period, our hospital infection control policy stated that adult and pediatric patients presenting with influenza-like illness should be placed in contact and droplet precautions. However, we realize that influenza-like illness may be insensitive indicator for some respiratory viral infections [15]. Nevertheless, such patients were placed in a private room, or if no private room was available, they were cohorted with patients identified to have the same respiratory virus. Despite this policy, nosocomial respiratory viral infections occurred. This most likely reflects inadequate screening of ill visitors and family or ill healthcare workers reporting for duty despite symptoms of a respiratory viral infection because these have not been stressed in recent educational efforts, and our hospital did not have a formal screening program for visitors and staff. However, based on an educational campaign and compliance monitoring, we believe that transmission of such infections in the hospital setting was less likely to be due to noncompliance with the policy, inadequate decontamination of the inanimate environment, or suboptimal hand hygiene compliance. Our hospital occupational health policy followed the Centers for Disease Control and Prevention guidelines for mitigating risk of influenza transmission from infected healthcare workers to patients that uses fever as a determining factor for which healthcare workers should not have patient contact [16]. However, such guidelines may be inadequate as previously noted [17]. Unfortunately, fever is an insensitive indicator of influenza infection in adult healthcare workers at onset of symptoms when there may be maximal risk of transmission [18, 19]. At least 1 reported influenza outbreak involved healthcare providers who apparently worked with mild illness [20]. Nevertheless, the vast majority of our patients’ nosocomial respiratory viral infections were not due to influenza. Thus, hospital policies and national guidelines should focus on reducing patient risk from all respiratory viruses, not just influenza.
Unfortunately, many community hospitals may not perform testing for respiratory viruses beyond rapid influenza testing. Thus, cases of nosocomial respiratory viral infections are often unrecognized. In addition, healthcare providers may not have a high index of suspicion for such hospital-acquired viral infections. As more hospitals use improved laboratory testing for such viruses, there will be a greater appreciation of the risk of such infections in hospitalized patients, a better understanding of their modes of transmission, and ultimately fewer such cases in the future [21]. Educating healthcare providers regarding the risk they pose to their patients when they are infected with respiratory viruses is vitally important, as well as changes in the culture of healthcare providers by dealing with the guilt they feel when they do not report to work with symptoms of a respiratory viral infection [22].
Our study has several potential limitations. It is unclear whether all of the viruses identified were the cause of active infection, or whether their presence in some cases reflected respiratory tract colonization or recent respiratory viral infection. Although diagnostic testing is recommended in our hospital policy for patients admitted with suspected respiratory viral infections, we do not know the compliance with this policy, and we may have underestimated the incidence of such infections. We also may have missed cases in patients who had symptom onset after hospital discharge. Our data was collected over 1 year on 1 hospital campus in the Northeastern United States, and it may not reflect the risk of such infections in different geographic regions, in hospitals with different patient populations, or those with different infection control and occupational health policies. Finally, the retrospective nature of our study required us to rely on established documentation in the patient’s medical record. Despite these limitations, we hope our findings will lead to a greater awareness of such infections and changes in hospital infection control policies regarding testing of patients with suggestive symptomatology, assessment of visitor restriction policies, and review of sick leave policies to potentially mitigate risk of such infections in future patients.
CONCLUSIONS
We report the second study that comprehensively investigated adult and pediatric patients with nosocomial respiratory viral infections. The first such study [5] involving patients hospitalized from 1977 through 1979 had a very similar incidence of such pediatric and adult infections compared with our findings. That study tested for fewer respiratory viruses than our study; nevertheless, the data suggest that little has changed regarding the risk of such hospital-acquired infections now nearly 40 years later. We hope that our findings will provide additional support for more frequent testing to identify respiratory viruses, beyond influenza, in hospitalized patients with new onset of respiratory symptoms suggestive of possible viral infection to aid in focusing infection control efforts and to stimulate a search for effective therapies and vaccines.
Acknowledgments
We thank Dr. Kenneth Rasinski for assistance in obtaining summary admission data for US hospitals and Susan Simundson for supplying admission data at our institution. We also acknowledge Dr. Kimberle Chapin who has instituted the sophisticated testing methodologies allowing us to diagnose various respiratory viruses at our institution.
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Graman PS, Hall CB. Epidemiology and control of nosocomial viral infections. Infect Dis Clin North Am 1989; 3:815–41. [PubMed] [Google Scholar]
- 2. Spaeder MC, Fackler JC. Hospital-acquired viral infection increases mortality in children with severe viral respiratory infection. Pediatr Crit Care Med 2011; 12:e317–21. [DOI] [PubMed] [Google Scholar]
- 3. Simon A, Khurana K, Wilkesmann A, et al. Nosocomial respiratory syncytial virus infection: impact of prospective surveillance and targeted infection control. Int J Hyg Environ Health 2006; 209:317–24. [DOI] [PubMed] [Google Scholar]
- 4. Micek ST, Chew B, Hampton N, Kollef MH. A case-control study assessing the impact of nonventilated hospital-acquired pneumonia on patient outcomes. Chest 2016; 150:1008–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Valenti WM, Menegus MA, Hall CB, et al. Nosocomial viral infections: I. Epidemiology and significance. Infect Control 1980; 1:33–7. [DOI] [PubMed] [Google Scholar]
- 6. Buettcher M, Heininger U. Prospective surveillance of nosocomial viral infections during and after hospitalization at a university children’s hospital. Pediatr Infect Dis J 2010; 29:950–6. [DOI] [PubMed] [Google Scholar]
- 7. Vaideeswar P, Bavdekar SB, Biswas P, et al. Viral ventilator-associated pneumonia: uncovering tip of the iceberg. Indian J Pathol Microbiol 2011; 54:339–43. [DOI] [PubMed] [Google Scholar]
- 8. Rao S, Nyquist AC. Respiratory viruses and their impact in healthcare. Curr Opin Infect Dis 2014; 27:342–7. [DOI] [PubMed] [Google Scholar]
- 9. Dare RK, Talbot TR. Health care-acquired viral respiratory diseases. Infect Dis Clin North Am 2016; 30:1053–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hong HL, Hong SB, Ko GB, et al. Viral infection is not uncommon in adult patients with severe hospital-acquired pneumonia. PLoS One 2014; 9:e95865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hall CB. Nosocomial viral respiratory infections: perennial weeds on pediatric wards. Am J Med 1981; 70:670–6. [DOI] [PubMed] [Google Scholar]
- 12. Wenzel RP, Deal EC, Hendley JO. Hospital-acquired viral respiratory illness on a pediatric ward. Pediatrics 1977; 60:367–71. [PubMed] [Google Scholar]
- 13. Rahamat-Langendoen JC, Riezebos-Brilman A, Hak E, et al. The significance of rhinovirus detection in hospitalized children: clinical, epidemiological and virological features. Clin Microbiol Infect 2013; 19:E435–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sidler JA, Haberthür C, Dumoulin A, et al. A retrospective analysis of nosocomial viral gastrointestinal and respiratory tract infections. Pediatr Infect Dis J 2012; 31:1233–8. [DOI] [PubMed] [Google Scholar]
- 15. Babcock HM, Merz LR, Fraser VJ. Is influenza an influenza-like illness? Clinical presentation of influenza in hospitalized patients. Infect Control Hosp Epidemiol 2006; 27:266–70. [DOI] [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention. Prevention Strategies for Seasonal Influenza in Healthcare Settings Available at: https://www.cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm Accessed 2 October 2016.
- 17. Mermel LA. Influenza fever restrictions for healthcare workers and pandemic planning: time for reappraisal. Infect Control Hosp Epidemiol 2015; 36:1248. [DOI] [PubMed] [Google Scholar]
- 18. Ridgway JP, Bartlett AH, Garcia-Houchins S, et al. Influenza among afebrile and vaccinated healthcare workers. Clin Infect Dis 2015; 60:1591–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lau LL, Cowling BJ, Fang VJ, et al. Viral shedding and clinical illness in naturally acquired influenza virus infections. J Infect Dis 2010; 201:1509–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Magill SS, Black SR, Wise ME, et al. Investigation of an outbreak of 2009 pandemic influenza A virus (H1N1) infections among healthcare personnel in a Chicago hospital. Infect Control Hosp Epidemiol 2011; 32:611– 5. [DOI] [PubMed] [Google Scholar]
- 21. Ginocchio CC, McAdam AJ. Current best practices for respiratory virus testing. J Clin Microbiol 2011; 49:S44–S8. [Google Scholar]
- 22. Tanksley AL, Wolfson RK, Arora VM. Changing the “working while sick” culture: promoting fitness for duty in health care. JAMA 2016; 315:603–4. [DOI] [PubMed] [Google Scholar]
- 23. Lessler J, Reich NG, Brookmeyer R, et al. Incubation periods of acute respiratory viral infections: a systematic review. Lancet Infect Dis 2009; 9:291–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Haas LE, de Rijk NX, Thijsen SF. Human metapneumovirus infections on the ICU: a report of three cases. Ann Intensive Care 2012; 2:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mufson MA, Mocega HE, Krause HE. Acquisition of parainfluenza 3 virus infection by hospitalized children. I. Frequencies, rates, and temporal data. J Infect Dis 1973; 128:141–7. [DOI] [PubMed] [Google Scholar]
- 26. Sims DG. A two year prospective study of hospital-acquired respiratory virus infection on paediatric wards. J Hyg (Lond) 1981; 86:335–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gagneur A, Sizun J, Vallet S, et al. Coronavirus-related nosocomial viral respiratory infections in a neonatal and paediatric intensive care unit: a prospective study. J Hosp Infect 2002; 51:59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]