Abstract
Background
Inappropriate antimicrobial use can threaten patient safety and is the focus of collaborative physician and pharmacist antimicrobial stewardship teams. However, antimicrobial stewardship is not comprehensively taught in medical or pharmacy school curricula. Addressing this deficiency can teach an important concept as well as model interprofessional healthcare.
Methods
We created an antimicrobial stewardship curriculum consisting of an online learning module and workshop session that combined medical and pharmacy students, with faculty from both professions. Learners worked through interactive, branched-logic clinical cases relating to appropriate antimicrobial use. We surveyed participants before and after the curriculum using validated questions to assess knowledge and attitudes regarding antimicrobial stewardship and interprofessional collaboration. Results were analyzed using paired χ2 and t tests and mixed-effects logistic regression.
Results
Analysis was performed with the 745 students (425 medical students, 320 pharmacy students) who completed both pre- and postcurriculum surveys over 3 years. After completing the curriculum, significantly more students perceived that they were able to describe the role of each profession in appropriate antimicrobial use (34% vs 82%, P < .001), communicate in a manner that engaged the interprofessional team (75% vs 94%, P < .001), and describe collaborative approaches to appropriate antimicrobial use (49% vs 92%, P < .001). Student favorability ratings were high for the online learning module (85%) and small group workshop (93%).
Conclusions
A curriculum on antimicrobial stewardship consisting of independent learning and an interprofessional workshop significantly increased knowledge and attitudes towards collaborative antimicrobial stewardship among preclinical medical and pharmacy students.
Keywords: antimicrobial stewardship, education, interprofessional, undergraduate medical education
Inappropriate use of antimicrobials is linked to the emergence of multidrug-resistant pathogens and adverse effects in patients [1]. Antimicrobial stewardship programs, directed at reducing the inappropriate use of antimicrobials, are becoming mandated in US healthcare systems [2]. Although education of clinicians is considered to be an essential element of any program designed to influence prescribing behavior [3], there has been less attention paid to teaching predoctoral students the principles of appropriate antimicrobial use, particularly early in training [4]. A survey of preclinical medical student microbiology curricula reported that only 65% of schools are teaching antimicrobial stewardship during their courses [5]. Ninety percent of 317 senior medical students and 89% of 579 graduating pharmacy students reported that they would like more education on responsible use of antimicrobials [6, 7]. However, the Infectious Diseases Society of America’s position statement, “Stewardship Commitments for the White House Forum on Antibiotic Stewardship” published in 2015 did not include education of health professional students as one of its commitments [8].
Research on antimicrobial prescribing practices by physician trainees indicates that norms around “prescribing etiquette” can interfere with the optimization of antimicrobial therapy as well as a disconnect between microbiology coursework and the practical challenges of antimicrobial prescribing [9–11]. Early introduction of core concepts of antimicrobial stewardship might normalize the idea of appropriate antimicrobial use as a shared responsibility and increase the acceptance of stewardship interventions. An interprofessional approach to stewardship is recommended by multiple professional and governmental organizations as an essential feature of a successful antimicrobial stewardship program [3, 12]. Because antimicrobial stewardship is explicitly an interprofessional activity, educating students about stewardship in an interprofessional environment can provide a more authentic simulation of practice. Moreover, standards in medical and pharmacy undergraduate education emphasize the importance of early interprofessional experiences [13–15].
We aimed to address these deficiencies in the literature by (1) developing and implementing a joint interprofessional curriculum in 2 professional schools to enable early learners to appreciate the importance of rational antimicrobial use as healthcare professionals and (2) determining the effect of this activity on knowledge and attitudes towards interprofessional healthcare teams. We hypothesized that an interprofessional curriculum that models an authentic work experience can be successfully implemented and developed in preclinical undergraduate medical and pharmacy education.
METHODS
Design and Setting
The learning objectives for the curriculum were developed by 1 infectious diseases specialist pharmacist (C. M.) and 2 infectious diseases physicians (B. S. S., P. V. C.-H.) after a focused needs assessment and review of the relevant literature [16]. The study took place during the 2013–2014, 2014–2015, and 2015–2016 academic years at the University of California, San Francisco (UCSF). The study was granted exempt review status from the UCSF Institutional Review Board.
Curriculum
Participants of the curriculum were second-year medical students and third-year pharmacy students at UCSF. The curriculum was embedded into the courses they were taking on microbiology and infectious diseases (medical students) or antimicrobial pharmacology (pharmacy students). Attendance at the interprofessional workshop was a course expectation; students were offered a small amount of bonus credit for completing the pre- and postworkshop surveys.
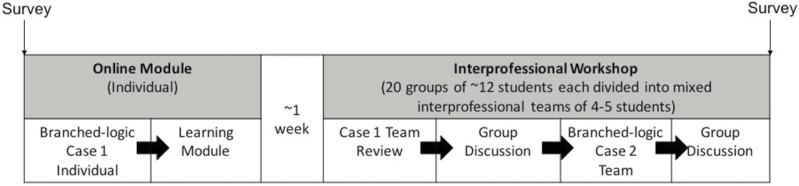
The curriculum (Figure 1) was designed as follows and delivered through the Moodle learning management system (Moodle Pty Ltd, Perth, Australia): (1) students viewed a case vignette online (Case 1) and answered related clinical questions; (2) an online independent learning module on antimicrobial stewardship was subsequently provided; then, (3) approximately 1 week later, the students participated in a 2-hour workshop on antimicrobial stewardship. The curriculum, including learning objectives, learning module, interactive case vignettes, and instructor materials, are freely available for access at the following site: http://tiny.ucsf.edu/stewardship. The workshops were led by a physician or pharmacist with expertise in antimicrobial use and consisted of approximately 12 students. Students were subdivided into mixed-professions small groups of 4–5 students. In small groups, students revisited Case 1 from the online module and came to a consensus group answer, which was then discussed with the larger group. The small groups then worked through Case 2 together again followed by group discussion. The cases used a branched-logic format: the decisions students made in the initial stages of the case determined the subsequent choices and case outcomes. The decisions required in the cases reflected key considerations in antimicrobial stewardship: whether to initiate treatment, impact of patient allergies and drug interactions on antimicrobial selection, adequacy of empiric spectrum of activity, and de-escalation of therapy based on culture results.
Figure 1.
Schematic of antimicrobial stewardship curriculum.
Assessment
Each student completed a survey of knowledge and attitudes towards antimicrobial use, antimicrobial resistance, and interprofessional practice before and after participation in the curriculum; the after survey included 2 additional items asking for them to rate the value of the experience (Figure 1). The survey instrument consisted of 19 Likert scale items asking for the level of agreement with statements related to antimicrobial use and resistance and interprofessional collaboration. The items related to antimicrobial use were adapted from a survey of physician attitudes toward antimicrobial prescribing and resistance [17]. The items related to interprofessional collaboration were adapted from a validated survey of attitudes towards interprofessional learning and interaction [18]. For purposes of primary analysis, the data were dichotomized into answers of “agree/strongly agree” versus “neutral/disagree/strongly disagree”.
Analysis
Analysis of changes in student attitudes before and after the survey was performed using McNemar’s test or the paired t test to account for the paired nature of the data. Interaction between study year and student profession with prepost survey changes were explored using mixed-effects logistic regression models. All analyses were performed with Stata SE software (version 13; StataCorp, College Station, TX).
RESULTS
A total of 822 students participated over the 3 study years (470 medical students, 352 pharmacy students); of these, 745 (91%) completed both pre- and postcurriculum surveys. Statistical analysis was performed on these 745 participants (425 medical students, 320 pharmacy students). The survey results are displayed in Table 1; results were similar across study years and thus pooled results are presented. The first 5 questions concerned perceptions of antimicrobial use and resistance. Attitudes were not significantly different between pre- and postsurvey answers, with the exception of the perception of patient demand being the major reason physicians prescribe unnecessary antibiotics, which increased (42.2% to 59.1%, P < .001). There was no evidence of interaction between profession and changes in attitudes.
Table 1.
Survey Responses Before and After Stewardship Curriculum
| Question | %Agree/Strongly Agree (n/N) | ||
|---|---|---|---|
| Precurriculum | Postcurriculum | P Valuea | |
| Knowledge and attitudes about antibiotic resistance | |||
| Antibiotic resistance is a major public health problem | 99.1 (763 of 770) | 99.2 (738 of 744) | .76 |
| Overprescribing of antibiotics is a major cause of antibiotic resistance | 95.7 (736 of 769) | 98.9 (735 of 743) | .002 |
| Physicians should only consider the needs of the individual patient when prescribing antibiotics | 26.0 (200 of 769) | 27.8 (206 of 742) | .19 |
| I am confident the development of new and effective drugs will keep pace with the growing rate of antibiotic resistance | 14.7 (113 of 770) | 18.7 (139 of 744) | .02 |
| Patient demand is the major reason that physicians prescribe unnecessary antibiotics | 39.8 (306 of 769) | 54.1 (402 of 743) | <.001 |
| Perceived efficacy in interprofessional collaboration | |||
| I am able to describe the role of each profession in appropriate antibiotic useb | 34.2 (263 of 769) | 82.4 (613 of 744) | <.001 |
| I can communicate in a manner that engages the interprofessional team | 75.4 (580 of 769) | 94.4 (702 of 744) | <.001 |
| I can describe collaborative approaches to appropriate antibiotic usec | 48.6 (374 of 769) | 92.2 (435 of 741) | <.001 |
| Attitudes towards interprofessional learning and collaboration | |||
| My skills in communicating with patients of clients would be improved through learning with students from other healthcare professions | 84.4 (648 of 768) | 91.9 (685 of 744) | <.001 |
| My skills in communicating with other healthcare professionals would be improved through learning with students from other healthcare professions | 89.7 (689 of 768) | 94.2 (699 of 742) | <.001 |
| I would prefer to learn only with peers from my own profession | 5.1 (39 of 770) | 8.9 (67 of 744) | .005 |
| Learning with students from other healthcare professions is likely to facilitate subsequent working professional relationships | 83.2 (637 of 766) | 91.4 (681 of 745) | <.001 |
| Learning with students from other healthcare professions would be more beneficial to improving my teamwork skills than learning only with my peers | 80.6 (620 of 769) | 90.2 (672 of 745) | <.001 |
| Collaborative learning would be a positive learning experience for all healthcare students | 86.1 (661 of 768) | 92.7 (690 of 744) | <.001 |
| Learning with students from other healthcare professions is likely to help to overcome stereotypes that are held about the different professions | 79.5 (611 of 769) | 88.5 (659 of 745) | <.001 |
| I would enjoy the opportunity to learn with students from other healthcare professions | 83.5 (643 of 770) | 91.5 (681 of 744) | <.001 |
| Learning with students from other healthcare professions is likely to improve the service for patient of client | 86.5 (665 of 769) | 92.9 (692 of 745) | <.001 |
a P value is based on McNemar’s test for students with paired data.
b P = .03 for interaction between student profession and paired change in response; medical students increased agreement to a greater extent than pharmacy students.
c P = .03 for interaction between student profession and paired change in response; medical students increased agreement to a greater extent than pharmacy students.
Three questions asked about students’ self-perceived efficacy in interprofessional collaboration; for all of these items, there were significant increases in students’ perceived abilities. In the preworkshop survey, less than half as many medical students as pharmacy students believed they could describe the role of other professions in appropriate antibiotic use (22.1% vs 58.1%). Both groups increased in their self-reported abilities on this question in the postsurvey (to 78.1% for medical students and to 87.9% for pharmacy students), with a greater increase seen in medical students (P = .03 for interaction). Medical students also had a greater increase in their ability to describe collaborative approaches to appropriate antibiotic use (40.4% to 90.9%) compared with pharmacy students (59.8% to 92.8%, P = .03 for interaction).
Among the 9 questions primarily concerned with attitudes towards interprofessional learning and collaboration, students generally expressed more favorable attitudes towards interprofessional learning and collaboration. Despite the overall favorable attitudes, the percentage of students who agreed or strongly agreed that they would prefer learning from peers from their own profession increased overall by 3.8% (P = .005); there was no evidence of interaction by student profession by this measure. Unlike the other survey items related to interprofessionalism, a rating of “Strongly Agree” represented a less favorable attitude towards interprofessional collaboration, so it is possible that this finding is an artifact of the reversal of the scale [19].
On the postcurriculum questionnaire, 84.5% (616 of 729) of students agreed or strongly agreed that completing the online learning module was a valuable learning experience, and 92.7% (676 of 729) belived that the small group workshop was a valuable learning experience. Workshop favorability ratings were high across all student-preceptor pairs, ranging from 86.7% for medical students with pharmacist preceptors to 96.3% for pharmacy students with physician preceptors. Invited open-ended student comments were highly favorable; common themes were the authenticity of the scenarios relative to other interprofessional education exercises and the recognition of the complementary knowledge that medical and pharmacy students each brought to bear on the problems. Some students believed that pharmacy students were disadvantaged because they had not yet completed their instruction in infectious diseases, whereas the medical students had.
DISCUSSION
We demonstrated that an interprofessional curriculum on antimicrobial stewardship, including medical and pharmacy students, can positively impact knowledge and attitudes towards both antimicrobial stewardship and interprofessional collaboration. Given the emphasis placed on antimicrobial stewardship as a key public health strategy [20], interventions that can raise awareness of stewardship and improve health professional teamwork in this area may carry a significant impact. The curriculum was also well received by learners from both professions regardless of the profession of their workshop leader.
Several studies have identified deficiencies in knowledge and behaviors of health professions trainees in antimicrobial use [6, 7, 21–23], leading some authors and organizations to recommend a greater focus on these topics in the undergraduate curriculum [8, 24, 25]. Equally important to improving knowledge is being able to apply it in the clinical environment, which requires an understanding of each clinician’s role in appropriate antimicrobial use. Some components of antimicrobial stewardship are taught in a majority of United States and United Kingdom medical and pharmacy schools [5, 26, 27]. However, content delivery is largely lecture-driven, only a minority of schools covered all recommended stewardship principles, and few programs offer opportunities for interprofessional education in stewardship. The current study suggests that an interprofessional curriculum on stewardship where students collaborate on authentic case simulations can substantially improve students’ knowledge of and comfort with their roles in and knowledge of antimicrobial stewardship.
This was a single-center study at an institution with medical and pharmacy undergraduate schools at the same campus, which enabled us to recruit a large number of physician and pharmacist workshop leaders. We recognize that some medical and pharmacy schools are not geographically accessible to each other to engage in this type of learning activity. However, because interprofessional educational experiences are mandated by the accrediting bodies for medicine [14] and pharmacy [15], there is strong pressure for creative solutions to expand the interprofessional education space. We encourage schools to identify ways to have medical students to interact with pharmacists involved in stewardship programs and for pharmacy students to be partnered with physicians involved in stewardship programs. At minimum, during the preclinical years when stewardship concepts are being introduced, it would be ideal to invite a colleague from the other discipline to be serve as a coleader of these sessions, to highlight the importance of interprofessional collaboration in stewardship. Given that a portion of this curriculum was delivered through an online learning platform, distance collaboration may be another method to involve learners from different professions.
Learner knowledge of antimicrobial stewardship concepts was assessed by a small number of survey items. This was driven by a limited number of available survey instruments in the literature related to antimicrobial stewardship appropriate to undergraduate health professions population and by a desire to limit the overall length of the survey to improve response rates. Future implementations of the curriculum will include a more robust assessment of antimicrobial stewardship knowledge.
CONCLUSIONS
This study adds to the limited literature available on antimicrobial stewardship education for undergraduate health professionals, and, to the best of our knowledge, it is the only study of an intervention targeting these learners. We hope that our curriculum can serve as an exemplar for both stewardship and interprofessional education activities at other institutions.
Acknowledgments
We acknowledge Linda Brinen for assistance in implementation of the curriculum and the faculty of the University of California, San Francisco (UCSF) Teaching Scholars Program for feedback on the project proposal.
Finanical support.
This study was supported by a grant from the UCSF Center for Innovation in Interprofessional Education and the UCSF Gold-Headed Cane Endowed Teaching Chair in Internal Medicine.
Potential conflicts of interest.
All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Tamma PD, Cosgrove SE. Antimicrobial stewardship. Infect Dis Clin North Am 2011; 25:245–60. [DOI] [PubMed] [Google Scholar]
- 2. Johnson LS, MacDougall C, Trivedi KK. The legislative momentum of antimicrobial stewardship: the US perspective. Curr Treat Options Infect Dis 2016; 8:93–101. [Google Scholar]
- 3. Dellit TH, Owens RC, McGowan JE, Jr, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for developing an institutional program to enhance antimicrobial stewardship. Clin Infect Dis 2007; 44:159–77. [DOI] [PubMed] [Google Scholar]
- 4. Luther VP, Ohl CA, Hicks LA. Antimicrobial stewardship education for medical students. Clin Infect Dis 2013; 57:1366. [DOI] [PubMed] [Google Scholar]
- 5. Melber DJ, Teherani A, Schwartz BS. A comprehensive survey of preclinical microbiology curricula among US medical schools. Clin Infect Dis 2016; 63:164–8. [DOI] [PubMed] [Google Scholar]
- 6. Abbo LM, Cosgrove SE, Pottinger PS, et al. Medical students’ perceptions and knowledge about antimicrobial stewardship: how are we educating our future prescribers? Clin Infect Dis 2013; 57:631–8. [DOI] [PubMed] [Google Scholar]
- 7. Justo JA, Gauthier TP, Scheetz MH, et al. Knowledge and attitudes of doctor of pharmacy students regarding the appropriate use of antimicrobials. Clin Infect Dis 2014; 59(Suppl 3):S162–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Schwartz BS, Armstrong WS, Ohl CA, Luther VP. Create allies, IDSA stewardship commitments should prioritize health professions learners. Clin Infect Dis 2015; 61:1626–7. [DOI] [PubMed] [Google Scholar]
- 9. Charani E, Castro-Sanchez E, Sevdalis N, et al. Understanding the determinants of antimicrobial prescribing within hospitals: the role of “prescribing etiquette”. Clin Infect Dis 2013; 57:188–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mattick K, Kelly N, Rees C. A window into the lives of junior doctors: narrative interviews exploring antimicrobial prescribing experiences. J Antimicrob Chemother 2014; 69:2274–83. [DOI] [PubMed] [Google Scholar]
- 11. De Souza V, MacFarlane A, Murphy AW, et al. A qualitative study of factors influencing antimicrobial prescribing by non-consultant hospital doctors. J Antimicrob Chemother 2006; 58:840–3. [DOI] [PubMed] [Google Scholar]
- 12. Barlam TF, Cosgrove SE, Abbo LM, et al. Implementing an antibiotic stewardship program: guidelines by the infectious diseases society of america and the society for healthcare epidemiology of america. Clin Infect Dis 2016; 62:e51–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: Report of an expert panel 2011. Available at: https://ipecollaborative.org/uploads/IPEC-2016-Updated-Core-Competencies-Report__final_release_.PDF. Accessed 14 November 2016.
- 14. Liason Committee on Medical Education. Functions and structure of a medical school Available at: www.lcme.org Accessed 13 June 2016.
- 15. Accreditation Council on Pharmacy Education. Accrediation standards and key elements for the professional program in pharmacy leading to the Doctor of Pharmacy degree Available at: https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf Accessed 13 June 2016.
- 16. Thomas PA, Kern DE, Hughes MT, Chen BY. (eds). Curriculum Development for MedicalEducation: A Six-Step Approach. 3rd Edition Baltimore, MD: Johns Hopkins University Press; 2016. [Google Scholar]
- 17. Metlay JP, Shea JA, Crossette LB, Asch DA. Tensions in antibiotic prescribing: pitting social concerns against the interests of individual patients. J Gen Intern Med 2002; 17:87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pollard K, Miers ME, Gilchrist M. Second year scepticism: pre-qualifying health and social care students’ midpoint self-assessment, attitudes and perceptions concerning interprofessional learning and working. J Interprof Care 2005; 19:251–68. [DOI] [PubMed] [Google Scholar]
- 19. Hughes GD. The impact of incorrect responses to reverse-coded survey items. Research in the Schools 2009; 16:76–88. Available at: http://www.msera.org/publications-rits.html. [Google Scholar]
- 20. Presidential Advisory Council on Combating Antibiotic-Resistant Bacteria. National strategy for combating antibiotic-resistant bacteria Available at: https://www.whitehouse.gov/sites/default/files/docs/carb_national_strategy.pdf Accessed 13 June 2016.
- 21. Dyar OJ, Pulcini C, Howard P, et al. European medical students: a first multicentre study of knowledge, attitudes and perceptions of antibiotic prescribing and antibiotic resistance. J Antimicrob Chemother 2014; 69:842–6. [DOI] [PubMed] [Google Scholar]
- 22. Srinivasan A, Song X, Richards A, et al. A survey of knowledge, attitudes, and beliefs of house staff physicians from various specialties concerning antimicrobial use and resistance. Arch Intern Med 2004; 164:1451–6. [DOI] [PubMed] [Google Scholar]
- 23. Minen MT, Duquaine D, Marx MA, Weiss D. A survey of knowledge, attitudes, and beliefs of medical students concerning antimicrobial use and resistance. Microb Drug Resist 2010; 16:285–9. [DOI] [PubMed] [Google Scholar]
- 24. Davenport LA, Davey PG, Ker JS; BSAC Undergraduate Education Working Party An outcome-based approach for teaching prudent antimicrobial prescribing to undergraduate medical students: report of a Working Party of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother 2005; 56:196–203. [DOI] [PubMed] [Google Scholar]
- 25. Ohl CA, Luther VP. Health care provider education as a tool to enhance antibiotic stewardship practices. Infect Dis Clin North Am 2014; 28:177–93. [DOI] [PubMed] [Google Scholar]
- 26. Castro-Sánchez E, Drumright LN, Gharbi M, et al. Mapping antimicrobial stewardship in undergraduate medical, dental, pharmacy, nursing and veterinary education in the United Kingdom. PLoS One 2016; 11:e0150056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Prescott W, Jr, Stuczynski L, Dahl E, et al. Infectious disease education across US pharmacy schools: what is being taught and how? In: 115th Meeting of the American College of Clinical Pharmacy, Galveston, TX: July 26–30, 2014. Abstract #73. [Google Scholar]