Abstract
Background:
This study aimed to determine the prevalence of nonalcoholic fatty liver disease (NAFLD) and its related risk factors among the general population of Isfahan city located in the central part of Iran.
Materials and Methods:
In this cross-sectional study, the prevalence of NAFLD among 483 general adult populations was determined using ultrasonography. Anthropometric and biochemical variables were compared in groups with and without NAFLD and their predictive value for occurrence of NAFLD was investigated also.
Results:
Prevalence of NAFLD was 39.3%. Frequency of focal fatty infiltration (FFI), Grade I, Grade II, and Grade III of NAFLD was 9.5%, 21.1%, 7.2%, 1.4%, respectively. Prevalence of different types of NAFLD and FFI, was not different between female and male participants (P = 0.238). Ordinal regression was determined that all of the studied variables have significant predictive value for NAFLD (P < 0.001, γ = 0.615). Spearman correlation indicated that there was a significant relationship between NAFLD and BMI (r = 0.37, P < 0.001), age (r = 0.15, P = 0.001), FBS (r = 0.20, P < 0.001), cholesterol (r = 0.19, P < 0.001), triglyceride (r = 0.20, P < 0.001), LDL (r = 0.16, P < 0.001), AST (r = 0.17, P < 0.001), and ALT (r = 0.31, P < 0.001).
Conclusions:
Considering the high prevalence of NAFLD specially its lower grades among Isfahani adult general population and their association with studied variables, it seems that interventional studies which target-related mentioned risk factors could reduce the overall occurrence of NAFLD.
Keywords: Iran, metabolic, nonalcoholic fatty liver disease, prevalence, risk factors
Introduction
Deposition of lipid in hepatocytes exceeding more than 5% of total liver weight in the absence of other etiologies of hepatic damages is defined as nonalcoholic fatty liver disease (NAFLD).[1] It is used for a wide spectrum of hepatic disease ranging from simple nonevaluative steatosis to progressive nonalcoholic steatohepatitis and finally lethal cirrhosis.[2]
Epidemiological studies have identified NAFLD as an emerging health problem worldwide due to its dramatically increasing rate during the last decades because of both lifestyle modification and also higher detection rate.[3,4] The rate for NAFLD in Western and Asian countries has reported to be 15%–40% and 9%–40%, respectively.[5,6] Prevalence of NAFLD in Iran has been reported to be 2.9%–7.1% in the general population.[7,8]
Although many studies have investigated the underlying factors responsible for NAFLD and many factors have been identified, the exact pathogenesis of this multifactorial disease is not fully understood. Accordingly, insulin resistance (IR), oxidative stress, diabetes, hyperlipidemia, obesity, and metabolic syndrome are considered as its important risk factors.[9,10]
The link between NAFLD and metabolic syndrome, diabetes, and cardiovascular disease (CVD) has been demonstrated in many studies.[11,12,13] One-third of participants with NAFLD fulfill the complete diagnostic criteria of metabolic syndrome and 90% of them have at least one of its components.[14] Moreover, it is associated with higher risk of CVD and its related mortality and morbidity.[15] Thus, like other chronic diseases, the cost of NAFLD for both patients and the health-care system is high.
There is no definite and effective treatment for NAFLD, and the management process of the disease is mainly based on ameliorating its related metabolic risk factors. Prevention and treatment strategies of the disease are similar.[16]
Many studies worldwide have indicated that variability in lifestyle and eating habits in different regions as well as differences in genetic and ethnicity resulted in disparities in the characteristics and features of NAFLD disease in different populations and geographical regions.[12,17] There is great variability in socioeconomic, environmental, ethnical, and genetic condition of the Iranian population. Hence, considering the importance of epidemiologic feature of the disease for implementing proper preventative strategies and interventional trials, this study aimed to determine the prevalence of NAFLD and its related risk factors and their predictive values among the general population of Isfahan city located in the central part of Iran.
Materials and Methods
This study was designed as a cross-sectional study in Isfahan city, during a 6-month period from September 2013 to March 2014. Studied population was selected by systematic clustering random sampling method according to the data obtained from family registry of twenty health-care centers in Isfahan city. Enrolled population aged 30–60 years and was invited to participate in the study. Written informed consent was obtained from each participant after explaining the goal and details of the method of the study.
The protocol of the study was approved by the Regional Ethics Committee of the Isfahan University of Medical Sciences.
Individuals with history of liver, kidney, thyroid, heart disease, any malignancy, chemotherapy, and alcohol consumption, pregnant women, or those who had delivered within the past 6 months, abnormal copper metabolism, and history of any medication with hepatic metabolism were not included in the study. Those who did not cooperate properly were also excluded from the study.
Demographic information of the finally selected individuals was obtained using a questionnaire. They asked to refer to selected laboratory for biochemical measurements after overnight fasting. Biochemical measurements include fasting blood glucose (FBS), lipid profile (cholesterol, triglyceride (TG), low-density lipoprotein cholesterol [LDL-C], high-density lipoprotein cholesterol [HDL-C]), and liver enzymes (alanine aminotransferase [ALT], aspartate aminotransferase [AST], and alkaline phosphatase [ALP]). All participants examined physically by a physician and referred to a radiologist (SHM) for evaluating NAFLD by abdominal ultrasonography. The anthropometrics and biochemical and liver enzymes levels were compared in patients with and without NAFLD.
Physical examination
Height and weight were measured in their light clothing and barefoot using Seca scale by a trained nurse. Body mass index (BMI) was calculated as weight divided by square of height (kg/m2).
Biochemical measurements
Venous blood sample was obtained from each participant after 10–12 h fasting for measurement of blood glucose and serum lipids (total cholesterol, LDL-C, HDL-C, and TG). Blood glucose and serum lipids levels were measured by enzymatic kits (Pars Azmoon, Tehran, Iran). Liver enzymes measured using Auto Analyzer Alpha Classic (Tehran, Iran) and Pars Azmoon reagent kits (Tehran, Iran).
Ultrasonographic assessment
Transabdominal ultrasonography was performed in all participants after 8–12 h fasting in the supine and 60° left lateral positions during quiet inspiration.
NAFLD was diagnosed by means of transabdominal ultrasonography using a 3.5 MHz transducer (Siemens SONOLINE G50-Germany) by a trained and expert radiologist (SHM). Diagnosis of NAFLD was based on bright hepatic echogenicity with a diffused increase of liver echogenicity blurring of the intrahepatic vessels and diaphragm and with evidence of contrast between the liver and kidney.
The severity of NAFLD was classified as follows: normal (without any fatty infiltration and normal liver echogenicity), focal fatty infiltration (FFI), Grade I (mild infiltration with normal visualization of the diaphragm and the intrahepatic vessel borders), Grade II (moderate infiltration with slightly impaired visualization of the diaphragm and the intrahepatic vessel borders), and Grade III (severe infiltration with poor visualization of the diaphragm and the intrahepatic vessel borders and posterior portion of the right lobe).[18]
Statistical analysis
Obtained data were analyzed using SPSS version 20 software (SPSS Inc., Chicago, IL, USA). Continuous variables were reported as mean ± standard deviation (SD) and frequencies for categorical variables reported as n (%). Mentioned variables were compared in participants with and without NAFLD using Chi-square test, one-way ANOVA, and t-test for qualitative and quantitative variables. The relationship between continuous variables and NAFLD was examined using Spearman correlation analysis. Multiple logistic regression adjusted for confounders was used for evaluating the relation between anthropometric and biochemical variables with NAFLD.
Ordinal regression was used to determine the predictive value of studied variable for NAFLD and its severity.
Results
Overall, 483 participants (291 female and 192 males) with mean age of 45.53 ± 8.92 years were studied. NAFLD was diagnosed in 190 (39.3%) of participants. Frequency of different grades of NAFLD was 46 (9.5%), 102 (21.1%), 35 (7.2%), 7 (1.4%) for FFI, Grade I, Grade II, and Grade III, respectively. Frequency of different grades of NAFLD according to sex groups is presented in Figure 1. Prevalence of overall NAFLD was 41.1% and 38.1% in male and female, respectively. There were no significant differences between female and male participants regarding the prevalence of different types of NAFLD, FFI, and normal groups (P = 0.238).
Figure 1.
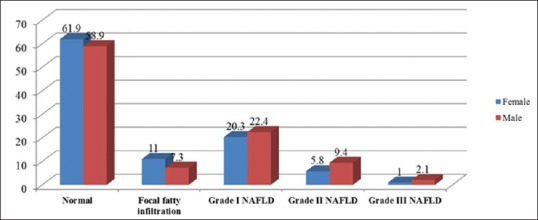
Frequency of different grades of nonalcoholic fatty liver disease according to sex groups among adult general population in Isfahan
Mean ± SD of anthropometrics and metabolic variables in participants with normal liver ultrasonography and those with different grades of NAFLD is presented in Table 1.
Table 1.
Mean±standard deviation of anthropometrics and metabolic variables in participants with normal liver ultrasonography and those with different grade of nonalcoholic fatty liver disease among adult general population in Isfahan
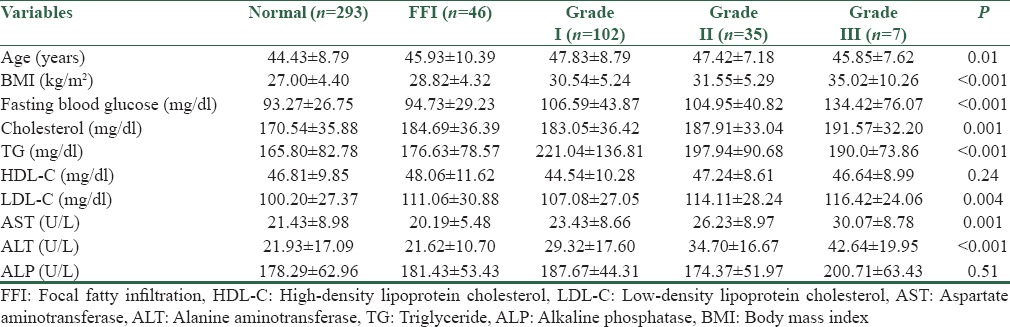
Spearman correlation indicated that there was a significant relationship between NAFLD and BMI (r = 0.37, P < 0.001), age (r = 0.15, P = 0.001), FBS (r = 0.20, P < 0.001), cholesterol (r = 0.19, P < 0.001), TG (r = 0.20, P < 0.001), LDL-C (r = 0.16, P < 0.001), AST (r = 0.17, P < 0.001), and ALT (r = 0.31, P < 0.001).
Odds ratio for participants having NAFLD for different anthropometrics and biochemical variables is presented in Table 2.
Table 2.
Odds ratio for having nonalcoholic fatty liver disease for different anthropometrics and biochemical variables among adult general population in Isfahan
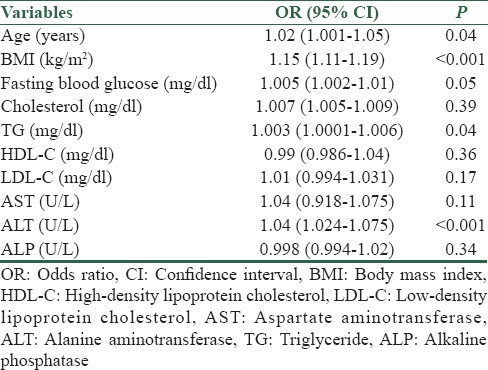
Ordinal regression was determined that all of the studied variables have significant predictive value for NAFLD (P < 0.001, γ = 0.615).
Discussion
In this study, we demonstrated the prevalence of NAFLD among adult Isfahani general population. Our results indicated that this metabolic disorder is considered as a common problem among our studied population. The most common form of NAFLD according to its classification was Grade I, followed by FFI. All of the studied variables have the ability to predict the occurrence of NAFLD, but the association was more significant for age, BMI, serum glutamate-pyruvate transaminase, FBS, and TG.
In this study, NAFLD was diagnosed using ultrasonography. Although the gold standard for diagnosing of NAFLD is magnetic resonance imaging,[19] many studies have suggested that ultrasonography is a cost-effective, useful, safe, noninvasive, and widely available method for diagnosis and follow-up of patients with NAFLD, especially in epidemiological studies.[20,21] Hence, in this study, we used this assay for diagnosis of NAFLD and for improving its accuracy a single radiologist had performed the procedure.
The reported prevalence rate of ultrasonographically diagnosed NAFLD in different studies and regions had a wide range of variability. The reported range of NAFLD varies from 20% to 60% in developed countries and from 1% to 30% in developing and Asian countries.[22,23] Prevalence of NAFLD has reported to be 34%, 21.8%, 10%, and 24.3% in the United States, Japan, China, and South Korea, respectively.[23,24,25,26] Several studies have demonstrated the prevalence of NAFLD in different groups of the Iranian population. The range was from 2.9% by Rogha et al. to 43.8% in a substudy from Amol cohort health study by Amirkalali et al.[27,28,29]
In this study, the rate was 39.3%. The differences in the reported rate of NAFLD in various studies may be due to differences in genetic, environmental, and lifestyle methods of studied population as well as definition and diagnostic methods of NAFLD in different ethnic and geographical regions. Moreover, the ultrasonographic diagnostic patterns of NAFLD based on the presence of a “bright” liver, with stronger echoes in the hepatic parenchyma than in the renal parenchyma, often associated with unusually fine liver texture and vessel blurring, in the absence of findings suggestive of other chronic liver diseases.
Our results were in accordance with those reported in the north of Iran and Shiraz.[28,29] Amirkalali et al. reported a high prevalence rate of NAFLD (43.8%) among adults population in the north of Iran. They suggested that the higher reported rate may be due to the high prevalence rate of metabolic syndrome in Iranian population. Previous studies have been reported that Iran has one of the highest prevalences of metabolic syndrome worldwide.[29,30] We did not evaluate the presence of metabolic syndrome in our studied population, but it possibly could be one explanation for obtained high prevalence rate of NAFLD.
In this study, FFI was included as NAFLD. It seems that our results and epidemiologic features of the disease are similar to that reported in Shiraz (21.5%).[28] They did not report FFI as NAFLD and this could explain their reported lower rate.
Sex differences in the prevalence of NAFLD have been reported differently in many studies. Some reported higher rate of the disease among men, whereas others reported the higher rate for women.[6,31,32]
It is suggested that the higher rate of NAFLD in men may be generally due to higher abdominal visceral fat mass in men.[33] The higher rate among postmenopause women may vary due to the menopausal status and lack of physical exercise in this period.[34] Therefore, we could conclude that NAFLD is an important health problem for men and postmenopausal women. In this study, there was no significant difference in the prevalence of NAFLD between men and women. It is recommended to perform more detailed analysis regarding the sex distribution of the disease and their risk factors.
The association between NAFLD and metabolic, anthropometrics factors and liver enzymes has been reported in several studies. Although the results were controversial in different studies regarding the association of the mentioned factors in different populations, the final concept is that NAFLD is considered as a metabolic disorder and it is associated with metabolic syndrome and any preventative intervention for preventing metabolic syndrome could be effective in preventing of NAFLD. Determining the mentioned association in each region separately would be more effective for planning our future prevention strategies; hence, in this study, we investigated the mentioned association and the predictive value of studied variables for occurrence of NAFLD.
In a study in Taiwan among 1016 healthy police population, the prevalence of NAFLD was reported to be 52.2%. They indicated that male gender, older age, higher BMI, higher ALT, presence of hyperuricemia, hypercholesterolemia, and hypertriglyceridemia were the significant factors associated with NAFLD.[35]
In a study in Japan among 5075 participants, Eguchi et al. have reported that the overall prevalence of NAFLD was 29.7%. There was a significant three-fold difference in the mean prevalence between males (41.0%) and females (17.7%). This prevalence showed a linear increase with BMI, TGs, and LDL-C regardless of threshold values, even without obesity.[36]
There was also similar study in this field from Taiwan, Israel, and Korea.[37,38,39]
In the Amol study by Amirkalali et al., NAFLD in men was associated with waist circumferences, serum ALT, and advanced age but in women with waist circumferences and advanced age.[29]
In a similar study in Shiraz, in the southern part of Iran, Lankarani et al. have reported a 21.5% rate of NAFLD among adult general population of Shiraz. They showed that NAFLD was associated with age, male gender, BMI, hypertension, high cholesterol, and TG and high waist circumferences. They also indicated that metabolic syndrome was significantly higher in patients with NAFLD than healthy population.[28]
In another study in Tehran, Ghamar-Chehreh et al. have investigated predictive factors independently associated with ultrasonographic grading of NAFLD. Their results demonstrated that HbA1C, hypertriglyceridemia, and body weight levels are independently associated with higher ultrasonographic NAFLD grades, but there was not any association with serum insulin levels, incidental FBS, BMI, systolic or diastolic blood pressure, total cholesterol, HDL-C, or LDL-C levels.[40]
Razavizade et al. in Kashan have studied the association between NAFLD, diagnosed and classified by ultrasonography and serum parameters. They indicated that serum ALT, TG, and HDL concentrations seem to be associated with the staging by liver ultrasonography in NAFLD. They concluded that mentioned factors might be used to predict the staging of liver ultrasonography in these patients.[41]
In a study in Ilam, Abangah et al. have the associations between serum parameters and BMI changes with the ultrasonography grade in patients with NAFLD. They showed that BMI and TG had significant correlation with NAFLD severity and high-grade ultrasonography. They concluded that BMI could have predictive value for NAFLD, but ALT could not because of its changes in different conditions.[42]
In a case–control study in Isfahan, Hashemi Kani et al. compared anthropometric and biochemical indices among patients with NAFLD and healthy group. They indicated that patients with NAFLD had higher weight, BMI, and waist circumference compared to the control group. Patients with NAFLD had higher level of liver enzymes, TG, LDL, total cholesterol, albumin, blood urea nitrogen, and uric acid.[43]
In the current study, although all studied risk factors were significantly higher in patients with NAFLD, the association was more prominent for age, BMI, TG, FBS, and ALT. Our findings in this regard could be used as baseline information for our future studies in the field of screening, preventing, and management of NAFLD.
In this study, the highest association was related to BMI, followed by ALT and then TG and FBS.
It is well recognized that increased BMI (obesity) has a crucial role in the development of NAFLD and many studies demonstrated its association with NAFLD. Moreover, it could be a predictor of the severity of NAFLD.[39,44,45]
Although the exact pathogenesis of ALT in developing NAFLD was not clearly demonstrated, it is considered as a surrogate marker for NAFLD. Its association with NAFLD has been reported in many studies. It could also be used as an important marker for disease severity and/or hepatic activity.[31,36,46] Jamali et al. indicated that the most common cause of increased ALT among the Iranian population is NAFLD.[47]
Lack of association between AST and NAFLD may be due to the fact that it is an intracellular and nonspecific enzyme of liver. Its level increased during tissue injury and cell death. Hence, it could be increased in other conditions not related to liver function.[48]
Regarding ALP, the lack of its association with NAFLD could be explained that previous studies indicated that ALP increased in severe grades of NAFLD, and as the high proportion of our patients with NAFLD had Grade I of the disease, the findings could be justified.[49]
The association between TG and NAFLD has been documented in several studies.[43,41] The nonsignificant association of cholesterol, HDL-C and LDL-C, could be explained with regard to that possibly these lipids alone cannot be an important indicator of IR.[41]
The limitation of this study was the cross-sectional design of the study. In this study, the biochemical measurements were performed only one time during the study. Another limitation was ultrasonographic assessment of NAFLD. Although ultrasonography is a safe and reliable noninvasive method for diagnosing the disease, it had some limitations as it could not distinguish low-grade fatty infiltration (<30%) and fibrosis.[50] It is recommended to conduct more prospective, longitudinal studies for obtaining more conclusive results in this field.
The strength of this study was appropriate sampling method of studied population in a way that they were representative of the general population. In addition, to reduce interobserver variability, all of the ultrasonographic measurements were performed by a single expert radiologist.
Conclusion
In general, our findings showed a higher rate of NAFLD among Isfahani adult general population; however, considering the high proportion of NAFLD cases was the milder form of the disease (Grade I and FFI) and the association of anthropometrics and metabolic variables with the occurrence of NAFLD, it seems that interventional studies which target-related risk factors could reduce the overall occurrence of NAFLD as well as its severe form and its related complications. However, the higher possibility of occurrence of end-stage liver disease as well as increased CVD in patients with NAFLD emphasize on planning further studies for evaluating the cost-effectiveness of NAFLD screening program and implementation of appropriate strategies for prevention, early detection, and proper management of the disease in our region.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Sanyal AJ, Brunt EM, Kleiner DE, Kowdley KV, Chalasani N, Lavine JE, et al. Endpoints and clinical trial design for nonalcoholic steatohepatitis. Hepatology. 2011;54:344–53. doi: 10.1002/hep.24376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khedmat H, Taheri S. Non-alcoholic steatohepatitis: An update in pathophysiology, diagnosis and therapy. Hepat Mon. 2011;11:74–85. [Google Scholar]
- 3.Tiniakos DG, Vos MB, Brunt EM. Nonalcoholic fatty liver disease: Pathology and pathogenesis. Annu Rev Pathol. 2010;5:145–71. doi: 10.1146/annurev-pathol-121808-102132. [DOI] [PubMed] [Google Scholar]
- 4.Alavian SM, Motlagh ME, Ardalan G, Motaghian M, Davarpanah AH, Kelishadi R. Hypertriglyceridemic waist phenotype and associated lifestyle factors in a national population of youths: CASPIAN Study. J Trop Pediatr. 2008;54:169–77. doi: 10.1093/tropej/fmm105. [DOI] [PubMed] [Google Scholar]
- 5.Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: From steatosis to cirrhosis. Hepatology. 2006;43(2 Suppl 1):S99–112. doi: 10.1002/hep.20973. [DOI] [PubMed] [Google Scholar]
- 6.Lazo M, Clark JM. The epidemiology of nonalcoholic fatty liver disease: A global perspective. Semin Liver Dis. 2008;28:339–50. doi: 10.1055/s-0028-1091978. [DOI] [PubMed] [Google Scholar]
- 7.Alavian SM, Mohammad-Alizadeh AH, Esna-Ashari F, Ardalan G, Hajarizadeh B. Non-alcoholic fatty liver disease prevalence among school-aged children and adolescents in Iran and its association with biochemical and anthropometric measures. Liver Int. 2009;29:159–63. doi: 10.1111/j.1478-3231.2008.01790.x. [DOI] [PubMed] [Google Scholar]
- 8.Sohrabpour A, Rezvan H, Amini-Kafiabad S, Dayhim M, Merat S, Pourshams A. Prevalence of nonalcoholic steatohepatitis in Iran: A population based study. Middle East J Dig Dis. 2010;2:14–9. [PMC free article] [PubMed] [Google Scholar]
- 9.Crabb DW, Galli A, Fischer M, You M. Molecular mechanisms of alcoholic fatty liver: Role of peroxisome proliferator-activated receptor alpha. Alcohol. 2004;34:35–8. doi: 10.1016/j.alcohol.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Li H, Wang YJ, Tan K, Zeng L, Liu L, Liu FJ, et al. Prevalence and risk factors of fatty liver disease in Chengdu, Southwest China. Hepatobiliary Pancreat Dis Int. 2009;8:377–82. [PubMed] [Google Scholar]
- 11.Targher G. Non-alcoholic fatty liver disease, the metabolic syndrome and the risk of cardiovascular disease: The plot thickens. Diabet Med. 2007;24:1–6. doi: 10.1111/j.1464-5491.2007.02025.x. [DOI] [PubMed] [Google Scholar]
- 12.Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142:1592–609. doi: 10.1053/j.gastro.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 13.Bhatia LS, Curzen NP, Calder PC, Byrne CD. Non-alcoholic fatty liver disease: A new and important cardiovascular risk factor? Eur Heart J. 2012;33:1190–200. doi: 10.1093/eurheartj/ehr453. [DOI] [PubMed] [Google Scholar]
- 14.Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37:917–23. doi: 10.1053/jhep.2003.50161. [DOI] [PubMed] [Google Scholar]
- 15.Ong JP, Pitts A, Younossi ZM. Increased overall mortality and liver-related mortality in non-alcoholic fatty liver disease. J Hepatol. 2008;49:608–12. doi: 10.1016/j.jhep.2008.06.018. [DOI] [PubMed] [Google Scholar]
- 16.Pacana T, Sanyal AJ. Vitamin E and nonalcoholic fatty liver disease. Curr Opin Clin Nutr Metab Care. 2012;15:641–8. doi: 10.1097/MCO.0b013e328357f747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kemmer N, Neff GW, Franco E, Osman-Mohammed H, Leone J, Parkinson E, et al. Nonalcoholic fatty liver disease epidemic and its implications for liver transplantation. Transplantation. 2013;96:860–2. doi: 10.1097/01.TP.0000436723.59879.01. [DOI] [PubMed] [Google Scholar]
- 18.Saverymuttu SH, Joseph AE, Maxwell JD. Ultrasound scanning in the detection of hepatic fibrosis and steatosis. Br Med J (Clin Res Ed) 1986;292:13–5. doi: 10.1136/bmj.292.6512.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sanyal AJ American Gastroenterological Association. AGA technical review on nonalcoholic fatty liver disease. Gastroenterology. 2002;123:1705–25. doi: 10.1053/gast.2002.36572. [DOI] [PubMed] [Google Scholar]
- 20.Kennedy G. Non-alcoholic fatty liver disease: Can ultrasound assist in early diagnosis of prediabetes and delay progression to type 2 diabetes mellitus. Sound Effects. 2009 [Google Scholar]
- 21.Hernaez R, Lazo M, Bonekamp S, Kamel I, Brancati FL, Guallar E, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: A meta-analysis. Hepatology. 2011;54:1082–90. doi: 10.1002/hep.24452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bellentani S, Bedogni G, Miglioli L, Tiribelli C. The epidemiology of fatty liver. Eur J Gastroenterol Hepatol. 2004;16:1087–93. doi: 10.1097/00042737-200411000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Zhou YJ, Li YY, Nie YQ, Ma JX, Lu LG, Shi SL, et al. Prevalence of fatty liver disease and its risk factors in the population of South China. World J Gastroenterol. 2007;13:6419–24. doi: 10.3748/wjg.v13.i47.6419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: Impact of ethnicity. Hepatology. 2004;40:1387–95. doi: 10.1002/hep.20466. [DOI] [PubMed] [Google Scholar]
- 25.Omagari K, Kadokawa Y, Masuda J, Egawa I, Sawa T, Hazama H, et al. Fatty liver in non-alcoholic non-overweight Japanese adults: Incidence and clinical characteristics. J Gastroenterol Hepatol. 2002;17:1098–105. doi: 10.1046/j.1440-1746.2002.02846.x. [DOI] [PubMed] [Google Scholar]
- 26.Park SH, Jeon WK, Kim SH, Kim HJ, Park DI, Cho YK, et al. Prevalence and risk factors of non-alcoholic fatty liver disease among Korean adults. J Gastroenterol Hepatol. 2006;21(1 Pt 1):138–43. doi: 10.1111/j.1440-1746.2005.04086.x. [DOI] [PubMed] [Google Scholar]
- 27.Rogha M, Najafi N, Azari A, Kaji M, Pourmoghaddas Z, Rajabi F, et al. Non-alcoholic steatohepatitis in a sample of Iranian adult population: Age is a risk factor. Int J Prev Med. 2011;2:24–7. [PMC free article] [PubMed] [Google Scholar]
- 28.Lankarani KB, Ghaffarpasand F, Mahmoodi M, Lotfi M, Zamiri N, Heydari ST, et al. Non alcoholic fatty liver disease in Southern Iran: A population based study. Hepat Mon. 2013;13:e9248. doi: 10.5812/hepatmon.9248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amirkalali B, Poustchi H, Keyvani H, Khansari MR, Ajdarkosh H, Maadi M, et al. Prevalence of non-alcoholic fatty liver disease and its predictors in North of Iran. Iran J Public Health. 2014;43:1275–83. [PMC free article] [PubMed] [Google Scholar]
- 30.Azizi F, Salehi P, Etemadi A, Zahedi-Asl S. Prevalence of metabolic syndrome in an urban population: Tehran Lipid and Glucose Study. Diabetes Res Clin Pract. 2003;61:29–37. doi: 10.1016/s0168-8227(03)00066-4. [DOI] [PubMed] [Google Scholar]
- 31.Fan JG, Farrell GC. Epidemiology of non-alcoholic fatty liver disease in China. J Hepatol. 2009;50:204–10. doi: 10.1016/j.jhep.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 32.Feldman M, Friedman LS, Brandt LJ. Nonalcoholic fatty liver disease. Gastrointestinal and Liver Disease. 8th ed. Canada: Saunders; 2006. pp. 1793–805. [Google Scholar]
- 33.García-Monzón C, Martín-Pérez E, Iacono OL, Fernández-Bermejo M, Majano PL, Apolinario A, et al. Characterization of pathogenic and prognostic factors of nonalcoholic steatohepatitis associated with obesity. J Hepatol. 2000;33:716–24. doi: 10.1016/s0168-8278(00)80301-3. [DOI] [PubMed] [Google Scholar]
- 34.Kabir M, Catalano KJ, Ananthnarayan S, Kim SP, Van Citters GW, Dea MK, et al. Molecular evidence supporting the portal theory: A causative link between visceral adiposity and hepatic insulin resistance. Am J Physiol Endocrinol Metab. 2005;288:E454–61. doi: 10.1152/ajpendo.00203.2004. [DOI] [PubMed] [Google Scholar]
- 35.Tung T, Chiu W, Lin T, Shih H, Hsu C. An exploration of prevalence and associated factors of nonalcoholic fatty liver disease in the Taiwanese police service. Iran J Public Health. 2011;40:54–62. [PMC free article] [PubMed] [Google Scholar]
- 36.Eguchi Y, Hyogo H, Ono M, Mizuta T, Ono N, Fujimoto K, et al. Prevalence and associated metabolic factors of nonalcoholic fatty liver disease in the general population from 2009 to 2010 in Japan: A multicenter large retrospective study. J Gastroenterol. 2012;47:586–95. doi: 10.1007/s00535-012-0533-z. [DOI] [PubMed] [Google Scholar]
- 37.Zelber-Sagi S, Nitzan-Kaluski D, Halpern Z, Oren R. Prevalence of primary non-alcoholic fatty liver disease in a population-based study and its association with biochemical and anthropometric measures. Liver Int. 2006;26:856–63. doi: 10.1111/j.1478-3231.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- 38.Lin YC, Chou SC, Huang PT, Chiou HY. Risk factors and predictors of non-alcoholic fatty liver disease in Taiwan. Ann Hepatol. 2011;10:125–32. [PubMed] [Google Scholar]
- 39.Kwon YM, Oh SW, Hwang SS, Lee C, Kwon H, Chung GE. Association of nonalcoholic fatty liver disease with components of metabolic syndrome according to body mass index in Korean adults. Am J Gastroenterol. 2012;107:1852–8. doi: 10.1038/ajg.2012.314. [DOI] [PubMed] [Google Scholar]
- 40.Ghamar-Chehreh ME, Khedmat H, Amini M, Taheri S. Predictive factors for ultrasonographic grading of nonalcoholic fatty liver disease. Hepat Mon. 2012;12:e6860. doi: 10.5812/hepatmon.6860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Razavizade M, Jamali R, Arj A, Talari H. Serum parameters predict the severity of ultrasonographic findings in non-alcoholic fatty liver disease. Hepatobiliary Pancreat Dis Int. 2012;11:513–20. doi: 10.1016/s1499-3872(12)60216-1. [DOI] [PubMed] [Google Scholar]
- 42.Abangah G, Yousefi A, Asadollahi R, Veisani Y, Rahimifar P, Alizadeh S. Correlation of body mass index and serum parameters with ultrasonographic grade of fatty change in non-alcoholic fatty liver disease. Iran Red Crescent Med J. 2014;16:e12669. doi: 10.5812/ircmj.12669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hashemi Kani A, Alavian SM, Esmaillzadeh A, Adibi P, Azadbakht L. Dietary quality indices and biochemical parameters among patients with non alcoholic fatty liver disease (NAFLD) Hepat Mon. 2013;13:e10943. doi: 10.5812/hepatmon.10943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee S, Jin Kim Y, Yong Jeon T, Hoi Kim H, Woo Oh S, Park Y, et al. Obesity is the only independent factor associated with ultrasound-diagnosed non-alcoholic fatty liver disease: A cross-sectional case-control study. Scand J Gastroenterol. 2006;41:566–72. doi: 10.1080/00365520500319591. [DOI] [PubMed] [Google Scholar]
- 45.Sogabe M, Okahisa T, Tsujigami K, Fukuno H, Hibino S, Yamanoi A. Visceral fat predominance is associated with non-alcoholic fatty liver disease in Japanese women with metabolic syndrome. Hepatol Res. 2014;44:515–22. doi: 10.1111/hepr.12146. [DOI] [PubMed] [Google Scholar]
- 46.Pratt DS, Kaplan MM. Evaluation of abnormal liver-enzyme results in asymptomatic patients. N Engl J Med. 2000;342:1266–71. doi: 10.1056/NEJM200004273421707. [DOI] [PubMed] [Google Scholar]
- 47.Jamali R, Khonsari M, Merat S, Khoshnia M, Jafari E, Bahram Kalhori A, et al. Persistent alanine aminotransferase elevation among the general Iranian population: Prevalence and causes. World J Gastroenterol. 2008;14:2867–71. doi: 10.3748/wjg.14.2867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ye J, Chen Z, Wang T, Tong J, Li X, Jiang J, et al. Role of tissue disorder markers in the evaluation of disease progress and outcome prediction: A prospective cohort study in non-cardiac critically ill patients. J Clin Lab Anal. 2010;24:376–84. doi: 10.1002/jcla.20397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Obika M, Noguchi H. Diagnosis and evaluation of nonalcoholic fatty liver disease. Exp Diabetes Res 2012. 2012 doi: 10.1155/2012/145754. 145754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ghamar-Chehreh ME, Amini M, Khedmat H, Moayed Alavian S, Daraei F, Mohtashami R, et al. Elevated alanine aminotransferase activity is not associated with dyslipidemias, but related to insulin resistance and higher disease grades in non-diabetic non-alcoholic fatty liver disease. Asian Pac J Trop Biomed. 2012;2:702–6. doi: 10.1016/S2221-1691(12)60213-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


