Abstract
Background:
This study was designed to evaluate the effect of melatonin on nonalcoholic fatty liver disease (NAFLD) in compared to placebo.
Materials and Methods:
A total of 100 patients with histopathological diagnosis NAFLD in two groups of case and control received oral melatonin or placebo thrice daily for 3 months. Collected data were weight, waist, systolic blood pressure (SBP), diastolic blood pressure (DBP), alanine aminotransferase (ALT), aspartate aminotransferase (AST), high sensitive C-reactive protein (hsCRP), fatty liver grade, and side effects which were measured at baseline and after treatment period using standard clinical chemistry techniques.
Results:
Before treatment the mean of weight, waist, SBP, DBP, ALT, AST, and hsCRP between cases and controls were similar (P > 0.5). After treatment, only the differences in the mean of hsCRP in cases was significantly lower than controls (P = 0.003). In case group, all variables after treatment were significantly decreased compare to baseline (P > 0.5) and only AST after treatment was similar to before treatment (P > 0.5). The mean of a decrease in the level of weight, waist, SBP, and ALT were not statistically significant between groups (P > 0.5). In the case group in compare to control group the level of DBP, AST, and hsCRP significantly more decreased. After treatment fatty, liver grade was statistically improved in more cases than controls (P = 0.001). Side effects were similar between the two groups.
Conclusion:
Melatonin significantly decreases liver enzymes, so the use of melatonin in patients with NAFLD can be effective.
Keywords: Liver disease, melatonin, nonalcoholic fatty liver disease
Introduction
Nonalcoholic fatty liver disease (NAFLD) is a condition defined by excessive fat accumulation in the form of triglycerides in the liver (>5% of hepatocytes histologically), and recently recognized as a major liver disease throughout the world.[1,2] Simple hepatic steatosis with rather good prognosis and nonalcoholic steatohepatitis (NASH) are the spectrum of NAFLD. NASH is often a precursor to the development of cirrhosis and in some cases, hepatocellular carcinoma.[2,3,4]
Because of differences in studied population and the diagnostic methods used, the reported prevalence of NAFLD largely varies. Worldwide, the prevalence of NAFLD in the general population ranges from 9% to 37%.[5,6,7,8] It is estimated that the prevalence of NAFLD in the adult population is between 30% and 40% and that up to 40% of people with NAFLD have NASH. Recent studies in Western countries reported that the prevalence of NAFLD in the general population is approximately 20–30%.[9,10]
The molecular mechanism underlying NAFLD progression is not completely understood, but insulin resistance, oxidative stress, and cytokine imbalance are known as key pathophysiological mechanisms in NAFLD.[11,12] These factors have been proposed to explain the transformation of NAFLD from simple steatosis to NASH, and interaction of free radicals with cellular constituents may result in their peroxidative deterioration leading to an impaired of cellular functions.[13] Despite the numerous studies on novel therapeutic options, the standards of pharmacological treatment of NAFLD have not been established. The effectiveness of Vitamin E, Vitamin C and betaine as some antioxidant agents have been evaluated, however, the evidences of the efficacy of such treatments have been equivocal.[14,15,16]
Treatment methods that could efficiently decrease both the oxidative stress and apoptosis of hepatocytes in NAFLD are still being searched for. Melatonin (N-acetyl-5-methoxytryptamine) produced by the pineal gland. As an effective antioxidant, directly scavenge a variety of free radicals. And also reduces free radical levels via stimulating the activities of antioxidative enzymes.[17,18] Decrease in oxidative stress, lessen liver damage, and improve liver histology in rats with high-fat diet-induced NAFLD, has shown after given melatonin simultaneously with the diet.[19] The hypocholesterolemic and lipid peroxidation inhibitory effect of melatonin has shown in some animal studies and the serum levels of cholesterol and triglycerides were reduced in mice with experimental diet-induced hypercholesterolemia in mice.[20,21] Furthermore, several studies in human demonstrated that treatment with melatonin was effective in NAFLD.[22,23,24,25,26,27,28] In rats with NAFLD melatonin alone or administered in combination with pioglitazone or pentoxifylline was been effective and data of animal study indicate that melatonin can be used as promising adjunct therapy in the clinical management of NAFLD with excellent safety and tolerability.[12]
There is no standard pharmacological treatment for NAFLD and data about effect of melatonin on NAFLD is limited. Therefore, present study was aimed to determine the effects of melatonin on the selected biochemical parameters in patients with NAFLD.
Materials and Methods
Between April and November 2013, after that the Ethics Committee of Arak University of Medical Sciences approved this double blind, randomized, controlled trial, 100 patients with NAFLD including 62 males and 38 females between 22 and 65 years who referred to Amir Almomanin Hospital in Arak, Iran, were enrolled. The diagnosis of NAFLD was based on both clinical and pathological findings in the liver and appropriate exclusion of other liver diseases. Patients in both gender with age between 20 and 65 years with diagnostic NAFLD were eligible if they had no diabetes mellitus, viral hepatitis, autoimmune hepatitis, drug-induced liver disease, primary biliary cirrhosis, primary sclerosing cholangitis, biliary obstruction, Wilson's disease, hemochromatosis, and decompensated cirrhosis. In addition, patients with the use of drugs known to produce fatty liver disease, and weight loss more than 10% from baseline in the previous 6 months were excluded from the study. Written informed consent was obtained from all studied patients. For diagnosis of NAFLD and ruling out other diseases that mimic NAFLD all of subject underwent laboratory tests for viral hepatitis such as hepatitis B surface antigen hepatitis C virus antibodies iron total iron-binding capacity and ferritin for hemochromatosis and serum ceruloplasmin and urinary Cu for Wilson and history of alcohol consumption for alcoholic fatty liver thus all of these diseases is ruled out before enrolling to study.
Using random-maker software “Random Allocation” eligible patients randomly divided into two case and control groups. Case group included 50 patients who received a tablet of melatonin (orally twice daily). The control group included 50 patients who received placebo which formally manufactured as the same as melatonin tablets. The treatment period was 6 weeks for both groups, and all patients were suggested to have same diet and exercise regimen during this period.
Clinical and laboratory data were collected before and after treatment. Collected data included weight, waist, systolic blood pressure (SBP), diastolic blood pressure (DBP), alanine aminotransferase (ALT), aspartate aminotransferase (AST), high sensitive C-reactive protein (hsCRP), fatty liver grade, and side effects. Weight in kilograms/(height in meter)2 was used to calculate body mass index and standard clinical chemistry techniques were used measured laboratory data. The grade of fatty liver was assessed by ultrasonography of the live in three grade of mild, moderate, and severe. All ultrasonographies evaluations performed by an expert radiologist, to avoid inter-operator discordance.
All statistical analyses were done using SPSS software for Windows, version 20 (SPSS Inc., Chicago, IL, USA). Data for continuous variables were recorded as means with standard deviations, and those for categorical variables were recorded as counts with percentages. Comparisons between categorical variables were performed using Chi-square test. In case of continuous variables, differences between means were compared using independent sample t-test, paired t-test, and repeated measurements of ANOVA. P < 0.05 was considered statistically significant.
Results
The flowchart of the study is shown in Figure 1. As shown, 12 of 112 reviewed patients with NAFLD did not enter to the study (five did not eligible, and seven refused informed consent). One hundred eligible patients were assigned to studied groups, and three of patients in both groups were excluded during follow-up. Finally, 49 patients in the case group and 48 patients in the control group completed the study and analyzed. The mean of age in cases was 42.5 ± 10.1 years and in controls was 40.6 ± 9.8 years (P = 0.35). Thirty-three (69%) patients of cases were male and 14 (31%) were female whereas in control group 27 (56%) were male and 21 (44%) were female (P = 0.26).
Figure 1.
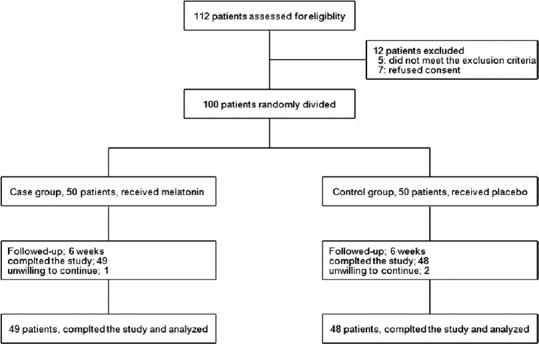
Flowchart of the study
Table 1 shows the comparison of measured parameters before and after treatment between studied groups. As shown before treatment, the differences in the mean of weight, waist, SBP, DBP, ALT, AST, and hsCRP between cases and controls were not statistically significant (P > 0.5). After treatment, only the differences in the mean of hsCRP in cases was significantly lower than controls (P = 0.003), and there were no significant differences groups for other variables (P > 0.5). In control group, no significant differences were noted after treatment in compared to baseline for all studied variables (P > 0.5). In the case group, all variables after treatment were significantly decreased compare to baseline (P > 0.5) and only AST after treatment was similar to before treatment (P > 0.5).
Table 1.
Comparison of BMI and laboratory data of 97 patients with nonalcoholic fatty liver disease
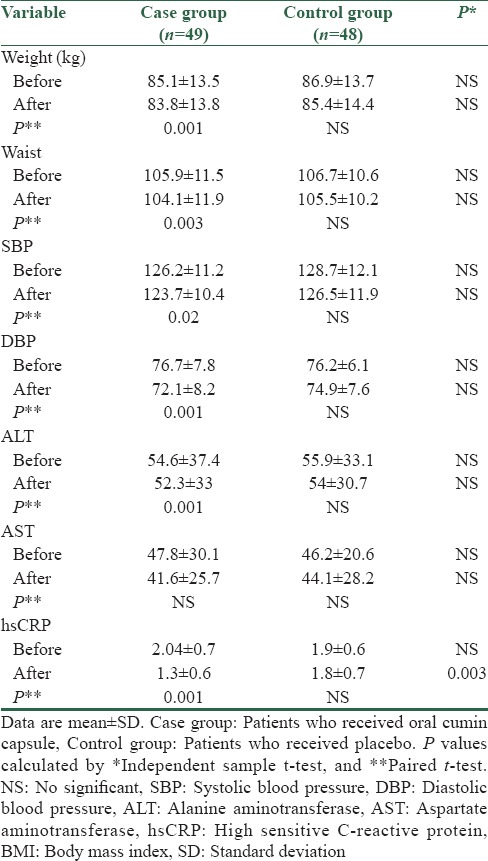
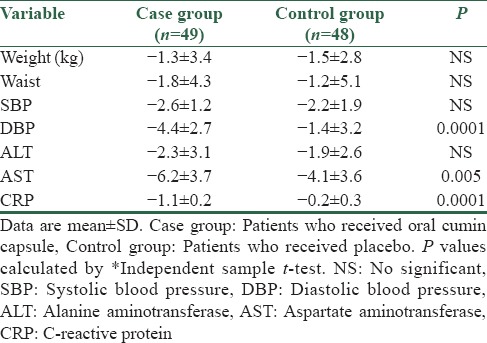
Table 2 shows the results of independent sample t-test in comparison of the mean of a decrease in studied variables after treatment compare to baseline between groups. As shown the mean of a decrease in the level of weight, waist, SBP, and ALT were not statistically significant between groups (P > 0.5). In the case group in compare to control group the level of DBP (4.4 and 1.4 respectively, P = 0.0001), AST (6.2 and 4.1 respectively, P = 0.005) and hsCRP (1.1 and 0.2 respectively, P = 0.0001) significantly more decreased.
Table 2.
Comparison of mean changes in studied variables of 100 patients with nonalcoholic fatty liver disease
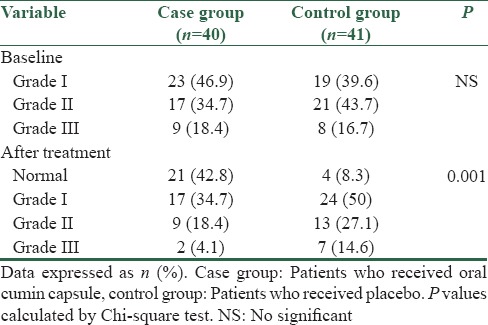
The results of comparing fatty liver grade before and after treatment between studied groups was shown in Table 3. Before treatment frequency of fatty liver grades between case and control groups was not statistically significant (P > 0.5). Before treatment, most of studied patients in both groups had grade I and II fatty liver steatosis but after treatment. After treatment in the case group, fatty liver in 21 patients improved and had normal grade of fatty liver in the control group fatty liver only in 4 patients was normal. Totally, after treatment the differences in the frequency of fatty liver grade between groups was statistically significant whereas fatty liver was improved in more cases than controls (P = 0.001). Between cases and controls no serious side effects were observed, and the rates of other side effects were similar between the two groups (data not shown).
Table 3.
The grade of steatosis before and after treatment between studied groups
Discussion
However, a sensitive indicator of liver cell damage in any form of liver disease is an increase in liver enzyme level because of no strict correlation with histologic liver lesions may suggest a liver disease that warrants treatment.[22] Consistent with the beneficial effect of melatonin on liver function, melatonin when given simultaneously with the diet has been shown to attenuate oxidative stress, lessen liver damage, and improve liver histology in rats with high-fat diet-induced NAFLD.[19] The present study was designed to assess the effect of melatonin in patients with NAFLD and results showed that in case group the mean of weight, waist, SBP, DBP, hsCRP, and ALT after treatment was significantly decreased compare to baseline, also, melatonin significantly decrease DBP, AST, and hsCRP in case group more than control group. In addition, in most of the patients who received melatonin grade of fatty liver improved than controls. These results demonstrated that use of melatonin in patients with NAFLD was more affected than placebo with no serious side effects.
Studies on the beneficial effect of melatonin are limited. In similar research by Gonciarz et al., the mean levels of aminotransferases ALT and AST after the 24-week treatment with melatonin significantly decreased compared with the baseline levels in patients with NAFLD.[23] These findings are similar to our results, as our study show statistically significant differences in the level of ALT and AST throughout the period of treatment with melatonin however treatment period in our study was shorter than Gonciarz et al.,[23] study.
Improvement of liver enzymes in overweight or obese patients with NAFLD/NASH after the reduction of weight have suggested in many reports in past few years.[24,25] In our study, there was significant weight loss and waist circumference reduction during the study period in case group and also ALT in these patients was significantly decreased which it can be explain by the effect of weight loss on ALT reduction. Other studies reported significant decrease in ALT after treatment with melatonin whereas weight loss during the study period was not significant.[23,25] Other studies in patients with NAFLD after treatment with melatonin for 6 months reported no effect on cholesterol and triglyceride levels, nor were these levels changed 3 months after discontinuation of melatonin, compared with a placebo group.[2,23] This can be explain by duration and doses of treatment regimen and probable differences in diet regimen and lifestyle, however, all patients suggested to have same diet and exercise regimen.
Melatonin in the doses of 10 mg/kg decreased the liver triglyceride content[26] whereas in rats fed with high-fat diet in the doses of 5 and 10 mg/kg reduced high cholesterol levels.[27] The antioxidative action of melatonin could be accredited the protective effect of melatonin in hepatic steatosis in rats. In addition, melatonin alone or in combination with other drugs, in other animal study reduced triglycerides and activities of liver enzymes in rats with NAFLD and the dose of 10 mg/kg reduced hepatic steatosis, serum levels of ALT, AST, and oxidative stress parameters.[12] These results in similar to our study reported the effects of melatonin in NAFLD in animal models, so, data in these studies with our results indicate that melatonin can be used in the clinical management of NAFLD.
Conclusion
The findings of this study show that melatonin significantly decrease liver enzymes in cases than placebo, therefore, the use of melatonin in patients with NAFLD can be effective. Also, NAFLD as the fast developing disorder needs serious and immediate attention, especially in the context of modern life style.
The limitation of our study is that we did not biopsy of liver thus we could not stage of our patients according to histology and could not evaluate the effect of melatonin on histology of NAFLD.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Angulo P. Nonalcoholic fatty liver disease. N Engl J Med. 2002;346:1221–31. doi: 10.1056/NEJMra011775. [DOI] [PubMed] [Google Scholar]
- 2.Gonciarz M, Gonciarz Z, Bielanski W, Mularczyk A, Konturek PC, Brzozowski T, et al. The pilot study of 3-month course of melatonin treatment of patients with nonalcoholic steatohepatitis: Effect on plasma levels of liver enzymes, lipids and melatonin. J Physiol Pharmacol. 2010;61:705–10. [PubMed] [Google Scholar]
- 3.Ong JP, Younossi ZM. Epidemiology and natural history of NAFLD and NASH. Clin Liver Dis. 2007;11:1–16. doi: 10.1016/j.cld.2007.02.009. vii. [DOI] [PubMed] [Google Scholar]
- 4.Ascha MS, Hanouneh IA, Lopez R, Tamimi TA, Feldstein AF, Zein NN. The incidence and risk factors of hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. Hepatology. 2010;51:1972–8. doi: 10.1002/hep.23527. [DOI] [PubMed] [Google Scholar]
- 5.Bedogni G, Miglioli L, Masutti F, Tiribelli C, Marchesini G, Bellentani S. Prevalence of and risk factors for nonalcoholic fatty liver disease: The dionysos nutrition and liver study. Hepatology. 2005;42:44–52. doi: 10.1002/hep.20734. [DOI] [PubMed] [Google Scholar]
- 6.Shen L, Fan JG, Shao Y, Zeng MD, Wang JR, Luo GH, et al. Prevalence of nonalcoholic fatty liver among administrative officers in Shanghai: An epidemiological survey. World J Gastroenterol. 2003;9:1106–10. doi: 10.3748/wjg.v9.i5.1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Omagari K, Kadokawa Y, Masuda J, Egawa I, Sawa T, Hazama H, et al. Fatty liver in non-alcoholic non-overweight Japanese adults: Incidence and clinical characteristics. J Gastroenterol Hepatol. 2002;17:1098–105. doi: 10.1046/j.1440-1746.2002.02846.x. [DOI] [PubMed] [Google Scholar]
- 8.Lai SW, Tan CK, Ng KC. Epidemiology of fatty liver in a hospital-based study in Taiwan. South Med J. 2002;95:1288–92. [PubMed] [Google Scholar]
- 9.Bosch FX, Ribes J, Díaz M, Cléries R. Primary liver cancer: Worldwide incidence and trends. Gastroenterology. 2004;127(5 Suppl 1):S5–S16. doi: 10.1053/j.gastro.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 10.Bellentani S, Scaglioni F, Marino M, Bedogni G. Epidemiology of non-alcoholic fatty liver disease. Dig Dis. 2010;28:155–61. doi: 10.1159/000282080. [DOI] [PubMed] [Google Scholar]
- 11.Berlanga A, Guiu-Jurado E, Porras JA, Auguet T. Molecular pathways in non-alcoholic fatty liver disease. Clin Exp Gastroenterol. 2014;7:221–39. doi: 10.2147/CEG.S62831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zaitone S, Hassan N, El-Orabi N, El-Awady el-S. Pentoxifylline and melatonin in combination with pioglitazone ameliorate experimental non-alcoholic fatty liver disease. Eur J Pharmacol. 2011;662:70–7. doi: 10.1016/j.ejphar.2011.04.049. [DOI] [PubMed] [Google Scholar]
- 13.Dowman JK, Tomlinson JW, Newsome PN. Pathogenesis of non-alcoholic fatty liver disease. QJM. 2010;103:71–83. doi: 10.1093/qjmed/hcp158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arendt BM, Allard JP. Effect of atorvastatin, Vitamin E and C on nonalcoholic fatty liver disease: Is the combination required? Am J Gastroenterol. 2011;106:78–80. doi: 10.1038/ajg.2010.310. [DOI] [PubMed] [Google Scholar]
- 15.Duvnjak M, Tomasic V, Gomercic M, Smircic Duvnjak L, Barsic N, Lerotic I. Therapy of nonalcoholic fatty liver disease: Current status. J Physiol Pharmacol. 2009;60(Suppl 7):57–66. [PubMed] [Google Scholar]
- 16.Sanyal AJ, Chalasani N, Kowdley KV, McCullough A, Diehl AM, Bass NM, et al. Pioglitazone, Vitamin E, or placebo for nonalcoholic steatohepatitis. N Engl J Med. 2010;362:1675–85. doi: 10.1056/NEJMoa0907929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rodriguez C, Mayo JC, Sainz RM, Antolín I, Herrera F, Martín V, et al. Regulation of antioxidant enzymes: A significant role for melatonin. J Pineal Res. 2004;36:1–9. doi: 10.1046/j.1600-079x.2003.00092.x. [DOI] [PubMed] [Google Scholar]
- 18.Tomás-Zapico C, Coto-Montes A. A proposed mechanism to explain the stimulatory effect of melatonin on antioxidative enzymes. J Pineal Res. 2005;39:99–104. doi: 10.1111/j.1600-079X.2005.00248.x. [DOI] [PubMed] [Google Scholar]
- 19.Hatzis G, Ziakas P, Kavantzas N, Triantafyllou A, Sigalas P, Andreadou I, et al. Melatonin attenuates high fat diet-induced fatty liver disease in rats. World J Hepatol. 2013;5:160–9. doi: 10.4254/wjh.v5.i4.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hoyos M, Guerrero JM, Perez-Cano R, Olivan J, Fabiani F, Garcia-Pergañeda A, et al. Serum cholesterol and lipid peroxidation are decreased by melatonin in diet-induced hypercholesterolemic rats. J Pineal Res. 2000;28:150–5. doi: 10.1034/j.1600-079x.2001.280304.x. [DOI] [PubMed] [Google Scholar]
- 21.Sener G, Balkan J, Cevikbas U, Keyer-Uysal M, Uysal M. Melatonin reduces cholesterol accumulation and prooxidant state induced by high cholesterol diet in the plasma, the liver and probably in the aorta of C57BL/6J mice. J Pineal Res. 2004;36:212–6. doi: 10.1111/j.1600-079x.2004.00122.x. [DOI] [PubMed] [Google Scholar]
- 22.Pagadala M, Zein CO, McCullough AJ. Predictors of steatohepatitis and advanced fibrosis in non-alcoholic fatty liver disease. Clin Liver Dis. 2009;13:591–606. doi: 10.1016/j.cld.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 23.Gonciarz M, Gonciarz Z, Bielanski W, Mularczyk A, Konturek PC, Brzozowski T, et al. The effects of long-term melatonin treatment on plasma liver enzymes levels and plasma concentrations of lipids and melatonin in patients with nonalcoholic steatohepatitis: A pilot study. J Physiol Pharmacol. 2012;63:35–40. [PubMed] [Google Scholar]
- 24.Nobili V, Manco M, Devito R, Di Ciommo V, Comparcola D, Sartorelli MR, et al. Lifestyle intervention and antioxidant therapy in children with nonalcoholic fatty liver disease: A randomized, controlled trial. Hepatology. 2008;48:119–28. doi: 10.1002/hep.22336. [DOI] [PubMed] [Google Scholar]
- 25.Promrat K, Kleiner DE, Niemeier HM, Jackvony E, Kearns M, Wands JR, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology. 2010;51:121–9. doi: 10.1002/hep.23276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pan M, Song YL, Xu JM, Gan HZ. Melatonin ameliorates nonalcoholic fatty liver induced by high-fat diet in rats. J Pineal Res. 2006;41:79–84. doi: 10.1111/j.1600-079X.2006.00346.x. [DOI] [PubMed] [Google Scholar]
- 27.Sewerynek E, Reiter RJ, Melchiorri D, Ortiz GG, Lewinski A. Oxidative damage in the liver induced by ischemia-reperfusion: Protection by melatonin. Hepatogastroenterology. 1996;43:898–905. [PubMed] [Google Scholar]
- 28.Celinski K, Konturek PC, Slomka M, Cichoz-Lach H, Brzozowski T, Konturek SJ, et al. Effects of treatment with melatonin and tryptophan on liver enzymes, parameters of fat metabolism and plasma levels of cytokines in patients with non-alcoholic fatty liver disease – 14 months follow up. J Physiol Pharmacol. 2014;65:75–82. [PubMed] [Google Scholar]


