Abstract
The current study aimed to examine the relationships between movement and resting pain intensity, pain-related distress, and psychological distress in participants scheduled for total knee arthroplasty (TKA). This study examined the impact of anxiety, depression, and pain catastrophizing on the relationship between pain intensity and pain-related distress. Data analyzed for the current study (N = 346) were collected at baseline as part of a larger Randomized Controlled Trial investigating the efficacy of TENS for TKA (TANK Study). Participants provided demographic information, pain intensity and pain-related distress, and completed validated measures of depression, anxiety, and pain catastrophizing. Only 58% of the sample reported resting pain >0 while 92% of the sample reported movement pain >0. Both movement and resting pain intensity correlated significantly with distress (rs = .86, p < .01 and .79, p < .01, respectively). About three quarters to two thirds of the sample (78% for resting pain and 65% for movement pain) reported different pain intensity and pain-related distress. Both pain intensity and pain-related distress demonstrated significant relationships with anxiety, depression, and catastrophizing. Of participants reporting pain, those reporting higher anxiety reported higher levels of distress compared to pain intensity. These findings suggest that anxious patients may be particularly distressed by movement pain preceding TKA. Future research is needed to investigate the utility of brief psychological interventions for pre-surgical TKA patients.
Keywords: Pain, total knee arthroplasty, distress
Introduction
Patient self-report is the gold standard of pain assessment, however, pain reports are inherently subjective and multidimensional. The impact of pain-related distress on the patient experience is not directly assessed by simple pain rating scales, which are often used clinically (Williamson & Hoggart, 2005). In addition, pain ratings are typically taken at rest, despite findings that movement pain is usually more severe than resting pain (Feldt KS, 2000), and significantly predicts postoperative function (Rakel et al., 2012).
Pain-related distress is frequently confused with pain intensity and psychological distress in the literature (Wells & Ridner, 2008). Pain intensity refers to a measure of pain severity; pain-related distress refers to the amount of distress caused by pain or the affective impact of pain severity; and psychological distress is a broader measure of distress which may or may not be directly pain-related. Failure to understand the relationships between pain intensity, pain-related distress, and psychological distress may contribute to challenging symptom management in patients with pain. Previous work suggests a high degree of overlap between pain intensity and distress (Fernandez & Turk, 1992; Knotkova, Crawford Clark, Mokrejs, Padour, & Kuhl, 2004). However, qualitative work suggests that about half (45%) of chronic pain patients differentiate between pain intensity and pain-related distress (de, Davies, & Chadury, 2000).
A number of psychological distress variables, including pain catastrophizing, anxiety, and depression are important in understanding pain. Pain catastrophizing is a widely researched measure of cognitive-affective responses to pain (Quartana, Campbell, & Edwards, 2009) which has been shown to predict pain intensity ratings in response to an acute pain paradigm (Sullivan & Bishop, 1995). Further, pain catastrophizing relates to pain intensity, disability, and distress (Severeijns, Vlaeyen, van den Hout, & Weber, 2001; Turner, Jensen, Warms, & Cardenas, 2002) and is a risk factor for persistent pain following Total Knee Arthroplasty (TKA; Burns et al., 2015). Anxiety is highly comorbid with chronic pain, predicts post-surgical pain, and has been show to exacerbate pain (al Absi & Rokke, 1991; Ip, Abrishami, Peng, Wong, & Chung, 2009; Kain, Sevarino, Alexander, Pincus, & Mayes, 2000; Noiseux et al., 2014; Rhudy & Meagher, 2000; Woo, 2010). Depression and pain are highly co-morbid and when pain patients are depressed, this results in greater functional impairment (Gambassi, 2009; Leo, 2005; Woo, 2010).
Previous research has identified that health-related quality of life, including mental health related quality of life is impaired in patients waiting for TKA (Desmeules, Dionne, Belzile, Bourbonnais, & Fremont, 2009). Examining psychological distress pre-TKA is important because of the predictive utility of psychological variables on surgical outcomes (Lewis, Rice, McNair, & Kluger, 2015; Mears, 2014; Noiseux et al., 2014; Utrillas-Compaired, De la Torre-Escuredo, Tebar-Martinez, & Asunsolo-Del Barco, 2014).
The purpose of the current study was to further elucidate the relationships between pain intensity, pain-related distress, and psychological distress in knee osteoarthritis patients scheduled for TKA. It was hypothesized that: (1) Pain intensity and pain-related distress would be highly correlated; (2) Pain intensity and pain-related distress would each have moderate relationships to depression, anxiety, and pain catastrophizing; and (3) Those who reported higher levels of depression, anxiety, and pain catastrophizing would report greater distress in relation to pain intensity.
Method
Design
This study used a cross-sectional design. The data were collected as part of a large, randomized, placebo controlled trial of Transcutaneous Electrical Nerve Stimulation (TENS) for control of rehabilitation pain following TKA (Rakel et al., 2014).
Participants
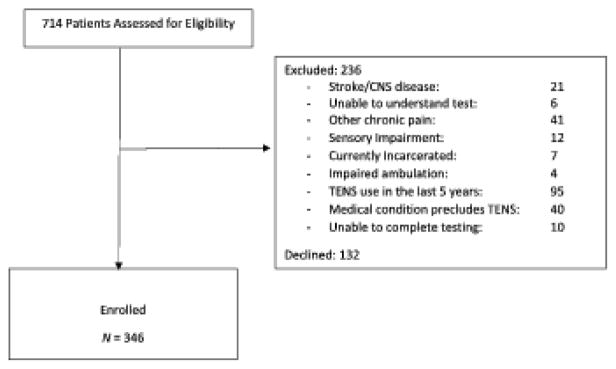
Participants were English-speaking patients with osteoarthritis who were scheduled for unilateral TKA at a Midwestern university-affiliated hospital or Veteran’s Administration hospital. A total of 346 participants were enrolled in this study; see Figure 1 for exclusion criteria and the number of potential participants excluded.
Figure 1.
Recruitment and exclusion criteria.
Measures
Demographic and medical information were assessed using a demographic and medical questionnaire that has been used by the research team in prior studies and asks questions in a standardized manner. Medical information included duration of pain (in months) and whether participants were currently taking opioid and non-opioid analgesics.
Pain Intensity was measured using a 21-point numeric rating scale (0–20 NRS) where 0 represented no pain and 20 represented ‘the most intense pain imaginable’. The NRS was used to assess both resting and movement pain. Movement pain was assessed using active flexion and extension of the surgical knee. An average score between flexion and extension pain ratings was used for analyses in this study. The 21-point scale was used rather than an 11-point scale because of the added sensitivity afforded by this scale and based on evidence supporting its use (Hadjistavropoulos et al., 2007; Herr, Spratt, Garand, & Li, 2007; Herr, Spratt, Mobily, & Richardson, 2004). Herr et al. (2004) showed the 21pt NRS most preferred of 5 tools (verbal 0–10 NRS, 0–20 NRS, Faces Pain Scale, Verbal Descriptor Scale, Vertical Visual Analogue Scale) and, when compared to the verbal 0–10 NRS, the 0–20 NRS had fewer failures (6.7 vs. 15.5%; Herr et al., 2007).
Pain-related Distress was assessed concurrently with pain intensity ratings for both movement and resting pain in participants who endorsed pain. The measure used to assess pain-related distress was designed for the current study and created to mirror the pain intensity measure. Pain-related distress was measured with a 21-point NRS that was identical to that used to assess pain intensity, except with different anchors. Participants who endorsed pain were asked how bothersome or distressing the pain in their knee was with 0 being no distress and 20 being the ‘most distress imaginable’.
Pain Catastrophizing was measured with the Pain Catastrophizing Scale (PCS; Sullivan, Bishop, & Pivik, 1995). The PCS is a 13 item self-report measure of pain catastrophizing with a total score and three subscale scores: Rumination, Magnification, and Helplessness. This measure has demonstrated good internal consistency (α = .87; Sullivan & Bishop, 1995).
Anxiety was assessed with the State-Trait Anxiety Inventory (STAI). Both the 20-item STAI-S (state) and 20-item STAI-T (trait) have demonstrated excellent internal consistency (α = .95 and .89, respectively) and have demonstrated moderate to strong correlations with other anxiety assessment tools (Elwood, Wolitzky-Taylor, & Olatunji, 2012; Grös, Antony, Simms, & McCabe, 2007).
Depression was assessed with the Geriatric Depression Scale (GDS). This 5-item ‘yes/no’ self-report scale was designed as a screening measure for depression in older adults. The five-item GDS has been shown to exhibit high sensitivity (.94), high specificity (.81), and a high positive predictive value (.81). Further, the five-item GDS and the 15-item GDS were found to have significant agreement (κ = .74 for both scales) with a clinical diagnosis of depression (Rinaldi et al., 2003).
Data collection protocol
Data analyzed in this study were collected at the pre-operative clinic visit approximately one week prior to surgery. At this visit, consented participants completed demographic questions and self-report surveys: STAI, PCS, and GDS. Research assistants then asked participants to rate pain intensity and pain-related distress while seated comfortably. Active extension and flexion of the surgical knee was then performed and participants were asked to rate their pain intensity and pain-related distress during each of these movements.
Data analyses
Pain intensity, pain-related distress, and anxiety were all found to have non-normal distributions (Shapiro Wilk tests: p < .05), so medians and interquartile ranges (25th–75th) are reported. Spearman’s rho correlations were used for hypothesis 1. A Wilcox Signed Ranks Test was used to compare resting pain intensity to movement pain intensity to identify the best pain measurement to use for Hypotheses two and three.
To test hypothesis two, Spearman’s correlations or Mann–Whitney U Tests were run between pain intensity and the psychological variables and between pain-related distress and the psychological variables.
To test hypothesis three, a difference variable was created between movement pain intensity and movement pain-related distress; intensity was subtracted from distress such that positive values indicated relatively higher levels of distress compared to intensity. This variable was relatively normally distributed and will be referred to as: distress/pain-difference. Pearson correlations were run between distress/pain difference and continuous variables (age, duration of pain, trait anxiety, state anxiety, pain catastrophizing) and t-tests were run for nominal measures: sex, depression screening, and presence or absence of analgesic consumption (opioid and non-opioid). Variables found to be significantly related to distress/pain-difference were then entered into a linear regression model and Variance Inflation Factor values were inspected for multicollinearity (2.5 was used as a cut-off indicating concern for multicollinearity). To determine if the relationships between the variables of interest differed by level of pain intensity, participants were then divided by intensity of movement pain (mild, moderate, severe) using cut-offs described in the literature and modified for use with a 0–20 NRS (Kapstad, Hanestad, Langeland, Rustoen, & Stavem, 2008) and separate analyses were performed for each of these groups.
Results
The 346 participants had a mean age of 62 years (SD = 9.58), were primarily female (54%), Caucasian (95%), married (61%), educated beyond high school (60%), and had household incomes <$60,000 (54%: see Table 1). Median resting pain intensity and distress was mild while median movement pain intensity and distress were mild to moderate (see Table 2).
Table 1.
Demographics.
| Sex | |
| Male | 158 (46%) |
| Female | 188 (54%) |
| Age | |
| Mean (SD) | 62.30 (9.58) |
| Marital Status * | |
| Never married | 19 (5%) |
| Married | 193 (56%) |
| Living with significant other | 8 (3%) |
| Divorced | 61 (18%) |
| Widowed | 34 (10%) |
| Did not answer | 31 (9%) |
| Education * | |
| <High school | 19 (5%) |
| Graduated high school | 88 (25%) |
| Some college | 94 (27%) |
| College graduate | 61 (18%) |
| Post college | 52 (15%) |
| Did not answer | 32 (9%) |
| Household Income | |
| <$10,000 | 32 (9%) |
| $10,000–$19,000 | 51 (15%) |
| $20,000–$39,000 | 59 (17%) |
| $40,000–$59,000 | 46 (13%) |
| $60,000–$79,000 | 34 (10%) |
| $80,000–$99,000 | 27 (8%) |
| $100,000–$199,000 | 27 (8%) |
| $200,000 or more | 6 (2%) |
| Did not answer | 64 (18%) |
Percentages are rounded so the total does not equal exactly 100.
Table 2.
Descriptive statistics.
| Variable | n | Median | IQR | Range |
|---|---|---|---|---|
| Resting pain | 346 | 2.00 | 0–5.00 | 0–19 |
| Resting pain-related distress | 263 | 1.00 | .00–5.00 | 0–20 |
| Movement pain | 346 | 7.00 | 3.00–11.50 | 0–20 |
| Movement pain-related distress | 294 | 7.50 | 3.00–12.50 | 0–20 |
| State anxiety | 311 | 33.00 | 26.00–40.00 | 20–67 |
| Trait anxiety | 313 | 33.00 | 27.00–39.00 | 20–68 |
| Pain catastrophizing | 318 | 9.00 | 4.00–15.00 | 0–50 |
| Screened positive | Screened negative | |||
| Depression | 322 | 25% | 75% |
Hypothesis 1
Fifty-eight percent of the sample reported resting pain >0, while 92% of the sample reported movement pain >0. In those reporting pain >0, pain intensity and pain-related distress were significantly correlated for both movement and resting pain (rs = .86, p < .01 and .79, p < .01, respectively). In those reporting resting pain >0, 22% of the sample reported the same value for resting pain intensity and distress and 71% of the sample rated resting pain and pain-related distress with a difference of three or less. In those reporting movement pain >0, 35% of the sample reported the same values for pain and distress and 79% of the sample rated movement pain intensity and pain-related distress with a difference of three or less.
Hypothesis 2
Small but significant correlations were found between the psychological variables and pain intensity and the psychological variables and pain-related distress (rs = .24–.28). Further, those who screened positive for depression had significantly higher levels of pain intensity and pain-related distress compared to those who screened negative for depression (see Table 3).
Table 3.
Relationships between psychological variables, pain intensity, and pain-related distress.
| Psychological variables | Pain intensity | Pain-related distress |
|---|---|---|
| Spearman’s correlation (p) | Spearman’s correlation (p) | |
| Trait anxiety | .26 (p = .00) | .28 (p = .00) |
| State anxiety | .25 (p = .00) | .26 (p = .00) |
| Pain catastrophizing | .28 (p = .00) | .24 (p = .00) |
| Mann–Whitney U Test | Mann–Whitney U Test | |
| Depression | ||
| Yes | Median = 8.75 | Median = 9.5 |
| No | Median = 6.5 | Median = 6.5 |
| p = .00 | p = .00 |
Hypothesis 3
Only trait anxiety demonstrated a significant relationship to distress/pain difference (see Table 4). Those scoring higher on trait anxiety had significantly higher distress/pain difference scores (r = .17, p < .05). Regression analysis was not performed since this was the only significant relationship.
Table 4.
Relationships of demographic and psychological variables with distress/pain difference variable (pain-related distress – pain intensity) for all participants reporting pain >0.
| Distress/Pain difference mean (SD) | t (p-value) | |
|---|---|---|
| Gender | ||
| Male (n = 119) | −.56 (2.79) | |
| Female (n = 163) | −.70 (2.84) | .41 (.68) |
| Taking opioids | ||
| Yes (n = 88) | −.86 (2.68) | .90 (.37) |
| No (n = 194) | −.54 (2.88) | |
| Taking non-opioid analgesics | ||
| Yes (n = 215) | −.72 (2.80) | |
| No (n = 67) | −.39 (2.88) | .83 (.40) |
| Depression | ||
| Yes (n = 69) | −.26 (3.08) | −1.57 (.09) |
| No (n = 192) | −.88 (2.96) | |
| Pearson correlation to distress/Pain difference | p-value | |
| Age (n = 282) | −.11 | .07 |
| Pain duration in months (n = 295) | .11 | .07 |
| Trait anxiety (n = 288) | .17 | .01* |
| State anxiety (n = 286) | .12 | .07 |
| Pain catastrophizing (n = 289) | .09 | .16 |
In further exploratory analyses (see Table 5), no variables were significantly correlated with the distress/pain difference variable in the mild pain group (pain > 0–7, 0–20 NRS). Therefore, regression analyses were not run. For the moderate pain group (pain > 7–14, 0–20 NRS), trait anxiety (r = .23, p < .05) and pain duration (r = .22, p < .05) both significantly correlated with the distress/pain-difference variable. A model regressing trait anxiety onto distress/pain difference, controlling for pain duration was significant: F(2, 106) = 5.15, p < .05, adjusted R2 = .07. Both pain duration (β = .18, p = .05) and trait anxiety, after controlling for pain duration (β = .22, p < .05) accounted for a significant amount of unique variance. For those reporting severe pain (pain > 14, 0–20 NRS), state anxiety significantly correlated with the distress/pain-difference variable (r = .33, p < .05). Since there was only one significant correlation, a regression model was not run.
Table 5.
Relationships of demographic and psychological variables with distress/pain difference for participants reporting mild, moderate, and severe levels of movement pain.
| Mild pain | Moderate pain | Severe pain | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | n | Distress/Pain Difference Mean (SD) | t (p-value) | n | Distress/Pain Difference Mean (SD) | t (p-value) | n | Distress/Pain Difference Mean (SD) | t (p-value) |
| Gender | |||||||||
| Male | 50 | −.28 (2.35) | 1.15 (.25) | 55 | −.74 (3.13) | −.32 (.75) | 14 | −.86 (2.88) | −.10 (.92) |
| Female | 66 | −.80 (2.41) | 60 | −.56 (2.91) | 37 | −.76 (3.46) | |||
| Opioids | |||||||||
| Yes | 29 | −.24 (2.64) | −.86 (.39) | 36 | −1.39 (2.55) | 1.81 (.07) | 23 | −.83 (2.85) | .08 (.94) |
| No | 87 | −.68 (2.30) | 79 | −.30 (3.15) | 28 | −.75 (3.66) | |||
| Non-opioids | |||||||||
| Yes | 87 | −.63 (2.39) | .41 (.68) | 90 | −.66 (2.85) | .08 (.94) | 38 | −1.08 (3.51) | 1.10 (.28) |
| No | 29 | .41 (2.41) | 25 | −.60 (3.58) | 13 | .08 (2.46) | |||
| Depression | |||||||||
| Yes | 20 | −.53 (1.97) | −.07 (.94) | 31 | −.29 (3.14) | −1.19 (.24) | 18 | .08 (1.66) | −1.49 (.08) |
| No | 86 | −.57 (2.56) | 75 | −1.03 (2.79) | 31 | −1.37 (3.94) | |||
| n | Pearson correlation to distress/Pain difference | p-value | n | Pearson correlation to distress/Pain difference | p-value | n | Pearson correlation to distress/Pain difference | p-value | |
| Age | 116 | −.08 | .40 | 115 | −.10 | .29 | 51 | −.19 | .19 |
| Pain duration | 106 | .03 | .77 | 110 | .27 | .01 | 48 | −.12 | .41 |
| Trait anxiety | 106 | .05 | .62 | 101 | .27 | .01 | 49 | .24 | .10 |
| State anxiety | 103 | .00 | .97 | 105 | .16 | .10 | 47 | .30 | .04 |
| PCS | 106 | .05 | .62 | 105 | .15 | .13 | 48 | .08 | .61 |
Discussion
This study aimed to clarify the relationships between pain intensity, pain-related distress, and psychological distress. About a quarter to a third of the sample in this study equated pain intensity and distress (22% resting pain, 35% movment pain). This is similar to the 39% of participants who did not differentiate between pain intensity and distress reported by Williams et al. (2000). Consistent with qualitative work suggesting that some patients embed distress in pain ratings (de et al., 2000), one possible explanation of these findings is that for some, pain intensity ratings may encompass a component of distress. Further, findings from this study found that while psychological distress variables related to pain intensity and pain-related distress, the relationships were small, indicating that these variables are related but unique.
The findings from this study suggest that anxious patients with moderate to severe pain may be more distressed by their pain than non-anxious patients. Median levels of state and trait anxiety in the current study were largely comparable to mean levels found in a previous study of pre-surgical TKA patients who completed the STAI (Hirschmann, Testa, Amsler, & Friederich, 2013). In Hirschmann et al.’s study, mean trait anxiety was 33 and in the current study, median trait anxiety was 33. Hirschmann et al. found slightly higher levels of state anxiety (M = 36; Hirschmann et al., 2013) then the median of 33 found in the current study. While median anxiety levels in this study do not meet clinical thresholds, anxiety still proved important in the relationship between pain intensity and pain-related distress.
The specific role of anxiety varied by level of pain intensity. In participants who reported moderate movement pain, those with higher levels of trait anxiety reported higher levels of distress relative to pain. In those who reported severe pain, those with higher levels of state anxiety reported higher levels of distress relative to pain. Previous experimental findings indicate that those with higher trait anxiety reported significantly higher levels of pain intensity and anxiety in response to a painful sitmulus and that increased state anxiety resulted in higher pain ratings across participants (Tang & Gibson, 2005). The current findngs from a clinical population are consistent with experimental evidence (Tang & Gibson, 2005); they suggest a general tendency towards anxiety (trait) may have more of an impact on pain-related distress in moderate pain. In the severe pain group, however, anxiety levels in the moment (state) have a greater impact on distress; perhaps the severe pain condition results in state anxiety. The role of anxiety in the relationship between movment pain intensity and distress, suggests that this may be an important variable to address in patients who would beneift from physical rehabiliation including movements involving painful areas of their body; such as patients recovering from TKA.
Contrary to the hypothesis, depression and pain catastrophizing were not found to relate to the difference between pain intensity and pain-related distress. These findings may have been impacted by the relatively low levels of pain catastrophizing in this sample. The median score of 9 on the PCS in this sample is well below the cut-off score of 30, which indicates clinically significant levels of pain catstrophizing (Sullivan, 2009). Rates of positive depression screening in this sample (25%), were higher than depression rates reported from the Mayo Clinic Total Joint registry (7229 patients who underwent arthroplasty from 1993–2005) of 4% in 1995 and15% in 2005 (Singh & Lewallen, 2014). Depression, however, was measured differently in the two studies, by self-report screening questions in the current study and by clinical diagnosis in the Mayo study, which may account for the differences found. An additional explanation for the current findings is that those who are more depressed or higher on pain catastrophizing may simply rate their pain as higher and fail to differentiate between pain intensity and distress. This is also a possiblility for those whith high anxiety. Further research is needed to better elucidate these differences.
Consistent with previous work (Feldt KS, 2000; Rakel et al., 2012; Srikandarajah & Gilron, 2011), the current study found movement pain reports to be significantly higher compared to resting pain. Further, the majority of participants (92%) reported movement pain (> 0) as compared to just over half of the sample (58%) reported resting pain. It is notable that over 40% of the sample did not report resting pain, since persistent pain is one of the indicators for TKA (Van Manen, Nace, & Mont, 2012). This begs the question of whether movement pain was assessed clinically in these research participants. Further, a recent review of post-surgical movement and resting pain identified that movement pain is usually more severe than resting pain and more directly impacts functional recovery (Srikandarajah & Gilron, 2011). Our findings support previous literature stressing the importance of assessing movement pain in clinical settings and research.
In addition to the importance of assessing movement pain, the current findings indicated the importance of assessing pain-related distress. While psychological interventions, as a part of multidisciplinary management, have shown to be effective for patients with chronic pain (Roditi & Robinson, 2011), psychologists are typically less involved with anxious presurgical and acute pain patients. The current findings support the need for multimodal analgesia that may include psychological interventions during the preoperative period.
Limitations
This study is not without limitations. The sample consisted of pre-TKA patients and findings would need to be examined in samples of patients with other disease profiles to determine the generalizability of these findings. Further, participants in this study were recruited as part of a larger treatment trial; findings may differ in a sample recutied specifically to examine pre-TKA pain-related distress. It is also worth noting that only 40 participants reported severe pain in this sample, limiting the power of the analyses with this sub-sample. In addition, the depression measure was used ouside of the age range it was developed for in just over half of the participant sample. Further, because this is a cross-sectional data collection with clinical patients and not an experimental paradigm or longitudinal analysis, the direction of relationships is based on theory. Finally, the results related to anxiety, although significant, were modest. Further research is needed to identify other variables not assessed in this study which also impact the relationship between pain intensity and pain-related distress.
Directions for future research
Further research is needed to determine the utility of brief screens to identify patients most likely to experience high levels of pain-related distress and whether this impacts treatment tolerance in pre-surgical and acute pain patients. In addition, future research is needed to determine the impact of brief psychological interventions targeting pain-related distress and anxiety in these patients. Such interventions may aim to improve pain management, increase engagement in physical rehabilitation, and aim to prevent the development of persistent pain. In addition, future research needs to determine whether psychologists can train other hospital staff (such as nurses) in the use of brief non-pharamacological interventions with acute pain patients.
Conclusion
Findings indicate that increased anxiety relates to higher levels of distress in relation to pain. This suggests the potential utility of psychologists in presurgical and acute pain settings and highlights the need for additional research to evaluate effective interventions aimed at addressing pain-related distress in the perioperative setting.
Acknowledgments
Funding
This work was supported by the National Institute of Nursing Research (NINR) [grant number R01 NR009844]; The University of Iowa College of Nursing; and DJO Inc. Dr Sluka is a consultant for DJO Inc., the manufacturer of the TENS units used for the larger RCT (the TANK study).
Footnotes
Disclosure statement
There are no other conflicts of interest.
References
- al Absi M, Rokke PD. Can anxiety help us tolerate pain? Pain. 1991;46:43–51. doi: 10.1016/0304-3959(91)90032-S. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/1896207. [DOI] [PubMed] [Google Scholar]
- Burns LC, Ritvo SE, Ferguson MK, Clarke H, Seltzer Z, Katz J. Pain catastrophizing as a risk factor for chronic pain after total knee arthroplasty: A systematic review. Journal of Pain Research. 2015;8:21–32. doi: 10.2147/JPR.S64730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de CWAC, Davies HT, Chadury Y. Simple pain rating scales hide complex idiosyncratic meanings. Pain. 2000;85:457–463. doi: 10.1016/S0304-3959(99)00299-7. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10781919. [DOI] [PubMed] [Google Scholar]
- Desmeules F, Dionne CE, Belzile E, Bourbonnais R, Fremont P. Waiting for total knee replacement surgery: Factors associated with pain, stiffness, function and quality of life. BMC Musculoskeletal Disorders. 2009;10:52. doi: 10.1186/1471-2474-10-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwood LS, Wolitzky-Taylor K, Olatunji BO. Measurement of anxious traits: A contemporary review and synthesis. Anxiety Stress Coping. 2012;25:647–666. doi: 10.1080/10615806.2011.582949. [DOI] [PubMed] [Google Scholar]
- Feldt KSOH. Pain and hip fracture outcomes for older adults. Orthopaedic Nursing. 2000;19:35–44. doi: 10.1097/00006416-200019060-00008. [DOI] [PubMed] [Google Scholar]
- Fernandez E, Turk DC. Sensory and affective components of pain: Separation and synthesis. Psychological Bulletin. 1992;112:205–217. doi: 10.1037/0033-2909.112.2.205. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/1454892. [DOI] [PubMed] [Google Scholar]
- Gambassi G. Pain and depression: The egg and the chicken story revisited. Archives of Gerontology and Geriatrics. 2009;49:103–112. doi: 10.1016/j.archger.2009.09.018. [DOI] [PubMed] [Google Scholar]
- Grös DF, Antony MM, Simms LJ, McCabe RE. Psychometric properties of the State-Trait Inventory for Cognitive and Somatic Anxiety (STICSA): Comparison to the State-Trait Anxiety Inventory (STAI) Psychological Assessment. 2007;19:369–381. doi: 10.1037/1040-3590.19.4.369. [DOI] [PubMed] [Google Scholar]
- Hadjistavropoulos T, Herr K, Turk DC, Fine PG, Dworkin RH, Helme R, … Williams J. An interdisciplinary expert consensus statement on assessment of pain in older persons. The Clinical Journal of Pain. 2007;23:S1–43. doi: 10.1097/AJP.0b013e31802be869. [DOI] [PubMed] [Google Scholar]
- Herr K, Spratt KF, Garand L, Li L. Evaluation of the Iowa pain thermometer and other selected pain intensity scales in younger and older adult cohorts using controlled clinical pain: A preliminary study. Pain Medicine. 2007;8:585–600. doi: 10.1111/j.1526-4637.2007.00316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herr KA, Spratt K, Mobily PR, Richardson G. Pain intensity assessment in older adults: Use of experimental pain to compare psychometric properties and usability of selected pain scales with younger adults. The Clinical Journal of Pain. 2004;20:207–219. doi: 10.1097/00002508-200407000-00002. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/15218405. [DOI] [PubMed] [Google Scholar]
- Hirschmann MT, Testa E, Amsler F, Friederich NF. The unhappy total knee arthroplasty (TKA) patient: Higher WOMAC and lower KSS in depressed patients prior and after TKA. Knee Surgery, Sports Traumatology, Arthroscopy. 2013;21:2405–2411. doi: 10.1007/s00167-013-2409-z. [DOI] [PubMed] [Google Scholar]
- Ip HY, Abrishami A, Peng PW, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: A qualitative systematic review. Anesthesiology. 2009;111:657–677. doi: 10.1097/ALN.0b013e3181aae87a. [DOI] [PubMed] [Google Scholar]
- Kain ZN, Sevarino F, Alexander GM, Pincus S, Mayes LC. Preoperative anxiety and postoperative pain in women undergoing hysterectomy. Journal of Psychosomatic Research. 2000;49:417–422. doi: 10.1016/s0022-3999(00)00189-6. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11182434. [DOI] [PubMed] [Google Scholar]
- Kapstad H, Hanestad BR, Langeland N, Rustoen T, Stavem K. Cutpoints for mild, moderate and severe pain in patients with osteoarthritis of the hip or knee ready for joint replacement surgery. BMC Musculoskeletal Disorders. 2008;9:55. doi: 10.1186/1471-2474-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knotkova H, Crawford Clark W, Mokrejs P, Padour F, Kuhl J. What do ratings on unidimensional pain and emotion scales really mean? A Multidimensional Affect and Pain Survey (MAPS) analysis of cancer patient responses. Journal of Pain and Symptom Management. 2004;28:19–27. doi: 10.1016/j.jpainsymman.2003.11.003. [DOI] [PubMed] [Google Scholar]
- Leo RJ. Chronic pain and comorbid depression. Current Treatment Options in Neurology. 2005;7:403–412. doi: 10.1007/s11940-005-0032-0. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/16079044. [DOI] [PubMed] [Google Scholar]
- Lewis GN, Rice DA, McNair PJ, Kluger M. Predictors of persistent pain after total knee arthroplasty: A systematic review and meta-analysis. British Journal of Anaesthesia. 2015;114:551–561. doi: 10.1093/bja/aeu441. [DOI] [PubMed] [Google Scholar]
- Mears DC. CORR insights((R)): Does preoperative psychologic distress influence pain, function, and quality of life after TKA? Clinical Orthopaedics and Related Research®. 2014;472:2466–2467. doi: 10.1007/s11999-014-3623-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noiseux NO, Callaghan JJ, Clark CR, Zimmerman MB, Sluka KA, Rakel BA. Preoperative predictors of pain following total knee arthroplasty. The Journal of Arthroplasty. 2014;29:1383–1387. doi: 10.1016/j.arth.2014.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: A critical review. Expert Review of Neurotherapeutics. 2009;9:745–758. doi: 10.1586/ern.09.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakel BA, Blodgett NP, Zimmerman MB, Logsden-Sackett N, Clark C, Noiseux N, … Sluka KA. Predictors of postoperative movement and resting pain following total knee replacement. Pain. 2012;153:2192–2203. doi: 10.1016/j.pain.2012.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakel BA, Zimmerman MB, Geasland K, Embree J, Clark CR, Noiseux NO, … Sluka KA. Transcutaneous electrical nerve stimulation for the control of pain during rehabilitation after total knee arthroplasty: A randomized, blinded, placebo-controlled trial. Pain. 2014;155:2599–2611. doi: 10.1016/j.pain.2014.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhudy JL, Meagher MW. Fear and anxiety: Divergent effects on human pain thresholds. Pain. 2000;84:65–75. doi: 10.1016/S0304-3959(99)00183-9. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/10601674. [DOI] [PubMed] [Google Scholar]
- Rinaldi P, Mecocci P, Benedetti C, Ercolani S, Bregnocchi M, Menculini G, Cherubini A. Validation of the five-item geriatric depression scale in elderly subjects in three different settings. Journal of the American Geriatrics Society. 2003;51:694–698. doi: 10.1034/j.1600-0579.2003.00216.x. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12752847. [DOI] [PubMed] [Google Scholar]
- Roditi D, Robinson ME. The role of psychological interventions in the management of patients with chronic pain. Psychology Research and Behavior Management. 2011;4:41–49. doi: 10.2147/PRBM.S15375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Severeijns R, Vlaeyen JW, van den Hout MA, Weber WE. Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. The Clinical Journal of Pain. 2001;17:165–172. doi: 10.1097/00002508-200106000-00009. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/11444718. [DOI] [PubMed] [Google Scholar]
- Singh JA, Lewallen DG. Time trends in the characteristics of patients undergoing primary total knee arthroplasty. Arthritis Care & Research. 2014;66:897–906. doi: 10.1002/acr.22233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srikandarajah S, Gilron I. Systematic review of movement-evoked pain versus pain at rest in postsurgical clinical trials and meta-analyses: A fundamental distinction requiring standardized measurement. Pain. 2011;152:1734–1739. doi: 10.1016/j.pain.2011.02.008. [DOI] [PubMed] [Google Scholar]
- Sullivan MJ. The pain catastrophizing scale: User manual. Montreal: McGill University; 2009. [Google Scholar]
- Sullivan MJ, Bishop SR. The pain catastrophizing scale: Development and validation. Psychological Assessment. 1995;4:524–532. [Google Scholar]
- Sullivan MJL, Bishop S, Pivik J. The pain catastrophizing scale: Development and validation. Psychological Assessment. 1995;7:524–532. [Google Scholar]
- Tang J, Gibson SJ. A psychophysical evaluation of the relationship between trait anxiety, pain perception, and induced state anxiety. The Journal of Pain. 2005;6:612–619. doi: 10.1016/j.jpain.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Turner JA, Jensen MP, Warms CA, Cardenas DD. Catastrophizing is associated with pain intensity, psychological distress, and pain-related disability among individuals with chronic pain after spinal cord injury. Pain. 2002;98:127–134. doi: 10.1016/s0304-3959(02)00045-3. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12098624. [DOI] [PubMed] [Google Scholar]
- Utrillas-Compaired A, De la Torre-Escuredo BJ, Tebar-Martinez AJ, Asunsolo-Del Barco A. Does preoperative psychologic distress influence pain, function, and quality of life after TKA? Clinical Orthopaedics and Related Research. 2014;472:2457–2465. doi: 10.1007/s11999-014-3570-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Manen MD, Nace J, Mont MA. Management of primary knee osteoarthritis and indications for total knee arthroplasty for general practitioners. Journal of the American Osteopathic Association. 2012;112:709–715. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23139341. [PubMed] [Google Scholar]
- Wells N, Ridner SH. Examining pain-related distress in relation to pain intensity and psychological distress. Research in Nursing & Health. 2008;31:52–62. doi: 10.1002/nur.20262. [DOI] [PubMed] [Google Scholar]
- Williamson A, Hoggart B. Pain: A review of three commonly used pain rating scales. Journal of Clinical Nursing. 2005;14:798–804. doi: 10.1111/j.1365-2702.2005.01121.x. [DOI] [PubMed] [Google Scholar]
- Woo AK. Depression and anxiety in pain. Rev Pain. 2010;4:8–12. doi: 10.1177/204946371000400103. [DOI] [PMC free article] [PubMed] [Google Scholar]