Abstract
Pentraxins are a superfamily of fluid phase pattern recognition molecules conserved in evolution and characterized by a cyclic multimeric structure. C reactive protein (CRP) and serum amyloid P component (SAP) constitute the short pentraxin arm of the superfamily. CRP and SAP are produced in the liver in response to IL-6 and are acute phase reactants in humans and mice respectively. In addition SAP has been shown to affect tissue remodeling and fibrosis by stabilizing all types of amyloid fibrils and by regulating monocyte to fibrocyte differentiation. Pentraxin 3 (PTX3) is the prototype of the long pentraxin arm. Gene targeted mice and genetic and epigenetic studies in humans suggest that PTX3 plays essential non-redundant roles in innate immunity and inflammation as well as in tissue remodeling. Recent studies have revealed the role of PTX3 as extrinsic oncosuppressor able to tune cancer-related inflammation. In addition, at acidic pH PTX3 can interact with provisional matrix components promoting inflammatory matrix remodeling. Thus acidification during tissue repair sets PTX3 in a tissue remodeling and repair mode, suggesting that matrix and microbial recognition are common, ancestral features of the humoral arm of innate immunity.
Keywords: Pentraxin, innate immunity, inflammation, pattern recognition molecules, clinical biomarker
Introduction
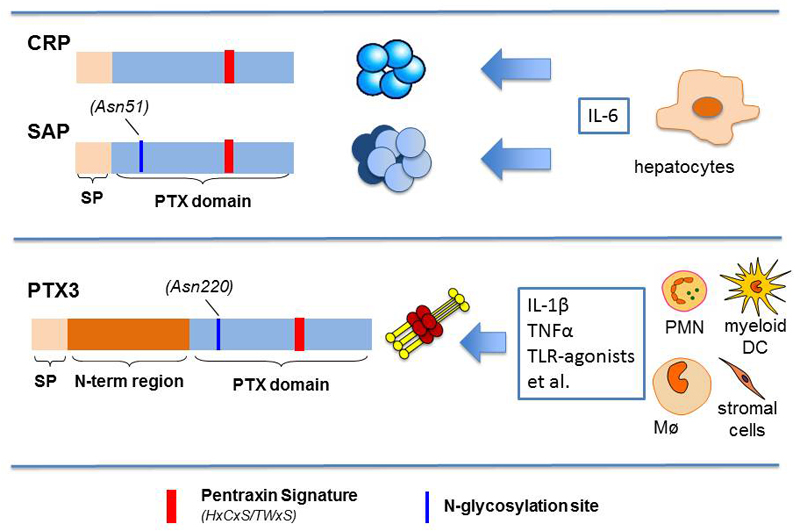
Innate immunity is the first strategy evolved to enable host defence from invading pathogens and to promote tissue growth and repair during development or following sterile tissue damage [1]. The innate immune response is activated when conserved structures on the surface of pathogens, the so called pathogen associated molecular patterns (PAMPs), are recognized by a set of cell-associated or soluble molecules collectively known as pattern recognition molecules (PRMs). Among soluble PRMs, pentraxins are a superfamily of evolutionarily conserved molecules with regulatory role in inflammation. Prototypes of the pentraxin family are C-reactive protein (CRP) and serum amyloid P component (SAP), short or “classical” pentraxins produced by hepatocytes in the liver in response to interleukin (IL)-6 (Figure 1), and main acute phase proteins in man and mouse respectively [2, 3]. Pentraxin 3 (PTX3), identified more recently, is the prototype of the long pentraxin subfamily [3]. PTX3 is expressed and released by haematopoietic and stromal cells in response to primary proinflammatory stimuli, and is an essential component of the humoral arm of innate immunity, participating in innate resistance to pathogens, regulation of inflammation, and tissue remodelling. Genetic data have prompted the ongoing clinical development of PTX3 as a candidate therapeutic agent for opportunistic infections.
Figure 1. Schematic representation of prototypes of the Pentraxin superfamily.
Short pentraxins CRP and SAP are secreted proteins produced by hepatocytes in response to IL-6. They contain a pentraxin signature characteristic of all the member of the Pentraxin family. PTX3 is the prototype of the long pentraxin subfamily produced by myeloid and stromal cells, but not by hepatocytes, in response to primary pro-inflammatory cytokines or microbial moieties. PTX3 is characterized by a pentraxin domain homologous to CRP and SAP, containing the pentraxin signature, and a long N-terminal domain unrelated to other known proteins.
Here we will review the main biological features of the three prototypic pentraxins with a major focus on PTX3. Based on recent results we provide evidences that microbial and matrix recognition are conserved functions of humoral innate immunity molecules.
The pentraxin family
Pentraxins are phylogenetically conserved, multimeric proteins that share a ~200 amino acids long domain with a distinctive primary motif, the so called “pentraxin signature” (His-x-Cys-x-Ser/Thr-Trp-x-Ser, where x is any amino acid) [3]. Based on structural organization, this family is divided into a short and a long arm. CRP and SAP, the prototypic short (or classical) pentraxins, feature a peculiar quaternary structure with five or ten identical protomer subunits arranged into symmetric pentamers [4]. Long pentraxins, on the other end, display an unrelated amino-terminal region coupled to a C-terminal pentraxin domain, and differ from the short counterparts in chromosomal localization, gene expression, cellular source and ligands [5]. First identified in the early 1990s as a cytokine-inducible gene in endothelial cells (ECs) and fibroblasts, PTX3 is the paradigm of the long arm of this family [6]. Other long pentraxins have been described, including guinea pig apexin in spermatozoa, neuronal pentraxin 1 (NP1 or NPTX1), NP2 (also called Narp or NPTX2) and neuronal pentraxin receptor (NPR), a transmembrane protein on neurons [5]. More recently, we discovered a new entry, PTX4, with a unique pattern of expression [7].
Gene regulation and protein structure
The human CRP gene has been mapped in the chromosome 1q23.2 locus and comprises two exons, the first coding for the leader peptide (1-18) and the initial two amino acids of the mature protein (19-20), the second for the remaining 21-224 sequence [8, 9]. The expressed protein is made of five identical non-glycosylated subunits, whose tertiary structure is stabilized by an intra-chain disulfide bond (Cys36-Cys97), highly conserved amongst pentraxins [10]. The human SAP gene has been identified as close paralog of CRP on chromosome 1, where the two genes share the same exon/intron architecture, and code for 51% identical protein sequences. SAP is a plasma glycoprotein that comprises 5 or 10 subunits, which again non-covalently associate into pentameric rings. As opposed to CRP, human SAP carries a single N-glycosylation site at Asn32 that is occupied by complex type oligosaccharide [4]. X-ray crystallography allowed generating 3D atomic models of both short pentraxins in association with small ligands. Based on these, CRP and SAP protomers adopt a flattened jelly-roll topology, analogous to lectins, and expose composite binding sites on opposite sides of the pentamers [4, 11, 12]. Moreover, modelling of the SAP/FcγRIIa complex has provided a general structural frame for the interaction of pentraxins with FcRs [13], and highlighted similarities to antibody recognition by these receptors, thus bridging molecular functions of the innate and adaptive immune systems [14].
CRP and SAP are soluble PRMs in the serum. As such, they recognize Pathogen Associated Molecular Patterns (PAMPs) as well as membrane phospholipids and nuclear components (collectively known as Danger Associated Molecular Patterns, DAMPs) that appear on and are released by host cells at sites of injury [15]. Indeed, CRP and SAP can opsonize microbial pathogens and apoptotic cells, and promote their Complement-mediated clearance [16]. Their synthesis mainly occurs in the liver and is primarily induced by IL-6, typically as a reaction to microbial challenge or tissue damage. CRP expression has been reported in other tissues than liver, however extra-hepatic sites marginally contribute to the plasma levels of this protein [17]. CRP is a major acute phase protein in humans, with levels ranging from 5 mg/l at baseline up to 1000-fold higher in the acute response [18]. Therefore, since its first report in the 1930’s, CRP has found extensive clinical applications as a sensitive yet non-specific systemic marker of infection, inflammation, and tissue damage [2]. SAP is an acute phase protein in the mouse, whereas its levels in the human serum are constitutively found in the 30-50 mg/l range [19].
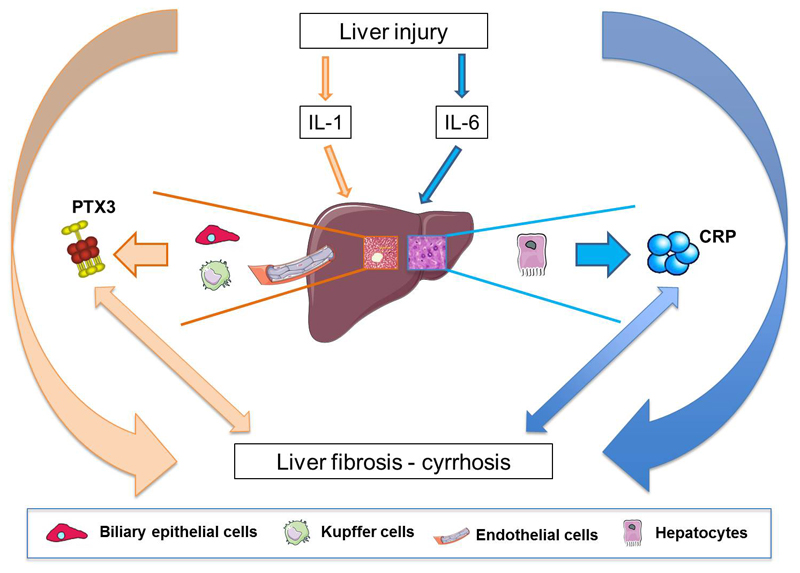
The human and murine Ptx3 genes both localize on chromosome 3 and comprise three exons, which code for the leader peptide, N- and C-terminal domains of the protein, respectively. Proximal promoters of both genes share several regulatory elements, including Pu1, AP-1, NF-κB, SP1, and NF-IL-6. The NF-κB site is required for the transcriptional response of Ptx3 to TNF-α and IL-1β, while AP-1 mediates its basal transcription [6, 20, 21]. In addition to inflammatory cytokines, Toll-like receptor (TLR) agonists, like microbial moieties (e.g. LPS, OmpA, lipoarabinomannans) and intact microorganisms, can rapidly induce PTX3 expression in several cell types, including myeloid dendritic cells (DC), macrophages, ECs, fibroblasts, kidney epithelial cells, synovial cells, chondrocytes, adipocytes, alveolar epithelial cells, glial cells, mesangial cells and granulosa cells [22]. Furthermore, both oxidized and enzymatically modified low density lipoproteins (ox-LDL) and anti-inflammatory high-density lipoproteins (HDL) promote PTX3 production in ECs and human primary vascular smooth muscle cells (SMCs) [23, 24]. As opposed to these cells, PTX3 is constitutively expressed both in human and murine lymphatic ECs [25]. Interestingly, neutrophils lack de novo synthesis of PTX3, however their specific granules contain a reservoir of pre-made protein that is promptly released in response to TLR engagement, and partially localizes in the extracellular traps (NETs) [26]. Neither resting T and B lymphocytes nor natural killer cells express PTX3 mRNA. In sharp contrast to the short pentraxins, hepatocytes do not make PTX3 [27, 28], whereas in injured liver Kupffer cells, endothelial cells and biliary epithelial cells can produce the protein (Figure 2), and IL-6 does not induce PTX3 synthesis in competent cells, thus highlighting a local rather than systemic activity of this long pentraxin [15]. In addition, IFN-γ inhibits PTX3 production in DCs, monocytes and macrophages, whereas IL-10 amplifies its LPS-dependent expression [29]. IL-4, dexamethasone, 1,25-dihydroxivitamin D3 and prostaglandin E2 also inhibit LPS-induced PTX3 in myeloid DCs [29]. Glucocorticoids can either inhibit PTX3 production in hematopoietic cells (e.g., DCs and macrophages) or induce its expression in non-hematopoietic cells (e.g., fibroblasts and ECs), due to differences in signal transduction by Glucocorticoid receptors in these cell lineages [30].
Figure 2. Production of short and long pentraxins in the liver.
Liver hepatocytes are the main source of CRP in response to IL-6, while IL-1 induces PTX3 production by Kupffer cells, endothelial cells and biliary epithelial cells. Production of short and long pentraxins in response to liver injury suggests a possible use of these molecules as biomarkers of liver fibrosis.
PTX3 is a homo-multimeric glycoprotein made of 8 protomer subunits, each containing 381 amino acids, including a 17aa signal peptide [6]. Like other long pentraxins, the PTX3 protein comprises a unique N-terminal region (residues 18-178 in the preprotein) and a C-terminal domain (residues 179–381 of the preprotein) homologous to the short pentraxins (with up to 57% similarity) [31]. The N-terminal region is unrelated to any known protein structure, however secondary structure predictions suggest that this domain contains coiled-coil elements, which likely drive the quaternary assembly of the protein [32]. 3D models of the C-terminal pentraxin domain have been generated instead, based on the crystal structures of CRP and SAP, that show this region to adopt a jelly roll topology, typical of the family [5, 33, 34]. Interestingly, the calcium-binding pocket of CRP and SAP is missing in the pentraxin domain of PTX3, which might explain some differences in the binding properties across these pentraxins (i.e., calcium is not required for the interaction of PTX3 with C1q). A single N-glycosylation site has been identified in the C-terminal domain of PTX3 at Asn220, which is fully occupied by core-fucosylated and sialylated complex type oligosaccharides. This glycosidic moiety modulates the interaction of PTX3 with other soluble PRMs, including C1q [34], factor H [35] and ficolin-1 [36], and is required for recognition of influenza virus [37] and engagement of P-selectin [38]. Biophysical investigations indicate that the PTX3 octamer has an elongated conformation with a large and a small domain interconnected by a stalk region [32]. The rather unique quaternary structure and protein glycosylation status dictate ligands recognition by PTX3 and, ultimately, the biological functions of this prototypic long pentraxin [32, 39].
Pentraxins and regulation of cell recruitment
Pentraxins participate in the regulation of the inflammatory response through different mechanisms. PTX3 and SAP, but not CRP, interact with P-selectin [38]. While the consequences of SAP interaction with P-selectin have not been investigated, the functional relevance of PTX3 binding to P-selectin has been analysed in in vivo models of leukocyte recruitment [40]. In a pleurisy model of leukocyte recruitment shown to be P-selectin-dependent, PTX3 blocked early neutrophil accumulation in response to inflammatory stimuli. Moreover, ptx3-/- mice showed greater recruitment of neutrophils in the same model, demonstrating the involvement of PTX3 in regulation of the magnitude of early leukocyte influx. Similar data were also obtained in a murine models of acid induced acute lung injury [38], and kidney ischemia and reperfusion [41]. Based on these data, it has been proposed a role for PTX3 as negative feedback mechanism governing regulation of early neutrophil recruitment. Thus, PTX3 might act as an intrinsic fine-regulator of initial inflammatory response, possibly limiting excessive inflammation-induced tissue damage.
Crosstalk with the Complement system
The Complement system is an important regulator of the inflammatory response. Pentraxins recognize a number of Complement components, and shape activation of this primordial system in a variety of physiopathological settings, including infection, inflammation and cancer [42].
Both CRP and SAP, in an aggregated or ligand-bound form, interact with C1q, the recognition unit of the classical Complement pathway (CCP), and lead to activation of CCP on pathogens [43]. In addition, CRP can synergize with ficolins in amplifying the effector functions of the lectin pathway (LCP) on bacteria, like Salmonella enterica [44]. The crosstalk between these two protein families might also contribute to removal of cellular debris, thus subsidizing tissue homeostasis [43]. For instance, when bound to self-antigens (e.g. apoptotic cells, damaged tissue), CRP retains the ability to enhance CCP activation, however this effect is restricted to the initial stages of the proteolytic cascade, with little deposition of the late components C5–C9 [45]. However, whether these short pentraxins exert protective or pathogenetic roles in Complement-mediated inflammation is still controversial [2, 46, 47]. Nonetheless, surface-bound CRP engages in a complex with factor H, the major soluble inhibitor of the alternative pathway (ACP), and inhibits ACP deposition [48, 49]. In addition, both CRP and SAP bind C4b binding protein (C4BP), the main soluble inhibitor of CCP and LCP [50, 51]. These processes might restrain Complement activation and prevent tissue injury, especially where the regulatory functions of factor H and C4BP are impaired, like in the case of factor H mutations and autoantibodies associated with atypical hemolytic uraemic syndrome (aHUS) and age-related macular degeneration (AMD) [52].
C1q is the first PTX3 ligand ever identified and, unlike short pentraxins, binding of PTX3 to C1q requires neither protein aggregation nor calcium ions [53, 54]. This interaction has opposite functional outcomes, depending on settings; when immobilized on a surface, PTX3 induces CCP deposition, whereas it inhibits this cascade in solution, possibly due to competitive blocking of activating sites on C1q [53]. PTX3 also recognizes LCP components, namely ficolin-1, ficolin-2 and mannose-binding lectin (MBL) [36, 55, 56]. In particular, the association with ficolin-2 or MBL results in a functional cooperation that promotes recruitment of either molecules onto microbial pathogens (i.e., Aspergillus fumigatus, Candida albicans) and LCP amplification [55, 56]. We have described a tight cooperation between PTX3 and ACP in a non-redundant protective mechanism against A. fumigatus [57]. Furthermore, similar to the short pentraxins, PTX3 binds factor H and C4BP [35, 58]. The interaction with factor H down-modulates ACP by promoting factor H recruitment onto PTX3-coated surfaces and preventing exaggerated Complement activation [35]. It has been reported that aHUS-associated mutations within the PTX3 binding region of factor H and factor H autoantibodies inhibit the interaction of factor H with PTX3 [59]. In addition, PTX3 recruits C4BP onto apoptotic cells or extracellular matrix (ECM), increasing the rate of C4b inactivation and reducing deposition of the lytic C5b-9 terminal complex [58]. Most interestingly, we have recently described that PTX3 can act as an extrinsic oncosuppressor gene by regulating Complement-dependent, macrophage-sustained, tumor-promoting inflammation [60] (see below).
Other than Complement, both PTX3 and short pentraxins share with antibodies the interaction with FcR. In this regard, SAP and IgGs bind FcγR with similar affinity, compete for common sites on FcγR, and inhibit immune-complex-mediated phagocytosis [13]. Furthermore, CRP and SAP, but not PTX3, bind FcαRI, and the CRP-dependent crosslinking of FcαRI leads to activation of macrophages (i.e., ERK phosphorylation, cytokine production, degranulation) and enhanced phagocytosis and TNF-α secretion in neutrophils [61]. Thus, pentraxins and antibodies have similar ancestral functions, and activate both Complement and FcγR/FcαR pathways [62].
Resistance to infections
The first ligand described for CRP was the C-polysaccharide of Streptococcus pneumoniae to which CRP binds through phosphorylcholine (PC), a major constituent of C-type capsule polysaccharides. Moreover, CRP binds various microorganisms, including fungi, yeasts, bacteria (e.g. S. pneumoniae, Hemophilus influenzae, Salmonella thyphimurium), and parasites (Plasmodium, Leishmania) through PC and carbohydrate structures, promoting Complement activation, opsonization, phagocytosis and resistance to infections [63]. Like CRP, SAP binds various bacteria, such as Streptococcus pyogenes and Neisseria meningitidis, and to influenza virus, playing a protective role [63, 64]. SAP binds to lipopolysaccharide (LPS), but controversial consequences have been described in SAP-deficient mice challenged in endotoxemia models [65]. SAP also interacts with and neutralizes Shiga toxin 2, the main mediator of sever hemorrhagic colitis and hemolytic uremic syndrome that occurs following ingestion of enterohemorrhagic E. coli O157:H7 [66]. FcRs and Complement are recognized as key systems in the CRP- and SAP-dependent immune response to infections [14]. Furthermore, this interaction of both short pentraxins with FcαRI might have additional implications in liver cirrhosis-associated infections for example by compensating defective mucosal IgA-mediated response observed in cirrhotic patients [67, 68].
PTX3 was originally described as a humoral patterns recognition molecule exerting a protective role in resistance against selected fungal (Aspergillus fumigatus) and bacterial (Pseudomonas aeruginosa) pathogens [69]. Its non-redundant protective role in innate resistance to infections was extended to Paracoccidoides brasiliensis, Klebsiella pneumoniae, and viruses, such as influenza virus [37, 70]. PTX3 was shown to act as an opsonin for bacteria and fungi, facilitating recognition and phagocytosis by myeloid cells in an Complement- and FcγR-dependent manner, and by neutralizing virus infectivity [15].
In addition to these data, it has been recently shown that human colostrum contains high levels of PTX3, and that mammary epithelial cell and myeloid milk cells constitutively produce PTX3. In addition, orally administered PTX3 provided protection against Pseudomonas aeruginosa lung infection in neonate mice, suggesting that breastfeeding constitutes an important source of PTX3, which contributes to innate resistance to infections of neonates [71]. In addition, PTX3 emerged as an essential component of the innate resistance against uropathogenic Escherichia coli, playing a non-redundant role both in animal models and in humans in urinary tract infections [72]. In particular, PTX3, which is produced locally by the uroepithelium and by infiltrating myelomonocytic cells in a TLR4/MyD88-dependent manner, bound E. coli and facilitated the clearance of microbes by phagocytosis, and tuned detrimental local inflammatory responses and tissue damage [72]. PTX3 was also shown to reduce the bacterial load in an infant rat model of meningococcal meningitis by interacting with acapsular Neisseria meningitidis, through outer membrane vesicles and selected meningococcal antigens, and acting as an amplifier of humoral responses to this bacterium [73].
Like for SAP, the interaction between PTX3 and certain influenza A viruses occurs through sialic acids expressed on the glycosidic moiety of PTX3 and the viral hemagglutinin (HA) glycoprotein, and results in virus neutralization and anti-viral activity. The specificity of this interaction determines the susceptibility of H1N1, H3N2, and H7N9 strains to the antiviral activities of PTX3 and SAP [37, 70]. It has recently been shown that amino acid residues in the vicinity of the receptor-binding pocket of HA are critical determinants of sensitivity to PTX3, and that in a mouse model of infection, PTX3-resistant mutants were responsible of increased virus replication, pulmonary inflammation and lung injury [74]. In contrast with the protective role in influenza virus infection, PTX3 was shown to interact to arthritogenic alphaviruses (chikungunya virus and Ross River virus) through the N-terminal domain, and to facilitate viral entry and replication during the acute phase of infection, leading to enhanced viral infectivity and prolonged disease [75].
PTX3 genetic variants have been recently described and associated with susceptibility to different infections, in particular pulmonary tuberculosis [76], Pseudomonas aeruginosa infections in cystic fibrosis Caucasian patients [77], Aspergillus fumigatus infections in patients undergoing hematopoietic stem cell transplantation [78], fungal infections in solid organ transplanted patients [79], and urinary tract infections [72], thus suggesting the relevance of functional evolutionary conservation of PTX3 in innate immunity. The protective haplotypes are associated to higher protein expression and circulating levels [78, 80], through still poorly understood molecular mechanisms.
Role of Pentraxins in tissue remodelling and repair
Several lines of evidence indicate that pentraxins are involved in tissue remodelling both in physiological and pathological conditions. SAP is a normal tissue protein as well as a plasma protein. It selectively binds fibronectin and is an abundant nonfibrillar component of all amyloid deposits of systemic amyloidosis, because it avidly binds to and stabilizes all types of amyloid fibrils. It was recently shown that the administration of a small-molecule drug (CPHPC), which effectively depletes circulating SAP, and reduced SAP from systemic amyloid deposits, followed by a monoclonal anti-SAP antibody, which activates Complement- and macrophage-dependent destruction of the SAP-containing amyloid deposits in tissues, safely cleared amyloid deposits and had therapeutic effects both in mice and humans [81, 82].
The involvement of PTX3 in tissue remodelling in physiological conditions was originally identified thanks to the sterility of PTX3-deficient mice [83]. Indeed, PTX3-deficient female mice display a severe deficiency in fertility, which has been attributed to defective assembly of the viscoelastic hyaluronan (HA)-rich matrix that forms around the oocyte in the preovulatory follicle, where correct deposition of cumulus matrix is necessary for fertilization in vivo. Besides PTX3 other molecules are required for effective incorporation of the newly synthesised HA into the matrix, including the HA-binding proteins tumor necrosis factor α-induced protein 6 (TNFAIP6 or TSG-6) and the serum proteoglycan inter-α-trypsin inhibitor (IαI). In fact, genetic or functional deletion of IαI or TSG-6 lead to impaired cumulus matrix formation and severe sub-fertility, a similar phenotype to that observed in Ptx3−/− mice [84]. PTX3 is produced by mouse cumulus cells during cumulus expansion and localizes within the matrix, where thanks to its multimeric organisation, it establishes multiple contacts with TSG-6 and IαI, thus providing structural integrity to the cumulus matrix [83, 85]. Tetramers of the PTX3 N-terminal domain are sufficient to sustain the assembly of the cumulus matrix [85], suggesting that PTX3 N-terminal domain alone might have functional activities.
Innate immunity has an important role in regulating inflammatory, remodelling and repair responses after tissue injury [1]. Among humoral components of innate immunity involved in tissue injury, SAP was shown to be involved in wound healing and regulation of fibrosis. In particular, SAP-deficient mice are more susceptible to bleomicin-induced lung fibrosis [86] and SAP was shown to prevent the differentiation of monocytes into fibroblast-like cells (fibrocytes) in vitro in part by interacting with FcγRI and delay normal murine dermal wound healing, through this mechanism [87]. Furthermore, animal studies and human phase 1 and phase 2 clinical trials showed that treatment with SAP decreases fibrosis in chronic fibrosing conditions, such as interstitial pulmonary fibrosis and myelofibrosis [88]. It has been recently shown that SAP plays anti-fibrotic effects independently from the interaction with FcγRI [89]. Indeed, in the absence of FcγR, SAP reduced but did not completely inhibit fibrocyte differentiation.
Fibrogenesis plays a crucial role in nonalcoholic fatty liver disease (NAFLD), the most common liver disease in Western Countries, with a prevalence of 25-30% in the general population [90]. Most patients have a simple hepatic steatosis without inflammation, but in a subgroup of patients progressive nonalcoholic steatohepatitis (NASH), fibrosis and cirrhosis may develop. Given that patients with advanced liver fibrosis and cirrhosis are at high risk for complications such as hepatocellular carcinoma, the development of non-invasive diagnostic and prognostic methods for the screening are crucial. CRP and PTX3 were found significantly elevated in patients with NASH compared to non-NASH, and levels were associated with the degree of fibrosis [91–93]. PTX3 levels are also increased in paracetamol-induced acute liver injury [27], correlating with severity. These data suggest that both CRP and PTX3 may be of clinical utility as biomarkers to distinguish NASH from NAFLD and to indicate the severity of hepatic fibrosis. However these results were not confirmed in a recent study [94], indicating that a more extensive analysis on the role of CRP and PTX3 as biomarkers of NAFLD and related diseases should be performed.
Unexpectedly, it has been shown that SAP binds the receptor DC-SIGN and a polycyclic aminothiazole DC-SIGN ligand mimicked SAP effects in vitro and in an in vivo model of pulmonary fibrosis by inducing IL-10 in lung epithelial cells. In the same conditions, PTX3 promoted the differentiation of human and murine monocytes to fibrocytes, acting through FcγRI [95]. Recently, it has been shown that PTX3 plays a non-redundant role in tissue repair and remodelling, but through a different mode of action [28]. In different models of tissue damage (skin wound healing, chemically-induced sterile liver and lung injury, arterial thrombosis) PTX3-deficiency was associated with increased clot formation, fibrin deposition and persistence, followed by increased collagen deposition. In these conditions of damage, macrophages and mesenchymal cells produced PTX3 in response to TLR activation and amplification by IL-1, which localized in the pericellular matrix of macrophages and mesenchymal remodelling cells. PTX3-deficient remodelling cells showed defective pericellular fibrinolysis in vitro and defective directional collective migration in the provisional fibrin-rich inflammatory matrix in vivo. In addition to skin wounding, the study was extended to CCL4-induced liver sterile injury. Upon injury, PTX3 localized in necroinflammatory areas associated with myeloid cells at early time points, and in the portal tracts associated with remodelling mesenchymal cells and macrophages in the resolution phase, whereas hepatocytes were not a source of PTX3 upon damage. PTX3 deficiency did not affect liver necrosis but it was associated with an increased number of thrombosed centrolobular veins in the acute phase of damage, and increased deposits of fibrin followed by augmented liver fibrosis. This phenotype is similar to that observed in mice with genetic modifications causing prothrombotic responses, which are associated with impaired liver tissue remodelling and fibrosis [96, 97]. In agreement with these data, the phenotype of PTX3-deficient mice in skin and liver damage was attributed to the interaction of PTX3 with fibrin and plasminogen at acidic pH, occurring in vivo in conditions of tissue damage-associated hypoperfusion and hypoxia, and to facilitated plasminogen-dependent fibrinolysis. Promotion of fibrinolysis is peculiar for PTX3, since the second exon-encoded non-pentraxin N-terminal domain of PTX3 was responsible for the interaction with fibrin and plasminogen and rescued the phenotype, whereas CRP did not interact with fibrin or plasminogen. Upon injury, fibrin acts as a provisional matrix protein and its timely remodelling plays a major role for subsequent normal repair, as demonstrated by the phenotype of mice with genetic deficiency of components of the fibrinolytic pathway [98]. The phenotype of ptx3-/- mice was abrogated by in vivo administration of selective inhibitors of fibrin deposition and platelet activation demonstrating that an altered fibrinolytic response to injury was responsible for the defective wound healing. These data indicate that PTX3-dependent promotion of fibrin-rich inflammatory matrix remodelling ensures a normal tissue repair, providing a novel link between innate immunity, haemostasis and tissue repair [99].
Role in Cancer-Related Inflammation
The concept that cancer has a strong connection with chronic inflammation, whether sustained by infections (e.g. hepatitis) or inflammatory conditions of diverse origin (e.g. prostatitis), is nowadays generally accepted [100]. Given the involvement of pentraxins in regulation of inflammation, it is expected a role of these molecules in the control of tumor development. Lack of genetic approaches has precluded the investigations on the role of CRP in in vivo models of carcinogenesis. However different reports have associated increased plasma levels of CRP with overall cancer risk and risks of lung, colorectum, endometrium, pancreatic and ovarian cancers [101–107]. Along the same line, emerging evidences indicate an elevated PTX3 expression in malignant cancer (e.g. glioma, liposarcoma, lung cancer, prostate carcinoma, pancreatic carcinoma, breast cancer metastatic to bones) [108–112]. Gene expression profiling applied to identify signatures correlating with clinical outcome in molecular subtypes of ovarian cancer, identified PTX3 as one of the modulated genes belonging to the stromal response/extracellular matrix signature associated to poor prognosis [113]. In addition a recent report associates PTX3 genetic variation with plasma levels of the protein and risk to develop hepatocellular carcinoma in hepatitis C virus infected subjects [114].
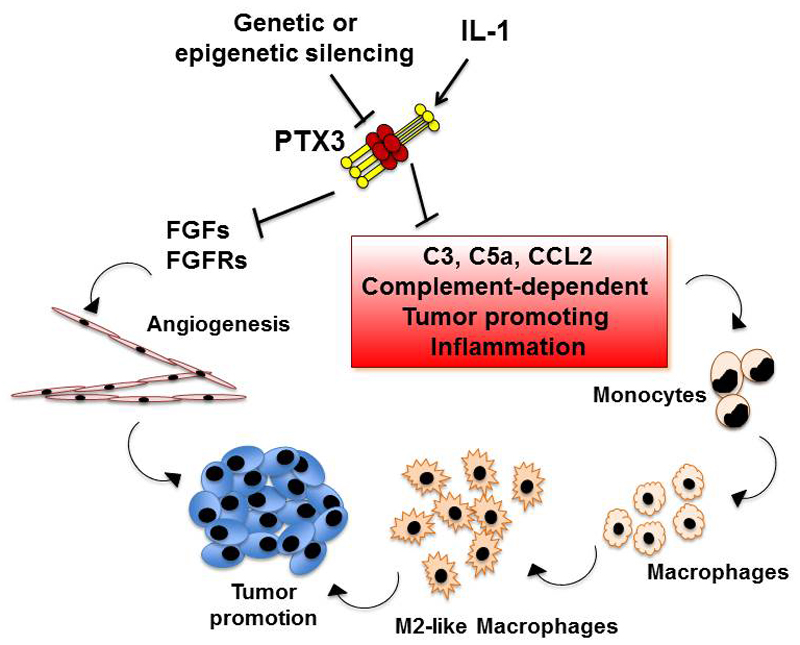
PTX3 promoter hypermethylation and consequent reduced PTX3 expression was reported in human esophageal squamous cell carcinoma [115], and in selected human mesenchymal and epithelial tumors [60]. Treatment of cancer cells with a methylation inhibitor (5-Aza-2’-deoxycytidine) rescued PTX3 protein expression, suggesting that PTX3 could act as extrinsic oncosuppressor (Figure 3). Availability of PTX3-deficient mice allowed further investigation on the role of PTX3 in tumor development. Susceptibility to mesenchymal and skin carcinogenesis, associated to the treatment respectively with 3-Methylcholantrene and 7,12-dymethylbenx[α] anthracene/teraphtalic acid, resulted greatly increased in ptx3-/- mice [60]. A deep analysis of the two models of carcinogenesis evidenced that PTX3-deficiency was associated to a more pronounced CRI, with a higher number of tumor-infiltrating macrophages (TAM), higher production of pro-inflammatory cytokines, higher neo-angiogenesis and increased Complement C3 deposition and C5a levels. In addition, PTX3-deficient tumors are characterized by increased Trp53 mutations, increased oxidative DNA damage and increased expression of DNA damage markers. Lack of PTX3 also results in lower factor H localization and consequent higher C3 deposition and tissue damage. Deficiency of C3 or inhibition of CCL2, with the consequent reduction of TAM, were sufficient to revert the phenotype observed in ptx3-/- animals. Thus PTX3 exerts a protective role in carcinogenesis and this effect is based on the regulation of Complement activation.
Figure 3. Oncosuppressive role of PTX3.
Genetic or epigenetic silencing of PTX3 results in higher growth rate of tumors. Two pathways are involved in the oncosuppressive role of PTX3. Lack of PTX3 may results in recovery of neo-angiogenesis and higher growth rate of FGF-dependent tumors. In addition PTX3 regulates Complement activation and M2-like macrophage recruitment in the tumors, two biological functions with a tumor-promoting effect. The evidence for PTX3 acting as an extrinsic oncosuppressor by taming Complement and macrophage-driven tumor promotion is based on gene targeted mice.
A protective role of PTX3 in tumor growth has been recently reported also in transgenic mice overexpressing the protein under the control of the endothelial-specific Tie2/Tek transcription regulatory sequences [116]. In particular PTX3 overexpression was associated to a reduced growth rate of FGF2-dependent tumors (i.e. prostate cancer and melanoma models), reduced metastatization and angiogenesis [116]. PTX3 also affects cell proliferation and epithelial-mesenchymal transition (EMT) in human melanoma cells in vitro [117]. Previous work indicates that PTX3 acts as a competitor of the interaction of some FGFs (i.e. FGF2, FGF8) with their receptor [118], thus exerting an anti-angiogenic role that likely explains the reduced growth rate of FGF2-dependent tumors. As a matter of fact, pharmacophore modeling was used to identify a small molecule acting as an extracellular FGF trap and exerting a significant anti-tumor activity in vivo [116].
Beside the reports describing a protective role of PTX3 against cancer, few papers suggest a pro-tumorigenic effect. It is reported that PTX3 promotes tumor cell migration and invasion and macrophage chemotaxis [103, 119, 120]. PTX3 silencing suppresses gastric cancer-related inflammation [120], however no convincing data concerning the mechanism of action of PTX3 in this context are reported.
Two papers published in 2015 addressed the prognostic value of the neuronal pentraxins NPTX1 and NPTX2 in human neuroblastoma and lung cancer respectively [121, 122]. NPTX2 and its receptor NPTXR are overexpressed in human stage IV neuroblastoma and in vivo targeting of the two molecules reduces tumor burden in orthotopic mouse models of human neuroblastoma [121]. Hypermethylation of NPTX1 promoter was observed in lung cancer. By comparing NPTX1 mRNA expression between lung cancer samples and matched nonmalignant lung tissues it has been shown a significant down-regulation of NPTX1 expression in tumor samples. In addition promoter methylation of NPTX1 correlates with poor survival [122].
Concluding remarks
Pentraxins are a phylogenetically conserved superfamily of proteins exerting common essential functions in defence from pathogens and in tissue repair. CRP is a widely used biomarker of inflammation in humans, however lack of a strict evolutionary conservation between mouse and man have precluded the use of straightforward genetic approaches to explore its functions in vivo. On the contrary gene targeted mice have allowed defining the functional role of PTX3 in innate immunity and inflammation as functional predecessor of antibodies. Genetic and epigenetic data are consistent with the hypothesis that PTX3 exerts similar functions in humans. PTX3-dependent Complement activation, opsonization of microbes and glycosylation-dependent regulation of inflammation, prompted ongoing translation efforts aiming at its development as a novel candidate therapeutic agent. Regulation of Complement activation is also essential in the oncosuppressive role recently described for PTX3. Data obtained in carcinogenesis models in ptx3-/- mice and further sustained by epigenetic data in human tumors, pave the way to new possible therapeutic approaches.
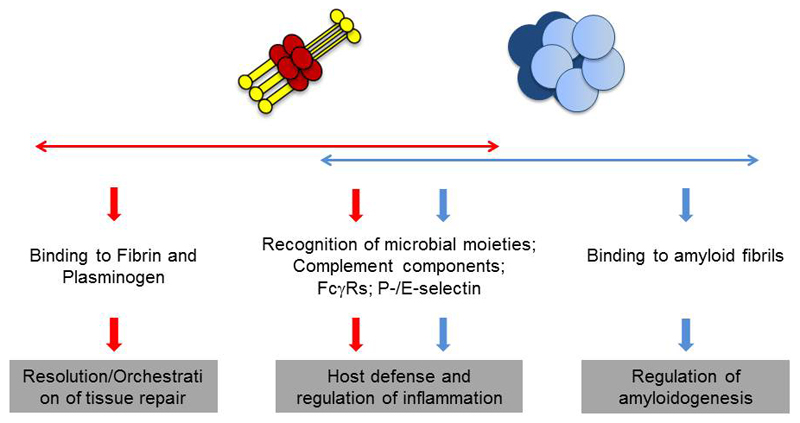
Interaction with microbes and ECM components is a common characteristic for pentraxins, in particular SAP and PTX3 (Figure 4), and collectins. In addition several ECM components (e.g. fibronectin, mindin, osteopontin, and vitronectin) interact with microbes. Among humoral PRM, ficolines and collectins contain ancestral collagen and fibrinogen domains [15]. Altogether, these data suggest the evolutionary link between microbial and ECM recognition in the humoral arm of innate immunity.
Figure 4. PTX3 and SAP share common properties in regulation of innate immunity and tissue remodelling.
Despite the structural differences, long pentraxin PTX3 and short pentraxin SAP share similar biological properties. Both have a role in innate immunity, recognizing pathogens, regulating Complement activation and promoting opsonisation through FcγR-dependent mechanisms. In addition both the molecules participate in matrix remodelling: SAP is an abundant component of all amyloid deposits and stabilizes amyloid fibrils; PTX3 orchestrates fibrin-rich inflammatory matrix remodelling.
Key Points.
Pentraxins are a superfamily of conserved proteins acting as Pathogen Recognition Molecules. CRP and SAP are prototypes of the short pentraxin subfamily while PTX3 is the prototype of the long pentraxin subfamily, being characterized by a long N-terminal domain associated to the C-terminal, pentraxin like domain.
Liver hepatocytes are the main source of short pentraxins CRP and SAP in response to Il-6, while myeloid cells, endothelial cells and stromal cells produce the long pentraxin PTX3. Primary proinflammatory signals (IL-1, TNF) and microbial components are the inducers of PTX3, outlining a local versus a systemic, IL-6 dependent production of CRP and SAP.
Pentraxins regulate Complement activity and promote microbial recognition and phagocytosis by myeloid cells in a Complement- and FcγR-dependent manner. In addition PTX3 acts as oncosuppressor gene, tuning Complement-mediated, macrophage-sustained, tumor promoting inflammation.
PTX3 and SAP exert a role in tissue remodeling suggesting that matrix and microbial recognition are related functions in evolution.
Ongoing efforts are evaluating the clinical utility of pentraxins, in particular CRP and PTX3, as candidate biomarkers useful to distinguish NASH from NAFLD.
Acknowledgments
The financial support of the European Commission (ERC-PHII, FP7-HEALTH-2011-ADITEC-N°280873), Ministero dell’Istruzione, dell’Università e della Ricerca (MIUR) (project FIRB RBAP11H2R9), Ministero della Salute (RF-2011-02348358), Cluster Alisei (MEDINTECH CTN01_00177_962865) and Italian Association for Cancer Research (AIRC) is gratefully acknowledged. AI is recipient of a Young Investigator Grant from Ministero della Salute (GR-2011-02349539).
References
- [1].Medzhitov R. Origin and physiological roles of inflammation. Nature. 2008;454:428–435. doi: 10.1038/nature07201. [DOI] [PubMed] [Google Scholar]
- [2].Casas JP, Shah T, Hingorani AD, Danesh J, Pepys MB. C-reactive protein and coronary heart disease: a critical review. J Intern Med. 2008;264:295–314. doi: 10.1111/j.1365-2796.2008.02015.x. [DOI] [PubMed] [Google Scholar]
- [3].Garlanda C, Bottazzi B, Bastone A, Mantovani A. Pentraxins at the crossroads between innate immunity, inflammation, matrix deposition, and female fertility. Annu Rev Immunol. 2005;23:337–366. doi: 10.1146/annurev.immunol.23.021704.115756. [DOI] [PubMed] [Google Scholar]
- [4].Emsley J, White HE, O'Hara BP, Oliva G, Srinivasan N, Tickle IJ, et al. Structure of pentameric human serum amyloid P component. Nature. 1994;367:338–345. doi: 10.1038/367338a0. [DOI] [PubMed] [Google Scholar]
- [5].Goodman AR, Cardozo T, Abagyan R, Altmeyer A, Wisniewski HG, Vilcek J. Long pentraxins: an emerging group of proteins with diverse functions. Cytokine Growth Factor Rev. 1996;7:191–202. doi: 10.1016/1359-6101(96)00019-6. [DOI] [PubMed] [Google Scholar]
- [6].Breviario F, d'Aniello EM, Golay J, Peri G, Bottazzi B, Bairoch A, et al. Interleukin-1-inducible genes in endothelial cells. Cloning of a new gene related to C-reactive protein and serum amyloid P component. J Biol Chem. 1992;267:22190–22197. [PubMed] [Google Scholar]
- [7].Martinez de la Torre Y, Fabbri M, Jaillon S, Bastone A, Nebuloni M, Vecchi A, et al. Evolution of the pentraxin family: the new entry PTX4. J Immunol. 2010;184:5055–5064. doi: 10.4049/jimmunol.0901672. [DOI] [PubMed] [Google Scholar]
- [8].Lei KJ, Liu T, Zon G, Soravia E, Liu TY, Goldman ND. Genomic DNA sequence for human C-reactive protein. J Biol Chem. 1985;260:13377–13383. [PubMed] [Google Scholar]
- [9].Woo P, Korenberg JR, Whitehead AS. Characterization of genomic and complementary DNA sequence of human C-reactive protein, and comparison with the complementary DNA sequence of serum amyloid P component. J Biol Chem. 1985;260:13384–13388. [PubMed] [Google Scholar]
- [10].Shrive AK, Cheetham GM, Holden D, Myles DA, Turnell WG, Volanakis JE, et al. Three dimensional structure of human C-reactive protein. Nat Struct Biol. 1996;3:346–354. doi: 10.1038/nsb0496-346. [DOI] [PubMed] [Google Scholar]
- [11].Thompson D, Pepys MB, Wood SP. The physiological structure of human C-reactive protein and its complex with phosphocholine. Structure. 1999;7:169–177. doi: 10.1016/S0969-2126(99)80023-9. [DOI] [PubMed] [Google Scholar]
- [12].Mikolajek H, Kolstoe SE, Pye VE, Mangione P, Pepys MB, Wood SP. Structural basis of ligand specificity in the human pentraxins, C-reactive protein and serum amyloid P component. J Mol Recognit. 2011;24:371–377. doi: 10.1002/jmr.1090. [DOI] [PubMed] [Google Scholar]
- [13].Lu J, Marnell LL, Marjon KD, Mold C, Du Clos TW, Sun PD. Structural recognition and functional activation of FcgammaR by innate pentraxins. Nature. 2008;456:989–992. doi: 10.1038/nature07468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Lu J, Marjon KD, Mold C, Du Clos TW, Sun PD. Pentraxins and Fc receptors. Immunol Rev. 2012;250:230–238. doi: 10.1111/j.1600-065X.2012.01162.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Bottazzi B, Doni A, Garlanda C, Mantovani A. An Integrated View of Humoral Innate Immunity: Pentraxins as a Paradigm. Annu Rev Immunol. 2010;28:157–183. doi: 10.1146/annurev-immunol-030409-101305. [DOI] [PubMed] [Google Scholar]
- [16].Poon IK, Hulett MD, Parish CR. Molecular mechanisms of late apoptotic/necrotic cell clearance. Cell Death Differ. 2010;17:381–397. doi: 10.1038/cdd.2009.195. [DOI] [PubMed] [Google Scholar]
- [17].Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;111:1805–1812. doi: 10.1172/JCI18921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Pepys MB. C-reactive protein and the acute phase response. Nature. 1982;296:12. doi: 10.1038/296012a0. [DOI] [PubMed] [Google Scholar]
- [19].Bijl M, Bootsma H, Van Der Geld Y, Limburg PC, Kallenberg CG, Van Rijswijk MH. Serum amyloid P component levels are not decreased in patients with systemic lupus erythematosus and do not rise during an acute phase reaction. Ann Rheum Dis. 2004;63:831–835. doi: 10.1136/ard.2002.004796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Altmeyer A, Klampfer L, Goodman AR, Vilcek J. Promoter structure and transcriptional activation of the murine TSG-14 gene encoding a tumor necrosis factor/interleukin-1-inducible pentraxin protein. J Biol Chem. 1995;270:25584–25590. doi: 10.1074/jbc.270.43.25584. [DOI] [PubMed] [Google Scholar]
- [21].Basile A, Sica A, d'Aniello E, Breviario F, Garrido G, Castellano M, et al. Characterization of the promoter for the human long pentraxin PTX3. Role of NF-kappaB in tumor necrosis factor-alpha and interleukin-1beta regulation. J Biol Chem. 1997;272:8172–8178. doi: 10.1074/jbc.272.13.8172. [DOI] [PubMed] [Google Scholar]
- [22].Moalli F, Jaillon S, Inforzato A, Sironi M, Bottazzi B, Mantovani A, et al. Pathogen recognition by the long pentraxin PTX3. J Biomed Biotechnol. 2011;2011:830421. doi: 10.1155/2011/830421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Presta M, Camozzi M, Salvatori G, Rusnati M. Role of the soluble pattern recognition receptor PTX3 in vascular biology. J Cell Mol Med. 2007;11:723–738. doi: 10.1111/j.1582-4934.2007.00061.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Norata GD, Marchesi P, Pirillo A, Uboldi P, Chiesa G, Maina V, et al. Long pentraxin 3, a key component of innate immunity, is modulated by high-density lipoproteins in endothelial cells. Arterioscler Thromb Vasc Biol. 2008;28:925–931. doi: 10.1161/ATVBAHA.107.160606. [DOI] [PubMed] [Google Scholar]
- [25].Sironi M, Conti A, Bernasconi S, Fra AM, Pasqualini F, Nebuloni M, et al. Generation and characterization of a mouse lymphatic endothelial cell line. Cell Tissue Res. 2006;325:91–100. doi: 10.1007/s00441-006-0171-y. [DOI] [PubMed] [Google Scholar]
- [26].Jaillon S, Peri G, Delneste Y, Fremaux I, Doni A, Moalli F, et al. The humoral pattern recognition receptor PTX3 is stored in neutrophil granules and localizes in extracellular traps. J Exp Med. 2007;204:793–804. doi: 10.1084/jem.20061301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Craig DG, Lee P, Pryde EA, Walker SW, Beckett GJ, Hayes PC, et al. Elevated levels of the long pentraxin 3 in paracetamol-induced human acute liver injury. Eur J Gastroenterol Hepatol. 2013;25:359–367. doi: 10.1097/MEG.0b013e32835ac77a. [DOI] [PubMed] [Google Scholar]
- [28].Doni A, Musso T, Morone D, Bastone A, Zambelli V, Sironi M, et al. An acidic microenvironment sets the humoral pattern recognition molecule PTX3 in a tissue repair mode. J Exp Med. 2015;212:905–925. doi: 10.1084/jem.20141268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Doni A, Michela M, Bottazzi B, Peri G, Valentino S, Polentarutti N, et al. Regulation of PTX3, a key component of humoral innate immunity in human dendritic cells: stimulation by IL-10 and inhibition by IFN-gamma. J Leukoc Biol. 2006;79:797–802. doi: 10.1189/jlb.0905493. [DOI] [PubMed] [Google Scholar]
- [30].Doni A, Mantovani G, Porta C, Tuckermann J, Reichardt HM, Kleiman A, et al. Cell-specific regulation of PTX3 by glucocorticoid hormones in hematopoietic and non-hematopoietic cells. J Biol Chem. 2008;283:29983–29992. doi: 10.1074/jbc.M805631200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Bottazzi B, Vouret-Craviari V, Bastone A, De Gioia L, Matteucci C, Peri G, et al. Multimer formation and ligand recognition by the long pentraxin PTX3. Similarities and differences with the short pentraxins C-reactive protein and serum amyloid P component. J Biol Chem. 1997;272:32817–32823. doi: 10.1074/jbc.272.52.32817. [DOI] [PubMed] [Google Scholar]
- [32].Inforzato A, Baldock C, Jowitt TA, Holmes DF, Lindstedt R, Marcellini M, et al. The angiogenic inhibitor long pentraxin PTX3 forms an asymmetric octamer with two binding sites for FGF2. J Biol Chem. 2010;285:17681–17692. doi: 10.1074/jbc.M109.085639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Introna M, Alles VV, Castellano M, Picardi G, De Gioia L, Bottazzai B, et al. Cloning of mouse ptx3, a new member of the pentraxin gene family expressed at extrahepatic sites. Blood. 1996;87:1862–1872. [PubMed] [Google Scholar]
- [34].Inforzato A, Peri G, Doni A, Garlanda C, Mantovani A, Bastone A, et al. Structure and function of the long pentraxin PTX3 glycosidic moiety: fine-tuning of the interaction with C1q and complement activation. Biochemistry (Mosc) 2006;45:11540–11551. doi: 10.1021/bi0607453. [DOI] [PubMed] [Google Scholar]
- [35].Deban L, Jarva H, Lehtinen MJ, Bottazzi B, Bastone A, Doni A, et al. Binding of the long pentraxin PTX3 to Factor H: Interacting domains and function in the regulation of complement activation. J Immunology. 2008;181:8433–8440. doi: 10.4049/jimmunol.181.12.8433. [DOI] [PubMed] [Google Scholar]
- [36].Gout E, Moriscot C, Doni A, Dumestre-Perard C, Lacroix M, Perard J, et al. M-ficolin interacts with the long pentraxin PTX3: a novel case of cross-talk between soluble pattern-recognition molecules. J Immunol. 2011;186:5815–5822. doi: 10.4049/jimmunol.1100180. [DOI] [PubMed] [Google Scholar]
- [37].Reading PC, Bozza S, Gilbertson B, Tate M, Moretti S, Job ER, et al. Antiviral Activity of the Long Chain Pentraxin PTX3 against Influenza Viruses. J Immunol. 2008;180:3391–3398. doi: 10.4049/jimmunol.180.5.3391. [DOI] [PubMed] [Google Scholar]
- [38].Deban L, Castro Russo R, Sironi M, Moalli F, Scanziani M, Zambelli V, et al. Regulation of leukocyte recruitment by the long pentraxin PTX3. Nat Immunol. 2010;11:328–334. doi: 10.1038/ni.1854. [DOI] [PubMed] [Google Scholar]
- [39].Ievoli E, Lindstedt R, Inforzato A, Camaioni A, Palone F, Day AJ, et al. Implication of the oligomeric state of the N-terminal PTX3 domain in cumulus matrix assembly. Matrix Biol. 2011;30:330–337. doi: 10.1016/j.matbio.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Stibenz D, Grafe M, Debus N, Hasbach M, Bahr I, Graf K, et al. Binding of human serum amyloid P componentto L-selectin. Eur J Immunol. 2006;36:446–456. doi: 10.1002/eji.200425360. [DOI] [PubMed] [Google Scholar]
- [41].Lech M, Rommele C, Grobmayr R, Eka Susanti H, Kulkarni OP, Wang S, et al. Endogenous and exogenous pentraxin-3 limits postischemic acute and chronic kidney injury. Kidney Int. 2013;83:647–661. doi: 10.1038/ki.2012.463. [DOI] [PubMed] [Google Scholar]
- [42].Inforzato A, Bottazzi B, Garlanda C, Valentino S, Mantovani A. Pentraxins in humoral innate immunity. Adv Exp Med Biol. 946:1–20. doi: 10.1007/978-1-4614-0106-3_1. [DOI] [PubMed] [Google Scholar]
- [43].Nauta AJ, Daha MR, van Kooten C, Roos A. Recognition and clearance of apoptotic cells: a role for complement and pentraxins. Trends Immunol. 2003;24:148–154. doi: 10.1016/s1471-4906(03)00030-9. [DOI] [PubMed] [Google Scholar]
- [44].Ng PM, Le Saux A, Lee CM, Tan NS, Lu J, Thiel S, et al. C-reactive protein collaborates with plasma lectins to boost immune response against bacteria. EMBO J. 2007;26:3431–3440. doi: 10.1038/sj.emboj.7601762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Gershov D, Kim S, Brot N, Elkon KB. C-Reactive protein binds to apoptotic cells, protects the cells from assembly of the terminal complement components, and sustains an antiinflammatory innate immune response: implications for systemic autoimmunity. J Exp Med. 2000;192:1353–1364. doi: 10.1084/jem.192.9.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Gill R, Kemp JA, Sabin C, Pepys MB. Human C-reactive protein increases cerebral infarct size after middle cerebral artery occlusion in adult rats. J Cereb Blood Flow Metab. 2004;24:1214–1218. doi: 10.1097/01.WCB.0000136517.61642.99. [DOI] [PubMed] [Google Scholar]
- [47].Pepys MB, Gallimore JR, Lloyd J, Li Z, Graham D, Taylor GW, et al. Isolation and characterization of pharmaceutical grade human pentraxins, serum amyloid P component and C-reactive protein, for clinical use. J Immunol Methods. 2012;384:92–102. doi: 10.1016/j.jim.2012.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Jarva H, Jokiranta TS, Hellwage J, Zipfel PF, Meri S. Regulation of complement activation by C-reactive protein: targeting the complement inhibitory activity of factor H by an interaction with short consensus repeat domains 7 and 8-11. J Immunol. 1999;163:3957–3962. [PubMed] [Google Scholar]
- [49].Okemefuna AI, Nan R, Miller A, Gor J, Perkins SJ. Complement factor H binds at two independent sites to C-reactive protein in acute phase concentrations. J Biol Chem. 2010;285:1053–1065. doi: 10.1074/jbc.M109.044529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Sjoberg AP, Trouw LA, McGrath FD, Hack CE, Blom AM. Regulation of complement activation by C-reactive protein: targeting of the inhibitory activity of C4b-binding protein. J Immunol. 2006;176:7612–7620. doi: 10.4049/jimmunol.176.12.7612. [DOI] [PubMed] [Google Scholar]
- [51].Garcia de Frutos P, Hardig Y, Dahlback B. Serum amyloid P component binding to C4b-binding protein. J Biol Chem. 1995;270:26950–26955. doi: 10.1074/jbc.270.45.26950. [DOI] [PubMed] [Google Scholar]
- [52].Kopp A, Hebecker M, Svobodova E, Jozsi M. Factor h: a complement regulator in health and disease, and a mediator of cellular interactions. Biomolecules. 2:46–75. doi: 10.3390/biom2010046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Nauta AJ, Bottazzi B, Mantovani A, Salvatori G, Kishore U, Schwaeble WJ, et al. Biochemical and functional characterization of the interaction between pentraxin 3 and C1q. Eur J Immunol. 2003;33:465–473. doi: 10.1002/immu.200310022. [DOI] [PubMed] [Google Scholar]
- [54].Bally I, Ancelet S, Moriscot C, Gonnet F, Mantovani A, Daniel R, et al. Expression of recombinant human complement C1q allows identification of the C1r/C1s-binding sites. Proc Natl Acad Sci U S A. 110:8650–8655. doi: 10.1073/pnas.1304894110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Ma YJ, Doni A, Hummelshoj T, Honore C, Bastone A, Mantovani A, et al. Synergy between ficolin-2 and PTX3 boost innate immune recognition and complement deposition. J Biol Chem. 2009 doi: 10.1074/jbc.M109.009225. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Ma YJ, Doni A, Skjoedt MO, Honore C, Arendrup M, Mantovani A, et al. Heterocomplexes of mannose-binding lectin and the pentraxins PTX3 or serum amyloid P component trigger cross-activation of the complement system. J Biol Chem. 2011;286:3405–3417. doi: 10.1074/jbc.M110.190637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Moalli F, Doni A, Deban L, Zelante T, Zagarella S, Bottazzi B, et al. Role of complement and Fc{gamma} receptors in the protective activity of the long pentraxin PTX3 against Aspergillus fumigatus. Blood. 2010;116:5170–5180. doi: 10.1182/blood-2009-12-258376. [DOI] [PubMed] [Google Scholar]
- [58].Braunschweig A, Jozsi M. Human pentraxin 3 binds to the complement regulator c4b-binding protein. PloS one. 2011;6:e23991. doi: 10.1371/journal.pone.0023991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Kopp A, Strobel S, Tortajada A, Rodriguez de Cordoba S, Sanchez-Corral P, Prohaszka Z, et al. Atypical hemolytic uremic syndrome-associated variants and autoantibodies impair binding of factor h and factor h-related protein 1 to pentraxin 3. J Immunol. 189:1858–1867. doi: 10.4049/jimmunol.1200357. [DOI] [PubMed] [Google Scholar]
- [60].Bonavita E, Gentile S, Rubino M, Maina V, Papait R, Kunderfranco P, et al. PTX3 is an extrinsic oncosuppressor regulating complement-dependent inflammation in cancer. Cell. 2015;160:700–714. doi: 10.1016/j.cell.2015.01.004. [DOI] [PubMed] [Google Scholar]
- [61].Lu J, Marjon KD, Marnell LL, Wang R, Mold C, Du Clos TW, et al. Recognition and functional activation of the human IgA receptor (FcalphaRI) by C-reactive protein. Proc Natl Acad Sci U S A. 2011;108:4974–4979. doi: 10.1073/pnas.1018369108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Inforzato A, Doni A, Barajon I, Leone R, Garlanda C, Bottazzi B, et al. PTX3 as a paradigm for the interaction of pentraxins with the complement system. Semin Immunol. 25:79–85. doi: 10.1016/j.smim.2013.05.002. [DOI] [PubMed] [Google Scholar]
- [63].Agrawal A, Singh PP, Bottazzi B, Garlanda C, Mantovani A. Pattern recognition by pentraxins. Adv Exp Med Biol. 2009;653:98–116. doi: 10.1007/978-1-4419-0901-5_7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Yuste J, Botto M, Bottoms SE, Brown JS. Serum amyloid P aids complement-mediated immunity to Streptococcus pneumoniae. PLoS Pathog. 2007;3:1208–1219. doi: 10.1371/journal.ppat.0030120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Noursadeghi M, Bickerstaff MC, Gallimore JR, Herbert J, Cohen J, Pepys MB. Role of serum amyloid P component in bacterial infection: protection of the host or protection of the pathogen. Proc Natl Acad Sci U S A. 2000;97:14584–14589. doi: 10.1073/pnas.97.26.14584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Armstrong GD, Mulvey GL, Marcato P, Griener TP, Kahan MC, Tennent GA, et al. Human serum amyloid P component protects against Escherichia coli O157:H7 Shiga toxin 2 in vivo: therapeutic implications for hemolytic-uremic syndrome. J Infect Dis. 2006;193:1120–1124. doi: 10.1086/501472. [DOI] [PubMed] [Google Scholar]
- [67].Wiest R, Lawson M, Geuking M. Pathological bacterial translocation in liver cirrhosis. J Hepatol. 2014;60:197–209. doi: 10.1016/j.jhep.2013.07.044. [DOI] [PubMed] [Google Scholar]
- [68].Saitoh O, Sugi K, Lojima K, Matsumoto H, Nakagawa K, Kayazawa M, et al. Increased prevalence of intestinal inflammation in patients with liver cirrhosis. World J Gastroenterol. 1999;5:391–396. doi: 10.3748/wjg.v5.i5.391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Garlanda C, Hirsch E, Bozza S, Salustri A, De Acetis M, Nota R, et al. Non-redundant role of the long pentraxin PTX3 in anti-fungal innate immune response. Nature. 2002;420:182–186. doi: 10.1038/nature01195. [DOI] [PubMed] [Google Scholar]
- [70].Job ER, Deng YM, Tate MD, Bottazzi B, Crouch EC, Dean MM, et al. Pandemic H1N1 influenza A viruses are resistant to the antiviral activities of innate immune proteins of the collectin and pentraxin superfamilies. J Immunol. 2010;185:4284–4291. doi: 10.4049/jimmunol.1001613. [DOI] [PubMed] [Google Scholar]
- [71].Jaillon S, Mancuso G, Hamon Y, Beauvillain C, Cotici V, Midiri A, et al. Prototypic long pentraxin PTX3 is present in breast milk, spreads in tissues, and protects neonate mice from Pseudomonas aeruginosa lung infection. J Immunol. 2013;191:1873–1882. doi: 10.4049/jimmunol.1201642. [DOI] [PubMed] [Google Scholar]
- [72].Jaillon S, Moalli F, Ragnarsdottir B, Bonavita E, Puthia M, Riva F, et al. The Humoral Pattern Recognition Molecule PTX3 Is a Key Component of Innate Immunity against Urinary Tract Infection. Immunity. 2014;40:621–632. doi: 10.1016/j.immuni.2014.02.015. [DOI] [PubMed] [Google Scholar]
- [73].Bottazzi B, Santini L, Savino S, Giuliani MM, Duenas Diez AI, Mancuso G, et al. Recognition of Neisseria meningitidis by the long pentraxin PTX3 and its role as an endogenous adjuvant. PLoS One. 2015;10:e0120807. doi: 10.1371/journal.pone.0120807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Job ER, Bottazzi B, Short KR, Deng YM, Mantovani A, Brooks AG, et al. A single amino acid substitution in the hemagglutinin of H3N2 subtype influenza A viruses is associated with resistance to the long pentraxin PTX3 and enhanced virulence in mice. J Immunol. 2014;192:271–281. doi: 10.4049/jimmunol.1301814. [DOI] [PubMed] [Google Scholar]
- [75].Foo SS, Chen W, Taylor A, Sheng KC, Yu X, Teng TS, et al. Role of pentraxin 3 in shaping arthritogenic alphaviral disease: from enhanced viral replication to immunomodulation. PLoS Pathog. 2015;11:e1004649. doi: 10.1371/journal.ppat.1004649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Olesen R, Wejse C, Velez DR, Bisseye C, Sodemann M, Aaby P, et al. DC-SIGN (CD209), pentraxin 3 and vitamin D receptor gene variants associate with pulmonary tuberculosis risk in West Africans. Genes Immun. 2007;8:456–467. doi: 10.1038/sj.gene.6364410. [DOI] [PubMed] [Google Scholar]
- [77].Chiarini M, Sabelli C, Melotti P, Garlanda C, Savoldi G, Mazza C, et al. PTX3 genetic variations affect the risk of Pseudomonas aeruginosa airway colonization in cystic fibrosis patients. Genes and immunity. 2010;11:665–670. doi: 10.1038/gene.2010.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Cunha C, Aversa F, Lacerda JF, Busca A, Kurzai O, Grube M, et al. Genetic PTX3 deficiency and aspergillosis in stem-cell transplantation. The New England journal of medicine. 2014;370:421–432. doi: 10.1056/NEJMoa1211161. [DOI] [PubMed] [Google Scholar]
- [79].Wojtowicz A, Lecompte TD, Bibert S, Manuel O, Rueger S, Berger C, et al. PTX3 Polymorphisms and Invasive Mold Infections After Solid Organ Transplant. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2015;61:619–622. doi: 10.1093/cid/civ386. [DOI] [PubMed] [Google Scholar]
- [80].Barbati E, Specchia C, Villella M, Rossi ML, Barlera S, Bottazzi B, et al. Influence of Pentraxin 3 (PTX3) Genetic Variants on Myocardial Infarction Risk and PTX3 Plasma Levels. PLoS One. 2012;7:e53030. doi: 10.1371/journal.pone.0053030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Bodin K, Ellmerich S, Kahan MC, Tennent GA, Loesch A, Gilbertson JA, et al. Antibodies to human serum amyloid P component eliminate visceral amyloid deposits. Nature. 2010;468:93–97. doi: 10.1038/nature09494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Richards DB, Cookson LM, Berges AC, Barton SV, Lane T, Ritter JM, et al. Therapeutic Clearance of Amyloid by Antibodies to Serum Amyloid P Component. N Engl J Med. 2015;373:1106–1114. doi: 10.1056/NEJMoa1504942. [DOI] [PubMed] [Google Scholar]
- [83].Salustri A, Garlanda C, Hirsch E, De Acetis M, Maccagno A, Bottazzi B, et al. PTX3 plays a key role in the organization of the cumulus oophorus extracellular matrix and in in vivo fertilization. Development. 2004;131:1577–1586. doi: 10.1242/dev.01056. [DOI] [PubMed] [Google Scholar]
- [84].Fulop C, Szanto S, Mukhopadhyay D, Bardos T, Kamath RV, Rugg MS, et al. Impaired cumulus mucification and female sterility in tumor necrosis factor-induced protein-6 deficient mice. Development. 2003;130:2253–2261. doi: 10.1242/dev.00422. [DOI] [PubMed] [Google Scholar]
- [85].Scarchilli L, Camaioni A, Bottazzi B, Negri V, Doni A, Deban L, et al. PTX3 Interacts with Inter-{alpha}-trypsin Inhibitor: implications for hyaluronan organization and cumulus oophorus expansion. J Biol Chem. 2007;282:30161–30170. doi: 10.1074/jbc.M703738200. [DOI] [PubMed] [Google Scholar]
- [86].Pilling D, Gomer RH. Persistent lung inflammation and fibrosis in serum amyloid P component (APCs-/-) knockout mice. PloS one. 2014;9:e93730. doi: 10.1371/journal.pone.0093730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].Cox N, Pilling D, Gomer RH. Serum amyloid P: a systemic regulator of the innate immune response. J Leukoc Biol. 2014;96:739–743. doi: 10.1189/jlb.1MR0114-068R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [88].Dillingh MR, van den Blink B, Moerland M, van Dongen MG, Levi M, Kleinjan A, et al. Recombinant human serum amyloid P in healthy volunteers and patients with pulmonary fibrosis. Pulmonary pharmacology & therapeutics. 2013;26:672–676. doi: 10.1016/j.pupt.2013.01.008. [DOI] [PubMed] [Google Scholar]
- [89].Cox N, Pilling D, Gomer RH. DC-SIGN activation mediates the differential effects of SAP and CRP on the innate immune system and inhibits fibrosis in mice. Proc Natl Acad Sci U S A. 2015;112:8385–8390. doi: 10.1073/pnas.1500956112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Stal P. Liver fibrosis in non-alcoholic fatty liver disease - diagnostic challenge with prognostic significance. World J Gastroenterol. 2015;21:11077–11087. doi: 10.3748/wjg.v21.i39.11077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Boga S, Koksal AR, Alkim H, Yilmaz Ozguven MB, Bayram M, Ergun M, et al. Plasma Pentraxin 3 Differentiates Nonalcoholic Steatohepatitis (NASH) from Non-NASH. Metabolic syndrome and related disorders. 2015;13:393–399. doi: 10.1089/met.2015.0046. [DOI] [PubMed] [Google Scholar]
- [92].Yoneda M, Mawatari H, Fujita K, Iida H, Yonemitsu K, Kato S, et al. High-sensitivity C-reactive protein is an independent clinical feature of nonalcoholic steatohepatitis (NASH) and also of the severity of fibrosis in NASH. J Gastroenterol. 2007;42:573–582. doi: 10.1007/s00535-007-2060-x. [DOI] [PubMed] [Google Scholar]
- [93].Yoneda M, Uchiyama T, Kato S, Endo H, Fujita K, Yoneda K, et al. Plasma Pentraxin3 is a novel marker for nonalcoholic steatohepatitis (NASH) BMC Gastroenterol. 2008;8:53. doi: 10.1186/1471-230X-8-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Maleki I, Rastgar A, Hosseini V, Taghvaei T, Rafiei A, Barzin M, et al. High sensitive CRP and pentraxine 3 as noninvasive biomarkers of nonalcoholic fatty liver disease. Eur Rev Med Pharmacol Sci. 2014;18:1583–1590. [PubMed] [Google Scholar]
- [95].Pilling D, Cox N, Vakil V, Verbeek JS, Gomer RH. The long pentraxin PTX3 promotes fibrocyte differentiation. PLoS One. 2015;10:e0119709. doi: 10.1371/journal.pone.0119709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Calvaruso V, Maimone S, Gatt A, Tuddenham E, Thursz M, Pinzani M, et al. Coagulation and fibrosis in chronic liver disease. Gut. 2008;57:1722–1727. doi: 10.1136/gut.2008.150748. [DOI] [PubMed] [Google Scholar]
- [97].Pohl JF, Melin-Aldana H, Sabla G, Degen JL, Bezerra JA. Plasminogen deficiency leads to impaired lobular reorganization and matrix accumulation after chronic liver injury. The American journal of pathology. 2001;159:2179–2186. doi: 10.1016/S0002-9440(10)63069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Bugge TH, Kombrinck KW, Flick MJ, Daugherty CC, Danton MJ, Degen JL. Loss of fibrinogen rescues mice from the pleiotropic effects of plasminogen deficiency. Cell. 1996;87:709–719. doi: 10.1016/s0092-8674(00)81390-2. [DOI] [PubMed] [Google Scholar]
- [99].Engelmann B, Massberg S. Thrombosis as an intravascular effector of innate immunity. Nat Rev Immunol. 2013;13:34–45. doi: 10.1038/nri3345. [DOI] [PubMed] [Google Scholar]
- [100].Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454:436–444. doi: 10.1038/nature07205. [DOI] [PubMed] [Google Scholar]
- [101].Guo L, Liu S, Zhang S, Chen Q, Zhang M, Quan P, et al. C-reactive protein and risk of breast cancer: A systematic review and meta-analysis. Scientific Reports. 2015;5:10508. doi: 10.1038/srep10508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [102].Heikkilä K, Harris R, Lowe G, Rumley A, Yarnell J, Gallacher J, et al. Associations of circulating C-reactive protein and interleukin-6 with cancer risk: findings from two prospective cohorts and a meta-analysis. Cancer Causes Control. 2009;20:15–26. doi: 10.1007/s10552-008-9212-z. [DOI] [PubMed] [Google Scholar]
- [103].Kondo S, Ueno H, Hosoi H, Hashimoto J, Morizane C, Koizumi F, et al. Clinical impact of pentraxin family expression on prognosis of pancreatic carcinoma. Br J Cancer. 2013;109:739–746. doi: 10.1038/bjc.2013.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Morizane C, Okusaka T, Morita S, Tanaka K, Ueno H, Kondo S, et al. Construction and Validation of a Prognostic Index for Patients With Metastatic Pancreatic Adenocarcinoma. Pancreas. 2011;40:415–421. doi: 10.1097/MPA.0b013e3182021376. [DOI] [PubMed] [Google Scholar]
- [105].Poole EM, Lee I-M, Ridker PM, Buring JE, Hankinson SE, Tworoger SS. A Prospective Study of Circulating C-Reactive Protein, Interleukin-6, and Tumor Necrosis Factor α Receptor 2 Levels and Risk of Ovarian Cancer. Am J Epidemiol. 2013;178:1256–1264. doi: 10.1093/aje/kwt098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [106].Mitsunaga S, Ikeda M, Shimizu S, Ohno I, Takahashi H, Okuyama H, et al. C-Reactive Protein Level Is an Indicator of the Aggressiveness of Advanced Pancreatic Cancer. Pancreas. 2015 doi: 10.1097/MPA.0000000000000465. [DOI] [PubMed] [Google Scholar]
- [107].Mitsunaga S, Ikeda M, Shimizu S, Ohno I, Takahashi H, Okuyama H, et al. C-Reactive Protein Level Is an Indicator of the Aggressiveness of Advanced Pancreatic Cancer. Pancreas. doi: 10.1097/MPA.0000000000000465. 9000; Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- [108].Choi B, Lee EJ, Song DH, Yoon SC, Chung YH, Jang Y, et al. Elevated Pentraxin 3 in bone metastatic breast cancer is correlated with osteolytic function. Oncotarget. 2014;5:481–492. doi: 10.18632/oncotarget.1664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [109].Diamandis EP, Goodglick L, Planque C, Thornquist MD. Pentraxin-3 is a novel biomarker of lung carcinoma. Clin Cancer Res. 2011;17:2395–2399. doi: 10.1158/1078-0432.CCR-10-3024. [DOI] [PubMed] [Google Scholar]
- [110].Germano G, Frapolli R, Simone M, Tavecchio M, Erba E, Pesce S, et al. Antitumor and anti-inflammatory effects of trabectedin on human myxoid liposarcoma cells. Cancer Res. 2010;70:2235–2244. doi: 10.1158/0008-5472.CAN-09-2335. [DOI] [PubMed] [Google Scholar]
- [111].Infante M, Allavena P, Garlanda C, Nebuloni M, Morenghi E, Rahal D, et al. Prognostic and diagnostic potential of local and circulating levels of pentraxin 3 in lung cancer patients. Int J Cancer. 2015 doi: 10.1002/ijc.29822. [DOI] [PubMed] [Google Scholar]
- [112].Stallone G, Cormio L, Netti GS, Infante B, Selvaggio O, Fino GD, et al. Pentraxin 3: a novel biomarker for predicting progression from prostatic inflammation to prostate cancer. Cancer Res. 2014;74:4230–4238. doi: 10.1158/0008-5472.CAN-14-0369. [DOI] [PubMed] [Google Scholar]
- [113].Tothill RW, Tinker AV, George J, Brown R, Fox SB, Lade S, et al. Novel molecular subtypes of serous and endometrioid ovarian cancer linked to clinical outcome. Clin Cancer Res. 2008;14:5198–5208. doi: 10.1158/1078-0432.CCR-08-0196. [DOI] [PubMed] [Google Scholar]
- [114].Carmo RF, Aroucha D, Vasconcelos LR, Pereira LM, Moura P, Cavalcanti MS. Genetic variation in PTX3 and plasma levels associated with hepatocellular carcinoma in patients with HCV. J Viral Hepat. 2015 doi: 10.1111/jvh.12472. [DOI] [PubMed] [Google Scholar]
- [115].Wang JX, He YL, Zhu ST, Yang S, Zhang ST. Aberrant methylation of the 3q25 tumor suppressor gene PTX3 in human esophageal squamous cell carcinoma. World J Gastroenterol. 2011;17:4225–4230. doi: 10.3748/wjg.v17.i37.4225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Ronca R, Giacomini A, Di Salle E, Coltrini D, Pagano K, Ragona L, et al. Long-Pentraxin 3 Derivative as a Small-Molecule FGF Trap for Cancer Therapy. Cancer cell. 2015;28:225–239. doi: 10.1016/j.ccell.2015.07.002. [DOI] [PubMed] [Google Scholar]
- [117].Ronca R, Di Salle E, Giacomini A, Leali D, Alessi P, Coltrini D, et al. Long pentraxin-3 inhibits epithelial-mesenchymal transition in melanoma cells. Molecular cancer therapeutics. 2013;12:2760–2771. doi: 10.1158/1535-7163.MCT-13-0487. [DOI] [PubMed] [Google Scholar]
- [118].Rusnati M, Camozzi M, Moroni E, Bottazzi B, Peri G, Indraccolo S, et al. Selective recognition of fibroblast growth factor-2 by the long pentraxin PTX3 inhibits angiogenesis. Blood. 2004;104:92–99. doi: 10.1182/blood-2003-10-3433. [DOI] [PubMed] [Google Scholar]
- [119].Chang WC, Wu SL, Huang WC, Hsu JY, Chan SH, Wang JM, et al. PTX3 gene activation in EGF-induced head and neck cancer cell metastasis. Oncotarget. 2015;6:7741–7757. doi: 10.18632/oncotarget.3482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [120].Choi B, Lee EJ, Park YS, Kim SM, Kim EY, Song Y, et al. Pentraxin-3 Silencing Suppresses Gastric Cancer-related Inflammation by Inhibiting Chemotactic Migration of Macrophages. Anticancer Res. 2015;35:2663–2668. [PubMed] [Google Scholar]
- [121].Bartolini A, Di Paolo D, Noghero A, Murgia D, Sementa AR, Cilli M, et al. The Neuronal Pentraxin-2 Pathway Is an Unrecognized Target in Human Neuroblastoma, Which Also Offers Prognostic Value in Patients. Cancer Res. 2015 doi: 10.1158/0008-5472.CAN-15-0649. [DOI] [PubMed] [Google Scholar]
- [122].Zhou C, Qin Y, Xie Z, Zhang J, Yang M, Li S, et al. NPTX1 is a novel epigenetic regulation gene and associated with prognosis in lung cancer. Biochem Biophys Res Commun. 2015;458:381–386. doi: 10.1016/j.bbrc.2015.01.124. [DOI] [PubMed] [Google Scholar]