Abstract
Background
The purpose of mammography screening is to decrease breast cancer mortality. To achieve this a high coverage by examination is needed. Within an organized screening programme, we examined the impact of changes in the invitation schedule on the interplay between coverage and participation.
Method
We studied nine cohorts aged 50–51 when first targeted by mammography screening in Copenhagen, Denmark. Population data were retrieved from the Danish Civil Registration System; invitation and attendance data from the screening programme database. Data were linked using unique personal identification numbers. Coverage by invitation was defined as (number of invited women/number of targeted women), coverage by examination as (number of screened women/number of targeted women), and participation rate as (number of screened women/number of invited women).
Results
Coverage by invitation was close to or above 95% for all newly recruited cohorts. In subsequent invitation rounds, both technical errors and changes in the invitation scheme affected the coverage by invitation. Coverage by examination at first invitation was 72.5% for the first cohort, but dropped to 64.2% for the latest cohort. Furthermore, coverage by examination dropped by increasing invitation number and with omission of re-invitation of previous non-attenders. Participation rate closely reflected changes in the invitation scheme.
Conclusion
Changes in the invitation schemes influenced coverage by invitation, coverage by examination, and participation rate. We observed a considerable gap between coverage by examination and participation rate, strongly indicating that the latter cannot without reservations, be taken as an indicator of the first.
Keywords: Attendance, breast cancer, mammography, mass screening, protective effect
Introduction
For mammography screening to reduce breast cancer mortality, a large proportion of the targeted women must be screened. Monitoring recruitment and participation is an essential part of the quality assurance of screening. The European Union recommends organized screening programmes. Quality indicators for mammography screening are specified in the European Guidelines for Quality Assurance in Breast Cancer Screening and Diagnosis,1 and these include monitoring the coverage of the targeted population by invitation to screening, the coverage of the targeted population by screening examination, and the participation rate in screening among invited women.
A survey of European mammography screening programmes showed that coverage by examination varied from about 30% to about 90%,2 indicating large differences in the potential impact of screening on breast cancer mortality. Low coverage by examination in an organized programme may reflect that some targeted women attend opportunistic screening or it may reflect low acceptability of screening. The organizational aspects of the programme very probably also play a role.
We evaluated the effect of variations in the invitation scheme on coverage and participation through more than 20 years of the organized, population-based mammography screening programme in Copenhagen, Denmark.
Methods
Setting
Organized, population-based mammography screening in the Copenhagen municipality started on 4th April 1991. Full descriptions of the programme have been published.3,4 The target population was women aged 50–69 residing in the municipality of Copenhagen, identified via the daily updated Danish Civil Registration System (CRS). Over time, various small subgroups were considered ineligible for screening (see below). Eligible women were personally invited to screening.
Invitation rounds were of approximately two years (Appendix Table 2). Invited women received a personal letter with a fixed, changeable date of appointment. Women born in January were invited during the first two months of the first year of an invitation round, women born in February were invited during the next two months, etc. Non-responders received a reminder. Initially, women already diagnosed with breast cancer and known in the register of the Danish Collaborative Breast Cancer Group were considered ineligible and excluded from invitation, but this stopped as it became clear that the register was not sufficiently updated for this purpose. Over time, exclusions encompassed some women with breast cancer, some with bilateral mastectomy, and some with breast prostheses prohibiting the mammography examination. Later, women with breast cancer surgery more than 18 months ago were again invited for screening. From the beginning, a woman could notify the clinic if she did not want to be invited again, in which case she did not receive any further invitation (Appendix Table 3).
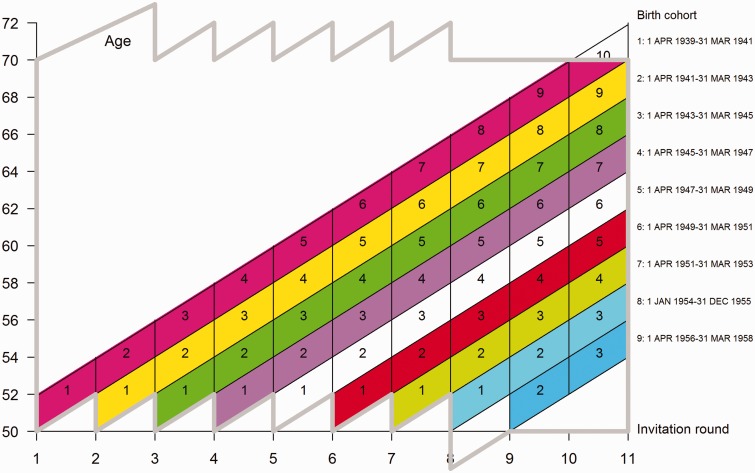
In invitation rounds 1–7, women aged 50–69 at the start of each round were invited (Figure 1). In invitation round 2, women aged 50–71 at the start were invited. All women were invited to the next round, except those who had notified the programme not to be re-invited, moved out of the area, or passed the upper age limit for re-invitation. In invitation rounds 6 and 7, approximately 10% of the target population were not invited due to unidentified technical errors in the invitation system.5
Figure 1.
Cohorts of women first targeted by the Copenhagen programme at age 50–51 by age, invitation rounds, and invitation numbers (marked in graph).
From invitation round 8 onwards, invitations were planned to be issued according to attained age, meaning that women aged 50–69 at the invitation date were invited to screening. Women received the first invitation at age 50–51 and the last at age 68–69, depending on age at first invitation. Exceptionally for round 8, invitations included all women from the age of 48 at the start of round 8. For invitation round 8, part of non-participants from round 7, including those not invited due to technical errors, were not invited. Women previously administratively excluded due to technical errors were re-invited in invitation round 9. However, in invitation rounds 9 and 10, women who had not responded to the previous two invitation rounds (previous passive non-participants) were not invited.
Data
CRS holds information on current and historical addresses for residents in Denmark since 1968. From the CRS, we identified the target population of the Copenhagen municipality screening programme from 1 April 1991 to 12 July 2012, covering 10 biennial invitation rounds. From invitation rounds 1–8, the Copenhagen screening programme kept a mammography register with the personal identification number (including information on and date of birth), date of invitation, dates of reminders, date of screening, outcome of screening, and (where relevant) dates and outcome of assessment and surgery. The register also included information on women who had notified the programme that they did not want to be invited, and the register included codes for ineligibility. From invitation round 9 onwards, the Copenhagen programme became incorporated into the larger programme for the Capital Region of Denmark. The structure of the mammography screening register for the Capital Region differs from the old register from Copenhagen. However, it is possible from this new register to obtain the same information as before, apart from ineligibility, for which only the latest registration was kept in the new register. We linked the data retrieved from the CRS and the screening registers, which provided us with a complete invitation history of all targeted women. The use of opportunistic screening has always been very limited in Denmark.6
Analysis
To control for age and number of offered screens when we compared coverage with participation, we constructed nine closed cohorts, each including women aged 50–51 at the start of their first invitation round (cohort 1–9). These cohorts were followed up from the first through subsequent invitation rounds (1–10, 1–9,… 1–2), each time including those present from the cohort at the start of a given round. We used the term ‘invitation number’ for the first, second, etc. number of times a given cohort had been offered screening. For study design and birth dates for cohorts, see Figure 1.
Each cohort was tabulated by number of women targeted, number of women invited, and number of women participating by invitation round and invitation number. We were not able to tabulate the number of eligible women for invitation rounds 9–10, as only the latest ineligibility code was kept in the system. We also calculated coverage by invitation (number of invited women divided by number of women in the target population), coverage by examination (number of participating women divided by number of women in the target population), and participation rate (number of participating women divided by number of invited women) by invitation round and invitation number.
The change in invitation scheme in round 8 to include all women from age 48 onwards meant that our cohort 9 started with the second invitation number.
Results
Our study included 47,990 screen targeted women, of whom 45,597 were invited; of these, 31,424 participated in screening (Appendix Table 4).
Coverage by invitation for the newly recruited cohorts of women aged 50–51 was close to 95% in all invitation rounds except round 2, where it reached 99.5%, and round 7 where it dropped to 93.7% (Table 1). For cohort 1, coverage by invitation dropped gradually over successive invitation numbers, from 95.6% at first invitation to 87.4% at fifth invitation. A dramatic drop to 70.0% at invitation 6 was observed, remaining low at invitations 7 and 8 and then increasing again to 76.6% at invitation 9. Similar changes were seen for cohort 2 at invitations 5 and 8, respectively, and for cohort 3 at invitations 4 and 7, respectively, and so forth for successive cohorts. These dramatic drops in coverage by invitation reflected the errors in the invitation scheme in invitation rounds 6–8, and the equally dramatic increases reflected the deletion of previous administrative exclusions in invitation round 9. The low number for cohort 1 invitation 10 (17.1%) reflected that women were no longer invited when they turned 70.
Table 1.
Coverage by invitation (%), coverage by participation (%), and participation rates (%) by invitation rounds and invitation numbers for women first targeted by the Copenhagen screening programme at age 50–51.
| Invitation round, first targeted = cohort number | Invitation number |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| Coverage by invitation (%) | ||||||||||
| 1 | 95.6 | 93.7 | 90.4 | 88.3 | 87.4 | 70.0 | 68.0 | 67.8 | 76.6 | 17.1 |
| 2 | 99.5 | 91.8 | 89.4 | 88.5 | 68.9 | 67.7 | 68.0 | 80.0 | 78.1 | |
| 3 | 95.9 | 93.5 | 92.3 | 72.2 | 70.0 | 69.1 | 82.0 | 79.0 | ||
| 4 | 95.6 | 93.4 | 78.1 | 76.3 | 74.6 | 78.9 | 76.6 | |||
| 5 | 94.9 | 92.8 | 89.7 | 84.8 | 70.8 | 68.4 | ||||
| 6 | 96.0 | 91.7 | 90.9 | 72.3 | 70.7 | |||||
| 7 | 93.7 | 91.7 | 75.3 | 72.6 | ||||||
| 8 | 95.4 | 91.0 | 88.5 | |||||||
| 9 | NR | 89.2 | 87.1 | |||||||
| Coverage by examination (%) | ||||||||||
| 1 | 72.5 | 66.0 | 65.6 | 63.9 | 61.7 | 59.3 | 56.6 | 56.5 | 52.4 | 11.1 |
| 2 | 70.4 | 64.1 | 62.9 | 60.0 | 57.4 | 57.1 | 57.5 | 57.3 | 54.5 | |
| 3 | 66.5 | 63.5 | 60.7 | 58.8 | 57.6 | 57.8 | 59.0 | 57.4 | ||
| 4 | 67.1 | 62.3 | 60.7 | 59.8 | 60.8 | 60.9 | 58.0 | |||
| 5 | 63.9 | 61.4 | 62.5 | 63.2 | 59.6 | 56.6 | ||||
| 6 | 62.7 | 63.0 | 63.8 | 60.8 | 58.5 | |||||
| 7 | 63.0 | 62.1 | 59.9 | 57.9 | ||||||
| 8 | 64.2 | 63.1 | 59.1 | |||||||
| 9 | NR | 60.6 | 58.9 | |||||||
| Participation rate (%) | ||||||||||
| 1 | 75.9 | 70.4 | 72.5 | 72.3 | 70.6 | 84.8 | 83.3 | 83.4 | 68.4 | 64.9 |
| 2 | 70.7 | 69.9 | 70.3 | 67.6 | 83.3 | 84.3 | 84.6 | 71.6 | 69.8 | |
| 3 | 69.3 | 67.9 | 65.7 | 81.4 | 82.3 | 83.6 | 72.0 | 72.7 | ||
| 4 | 70.2 | 66.7 | 77.7 | 78.4 | 81.6 | 77.1 | 75.7 | |||
| 5 | 67.4 | 66.1 | 69.7 | 74.5 | 84.2 | 82.9 | ||||
| 6 | 65.3 | 68.7 | 70.2 | 84.1 | 82.8 | |||||
| 7 | 67.2 | 67.8 | 79.6 | 79.8 | ||||||
| 8 | 67.2 | 69.3 | 66.8 | |||||||
| 9 | NR | 68.4 | 68.0 | |||||||
 : invitation round 1–5.
: invitation round 1–5.
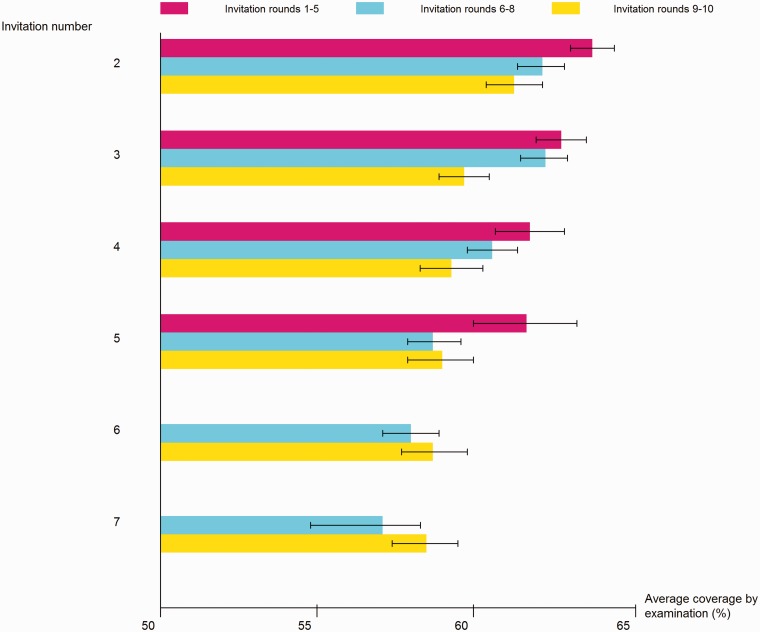
Coverage by examination for the newly recruited women was 72.5% for cohort 1, but dropped below 70% for cohort 3 onwards, and was 64.2% for cohort 8. For cohorts 1–4, coverage by examination dropped by increasing invitation number, for cohort 1 from 72.5% at invitation 1 to 52.4% at invitation 9 (Table 1 and Figure 2). Cohorts 5–8 started out with a lower coverage by examination (around 63%) than the previous cohorts, but tended to maintain this level through the next 3–4 invitations. Two changes in the invitation scheme affected invitation rounds 9 and 10. First, previous administrative exclusions due to technical errors were deleted. Second, women not participating in the previous two rounds were not invited. These changes did not clearly affect the coverage by examination in the earliest cohorts, probably because these old cohorts would have accumulated many technical errors, and the deletion of these errors would tend to increase coverage by examination, and because the omitting to invite those not attending the last two times would tend to decrease coverage by examination. However, in cohorts 5–8, where less technical errors were accumulated, omitting to invite women not attending the last two times clearly resulted in a decrease in coverage by examination, e.g. from 63.8 to 60.8%/58.5% in cohort 6. In cohort 8, this change would be expected only in invitation 3, which was also the case.
Figure 2.
Average coverage by examination (%) for cohorts of women first targeted by the Copenhagen programme age 50–51 by invitation number and invitation round.
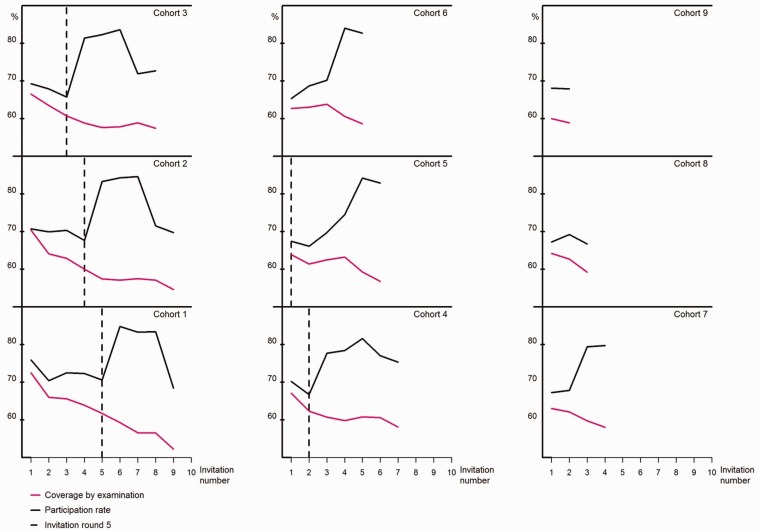
Participation rate at first invitation number was 75.9% for cohort 1, but dropped below 70% from cohort 5 onwards, reaching 67.2% for cohort 8 (Table 1). For cohort 1, the dramatic changes in coverage by invitation across invitation number were reflected in opposite dramatic changes in the participation rate, increasing from 70.6% at invitation 5 to 84.8% at invitation 6 and then dropping again to 68.4% at invitation 9. Similar patterns were seen for the other cohorts. While the changes due to the errors in the invitation scheme during invitation rounds 6–8 became less visible in the participation rates for the later cohorts, the drop in coverage by invitation during invitations rounds 9 and 10 was clearly reflected in increased participation rates.
The interplay between coverage by examination and participation rate is illustrated in Figure 3. The figure clearly shows the gap that developed between the two measures after invitation 5.
Figure 3.
Coverage by examination (%) and participation rate (%) for cohorts of women first targeted by the Copenhagen programme age 50–51 by invitation number.
Discussion
This study demonstrates the impact of the invitation scheme on the European Union quality indicators for mammography screening. We had four important observations. First, the participation rate in an organized mammography screening programme seemed highly dependent on the invitation scheme, with about a 20% increase (e.g. invitation 4 from 67.6 to 84.1%/79.8%) when invitations were restricted to those who participated in the previous round. Second, coverage by examination seemed to decrease by between 8 and 16% with increasing invitation number over seven invitation rounds (e.g. cohort 4 from 67.1 to 58.0%). Third, for the latest recruited cohorts the coverage by examination tended to drop by 5–10% when non-attenders from the previous round were not re-invited (e.g. cohort 6 from 63.8 to 60.8%/58.5%). This change was less visible in the earlier recruited cohorts, where it was balanced out by simultaneous deletion of old technical errors. Fourth, over time the participation rate became an increasingly bad indicator of coverage by examination (e.g. cohort 1 showing a gap from 68.4 to 52.4% at invitation 9).
Our study had several strengths. Because the CRS tracks all residents in Denmark, we could on each starting date of an invitation round identify the closed cohort of women aged 50–51 and living in the municipality of Copenhagen. All invitations and participations were recorded in the programme registers. Linkage between CRS and screening registers was based on the unique personal identification numbers, so we could accurately identify the target population, the invited women, and the participating women. Many studies have documented the impact of the information approach on the participation in screening.7–10 It is a further strength of our study that throughout the entire study period, invited women received a personal invitation letter with a fixed, changeable date of appointment.
A limitation in the study was that because the latest ineligibility code was not kept in the system for invitation rounds 9–10, it was not possible to separate out the impact of changes in ineligibility criteria from the impact of errors in the invitation data. However, the only quantitatively important change in ineligibility was probably the increase in coverage by invitation from 95.6% in invitation round 1 to 99.5% in invitation round 2, when the linkage with the register of the Danish Breast Cancer Cooperative Group stopped. In invitations rounds 1–7, some women could be 53 before their first invitation. The new invitation scheme by attained age was introduced to remedy this problem. For that reason, in invitation rounds 8–10 women turning 50 before their birth cohort had been invited were invited in the current round. In invitation round 10, those turning 70 during the round were invited in total only nine times. To take account of this, from invitation round 11 onwards, all women are now invited before they turn 70.
Based on our results it might be expected that a high coverage by invitation would be associated with a low participation rate, however such an association could not be found in the survey data from 25 European screening programmes.2 Both coverage by invitation and participation rate can be affected by local factors, complicating comparison across European countries.
For mammography screening to decrease breast cancer mortality in the targeted population, coverage by examination must be high.1,11 Breast cancer mortality in the target population of the Copenhagen programme decreased by 25% during the first 10 years after the programme started.12 These results derived from the early recruited cohorts starting out with a coverage by examination of 67–73%. However, the cohorts recruited later started out with a coverage by examination of 63–64%, a drop expected to have an impact on the outcome of screening at the population level. During the first 10 years of the Copenhagen programme, breast cancer mortality in screened women dropped by 37%, and this effect is expected to be seen also in screened women from later recruited cohorts.
The slight drop in coverage by examination following the cessation of re-invitation of non-attenders was seen for the later, but not the earlier cohorts, probably due to the coinciding deletions of technical errors. The drop is a matter of concern, especially because the later cohorts already had a lower coverage by examination at first invitation than previous cohorts. In 2015, the Copenhagen programme went back to the previous procedure and now re-invites all women except those who actively opted out. We will thus never get long-term data from Copenhagen on the impact of the limited invitation scheme. Nevertheless, our data can serve as a warning for other programmes that for logistical reasons want to limit invitations to previous attenders.
The European Guidelines1 use coverage by invitation, coverage by examination, and participation rate as quality indicators, but acceptable and desirable levels of achievement are given only for the participation rate (70 and 75%, respectively). There are good reasons for this limitation, as the participation rate can normally be calculated from the screening programme data alone, while the two other measures require access to accurate and updated population data. Our study nevertheless demonstrated that the participation rate can be considerably higher than the coverage by examination. Unless limitations in the invitation scheme are taken into account, health authorities focusing on the participation rate may expect their target population to be better protected against death from breast cancer by a screening programme than is actually the case.
Our study demonstrates the complexity of measuring even simple quality indicators, such as coverage by invitation, coverage by examination, and participation rate. Part of this complexity may be derived from errors in the invitation scheme in the Copenhagen programme, but Denmark has better population registers than almost all other screening settings, and it is unlikely that errors such as those in the Copenhagen programme would not also occur in other programmes. The difference may be that the quality of the Danish registers allowed the impact of such errors to be documented.
Conclusion
Our study demonstrates that coverage by examination tended to decrease over successive rounds of a mammography screening programme. The participation rate was highly sensitive to changes in the invitation scheme, increasing considerably when previous non-attenders were not re-invited. We observed a considerable gap between the coverage of examination and the participation rate, strongly indicating that the latter cannot, without reservations, be taken as an indicator of the former. Health care administrators should be aware of this interplay between the quality indicators, in order to avoid that interpretation that the participation rate is a direct reflection of the coverage by examination.
Supplementary Material
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Perry N, Broeders M, de WC, et al. European guidelines for quality assurance in breast cancer screening and diagnosis. Fourth edition—summary document. Ann Oncol 2008; 19: 614–622. [DOI] [PubMed] [Google Scholar]
- 2.Giordano L, von KL, Tomatis M, et al. Mammographic screening programmes in Europe: organization, coverage and participation. J Med Screen 2012; 19: 72–82. [DOI] [PubMed] [Google Scholar]
- 3.Domingo L, Jacobsen KK, von Euler-Chelpin M, et al. Seventeen-years overview of breast cancer inside and outside screening in Denmark. Acta Oncol 2013; 52: 48–56. [DOI] [PubMed] [Google Scholar]
- 4.von Euler-Chelpin M, Olsen AH, Njor S, et al. Socio-demographic determinants of participation in mammography screening. Int J Cancer 2008; 122: 418–423. [DOI] [PubMed] [Google Scholar]
- 5.Jacobsen KK, von Euler-Chelpin M. Performance indicators for participation in organized mammography screening. J Public Health (Oxf) 2012; 34: 272–278. [DOI] [PubMed] [Google Scholar]
- 6.Jensen A, Olsen AH, von Euler-Chelpin M, et al. Do nonattenders in mammography screening programmes seek mammography elsewhere? Int J Cancer 2005; 113: 464–470. [DOI] [PubMed] [Google Scholar]
- 7.Denhaerynck K, Lesaffre E, Baele J, et al. Mammography screening attendance: meta-analysis of the effect of direct-contact invitation. Am J Prev Med 2003; 25: 195–203. [DOI] [PubMed] [Google Scholar]
- 8.Giordano L, Stefanini V, Senore C, et al. The impact of different communication and organizational strategies on mammography screening uptake in women aged 40–45 years. Eur J Public Health 2012; 22: 413–418. [DOI] [PubMed] [Google Scholar]
- 9.Goelen G, De CG, Hanssens S. A community peer-volunteer telephone reminder call to increase breast cancer-screening attendance. Oncol Nurs Forum 2010; 37: E312–E317. [DOI] [PubMed] [Google Scholar]
- 10.Hegenscheid K, Hoffmann W, Fochler S, et al. Telephone counseling and attendance in a national mammography-screening program a randomized controlled trial. Am J Prev Med 2011; 41: 421–427. [DOI] [PubMed] [Google Scholar]
- 11.Klabunde CN, Sancho-Garnier H, Broeders M, et al. Quality assurance for screening mammography data collection systems in 22 countries. Int J Technol Assess Health Care 2001; 17: 528–541. [PubMed] [Google Scholar]
- 12.Olsen AH, Njor SH, Vejborg I, et al. Breast cancer mortality in Copenhagen after introduction of mammography screening: cohort study. BMJ 2005; 330: 220–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.