Abstract
Background
Coronary artery disease (CAD) occurs at younger age in India but only a limited number of studies have evaluated risk factors and management status. This is a multisite observational registry to assess risk factors and treatment patterns in young patients presenting with acute coronary syndrome (ACS) and stable ischemic heart disease (IHD).
Methods
We recruited 997 young patients (men <55, women <65 y) presenting with ACS or stable IHD successively at 22 centers across India. Details of baseline risk factors and management status were obtained. Descriptive statistics are reported.
Results
Mean age of participants was 49.1 ± 8y, 72% were men and 68% had ACS. Family history of CAD was in 50%, diabetes 44%, hypertension 49%, history of dyslipidemia 11%, smoking/tobacco use 39%, and sedentary habits in 20%. 1.3% had “possible familial hypercholesterolemia”. Metabolic risk factors (high BMI, diabetes and hypertension) were significantly greater in women (p < 0.01). Women were older at diagnosis of CAD and presented more often with non-ST elevation ACS. In the study cohort antiplatelet use was in 85%, beta-blockers 38%, statins 63% and ACE inhibitors/ARBs in 41% while in ACS patients it was 80.5%, 54.6%, 80.8% and 40.8%, respectively. 35.9% patients underwent percutaneous coronary intervention while coronary bypass surgery was performed in 10.4%.
Conclusions
Conventional risk factors including family history continue to play a pivotal role in premature CAD in Indians. Women have more of metabolic risk factors, present at a later age and have non-ST elevation ACS more often. There is a need to focus on improving use of evidence-based drug therapies and interventions.
Keywords: Premature CAD, Coronary risk factors, Epidemiology, Drug therapy
1. Introduction
Cardiovascular diseases (CVD) are the most important causes of mortality and morbidity in India1. Global Burden of Diseases (GBD) Study has reported that from year 1990 to 2013, IHD in India increased to become number 1 cause of death2. This study also reported that number of patients with IHD increased from less than a million to 2 million. IHD in India is characterized by increasing numbers, regional variations, premature onset, poor management and greater mortality1, 3.
Premature IHD can have devastating consequences for the individual, the family, and the society4. INTERHEART study reported that 9 standard risk factors- dyslipidemia (high apolipoprotein B/apolipoprotein A1 ratio), smoking, hypertension, diabetes, high waist-hip ratio, unhealthy diet, low physical activity, irregular alcohol consumption and psychosocial stress- explained more than 90% of the first acute myocardial infarction5. Premature IHD in the South Asian region was explained due to premature onset of the same biological risk factors in the INTERHEART study6. Smaller case-control studies in India have reported importance of these risk factors7. A case-control study highlighted importance of thrombotic (smoking, low fruit/vegetables intake, fibrinogen, homocysteine) as well as atherosclerotic (hypertension, high fat diet, dyslipidemia) risk factors in causing premature IHD8. Quality of care of acute coronary syndrome (ACS) patients in India has been reported in large registries. The nationwide CREATE registry (n = 20468) reported that use of evidence based medical drugs (thrombolytics, beta-blockers, antiplatelets, RAAS blockers and statins) as well as revascularization (coronary interventions or surgery) was low9. Similar results were reported in Kerala ACS registry (n = 25748)10 and multicenter DEMAT11 and SPREAD12 registries. However, all these studies were focused in all age-groups and not in premature IHD patients. We undertook a multi-centric, prospective, observational study across India to find out possible risk factors associated with CAD among young Indian population. The study included not only patients of ACS but also patients with stable IHD, and analyzed different treatment strategies.
2. METHODS
Coronary Artery Disease in the Young (CADY) is a prospective observational study to examine the risk factor profile and management strategies in premature CAD in a cohort of Indian patients. 997 patients were recruited in 22 participating centers between November 2010 and January 2012. The centers are distributed across India, more from South India (Fig. 1). Men less than 55 years of age and women less than 65 years presenting with CAD or those with established CAD on follow up were included in the study. The diagnosis of CAD was made by a positive stress test or a definite imaging technique. Patients who had prior PTCA or CABG were also included in the study. Ethics clearance was obtained from the central coordinating unit and individual sites. Informed consent was obtained from all patients.
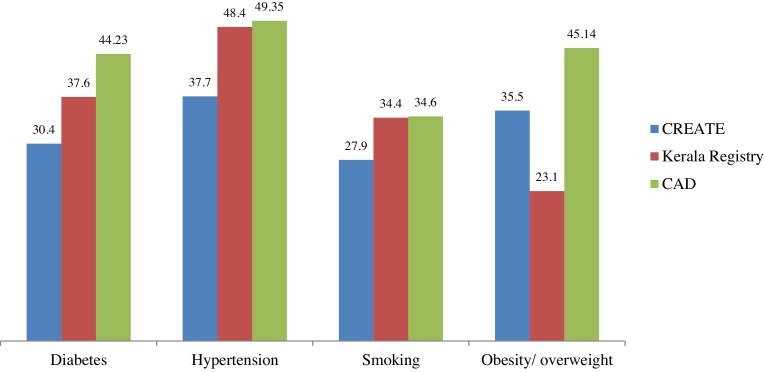
Fig. 1.
Comparison of Risk factors.
The data collection was performed either by the designated staff or trained research coordinators. Demographic data regarding socioeconomic status and age were collected. Medical history of associated risk factors such as hypertension, diabetes, dyslipidemia, stroke and peripheral vascular disease were documented. Data on lifestyle factors such as diet, smoking, non-smoked tobacco use, alcohol consumption, exercise patterns and psychosocial factors were also obtained. Data regarding socioeconomic status was obtained using Kuppuswami classification13 and for psychosocial stress we used the modified INTERHEART questionnaire14. Details of hospitalization including diagnostic tests, medications and laboratory tests were obtained from hospital records. Dutch lipid clinic network (DLCN) criteria was used to identify patients with familial hypercholesterolemia. TIMI score for patients with non-Q ACS15 were also calculated during hospitalization. Treatment advice at discharge was noted from the hospital records. Although the study was designed to gather follow-up information up to 24 months after enrolment this report is restricted to the data available at discharge.
2.1. Statistical analyses
All the data were computerized and data analysis performed using EpiInfo programme. Descriptive statistics are reported.
The study is registered with Clinical Trials Registry of India at www.ctri.nic.in (CTRI/2012/12/003232).
3. Results
Patient enrolment was performed in different parts of the country to cover various geographical regions. Of the 997 participants, 714 (72%) were men. Mean age of study participants was 49.1 years, 46.7 years in men and 55.1 years in women. Out of 997 patients, 680 (68%) had ACS and 317 (32%) stable IHD. Of the 680 ACS patients, 51% had ST-elevation myocardial infarction (STEMI) and 49% had NSTE-ACS. According to the universal definition of myocardial infarction16, it was determined that 3 patients had type-2, 2 had type-4b and the rest had type-1 infarctions. Of these, 348 had STEMI and 158 had non-STEMI. 57.6% of patients with NSTE-ACS had a TIMI score of 3 or greater.
Socio-demographic characteristics and associated risk factors are shown in Table 1, Table 2. 75.6% of participants belonged to middle socioeconomic status. Moderate to high psychosocial stress level was reported in 55.9% of the study population. Family history of premature IHD was present in half of the participants (49.6%) and was more in men (72.3%) as compared to women (27.7%). Significant proportion of participants had modifiable risk factors: hypertension 49.3%, diabetes 44.2%, dyslipidemia 11.4%, smoking and/or tobacco use 38.6%, overweight/obesity in 56.3% and sedentary habits in 19.5%. 210 (21%) patients had previous coronary interventions (PCI) or coronary bypass surgery, 14 (1.4%) peripheral arterial disease and 11 (1.1%) had stroke. Women, as compared to men, had greater prevalence of diabetes (62.1 vs 37.1%, p < 0.001), hypertension (72.1 vs 40.3%, p < 0.0001) and overweight/obesity (60.1 vs 35.2%, p < 0.0001), whereas men had greater prevalence of smoking/tobacco use (52.7 vs 3.2%, p < 0.0001). “Possible Familial Hypercholesterolemaia” (FH) was diagnosed in 13 (1.3%) patients applying DLCN criteria, mean age being 55.07 years, 08 were male patients and 10 had ACS and others stable IHD.
Table 1.
Socio-demographic characteristics.
| Total | Male | Female | |
|---|---|---|---|
| Age, years – Mean (SD) | 49.07 (8) | 46.67 (7) | 55.14 (7) |
| Psychosocial (n %) | |||
| Excellent | 44 (4) | 28 (4) | 16 (6) |
| Good/Fair | 937 (94) | 675 (95) | 262 (93) |
| Poor | 11 (1.10) | 6 (0.84) | 5 (1.76) |
| Socioeconomic characteristics (n %) | |||
| Upper | 87 (9) | 74 (10) | 13 (5) |
| Middle | 755 (76) | 570 (80) | 185 (65) |
| Lower | 139 (14) | 64 (9) | 85 (30) |
Table 2.
Associated Risk Factors.
| Charactertistics | CAD n (%) | Male n (%) | Female n (%) | P-value |
|---|---|---|---|---|
| 997 | 714 | 283 | ||
| Age | 49.1 ± 8 | 46.67 ± 7 | 55.1 ± 7 | <0.001 |
| Diabetes Mellitus | 441 (44.23) | 265 (37.11) | 176 (62.19) | <0.0001 |
| Hypertension | 492 (49.35) | 288 (40.34) | 204 (72.08) | <0.0001 |
| Dyslipidemia | 114 (11.43) | 76 (10.64) | 38 (13.43) | 0.2119 |
| Psychosocial (fair and poor) | 559 (56.07) | 403 (56.44) | 156 (55.12) | 0.7050 |
| Physical activity (low) | 195 (19.56) | 120 (16.80) | 75 (26.50) | 0.0005 |
| Socioeconomic characteristics (upper) | 87 (8.73) | 74 (10.36) | 13 (4.59) | 0.0036 |
| Socioeconomic characteristics (Middle) | 755 (75.73) | 570 (79.83) | 185 (65.37) | <0.0001 |
| Socioeconomic characteristics (Lower) | 139 (13.94) | 64 (8.96) | 85 (30.04) | <0.0001 |
| Family history (Positive) | 495 (49.65) | 358(72.32) | 137 (27.68) | 0.6241 |
| Substance Use (Tobacco) | 385 (38.62) | 376 (52.66) | 9 (3.18) | <0.0001 |
| Waist circumference | 362 (36.31) | 251(35.15) | 111 (39.22) | 0.2301 |
| Body Mass Index (≥23) | 562(56.37) | 395 (55.32) | 167 (59.01) | 0.2891 |
Note: P < 0.05 implies significant difference between proportions.
Details of therapies are provided in Table 4. In the overall group, 834 (83.7%) received antiplatelet drugs (aspirin and/or clopidogrel), 632 (63.5%) statins, 413 (41.4%) ACE inhibitors/ARBs, and 386 (38.7%) beta blockers. Calcium channel blockers were prescribed in 94 (9.43%) patients and nitrates in 149 (14.9%). 358 (35.91%) underwent percutaneous coronary intervention, 261 (36.55%) being male and 97 (34.28%) being female patients. 104 (10.43%) underwent coronary bypass surgery.
Table 4.
Drug therapies in acute coronary syndrome and stable IHD groups.
| Evidence based drugs | Total 997 n (%) |
Acute coronary syndrome 680 n (%) |
Stable IHD 317 n (%) |
p value |
|---|---|---|---|---|
| Antiplatelet drugs | 835 (83.7) | 544(80.5) | 291(91.8) | <0.0001 |
| ACE inhibitors/ARBs | 413 (41.4) | 244(35.9) | 169 (53.3) | <0.0001 |
| Beta blockers | 386 (38.7) | 371(54.6) | 15(4.7) | <0.0001 |
| Statins | 637 (63.5) | 549(80.8) | 88(27.7) | <0.0001 |
In the hospitalized group of 735 patients, 649 had ACS and 86 had stable IHD. 561(86.2%) patients of ACS stayed in the hospital for 1–7 days, 29.3% for less than 48 hours. 42(43.7%); patients of stable IHD were in the hospital for 1–7 days, and 18.6% for less than 48 hours.
4. Discussion
This study shows that prevalence of standard coronary risk factors (smoking, hypertension, diabetes and dyslipidemia) is high in premature CAD in India and is similar to previous case-control studies from the country4 and registries (Fig. 1) Women with premature CAD have greater prevalence of metabolic risk factors as compared to men. High prevalence of family history, especially in men, is a unique finding and suggests importance of genetic factors17. This study also shows a low use of evidence-based therapies in ACS.
CREATE9, Kerala-ACS10 DEMAT11 and SPREAD study12 registries have provided information on coronary atherosclerotic risk factors, treatment patterns and outcomes in Indian populations. However, these studies included all age groups and only patients of ACS. Kerala ACS study was confined to the Kerala state population. The present study, a multisite, prospective registry included patients with ACS as well as patients with stable IHD from different states of the country, which would give a better overall view of the burden of CAD in the country. Moreover, this study focused on premature CAD, a major concern for patients, practitioners and policy makers in India. In the present study, of the 997 patients, 68% had ACS and 32% had stable IHD. Prevalence of premature stable IHD is an underestimate. On the basis of studies in US, it was estimated that there are 30 patients of stable IHD for every patient with ACS18. The situation is likely to be no different in our country and that gives an idea of the magnitude of the burden of premature IHD. Of the 680 ACS patients, 51% had STEMI and 49% had NSTE-ACS. In the CREATE registry STEMI was in 61% and the gap between numbers of STEMI and NSTE ACS has narrowed in the present study. Secular trends in awareness and treatment of risk factors and better management of stable IHD in India may have contributed to this “evolution” in CAD epidemiology. On the other hand, in the Kerala-ACS registry, STEMI rates were lower (37%) as compared to NSTE-ACS (63%). Kerala state which has the highest literacy rate in the country has probably marched much ahead in terms of epidemiological evolution.
Almost half of the study participants have history of premature CAD in the family. Parental history of premature CAD has been shown to be an important, independent, consistent and global determinant of future MI risk17. This association was not affected after adjustment for age-, sex-, region, and the 9 INTERHEART risk factors. High prevalence of family history, especially in men, points to presence of genetic factors in premature CAD in India. Although there are no large association studies of genetic factors with coronary atherosclerosis or ACS in India, studies among emigrant South Asians have reported that a few genetic markers are important. The markers with significant associations include 9p21 genotypes and a few single nucleotide polymorphisms. Large studies for identification of genetic markers are required among premature IHD patients. Meanwhile, clinicians caring for CAD patients should screen the close relatives of the patient for family history of premature CAD. Other risk factors included diabetes in 44%, hypertension in 49%, history of dyslipidemia in 11%, smoking/tobacco use in 39%, low physical activity in 20%, high BMI ≥23 kg/m2 in 56% and high waist circumference in 42%. These rates are similar to previous case-control studies although the INTERHEART study reported that dyslipidemia was the most important risk factor.
FH is underdiagnosed and undertreated, as the awareness is poor amongst medical and nonmedical communities. FH is a common genetic disorder, with global prevalence being 1 in 200, and is a common cause for premature CAD. From various criteria that are available for diagnosis of FH – MEDPED criteria, Dutch Lipid Clinic Network(DLCN) criteria, Simon Broom criteria, and Japanese criteria – DLCN criteria18 was applied to identify FH in this patient population. This takes into consideration family history, clinical history and findings, serum LDL-C levels and genetic testing. No genetic tests were carried out in our patients. Diagnostic yield of sequencing genes for LDL-receptors, apo-B and PCSK-9 is generally poor. In a study19 where genes were sequenced in 1,26,025 participants, it was seen that FH was detected in <2% of participants who had a serum LDL-C level of >190 mg%. Importantly, at any level of LDL-C, the CV risk is higher in subjects with mutation.
“Possible FH” was identified in 13(1.3%) patients. It is probably an underestimation for various reasons. Firstly, it was not prospectively and actively sought for. Only on a sound suggestion from a reviewer, this was done. Some of these patients were already on statins, altering the serum LDL-C values. Markers like xanthomas could have been missed. Genetic tests were not carried out. Clinical criteria may not be sufficient to assess prevalence of FH20. “Possible FH” have mutation in 20–30% of subjects. Since premature CAD is a major problem in our country and FH is probably one of the reasons, it is necessary to look for FH in our population.
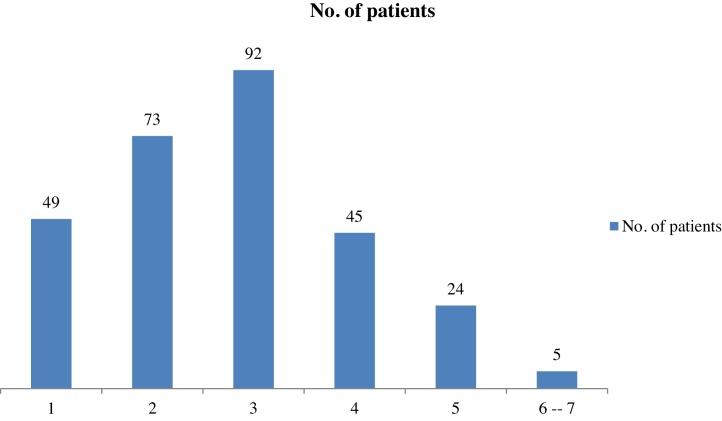
There is clearly a need to improve the utilization of evidence based drug therapy in patients with CAD, especially premature CAD in India. Availability of generic drugs and combination pills in the market are likely to enhance evidence based practice and adherence to therapy. We have observed that 46.1% of patients underwent PCI or CABG. Appropriateness of the procedures has not been analyzed. However, when we look at the NSTE-ACS patients, 57.6% had a TIMI score of 3 or more, making them eligible for intervention (Fig. 2). Once the diagnosis of CAD is established, appropriate treatment has to be instituted. Use of all the drug classes is suboptimal (Table 4) but is similar to CREATE and Kerala-ACS. Prospective Urban Rural Epidemiology (PURE)21 as well as Andhra Pradesh Rural Health Initiative (APRHI)22 studies have reported that treatment levels for secondary prevention in urban and rural areas in India are disappointing. In APRHI study use of aspirin, beta-blockers, ACE inhibitors/ARBs, and statins was severely underutilized. Of the patients with ischemic heart disease, fewer than 16%, 25%, 10%, and 6% were using aspirin, β-blockers, ACE inhibitors, and statins respectively.
Fig. 2.
Timi score for NSTE-ACS patients.
Dual antiplatelet therapy (DAPT) was received by 473 patients (all 358 patients undergoing PCI receiving DAPT), and 361 were on single antiplatelet.
The hospitalization period does appear longer than expected – only 29.3% of ACs patients and 18.6% of stable IHD patients staying in the hospital for less than 48 hours. The study did not look into the factors leading to prolonged hospitalization of these patients. The lack of health insurance coverage in the majority of patients, referral from and to other disciplines in the hospital for cardiac and non-cardiac evaluation and complications following interventions are possible explanations for a prolonged hospital stay.
4.1. Any thing new?
Though this study confirms the findings of the previous studies as regards CAD risk factors, there are two aspects which we feel should be communicated to the medical and non-medical community with renewed emphasis.
4.1.1. CAD in women
Various aspects of CAD, including epidemiology and clinical manifestations differ between men and women, and these differences are explained by biological factors like hormonal influence, and socio-cultural processes, like gender bias23. Women have clinical CAD presenting about 10 years later than it does in men. That means women have an additional period of 10 years to practise preventive measures to effectively counter CAD. The INTERHEART study (5) showed hypertension and diabetes were more important risk factors in young Indian women than men. And this study showed women to have more comorbidities like hypertension, diabetes, dyslipidemia and obesity, which are amenable to corrective preventive measures. Smoking amongst female population, is less prevalent, a characteristic feature which they would do well to retain and improve further. Women have a wider window of opportunities for prevention of premature CAD.
GUSTO IIb (Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes), TIMI IIIB (Thrombolysis In Myocardial Infarction), and the Euro Heart Survey studies showed that women present more frequently with unstable angina and non–ST-elevation myocardial infarction (NSTEMI), whereas men have ACS with ST elevation (STEMI).24, 25, 26 It has been shown that women are less likely to undergo reperfusion therapy after ACS.27, 28 In our study, women had NSTE-ACS more often than men (42% vs 29.8%), though not adjusted for age, and there was no gender bias in interventional treatment.
4.1.2. ACS vs Stable IHD
In case of secondary prevention of CAD, it is worth emphasizing another step – “Prevent stable IHD progressing to ACS”. The conventional risk factors for CAD account for 90% of acute cardio-vascular events.5 The conventional risk factors for the development of CAD – hypertension, hypercholesterolaemia, diabetes, sedentary life-style, obesity, smoking and a family history have an adverse influence on prognosis in those with established disease, since they influence the progression of atherosclerotic disease process. Appropriate intervention, if instituted can reduce the risk. Once the primary prevention fails, and the patient develops stable IHD, we should strive to prevent its progression to ACS, which would reduce mortality, morbidity and associated economic and psycho-social burden. The message is “If you fail to prevent the development of an atheromatous plaque, then preserve the stability of the atheromatous plaque”. Prevention of progression of the atheromatous plaque or even regression of the atheromatous plaque is a reality now, with effective secondary preventive measures.
Comparison between patients of ACS and stable IHD (Table 3) showed that low physical activity and increased waist circumference were significantly more common in patients with ACS, while diabetes, hypertension and lower psycho-social class were more frequent with stable IHD. Inflammatory markers (like hsCRP) were not assessed in the study, and the study is not equipped to explain these points. However, it is not inappropriate to surmise that physical activity and central obesity probably received less attention, while patients with diabetes and hypertension were adequately managed.
Table 3.
Distribution of patients falling in each characteristics by disease status.
| Characteristics – n (%) | Total | ACS | Stable IHD | P- Value |
|---|---|---|---|---|
| 997 | 680 (68.20) | 317 (31.80) | ||
| Diabetes Mellitus | 441 (44.23) | 280 (41.18) | 161 (50.79) | 0.0044 |
| Hypertension | 492 (49.35) | 320 (47.06) | 172 (54.26) | 0.0340 |
| Dyslipidemia | 114 (11.43) | 135 (19.85) | 61 (19.24) | 0.8181 |
| Psychosocial (fair and poor) | 559 (56.07) | 360 (52.94) | 199 (62.78) | 0.0036 |
| Physical activity (low) | 195 (19.56) | 148 (21.76) | 47 (14.83) | 0.0102 |
| Substance Use (Tobacco) | 385 (38.62) | 271 (39.85) | 114 (35.96) | 0.2380 |
| Waist circumference ((Females ≥80 cm and males ≥90 cm)) | 421 (42.23) | 326 (47.94) | 95 (29.97) | <0.0001 |
| Body Mass Index (≥ 23) | 562 (56.37) | 394 (57.94) | 168 (53) | 0.1416 |
| Family history (positive) | 495 (49.65) | 337 (49.56) | 158 (49.84) | 0.9362 |
| Socioeconomic characteristics | ||||
| Upper I | 87 (8.73) | 65 (9.56) | 22 (6.94) | 0.1738 |
| Upper Middle II | 454 (45.54) | 299 (43.97) | 155 (48.9) | 0.1471 |
| Lower Middle III | 301 (30.19) | 215 (31.62) | 86 (27.13) | 0.1499 |
| Upper Lower IV | 138 (13.84) | 87 (12.79) | 51 (16.09) | 0.1615 |
| Lower | 11 (1.1) | 9 (1.32) | 2 (0.63) | 0.3320 |
Framingham study29 has shown that aggressive life style measures reduce events in stable IHD. What we know from clinical studies is that aspirin, beta blockers, statins, ACE inhibitors and therapeutic life style changes reduce mortality in stable IHD and so do the appropriately instituted revascularization procedures. Before these measures were widely applied, the annual mortality rate in patients with stable IHD was 4.5%, and now it is 1–3%.30
The usage of drugs was suboptimal, as mentioned earlier. Antiplatelets and ACE-I/ARB’s were more frequently used in stable IHD patients than in ACS patients, while the use of BB and statins were more frequent in patients with ACS than in patients with stable IHD (Table 4), clearly indicating the urgent need to improve the awareness and practice of evidence based therapy.
Limitations of the study include the inherent limitations of registries such as biases because of regionality, gender-representation, and risk factor assessments as reported above. The follow up was also not adequate to comment on outcomes and adherence to therapy. On the other hand, this multi-centric observational registry of premature CAD in Indians indicates that the conventional risk factors are important and there is an urgent need to focus on these risk factors in primary and secondary prevention.
5. Conclusion
This multi-centric observational registry of premature CAD in Indians indicates that the conventional risk factors continue to be the major cause of CAD in the young. There is an urgent need to focus on these risk factors in primary and secondary prevention. It should not be difficult to correct underuse of life style modification and drugs. Effective secondary prevention would ensure stability of stable IHD. There is a greater scope for preventive practice in the female population, given the delayed onset of CAD and higher rate of comorbidities, offering more time and more opportunities.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.ihj.2016.09.009.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Gupta R., Guptha S., Sharma K.K. Regional variations in cardiovascular risk factors in India: India Heart Watch. World J Cardiol. 2012;4:112–120. doi: 10.4330/wjc.v4.i4.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. GBD 2013 Mortality and Causes of Death Collaborators. Lancet. 2015;385:117–170. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reddy K.S., Yusuf S. Emerging epidemic of cardiovascular disease in developing countries. Circulation. 1998;97:596–601. doi: 10.1161/01.cir.97.6.596. [DOI] [PubMed] [Google Scholar]
- 4.Sharma M., Ganguly N.K. Premature coronary artery disease in Indians and its associated risk factors. Vasc Health Risk Manag. 2005;1:217–225. [PMC free article] [PubMed] [Google Scholar]
- 5.Yusuf S., Hawken S., Ounpuu S. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 6.Joshi P., Islam S., Pais P. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297:286–294. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 7.Vamadevan S.A., Prabhakaran D. Coronary artery disease in Indians: implications of the INTERHEART study. Indian J Med Res. 2010;132:561–566. doi: 10.4103/0971-5916.73396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Panwar R.B., Gupta R., Gupta B.K. Atherothrombotic risk factors and premature coronary heart disease in India: a case-control study. Indian J Med Res. 2011;134:26–32. [PMC free article] [PubMed] [Google Scholar]
- 9.Xavier D., Pais P., Devereaux P.J. Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 10.Mohanan P.P., Mathew R., Harikrishnan S. Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS Registry. Eur Heart J. 2013;34:121–129. doi: 10.1093/eurheartj/ehs219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pagidipati N.J., Huffman M.D., Jeemon P. Association between gender, process of care measures, and outcomes in ACS in India: results from the detection and management of coronary heart disease (DEMAT) registry. PLoS One. 2013;8(April (4)):e62061. doi: 10.1371/journal.pone.0062061. Print 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kamath D.Y., Xavier D., Gupta R. Rationale and design of a randomized controlled trial evaluating community health worker-based interventions for the secondary prevention of acute coronary syndromes in India (SPREAD) Am Heart J. 2014;168(5):690–697. doi: 10.1016/j.ahj.2014.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar N., Shekhar C., Kumar P. Kuppuswamy’s socioeconomic status scale: updating for 2007. Indian J Pediatr. 2007;74:1131–1132. [PubMed] [Google Scholar]
- 14.Rosengren A., Yusuf S., Hawken S. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;17(364):953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 15.Pollack C.V., Frank D. Sites application of the TIMI risk score for unstable angina and non-ST elevation acute coronary syndrome to an unselected emergency department chest pain population. Acad Emerg Med. 2006;13:13–18. doi: 10.1197/j.aem.2005.06.031. [DOI] [PubMed] [Google Scholar]
- 16.Thygesen K., Alpert J.S., White H.D. Joint ESC/ACCF/AHA/WHF task force for the redefinition of myocardial infarction: universal definition of myocardial infarction. Eur Heart J. 2007;28:2525–2538. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 17.Chow C.K., Islam S., Bautista L. Parental history and myocardial infarction risk across the world: the INTERHEART Study. J Am Coll Cardiol. 2011;57:619–627. doi: 10.1016/j.jacc.2010.07.054. [DOI] [PubMed] [Google Scholar]
- 18.Civeira F. Guidelines for the diagnosis and management of heterozygous familial hypercholesterolemia. Atherosclerosis. 2004;173:55–68. doi: 10.1016/j.atherosclerosis.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 19.Khera A.V., Won H.H., Peloso G.M. Diagnostic yield and clinical utility of sequencing familial hypercholesterolemia genes in patients with severe hypercholesterolemia. J Am Coll Cardiol. 2016;67:2578–2589. doi: 10.1016/j.jacc.2016.03.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Ferranti S.D., Rodday A.M., Mendelson M.M. Prevalence of Familial Hypercholesterolemia in the 1999 to 2012 United States National Health and Nutrition Examination Surveys (NHANES) Circulation. 2016;133:1067–1072. doi: 10.1161/CIRCULATIONAHA.115.018791. [DOI] [PubMed] [Google Scholar]
- 21.Yusuf S., Rangarajan S., Teo K., Islam S., Li W. Cardiovascular risk and events in 17 low-, middle-and high-income countries. N Engl J Med. 2014;371:818–827. doi: 10.1056/NEJMoa1311890. [DOI] [PubMed] [Google Scholar]
- 22.Joshi Rohina, Clara K., Chow P., Krishnam Raju. Fatal and nonfatal cardiovascular disease and the use of therapies for secondary prevention in a rural region of India. Circulation. 2009;119:1950–1955. doi: 10.1161/CIRCULATIONAHA.108.819201. [DOI] [PubMed] [Google Scholar]
- 23.Vera R.Z., Sabine O.P., Eva P. Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. Eur Heart J. 2016;37:24–34. doi: 10.1093/eurheartj/ehv598. [DOI] [PubMed] [Google Scholar]
- 24.Hochman J.S., Tamis J.E., Thompson T.D. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. Global use of strategies to open occluded coronary arteries in acute coronary syndromes GUSTO IIb investigators. N Engl J Med. 1999;341:226–232. doi: 10.1056/NEJM199907223410402. [DOI] [PubMed] [Google Scholar]
- 25.Hochman J.S., McCabe B.S., Stone P.H. Outcome and profile of women and men presenting with acute coronary syndromes: a report from TIMI IIIB. TIMI investigators. Thrombolysis in myocardial infarction. J Am Coll Cardiol. 1997;30:141–148. doi: 10.1016/s0735-1097(97)00107-1. [DOI] [PubMed] [Google Scholar]
- 26.Hasdai D., Porter A., Rosengren A. Effect of gender on outcomes of acute coronary syndromes. J Am Coll Cardiol. 2003;91:1466–1469. doi: 10.1016/s0002-9149(03)00400-4. [DOI] [PubMed] [Google Scholar]
- 27.Alfredsson J., Stenestrand U., Wallentin L. Gender differences in management and outcome in non-ST-elevation acute coronary syndrome. Heart. 2007;93:1357–1362. doi: 10.1136/hrt.2006.102012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lansky A.J., Hochman J.S., Ward P.A. Percutaneous coronary intervention and adjunctive pharmacotherapy in women: a statement for healthcare professionals from the American Heart Association. Circulation. 2005;111:940–953. doi: 10.1161/01.CIR.0000155337.50423.C9. [DOI] [PubMed] [Google Scholar]
- 29.Lloyd-Jones D.M., Leip E.P., Larson M.G. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 30.Braunwald’s heart disease, 10th Edition. Stable ischemic heart disease, chapter 54, page 1190, Elsevier Saunders Philadelphia.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.