Abstract
Background
Cryoballoon ablation of atrial fibrillation (AF) involves successful electrical pulmonary vein isolation (PVI). Pulmonary vein (PV) ostial occlusion with cryoballoon is classically assessed using PV angiography. A pressure-guided technique to assess ostial occlusion has been evaluated in small cohorts with mixed results. We evaluated the efficacy of this pressure-guided PVI technique and its impact on reducing contrast and fluoroscopy time as compared to the traditional approach.
Methods
We evaluated patients with paroxysmal AF, who underwent cryoballoon PVI. Patients prior to January 20th, 2013 underwent confirmation of PV occlusion by angiography only. Patients ablated after this time had PV occlusion initially determined by pressure monitoring and further confirmed by contrast injection into the PV in most cases (Pressure-guided PVI). Differences in the volume of contrast used and fluoroscopy time were evaluated.
Results
46 patients had pressure-guided PVI and29 patients had occlusion of PV confirmed by angiography alone. Pressure-guided PVI was 99.5% successful in ablating AF, which was non-inferior to traditional method of PV isolation. This technique used an average of 8 cc of contrast and 21.5 min of fluoroscopy time, which was significantly less than the contrast amount used, and fluoroscopy time with angiographic isolation of PV.
Conclusion
Pressure-guided PVI is an effective method for cryoablation of AF. This method not only significantly reduces the volume of contrast used but also decreases the fluoroscopy without compromising the success of PVI.
Keywords: Atrial fibrillation, Pulmonary vein isolation, Cryoablation, Pressure-Guided technique, Cryoballoon catheter
1. Introduction
Pulmonary vein isolation (PVI) through catheter ablation is a well-established treatment for atrial fibrillation (AF) [1]. Focal point-by-point radiofrequency (RF) catheter ablation has demonstrated significant success in treating AF [2], [3]. As accomplishing PVI with RF catheter ablation is technically challenging, time-consuming, and dependent on operator competency, this led to the development of balloon-based ablation technologies such as cryoablation with a cryoballoon catheter (Arctic Front, Medtronic, Minneapolis, MN) [4], [5]. This technique creates uninterrupted, circumferential lesions around the target pulmonary vein (PV) without conduction gaps. Pulmonary vein occlusion is indispensable for attaining antral contact and PVI and is generally evaluated angiographically with the injection of an intravenous contrast. However, it is associated with prolonged fluoroscopy time and risks of contrast injection, such as contrast allergy and renal injury [6]. To overcome these potential complications, a novel technique to correlate PV occlusion with changes in a pressure curve recorded at the distal tip of the cryoballoon catheter has been described [5]. These studies, however, have shown mixed results with regards to the efficacy of the procedure. Therefore, we decided to look at our experience with the use of the pressure-guided PVI technique, evaluating its efficacy and the impact on reducing contrast and fluoroscopy time as compared to the traditional approach of using angiography alone to assess PV ostial occlusion.
2. Material and methods
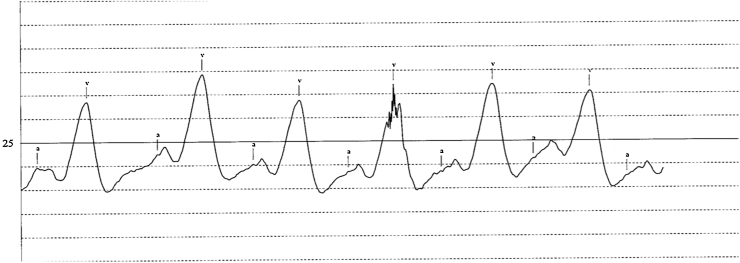
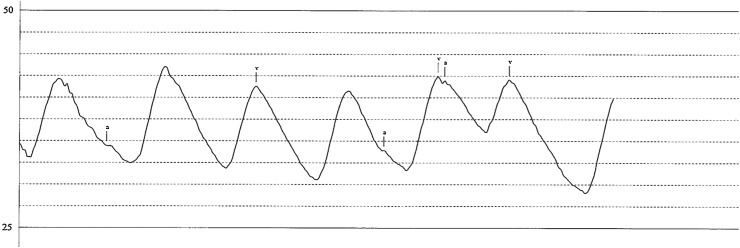
We retrospectively evaluated patients with paroxysmal AF who underwent cryoballoon PVI at Sanford Heart Hospital in Sioux Falls, South Dakota. Prior to January 20, 2013, patients underwent confirmation of PV occlusion by angiography only (angiography-guided PVI). Patients ablated after this time had PV occlusion initially determined by pressure monitoring and further confirmed by contrast injection into the PV (pressure-guided PVI). Each patient had a preprocedural CT to assess the size of the pulmonary vein ostium to allow appropriate sizing of the cryoablation balloon catheter. All procedures were performed under general anesthesia by one operator. We evaluated the volume of contrast used and the fluoroscopy time In the pressure-guided PV occlusion group, we used 28 mm cryoballoon catheter in all patients. In the angiographic PV occlusion group, 28 mm cryoballoon catheter was used in twenty-four patients, and in the remaining five patients, 23 mm cryoballoon catheter was used. An example of normal pressure waveforms in the left atrium obtained by the cryoablation catheter is shown in Fig. 1. The pressure waveforms obtained in the pulmonary vein after the successful ostial occlusion is shown in Fig. 2. Successful PVI was defined as the presence of entrance and exit blocks in the each of the PVs, when mapped with a circumferential-mapping catheter at the conclusion of the last freeze. All patients had four pulmonary veins, except for a single patient in the pressure-guided PVI group who had a single ostium for the left superior and inferior PV.
Fig. 1.
Pressure tracing from left atrium using the cryoablation catheter showing normal wave forms.
Fig. 2.
Pressure tracing obtained from the pulmonary vein after occlusion of the ostium using cryoballoon catheter.
3. Statistical analysis
We calculated the variables, mean and standard deviation for the contrast volume used in cc and fluoroscopy time in minutes. These variables were compared using an unpaired t-test. A p value of < 0.05 was considered statistically significant. We used GraphPad scientific software for the statistical analysis.
4. Results
We analyzed 183 PVs in 46 patients (61 ± 23 years old, 10 females) in the pressure-guided PVI group and 116 PVs in 29 patients (55 ± 20 years old, 14 females) in the PV occlusion confirmed by angiography alone group. The pressure-guided technique resulted in a high procedural success rate (99.45%), less contrast volume utilization (average: 8.05 cc) and less fluoroscopy time (average: 21.47 min) as shown in the table below (Table 1). In comparison, the exclusive angiographic isolation of PVs showed a relatively low success rate (96.55%), more contrast volume utilization (average: 29.84 cc) and more fluoroscopy time (average: 29.10 min). While the procedural success rates were similar, the contrast volume and fluoroscopy time were significantly lower in the pressure-guided PVI group as shown in the table below. Phrenic nerve palsy (PNP) was observed in 4.3% (2/46) of patients in the pressure-guided PV occlusion group and 6.9% (2/29) of patients in the angiographic PV occlusion group. Among these groups, one patient in each group had persistent PNP.
Table 1.
Representative Results.
| Pressure-Guided PV Occlusion (46 patients) |
PV Occlusion by Angiography Only (29 patients) |
p-value | |
|---|---|---|---|
| Number of PVs successfully ablated/total PVs (%) | 182/183 (99.45%) | 112/116 (96.55%) | 0.0764 |
| Contrast Volume in cc Mean (SD) |
8.05 (4.24) | 29.84 (15.29) | <0.0001 |
| Fluoroscopy Time in Minutes Mean (SD) |
21.47 (6.23) | 29.10 (8.26) | <0.0001 |
PV, pulmonary vein.
5. Discussion
The North American Arctic Front STOP-AF trial demonstrates a 69.9% long-term success rate with the first-generation cryoablation catheter compared to anti-arrhythmic agents, which is higher than the standard RF ablation based on a recent meta-analysis of randomized and observational studies [7].
The procedural success of cryoballoon ablation (CBA) depends on complete PV occlusion [6]. Initially, angiography constituted a method of confirming PV occlusion. However, due to the complications of radioiodine contrast, prolonged fluoroscopy times, and the frequent coexistence of chronic kidney disease in patients with AF, various predictors of PV occlusion and electrical isolation have been analyzed [8]. In 2009, Siklody et al. introduced the transesophageal-Doppler-echocardiography (TEE)-guided cryoballoon apposition of PV and electrical isolation [4]. This is, though, associated with periprocedural complications with general anesthesia and requires a well-trained echocardiographer throughout the procedure. A subsequently studied method involved a pressure-guided technique for assessing PV occlusion and electrical isolation by measuring the change from the left atrial (LA) to pulmonary artery (PA) pressure curve [5]. In this study, twelve patients were examined, and the pulmonary artery pressure waveform was obtained in 47 of 51 PVs. The Doppler TEE confirmed occlusion in all cases except for one left lower PV. In 2013, Kosmidou et al. assessed direct pressure monitoring for PV occlusion in thirty-five patients. An occlusive pressure waveform was established in 113 PVs, and among these, electrical isolation was achieved in 111 PVs (procedure success rate: 98.2%) [6]. The initial ten procedures required a contrast injection to assess PV occlusion. However, subsequent contrast utilization was minimized or eliminated in the remaining twenty-five procedures due to the accuracy and reproducibility of the occlusive pressure waveform.
In 2014, Safavi-Naeini et al. reported that a change in the pressure waveform at the distal tip of the cryoballoon from the LA pressure waveform to the PA waveform was not a reliable predictor of complete PV occlusion during cryoballoon ablation. They examined 72 PVs in eighteen patients. Among these, PV occlusion was achieved in 67/72 veins based on the change in the pressure waveform. To assess complete PV occlusion, a simultaneous administration of the contrast agent was performed. The study authors noticed that angiographic complete PV occlusion was detected in 43 of 67 PVs (64%) at the point when there was a change in the waveform from LA to PA. In the remaining 24 PVs, PV occlusion was completed with the adjustment of the cryoballoon under intracardiac echocardiographic guidance [8].
To date, we have conducted the largest observational analysis in terms of a number of patients and number of pulmonary veins examined to assess the accuracy of change in the pressure waveform from LA to PA at the distal tip of the cryoballoon catheter to confirm PV occlusion in the CBA of atrial fibrillation. Our study results showed that the procedural success rate of the pressure-guided technique for PVI and shorter fluoroscopy time are analogous to previously published studies [5], [6]. The procedural complication of right phrenic nerve palsy (total 5.3%) is similar to the previously published studies [9].
Our study is a retrospective analysis of data. Moreover, it is a single-center, single-operator study, which may bias the results. Also, we used two 180-s cryo applications for pressure-guided PVI versus two 240-s applications in the angiography-only group which may bias the observed findings in the catheterization laboratory. The fact that there was an improved learning curve for the provider involved would also be one of the limitations of our study.
6. Conclusion
Cryoballoon ablation for atrial fibrillation through pressure-guided occlusion and electrical isolation of PVs is a safe, fast, and effective strategy. Most importantly, it is associated with decreased contrast usage and fluoroscopy time
Conflict of interest
All authors declare no conflict of interest related to this study.
Acknowledgements
None.
References
- 1.Su W., Kowal R., Kowalski M. Best practice guide for cryoballoon ablation in atrial fibrillation: the compilation experience of more than 3000 procedures. Heart Rhythm: Off. J. Heart Rhythm Soc. 2015;12(7):1658–1666. doi: 10.1016/j.hrthm.2015.03.021. [DOI] [PubMed] [Google Scholar]
- 2.Calkins H., Reynolds M.R., Spector P. Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews and meta-analyses. Circ. Arrhythm. Electrophysiol. 2009;2(4):349–361. doi: 10.1161/CIRCEP.108.824789. [DOI] [PubMed] [Google Scholar]
- 3.Wilber D.J., Pappone C., Neuzil P. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA. 2010;303(4):333–340. doi: 10.1001/jama.2009.2029. [DOI] [PubMed] [Google Scholar]
- 4.Siklody C.H., Minners J., Allgeier M. Cryoballoon pulmonary vein isolation guided by transesophageal echocardiography: novel aspects on an emerging ablation technique. J. Cardiovasc. Electrophysiol. 2009;20(11):1197–1202. doi: 10.1111/j.1540-8167.2009.01524.x. [DOI] [PubMed] [Google Scholar]
- 5.Siklody C.H., Minners J., Allgeier M. Pressure-guided cryoballoon isolation of the pulmonary veins for the treatment of paroxysmal atrial fibrillation. J. Cardiovasc. Electrophysiol. 2010;21(2):120–125. doi: 10.1111/j.1540-8167.2009.01600.x. [DOI] [PubMed] [Google Scholar]
- 6.Kosmidou I., Wooden S., Jones B., Deering T., Wickliffe A., Dan D. Direct pressure monitoring accurately predicts pulmonary vein occlusion during cryoballoon ablation. J. Vis. Exp. JoVE. 2013;72:e50247. doi: 10.3791/50247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Packer D.L., Kowal R.C., Wheelan K.R. Cryoballoon ablation of pulmonary veins for paroxysmal atrial fibrillation: first results of the North American Arctic Front (STOP AF) pivotal trial. J. Am. Coll. Cardiol. 2013;61(16):1713–1723. doi: 10.1016/j.jacc.2012.11.064. [DOI] [PubMed] [Google Scholar]
- 8.Safavi-Naeini P., Shanoon F., Nazeri A. Cryoballoon pressure waveform change during balloon inflation is not a reliable predictor of adequate pulmonary vein occlusion. Pacing Clin. Electrophysiol. PACE. 2014;37(12):1702–1707. doi: 10.1111/pace.12491. [DOI] [PubMed] [Google Scholar]
- 9.Andrade J.G., Khairy P., Guerra P.G. Efficacy and safety of cryoballoon ablation for atrial fibrillation: a systematic review of published studies. Heart Rhythm: Off. J. Heart Rhythm Soc. 2011;8(9):1444–1451. doi: 10.1016/j.hrthm.2011.03.050. [DOI] [PubMed] [Google Scholar]