Abstract
Background:
Suture-button repair is a widely accepted surgical treatment for acute and isolated ankle syndesmosis injuries. To our knowledge, midterm results have not previously been reported.
Purpose:
To evaluate the clinical, qualitative, and quantitative radiological midterm outcomes of suture-button repair after acute isolated ankle syndesmosis injuries.
Study Design:
Retrospective case series; Level of evidence, 4.
Methods:
Clinical outcomes were measured using the Foot and Ankle Disability Index (FADI) and the American Orthopaedic Foot and Ankle Society (AOFAS) score. Three-tesla magnetic resonance imaging (MRI) was performed bilaterally at the ankle. Besides morphological sequences for evaluation of the syndesmosis and degenerative changes of the ankle using the Ankle Osteoarthritis Scoring System (AOSS), the MR protocol included a coronal 2-dimensional multislice multiecho sequence for quantitative cartilage T2-weighted mapping. Spearman correlations and paired t tests were used for statistical analysis.
Results:
This retrospective study included 19 consecutive patients (mean age, 29.7 ± 11.5 years) with acute isolated syndesmosis injuries treated with a suture-button system between January 2006 and June 2014, with a mean follow-up of 5.1 ± 2.6 years. Postoperatively, the median FADI score was 136 (range, 78-136), and the median AOFAS score was 100 (range, 87-100). Seventeen (89.5%) patients reported to have reached their preinjury level of sports activities. MRIs of 16 patients were obtained and all showed intact anterior and posterior syndesmotic ligaments; however, in most patients, the previously injured syndesmotic ligament was thickened compared with the uninjured ankle. Average width of the anterior (P = .81) and posterior (P = .60) syndesmosis was not significantly different between the ipsilateral (3.2 ± 1.2 and 4.4 ± 0.9 mm) and contralateral ankles (3.0 ± 0.6 and 4.2 ± 0.7 mm). The median AOSS score was 1.5 (range, 0-11) for the ipsilateral ankle and 0 (range, 0-6) for the contralateral ankle. T2 values of articular cartilage did not significantly differ between the involved and the uninjured ankle (P = .68). Five patients needed hardware removal due to persistent skin irritation, and 1 patient suffered from reinstability of the ankle resulting in revision surgery 2 years after the index surgery.
Conclusion:
Suture-button fixation is an excellent treatment for acute and isolated syndesmosis injuries, resulting in stable ankles without early or advanced osteoarthritic changes at midterm follow-up.
Keywords: syndesmosis, upper ankle joint, suture-button, tight-rope, T2-weighted mapping
Proper treatment of isolated injuries of the syndesmosis complex is challenging but needed to avoid chronic instability, cartilage damage, and early osteoarthritic changes of the ankle joint. Thus, several treatment options have been discussed in the literature.11 Conservative treatment is recommended in stable syndesmotic injuries; these mainly include lesions of the anterior inferior tibiofibular ligament with or without integrity of the interosseous ligament with an intact deltoid ligament and the absence of subjective instability.26
Unstable syndesmotic injuries, mostly with additional lesions of the deltoid ligament, should be managed operatively.26,27 If treated operatively, 2 different procedures are widely used: insertion of a syndesmotic screw and suture-button fixation. Insertion of a syndesmotic screw results in a more rigid fixation of the syndesmosis, and importantly, early weightbearing can cause screw breakage.3 Another disadvantage of the traditional syndesmotic screw is that it requires obligatory implant removal after the index operation; the hardware removal rate with the suture-button device is significantly lower.7,22 Alternatively, fixation with a suture-button allows physiological micromovement between the distal tibia and fibula. This also enables early postoperative weightbearing and adequate reduction of the syndesmosis.12,21,23,29 Over the past few years, syndesmotic injuries, mostly associated with bony or further ligament lesions, were treated more commonly with the suture-button fixation system and have shown promising postoperative outcome results in short-term follow-up.5,7,17,22
The objective of the current study was to assess the clinical and magnetic resonance imaging (MRI) outcomes of a suture-button fixation system used to treat acute instability of tibiofibular syndesmotic lesions. Our hypotheses were that patients would neither suffer from any pain or malfunction nor would there be any relevant lesions of the cartilage after treatment with a suture-button fixation system.
Methods
The study was approved by the institutional ethics committee and registered in the German clinical trial registry; informed consent was obtained from all patients. Inclusion criteria for this study consisted of adult patients of both sexes who were treated operatively for isolated and acute (within 3 weeks after trauma9) lesions to the syndesmotic complex with a suture-button fixation system. Syndesmotic lesions were concurrently diagnosed as unstable due to either objective instability in clinical examination or the patient’s subjective instability in combination with a verified lesion of the syndesmosis on a 3-T MR image. Proceeding with surgical management was decided by findings from clinical examination, standard anteroposterior and lateral radiographs, MR scans, and the patient’s demands. More precisely, we indicated surgery when clinical examination of the upper ankle joint (squeeze test, Kleiger test, tenderness proximally over the anterior tibiofibular ligament and proximal along the interosseous membrane1) showed an instable ankle joint, MR examination showed a torn anterior and/or posterior tibiofibular ligament, and patients considered themselves as highly active.
Exclusion criteria were patients with additional pathologies (eg, fractures or osteochondral lesions) affecting the ankle, additional operative treatment, or chronic tibiofibular instability.
All syndesmotic injuries were treated with the suture-button system during the study period, and no patient was excluded from the study because of other types of fixation.
Surgical Technique
All patients were placed in the supine position. After incision on the lateral fibula, the ankle was placed in moderate plantar flexion, which facilitates accurate fibular reduction into the incisural notch of the tibia. Under fluoroscopy, the reduction was held in place with a Weber clamp and carefully controlled in all planes. Afterward, a Kirschner wire (K-wire) was inserted approximately 2 cm proximal of the tibiotalar joint, and a parallel entrance position was controlled for under fluoroscopy in anteroposterior and lateral views. The K-wire was overdrilled by the 4-mm cannulated drill and the Tightrope (Arthrex) inserted. The medial button was passed through the medial cortex of the tibia, and the pulley was tightened to complete the reduction of the tibiofibular joint (confirmed by fluoroscopy). When both buttons were flush with the bone, the FiberWire (Arthrex) was hand tied on the lateral side, with the foot in 20° of internal rotation and 10° of plantar flexion, and cut to 1 cm in length.24 Postoperatively, all patients were placed in a short-leg splint in the neutral position, and weightbearing was prohibited for 2 weeks. After suture removal at 2 weeks, the splint was removed and a pneumatic cam boot was applied. Range of motion (ROM) was restricted to plantarflexion/dorsiflexion 20°/0°/0° and no pronation for 6 weeks. After 6 weeks of full weightbearing, anteroposterior and lateral views were obtained, and the boot was removed before allowing full mobilization of the ankle. Strengthening and running were allowed after 6 weeks; full return to competitive sports was permitted after 10 to 12 weeks.
Functional and Subjective Assessment
All patients were assessed between March and April 2016 at final follow-up. Assessment consisted of a clinical examination and MRI of both ankles as well as a postoperative questionnaire. The postoperative questionnaire included: level of sporting activities, the German version of the Foot and Ankle Disability Index (FADI),16 presence of irritations caused by the medial or lateral suture button, and whether the patient underwent removal of the suture button. Furthermore, subjective level of satisfaction of surgical treatment, scored as excellent, good, fair, or poor, was recorded. All patients were examined by 2 orthopaedic surgeons (F.P.F. and J.P.).
Patients also underwent clinical examination of both ankles, which included measurement of ROM using a goniometer. Medial and lateral stability were also tested, and the American Orthopaedic Foot and Ankle Society (AOFAS) ankle hindfoot scoring data were calculated.
Radiological Assessment
High-resolution 3-T MRI of the ipsilateral and contralateral ankles was performed using a whole-body scanner (Ingenia; Philips Healthcare) with a dedicated 8-channel foot ankle coil (Figure 1) with the foot in slight dorsal-extension. In addition to morphological sequences (see the Appendix), a 2-dimensional multislice multiecho (MSME) spin-echo T2-weighted mapping sequence was acquired for cartilage T2 relaxation time measurements. A 3-dimensional T1-weighted gradient echo sequence with short echo times was acquired for morphological detection of calcifications of the syndesmosis. Detailed MR parameters are given in the Appendix.
Figure 1.
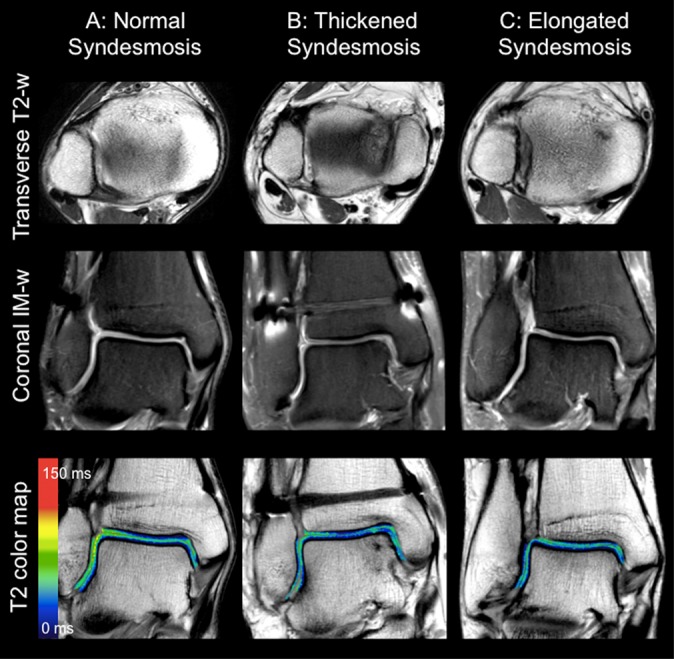
Postoperative ankle magnetic resonance (MR) images of patients who received suture-button fixation of acute, isolated syndesmosis injuries. Left column: Patient A with a normal-appearing syndesmosis. Middle column: Patient B with a thickened anterior syndesmosis relative to the contralateral ankle. Right column: Patient C with an elongated anterior syndesmosis relative to the contralateral ankle. Transverse T2-weighted (T2-w) (first row), coronal intermediate-weighted (IM-w) (second row), and color-coded T2 relaxation time maps overlayed on the first echo image of the multislice multiecho sequence (third row) are presented for each patient. Red color indicates high cartilage T2 relaxation times; blue color indicates low cartilage T2 relaxation times. T2 relaxation times and degenerative changes of the ankle were not significantly increased in ipsilateral ankles compared with contralateral ankles, and T2 relaxation times were not significantly increased in patients with thickened or elongated syndesmoses.
MR Image Analysis
MR images of both ankles were transferred on Picture Archiving Communication System (PACS) workstations (Easy Vision; Philips). MR images were assessed semiquantitatively by 1 musculoskeletal radiologist (P.M.J.). The Ankle Osteoarthritis Scoring System (AOSS)20 was used to quantify degenerative changes of the ankle. This score contains 5 major criteria (depth of cartilage damage, defect of the subchondral bone, osteophytes, subchondral cysts, bone marrow edema) and 5 minor criteria (anterolateral or anteromedial meniscoid, effusion, loose joint bodies, synovitis). The major criteria are evaluated with up to 3 (0-3) points and the minor criteria with up to 1 (0-1) point. The range of the total score is from 0 to 20 points (0 indicating the healthiest score). The syndesmotic ligaments, including the anterior inferior tibiofibular ligament (AITFL), the posterior inferior tibiofibular ligament (PITFL), and the interosseous tibiofibular ligament (ITFL) were graded as follows: unaffected (grade 0), hyperintense signal alterations on T2-weighted images (grade 1), partial tear (grade 2, partial discontinuity but preserved remnant fibers), and complete tear (grade 3, complete discontinuity of the ligament).10 Widening of the syndesmosis was measured separately for the anterior width of syndesmosis and the posterior width of syndesmosis on transverse T2-weighted images.4 Malreduction of the syndesmosis was defined as a 2-mm difference in the width of the syndesmosis, separately for anterior and posterior syndesmosis, compared with the untreated contralateral ankle. Calcification of the syndesmosis was documented as present or absent. T2 relaxation time maps were calculated pixelwise from MSME spin-echo images using a monoexponential nonnegative least-squares-fit analysis provided by the manufacturer. For T2 relaxation time measurements, segmentation of tibial, talar, and fibular cartilage compartments was performed by 1 observer (G.F.) by manually drawing regions of interest on all slices using OsiriX Lite v.7.0.2 software (Pixmeo SARL).
Statistical Analysis
Statistical analysis was performed using SPSS version 17.0 (IBM Corp). The distribution of data was tested by plotting graphs and was shown to be nonnormal for outcome scores and syndesmosis width and normal for T2 values. Outcomes scores and widths of syndesmosis were compared with the contralateral ankle using the Wilcoxon test. T2 values were compared using the Student t test. Correlations between clinical and radiographic outcomes were determined by calculating the Spearman coefficient (rho). A P value <.05 was considered to indicate statistical significance for all tests. Because of the limited number of patients included, a formal post hoc power analysis was not appropriate, as more patients could not be included to increase power. Instead, the effect size of our study was generated directly from our sample size.
Results
Between January 2006 and June 2014, 19 (9 female, 10 male) patients met the inclusion criteria and were part of the study. No patient was lost to follow-up. Mean patient age was 29 ± 11 years at the time of surgery, and the mean follow-up time from surgery was 62 ± 31 months. The mechanism of trauma was always a hyperdorsiflexion and external rotation of the ankle. Injury occurred during noncontact sports (n = 12), direct trauma to the ankle from an opponent in a contact sport (n = 2), or as the result of a fall (n = 5). All ankles appeared to be unstable on clinical examination, with 11 cases demonstrating a torn AIFTL and the remaining 8 cases showing an additionally injured PITFL.
Clinical Outcome
The FADI score was calculated for all 19 patients, with a median of 136 (range, 78-136) out of 136 points.
Three patients refused to undergo postoperative clinical examination and MRI of the ankle because they were no longer experiencing any problems concerning pain or malfunction. Clinical examination for acute lesions of the syndesmosis was negative in all patients for the ipsilateral and uninjured ankle. The median AOFAS score was 100 points (range, 87-100).
Fifteen patients recorded excellent satisfaction, while 2 reported good, 1 reported fair, and 1 patient reported poor satisfaction. This patient was suffering from recurrent pain and instability of the ankle. Therefore, the tibiofibular joint was restabilized with a temporary syndesmotic screw in an external hospital 2 years after the index operation. Nine patients suffered from skin irritation because of the prominence of the suture button, especially while wearing hiking or skating boots. Five of these patients (2 external, 3 in our department) required removal of the suture-button device. Besides the hardware removal and 1 patient being retreated with a second operation, there were no reported complications related to the surgical procedure. Seventeen of 19 patients (89%) returned to their preinjury level of sports.
Eight patients participated in competitive contact sports, of whom 7 returned to the initial level. Nine patients performed ball sports at the recreational level, of whom 8 returned to the initial level. Two patients did not participate in any type of sports. Mean time to resumption of sports was 3 months.
Mean dorsiflexion ROM in the ipsilateral and contralateral ankle was 17°. Mean ipsilateral and contralateral plantarflexion was 37°. Mean ipsilateral and contralateral supination was 17° and 18°, respectively. Mean ipsilateral and contralateral pronation was 29° and 30°, respectively.
MRI Results
Mean ± SD cartilage T2 relaxation times of the ipsilateral (talus, 30.6 ± 2.1 ms; fibula, 35.0 ± 6.4 ms; tibia, 34.0 ± 3.4 ms) and contralateral (talus, 31.3 ± 2.3 ms; fibula, 34.0 ± 5.6 ms; tibia, 33.7 ± 1.8 ms) ankle did not differ significantly (talus, P = .17; tibia, P = .68; fibula, P = .69). The mean widths of the anterior and posterior syndesmoses for the ipsilateral ankle were 3.2 ± 1.2 mm and 4.4 ± 0.9 mm, respectively, and did not show significant difference compared with the contralateral ankle (3.0 ± 0.6 mm and 4.2 ± 0.7 mm, respectively; anterior, P = .81; posterior, P = .59) (Figure 2). Malreduction of the syndesmosis was found in 2 cases (patients 9 and 15) with a difference of 2.7 mm (2.5 − 5.2) in the width of the AITFL and a difference of 3 mm (3.2 − 6.2) in the width of the PIFTL from the involved to the uninjured ankle, respectively (Figure 2). MRI showed minor morphological osteoarthritic changes of the ipsilateral ankle in 10 patients and of the contralateral ankle in 3 patients. Median AOSS score was 1.5 (range, 0-11) for the ipsilateral ankle and 0 (range, 0-6) for the contralateral ankle (P = .014). The main morphological findings, which caused the greater AOSS score in the ipsilateral ankle, were osteophytes in 6 and signal alterations in the articular cartilage in 5 patients. Calcification of the syndesmosis was present for the ipsilateral ankle in 6 patients; no patient showed calcification of the syndesmosis for the contralateral ankle. The AITFL and PITFL showed a normal signal on MRI in 3 and 11 patients, respectively, and were signal-altered (thickened) in 13 and 5 patients, respectively. Despite 2 patients with malreduction of the AIFTL/PIFTL, there were no clear correlations between patients with thickening and/or calcification of syndesmotic ligaments or widening of the anterior and/or posterior syndesmosis and osteoarthritic changes to the ankle joint. None of the syndesmotic ligaments in the ipsilateral and contralateral ankles were completely or partially ruptured. Morphological analysis of the contralateral ankle showed a thickened anterior and posterior syndesmosis in 1 patient, a signal alteration in the tibial cartilage in 1 patient, and talar bone marrow edema in 1 patient. None of the syndesmotic ligaments of the uninjured ankle showed a malreduction (widening >5 mm).
Figure 2.
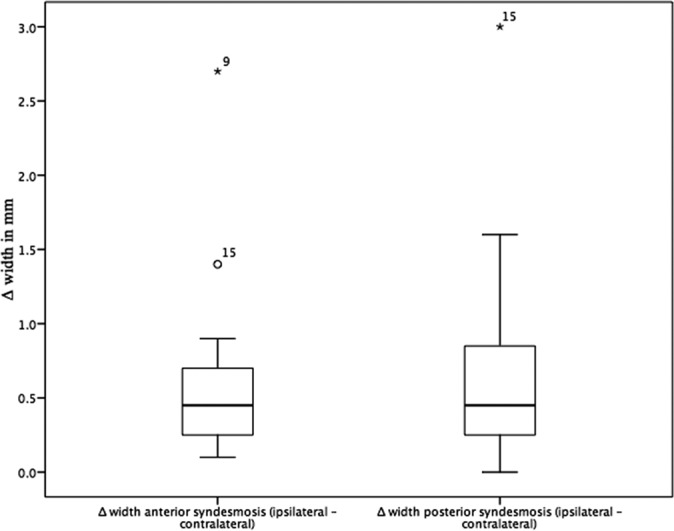
Change in width of the syndesmosis (ipsilateral – contralateral) in millimeters. Two patients (9 and 15) differed strongly from the mean, presenting a change in width of the anterior syndesmosis of 1.4 (patient 15) and 2.7 mm (patient 9). Additionally, patient 15 presented a 3-mm change in width of the posterior syndesmosis.
Correlation of MRI and Clinical Outcome
Despite a significant correlation between T2 relaxation times of the ipsilateral fibula with the FADI and AOFAS scores, there was no statistically significant correlation found between global T2 relaxation times and clinical scores (Table 1). In addition, AOSS scores did not show a significant correlation with clinical scores. Global differences in width of the anterior and posterior syndesmosis did not correlate with clinical scores (Table 1). Mean ± SD T2 values of the entire ankle joint in patients with thickened syndesmotic ligaments (33.2 ± 5.3 ms) did not show a significant difference (P = .44) compared with patients who showed normal syndesmotic ligaments (34.8 ± 4.1 ms) on MRI.
TABLE 1.
Correlations of Clinical Scores (AOFAS, FADI) With T2 Values, Width of Syndesmosis, and AOSS of the Ipsilateral Anklea
| T2 Values | Width of Syndesmosis | |||||
|---|---|---|---|---|---|---|
| Talus | Tibia | Fibula | Anterior | Posterior | AOSS | |
| AOFAS | ||||||
| Spearman correlation coefficient (R) | 0.14 | 0.19 | 0.56 | 0.32 | 0.29 | 0.10 |
| P value | .58 | .49 | .02 | .76 | .12 | .70 |
| FADI | ||||||
| Spearman correlation coefficient (R) | 0.27 | 0.47 | 0.60 | 0.40 | 0.11 | 0.13 |
| P value | .31 | .07 | .02 | .57 | .81 | .64 |
aAOFAS, American Orthopaedic Foot and Ankle Society; AOSS, Ankle Osteoarthritis Scoring System; FADI, Foot and Ankle Disability Index.
Discussion
This study showed reliable clinical results (FADI, AOFAS) after treatment with the suture-button system for acute and isolated syndesmotic injuries; moreover, no relevant difference in quantitative MRI could be detected compared with the unaffected ankle.
As the suture-button fixation system for syndesmotic lesions has been widely used over the past few years, there have been a number of studies reporting good clinical and radiological short-term results.5,7,17,18,25,28
Naqvi et al15 performed a randomized controlled trial to assess the reduction of syndesmosis after suture-button fixations with a short-term follow-up of 2.5 years. In contrast to our study, they measured the widening of the syndesmosis with single-sliced computed tomography scans compared with the uninjured ankle and did not report any cartilage condition. In total, none of the 23 assessed patients showed malreduction. However, according to our criterion, we detected 2 cases of malreduction in a 42-year-old female and a 20-year-old male at the time of surgery. The first patient showed a difference between the width of the ipsilateral (5.2 mm) and the contralateral (2.5 mm) anterior syndesmosis of 2.7 mm, whereas the second patient showed a difference between the width of the ipsilateral (3.2 mm) and the contralateral (6.2 mm) posterior syndesmosis of 3 mm. Regarding the clinical outcome, these patients showed mean AOFAS and FADI scores of 90 and 89 points and 129 and 109 points, respectively. Adequate reduction of the anterior and posterior syndesmosis was found in the remaining patients.
Degroot et al7 reported good to excellent clinical outcomes with a mean AOFAS score of 94.2 points after a mean follow-up of 20 months in 24 patients. All patients suffered from concomitant fractures and received additional surgical treatment.
In 2012, Schepers19 systematically reviewed the current literature about suture-button fixation and concluded a mean AOFAS score of 89 points. However, with a median AOFAS score of 100 points, our results are better. An explanation could be that our study group included young active patients with a mean age of 29.7 years who did not suffer from concomitant lesions and were therefore treated with isolated suture-button fixation of the tibiofibular joint. Thus, the severity and complexity of trauma mentioned by Schepers19 may result in a lower clinical score.
The most important factor for clinical outcomes in the treatment of syndesmotic ankle sprains is the accuracy of reduction of the distal tibiofibular clear space.14 In 2011, Teramoto et al23 evaluated whether the suture-button system provides adequate fixation for syndesmosis injuries. Exerting anterior, posterior, and external rotation forces to 6 normal fresh-frozen cadaver legs and subsequently measuring the diastasis of syndesmosis, they indicated that the suture-button system did not provide multidirectional stabilization for syndesmosis injuries. However, it was unclear whether the rotational forces used in this study were physiologic. This is not in line with the findings of Wang et al,29 Klitzman et al,12 and Soin et al,21 who found an adequate stabilization of the syndesmosis after suture-button fixation in similar biomechanical studies. Our clinical as well as radiological results support these findings as we present mostly excellent patient satisfaction and a high return-to-sport rate.
Until now, the longest reported follow-up (2.5 years) of patients treated with the suture-button fixation system was described in 2012, with a mean AOFAS score of 89.6 points.15 With a mean follow-up of more than 5 years, these midterm results represent the longest evaluation of the suture-button system for syndesmotic ankle sprains. The suture-button device had to be removed in 5 patients because of pain and skin irritation, mostly while undertaking sporting activities in tight shoes (eg, hockey, climbing). This percentage of implant removal (26%) is slightly higher compared with previous studies (0%-25%)7,18,22 and may be caused by the long follow-up period, the high population of competitive athletes, and the type of sports in the present study.
As osteoarthritic changes and quality of articular cartilage of the ankle may predict the clinical long-term outcome, it is important to determine these parameters in MRI imaging in relation to the uninjured ankle. Therefore, we calculated the AOSS score and additionally evaluated T2 values of articular cartilage of both ankles. A slightly higher mean AOSS score was found in the injured ankle, which represents minimal osteoarthritic changes to the ankle. These osteoarthritic changes may be explained by the initial trauma, which influences the entire ankle joint. Additionally, we cannot rule out that the scar tissue around the former syndesmosis is not as stable as the original syndesmosis, resulting in micromovements that could potentially lead to the observed findings. In general, once these changes have occurred, they are difficult to reverse. As we did not detect a negative correlation with the clinical findings in patients with a higher AOSS score, we believe that these changes are too small to indicate clinical relevance at this time. Further investigations of these patients are needed to assess the clinical outcome. T2 values of the ipsilateral and uninvolved ankle did not show significant differences. This may indicate a comparable ultrastructure of cartilage in both ankles. Cartilage T2 relaxation time measurements at the knee have been shown to correlate with cartilage matrix degeneration, predict morphological cartilage loss, and are often used for quantitative evaluation of articular cartilage repair techniques.2,8,13,30 However, a clear correlation between T2-weighted mapping and clinical outcome after cartilage repair is still lacking.6 Moreover, in our study, global T2 values of the injured ankle did not correlate with the clinical scores.
This study has a number of limitations. Clinical scores and MRI were obtained at 1 time point. Therefore, a longitudinal comparison could not be made. Clinical examination and MRI were not available for 3 patients because they were no longer experiencing problems and were unwilling to return for further testing. The median FADI score in this group was 136, which is identical to the results from the remaining patients (median FADI, 136) who were additionally evaluated with the AOFAS score. The small number of patients is due to the specific inclusion criteria. Despite these limitations, a strength of this study is the comparison with the uninjured ankle on MRI and the homogenous study group who were treated using the suture-button fixation system.17
Conclusion
Suture-button fixation is an excellent treatment for acute and isolated syndesmosis injuries, resulting in stable ankles without early or advanced osteoarthritic changes at midterm follow-up.
Acknowledgment
The authors acknowledge the German Research Foundation (DFG) and the Technical University of Munich for their support through the Open Access Publishing funding program.
Appendix
Magnetic Resonance Pulse Sequence Parametersa
| Sequence | 2D IM-w TSE | 2D T1-w TSE | 2D IM-w TSE a | 2D T2-w TSE a | MSME SE T2 a | 3D T1-w GE |
|---|---|---|---|---|---|---|
| Additional features | fs, BLADE | DRIVE pulse | fs, BLADE | |||
| Plane | Coronal | Coronal | Sagittal | Transverse | Coronal | Transverse |
| Echo time, ms | 40 | 20 | 40 | 80 | 20, 30, 40, 50, 60, 70 | 1,8 |
| Repetition time, ms | 3000 | 667 | 2500 | 4341 | 2200 | 5 |
| Field of view, mm | 140 | 140 | 140 | 140 | 100 | 100 |
| Slice thickness, mm | 3 | 3 | 3 | 3 | 2.8 | 0.7 |
| In-plane resolution, mm2 | 0.4 × 0.5 | 0.3 × 0.38 | 0.4 × 0.5 | 0.28 × 0.27 | 0.3 × 0.3 | 0.5x0.5 |
| Flip angle, deg | 90 | 90 | 90 | 90 | 90 | 5 |
| Number of slices | 23 | 23 | 23 | 31 | 17 | 71 |
| Receiver bandwidth, Hz/pixel | 232 | 241 | 201 | 249 | 232 | 479 |
| Distance, mm | 3.3 | 3.3 | 3.3 | 3.3 | 3.1 | 0.7 |
| Acquisition time, min | 04:54 | 04:30 | 04:45 | 04:47 | 12:19 | 02:20 |
aBLADE, motion correction with radial blade; fs, fat-saturated; IM, intermediate; MSME SE, multislice multiecho spin-echo; TSE, turbo spin echo; w, weighted.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: A.B.I., K.B., and S.B. are consultants for Arthrex.
Ethical approval for this study was obtained from the Technical University of Munich (number: 326/15s).
References
- 1. Alonso A, Khoury L, Adams R. Clinical tests for ankle syndesmosis injury: reliability and prediction of return to function. J Orthop Sports Phys Ther. 1998;27:276–284. [DOI] [PubMed] [Google Scholar]
- 2. Baum T, Joseph GB, Karampinos DC, Jungmann PM, Link TM, Bauer JS. Cartilage and meniscal T2 relaxation time as non-invasive biomarker for knee osteoarthritis and cartilage repair procedures. Osteoarthritis Cartilage. 2013;21:1474–1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bell DP, Wong MK. Syndesmotic screw fixation in Weber C ankle injuries—should the screw be removed before weight bearing? Injury. 2006;37:891–898. [DOI] [PubMed] [Google Scholar]
- 4. Clanton TO, Ho CP, Williams BT, et al. Magnetic resonance imaging characterization of individual ankle syndesmosis structures in asymptomatic and surgically treated cohorts. Knee Surg Sports Traumatol Arthrosc. 2016;24:2089–2102. [DOI] [PubMed] [Google Scholar]
- 5. Cottom JM, Hyer CF, Philbin TM, Berlet GC. Treatment of syndesmotic disruptions with the Arthrex Tightrope: a report of 25 cases. Foot Ankle Int. 2008;29:773–780. [DOI] [PubMed] [Google Scholar]
- 6. de Windt TS, Welsch GH, Brittberg M, et al. Is magnetic resonance imaging reliable in predicting clinical outcome after articular cartilage repair of the knee? A systematic review and meta-analysis. Am J Sports Med. 2013;41:1695–1702. [DOI] [PubMed] [Google Scholar]
- 7. Degroot H, Al-Omari AA, El Ghazaly SA. Outcomes of suture button repair of the distal tibiofibular syndesmosis. Foot Ankle Int. 2011;32:250–256. [DOI] [PubMed] [Google Scholar]
- 8. Domayer SE, Apprich S, Stelzeneder D, et al. Cartilage repair of the ankle: first results of T2 mapping at 7.0 T after microfracture and matrix associated autologous cartilage transplantation. Osteoarthritis Cartilage. 2012;20:829–836. [DOI] [PubMed] [Google Scholar]
- 9. Flint JH, Wade AM, Giuliani J, Rue JP. Defining the terms acute and chronic in orthopaedic sports injuries: a systematic review. Am J Sports Med. 2014;42:235–241. [DOI] [PubMed] [Google Scholar]
- 10. Grossterlinden LG, Hartel M, Yamamura J, et al. Isolated syndesmotic injuries in acute ankle sprains: diagnostic significance of clinical examination and MRI. Knee Surg Sports Traumatol Arthrosc. 2016;24:1180–1186. [DOI] [PubMed] [Google Scholar]
- 11. Hunt KJ. Syndesmosis injuries. Curr Rev Musculoskelet Med. 2013;6:304–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Klitzman R, Zhao H, Zhang LQ, Strohmeyer G, Vora A. Suture-button versus screw fixation of the syndesmosis: a biomechanical analysis. Foot Ankle Int. 2010;31:69–75. [DOI] [PubMed] [Google Scholar]
- 13. Kubosch EJ, Erdle B, Izadpanah K, et al. Clinical outcome and T2 assessment following autologous matrix-induced chondrogenesis in osteochondral lesions of the talus. Int Orthop. 2016;40:65–71. [DOI] [PubMed] [Google Scholar]
- 14. Miller RS, Weinhold PS, Dahners LE. Comparison of tricortical screw fixation versus a modified suture construct for fixation of ankle syndesmosis injury: a biomechanical study. J Orthop Trauma. 1999;13:39–42. [DOI] [PubMed] [Google Scholar]
- 15. Naqvi GA, Cunningham P, Lynch B, Galvin R, Awan N. Fixation of ankle syndesmotic injuries: comparison of tightrope fixation and syndesmotic screw fixation for accuracy of syndesmotic reduction. Am J Sports Med. 2012;40:2828–2835. [DOI] [PubMed] [Google Scholar]
- 16. Nauck T, Lohrer H. Translation, cross-cultural adaption and validation of the German version of the Foot and Ankle Ability Measure for patients with chronic ankle instability. Br J Sports Med. 2011;45:785–790. [DOI] [PubMed] [Google Scholar]
- 17. Peterson KS, Chapman WD, Hyer CF, Berlet GC. Maintenance of reduction with suture button fixation devices for ankle syndesmosis repair. Foot Ankle Int. 2015;36:679–684. [DOI] [PubMed] [Google Scholar]
- 18. Rigby RB, Cottom JM. Does the Arthrex TightRope® provide maintenance of the distal tibiofibular syndesmosis? A 2-year follow-up of 64 TightRopes® in 37 patients. J Foot Ankle Surg. 2013;52:563–567. [DOI] [PubMed] [Google Scholar]
- 19. Schepers T. Acute distal tibiofibular syndesmosis injury: a systematic review of suture-button versus syndesmotic screw repair. Int Orthop. 2012;36:1199–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Schmal H, Henkelmann R, Mehlhorn AT, et al. Synovial cytokine expression in ankle osteoarthritis depends on age and stage. Knee Surg Sports Traumatol Arthrosc. 2015;23:1359–1367. [DOI] [PubMed] [Google Scholar]
- 21. Soin SP, Knight TA, Dinah AF, Mears SC, Swierstra BA, Belkoff SM. Suture-button versus screw fixation in a syndesmosis rupture model: a biomechanical comparison. Foot Ankle Int. 2009;30:346–352. [DOI] [PubMed] [Google Scholar]
- 22. Storey P, Gadd RJ, Blundell C, Davies MB. Complications of suture button ankle syndesmosis stabilization with modifications of surgical technique. Foot Ankle Int. 2012;33:717–721. [DOI] [PubMed] [Google Scholar]
- 23. Teramoto A, Suzuki D, Kamiya T, Chikenji T, Watanabe K, Yamashita T. Comparison of different fixation methods of the suture-button implant for tibiofibular syndesmosis injuries. Am J Sports Med. 2011;39:2226–2232. [DOI] [PubMed] [Google Scholar]
- 24. Thornes B. Ankle syndesmosis injuries treated with the TightRope suture-button kit. Tech Foot Ankle Surg. 2006;5:45–53. [Google Scholar]
- 25. Thornes B, Shannon F, Guiney AM, Hession P, Masterson E. Suture-button syndesmosis fixation: accelerated rehabilitation and improved outcomes. Clin Orthop Relat Res. 2005;431:207–212. [PubMed] [Google Scholar]
- 26. van Dijk CN, Longo UG, Loppini M, et al. Classification and diagnosis of acute isolated syndesmotic injuries: ESSKA-AFAS consensus and guidelines. Knee Surg Sports Traumatol Arthrosc. 2016;24:1200–1216. [DOI] [PubMed] [Google Scholar]
- 27. van Dijk CN, Longo UG, Loppini M, et al. Conservative and surgical management of acute isolated syndesmotic injuries: ESSKA-AFAS consensus and guidelines. Knee Surg Sports Traumatol Arthrosc. 2016;24:1217–1227. [DOI] [PubMed] [Google Scholar]
- 28. Wang C, Ma X, Wang X, Huang J, Zhang C, Chen L. Internal fixation of distal tibiofibular syndesmotic injuries: a systematic review with meta-analysis. Int Orthop. 2013;37:1755–1763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wang L, Wang B, Xu G, Song Z, Cui H, Zhang Y. Biomechanical comparison of bionic, screw and Endobutton fixation in the treatment of tibiofibular syndesmosis injuries. Int Orthop. 2016;40:307–314. [DOI] [PubMed] [Google Scholar]
- 30. Welsch GH, Mamisch TC, Domayer SE, et al. Cartilage T2 assessment at 3-T MR imaging: in vivo differentiation of normal hyaline cartilage from reparative tissue after two cartilage repair procedures—initial experience. Radiology. 2008;247:154–161. [DOI] [PubMed] [Google Scholar]


