Abstract
Inhalation of molecular hydrogen (H2) gas ameliorates oxidative stress-induced acute injuries in the brain. Consumption of water nearly saturated with H2 also prevents chronic neurodegenerative diseases including Parkinson’s disease in animal and clinical studies. However, the molecular mechanisms underlying the remarkable effect of a small amount of H2 remain unclear. Here, we investigated the effect of H2 on mitochondria in cultured human neuroblastoma SH-SY5Y cells. H2 increased the mitochondrial membrane potential and the cellular ATP level, which were accompanied by a decrease in the reduced glutathione level and an increase in the superoxide level. Pretreatment with H2 suppressed H2O2-induced cell death, whereas post-treatment did not. Increases in the expression of anti-oxidative enzymes underlying the Nrf2 pathway in H2-treated cells indicated that mild stress caused by H2 induced increased resistance to exacerbated oxidative stress. We propose that H2 functions both as a radical scavenger and a mitohormetic effector against oxidative stress in cells.
Introduction
Administration of molecular hydrogen (H2) has the potential to improve many diseases such as ischemic brain and heart infarctions, glaucoma, stress-induced cognitive decline, Parkinson’s disease, metabolic syndrome, and inflammatory diseases [1–3]. As a weak reductant, H2 rapidly diffuses into every tissue and cell and selectively scavenges highly toxic reactive oxygen species (ROS) including the hydroxyl radical (·OH) and peroxynitrite [4]. H2 can be administered or taken into the body by numerous routes. These are roughly classified into three types: inhalation of H2 gas, drinking of H2-dissolved water (HW), and injection of H2-dissolved saline. Administration of H2 varies depending on the disease. However, when HW is orally administrated, the amount of H2 is too small to detoxify a huge amount of ROS in the diseased tissue. The molecular mechanisms underlying the remarkable effects of a small amount of H2 remain unclear.
Several lines of evidence indicate that ·OH generated by ionizing irradiation of water reacts directly with H2. We also confirmed that the dissolved H2 reduces ·OH produced by the Fenton reaction, ultraviolet irradiation, or sonication in vitro, as judged by the fluorescence of 3'-p-(hydroxyphenyl) fluorescein and the electron spin resonance spectrum of 5,5-dimethyl-1-pyrroline N-oxide [4–6]. The reduction of ·OH by H2 was further observed in cultured cells, male germ cells in mouse, and retinas in rat [4, 7, 8]. These observations indicate that a sufficient amount of H2 can efficiently moderate oxidative damage induced by ·OH. On the other hand, H2 indirectly reduces oxidative stress by inducing anti-oxidation systems in vivo. Treatment with H2 induces hemeoxygenase-1 (HO-1), superoxide dismutase (SOD), and catalase, and reduces cyclooxygenase-2 and endothelin-1 (ET-1) expression [9–12]. In Nrf2-deficient mice, the therapeutic effects of inhaling H2 gas on hyperoxic lung injury decline with decreasing expression of HO-1 [13], indicating that activation of Nrf2 is involved in the biological pathways underlying the effects of H2.
In the current study, we investigated the effect of H2 on mitochondria in cultured neuroblastoma SH-SY5Y cells and found that H2 increased the mitochondrial membrane potential (ΔΨm) and cellular ATP level, with an accompanying decrease in the reduced glutathione (GSH) level. Pretreatment of cells with H2 suppressed H2O2-induced oxidative stress, whereas post-treatment did not. These results raise the possibility that H2 functions differentially as an inducer of an adaptive response and as a radical scavenger in cells.
Methods
Cell culture and H2 treatment
Human neuroblastoma SH-SY5Y cells (ATCC CRL-2266) were maintained in Dulbecco’s modified eagle medium (DMEM) containing 10% fetal bovine serum (FBS), 25 mM HEPES, 1 mM pyruvate, penicillin-streptomycin, and 10 mM glucose (Glc) or galactose (Gal). Culture with Gal as the sole source of sugar forces mammalian cells to rely on mitochondrial oxidative phosphorylation (OXPHOS) [14].
H2-mixed gas was composed of 10% O2, 5% CO2, 35% N2, and 50% H2 (purity > 99.999%; Iwatani, Tokyo, Japan). N2-mixed gas was composed of 10% O2, 5% CO2, and 85% N2. Cells grown on culture dishes (5 × 104/cm2) for 1 day in a 5% CO2 incubator were set in acrylamide boxes (6.8 × 103/cm3), which were strewn with wet paper to prevent desiccation. The boxes were sealed and filled with an appropriate mixed gas at a flow rate of 1 L/min for 30 min under normal pressure (Fig 1A). After filling, cells in the boxes were incubated at 37°C for the indicated duration. Immediately after incubation, the H2 and O2 concentrations in the culture medium were monitored with specific electrodes (Unisense, Aarhus N, Denmark). Under H2-mixed gas, the H2 concentration was maintained at 390±40 μM. Under both H2- and N2-mixed gases, the O2 concentration was maintained at 120±10 μM (Fig 1B).
Fig 1. Cell culture system under an atmosphere containing H2 gas.
(A) Schematic representation of the culture system. 1. Pressure-reducing regulator. 2. Pressure gauge. 3. Flowmeter with flow control valve. 4. Three-way plug valve. 5. Multi-gas controller. 6. Bubbler bottle. 7. Gate valve. 8: Acrylamide box. 9. Culture dish. 10. H2 electrode. 11. O2 electrode. Note that, to avoid sudden ignition, H2- and O2-containing gases were mixed in a bubbler bottle with water. (B) H2 and O2 concentrations in culture medium were monitored with specific electrodes. Under H2-mixed gas, the H2 concentration was maintained at 390±40 μM. Under both H2- and N2-mixed gases, the O2 concentration was maintained at 120±10 μM.
Cell survival assay
Cells (5 × 104/cm2) grown in a 24- or 96-well plate for 1 day were used. For pretreatment with mixed gases, cells were incubated in a box containing an appropriate mixed gas for the indicated duration. Immediately after exposure to the mixed gas, the culture medium was replaced with DMEM containing 1% FBS with/without H2O2 and cells were further incubated in a conventional 5% CO2 incubator for 18 h. For post-treatment with mixed gases, the culture medium was replaced with DMEM containing 1% FBS with/without H2O2 and cells were further incubated in a box filled with an appropriate mixed gas for 18 h. After incubation, cell viability was estimated by a modified 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrasodium bromide viability assay according to the manufacturer’s instructions (WST-1 assay, DOJINDO, Kumamoto, Japan) or a two-color fluorescence cell viability assay (LIVE/DEAD Viability/Cytotoxicity assay, Thermo Fisher, Waltham, MA, USA), which is based on the simultaneous determination of intracellular esterase activity and plasma membrane integrity.
Evaluation of mitochondrial membrane potential
To monitor (ΔΨm, JC-1 dye (Thermo Fisher) was used. After incubation in a box containing an appropriate mixed gas, cells in a 24-well plate were stained with 20 μM JC-1 for 10 min and then evaluated by confocal microscopy. Red aggregates and green monomers were recorded with excitation (Ex) at 535 nm/emission (Em) at 590 nm and Ex at 485 nm/Em at 535 nm, respectively. Relative (ΔΨm was analyzed using Image J software (Version 1.44, NIH, Bethesda, MD, USA). Data are shown as the arbitrary aggregate fluorescence units in three separate experiments.
Oxygen consumption rate
The oxygen consumption rate in state 3 was determined at 37°C using high-resolution respirometry (Oroboros Oxygraph-2k, Innsbruck, Austria), essentially according to the protocol provided by the manufacturer. The resting respiration rate (state 2, the absence of adenylates) was measured following the transfer of 5 × 106 cells to glass chambers in 2 ml of mitochondrial respiration medium (0.5 mM EGTA, 3 mM MgCl2, 60 mM K-lactobionate, 20 mM taurine, 10 mM KH2PO4, 20 mM HEPES, 110 mM sucrose, and 1 g/l bovine serum albumin, pH 7.1). After measurement of endogenous respiration, 5 mM pyruvate, 10 mM glutamate, and 2 mM malate were added, and cells were permeabilized with 50 μg of digitonin. Complex I respiration was specifically assessed through the further addition of 1 mM ADP, followed by titration of 10 mM succinate as the complex II substrate to measure complex I and II respiration.
ATP production
Cellular ATP in each 96-well culture plate was extracted and reacted with luciferin-luciferase according to the manufacturer’s instructions (Cellular ATP Measurement System, TOYO INK, Tokyo, Japan). Bioluminescence was measured with a microplate luminometer (Envision, PerkinElmer, MA, USA).
Cellular oxidative stress
To monitor the accumulation of mitochondrial thiol, after incubation in a box containing an appropriate mixed gas, cells in a 24-well plate were stained with 1 μM MitoTracker Red (MTR, Thermo Fisher) for 10 min, fixed with 4% paraformaldehyde, washed twice with phosphate-buffered saline, and then evaluated by confocal microscopy with Ex at 535 nm/Em at 590 nm. Cells were imaged and analyzed using Image J software. Data are shown as the arbitrary fluorescence units in three separate experiments.
Total glutathione and oxidized glutathione (GSSG) were measured using a luminescence-based system (GSH/GSSG-Glo Assay, Promega, Madison, WI, USA). Cells were washed with Hank’s Balanced Salt Solution and lysed with lysis regents. The GSH/GSSG ratio was calculated directly from luminescence measurements (in relative light units, RLU) using the following formula: GSH/GSSG ratio = (total glutathione RLU—GSSG RLU) / (GSSG RLU/2).
To monitor mitochondrial superoxide and cellular ROS, cells were incubated with 5 μM MitoSOX Red (Thermo Fisher) and 1 μM 5-(and-6)-chloromethyl-2′,7′-dichlorodihydrofluorescein diacetate, acetyl ester (Thermo Fisher) prepared in Hank’s Balanced Salt Solution for 10 min at 37°C, washed three times, and then scanned using a microplate fluorometer (Envision) with Ex at 510 nm/Em at 580 nm and Ex at 495 nm/Em at 520 nm, respectively.
Cell staining
Immunocytochemistry was performed as previously described [15]. Cells were fixed with 4% paraformaldehyde prepared in phosphate-buffered saline, permeabilized with 0.2% Triton X-100, and incubated with an anti-Nrf-2 rabbit polyclonal antibody (C-20, Santa Cruz, Dallas, TX, USA). After incubation with a BODIPY FL-conjugated secondary antibody (anti-rabbit IgG; Thermo Fisher), cells were visualized by confocal laser microscopy.
Measurement of mitochondrial DNA copy number
Total DNA was isolated from cells using proteinase K digestion followed by standard phenol/chloroform extraction and ethanol precipitation, and subjected to TaqMan probe-based quantitative PCR analysis using a real-time PCR system (StepOnePlus, Thermo Fisher). The primers and probes for MT-ND1 gene in the mitochondrial DNA (mtDNA) and 18S rRNA gene in the nuclear DNA (nDNA,) used are listed in Table 1. The mtDNA copy number was calculated as a ratio of mtDNA/nDNA.
Table 1. Primers and probes used for semiquantitative PCR.
| Gene | Primer/probe sequences |
|---|---|
| MT-ND1 | Forward primer: CACCCAAGAACAGGGTTTGT Reverse primer: TGGCCATGGGTATGTTGTTAA Probe: 6FAM/TTACCGGGCTCTGCCATCT/TAMRA |
| 18S rRNA | Forward primer: TAGAGGGACAAGTGGCGTTC Reverse primer: CGCTGAGCCAGTCAGTGT Probe: VIC/AGCAATAACAGGTCTGTGATG/TAMRA |
| ACTB | Forward primer: CCTTCTACAATGAGCTGCGT Reverse primer: TGGATAGCAACGTACATGGC Probe: 56-FAM/ATCTGGGTC/ZEN/ATCTTCTCGCGGTTG/3IABkFQ |
| CAT | Forward primer: GAGCACAGCATCCAATATTCTG Reverse primer: TCCTCATTCAGCACGTTCAC Probe: 56-FAM/TGCCCGCAC/ZEN/CTGAGTAACGTTATC/3IABkFQ |
| GCLC | Forward primer: CTCAGACATTGGATGGAGAGTAG Reverse primer: GAGCAGTACCACAAACACCA Probe: 56-FAM/TCGACCCAT/ZEN/GGAGGTGCAATTAACA/3IABkFQ |
| GPX1 | Forward primer: CTTCCCGTGCAACCAGTT Reverse primer: TCTCGAAGAGCATGAAGTTGG Probe: 56-FAM/TCGTTCTTG/ZEN/GCGTTCTCCTGATGC/3IABkFQ |
| GSR | Forward primer: CGATCTATOAOGCACTTACCA Reverse primer: GCATTTCATCACACCCAAGTC Probe: 56-FAM/CCAACCACC/ZEN/TTTTCTTCCTTGTTAGCAC/3IABkFQ |
| HMOX1 | Forward primer: AGGCAGAGGGTGATAGAAGAG Reverse primer: CTCTGGTCCTTGGTGTCAT Probe: 56-FAM/AGAGCTGGA/ZEN/TGTTGAGCAGGAACG/31ABkFQ |
| SOD2 | Forward primer: GCTTGGTTTCAATAAGGAACGG Reverse primer: GCTCCCACACATCAATCCC Probe: 56-FAM/CCACTGCAA/ZEN/GGAACAACAGGCC/3IABkFQ |
Semiquantitative PCR analysis of the mRNA levels of anti-oxidative enzymes
Cellular total RNA was extracted using an RNeasy Plus Mini kit (QIAGEN, Valencia, CA, USA) and subjected to reverse transcription with a first-strand synthesis system (SuperScript II, Thermo Fisher). Samples of the resulting cDNA were subjected to TaqMan probe-based quantitative PCR analysis using a real-time PCR system. The primers and probes used are listed in Table 1. Relative gene expression was calculated using the standard curve method. The mRNA levels were normalized to that of ACTB (β-actin) gene.
Western blot analysis
Cells were homogenized in RIPA buffer and centrifuged (15,000 g at 4°C for 20 min), and the supernatants were collected and stored at −80°C. Denatured proteins (10 μg in each lane) were separated on a 10% acrylamide gel and electrotransferred onto a polyvinylidene fluoride (PVDF) membrane. The PVDF membrane was blocked with skim milk and incubated at 4°C overnight with primary polyclonal rabbit antibodies against γ-glutamylcysteine synthetase heavy subunit (γ-GCSc; 1:200, H-338, Santa Cruz), heme oxygenase-1 (HO-1; 1:500, ADI-SPA-896, Enzo Life Sci., Farmingdale, NY, USA), superoxide dismutase 2 (SOD2; 1:200, FL-222, Santa Cruz) and polyclonal goat antibodies against NAD(P)H quinone oxidoreductase 1 (NQO1; 1:200, C-19, Santa Cruz), Nrf2 (1:200, T-19, Santa Cruz). After washing, membranes were incubated with peroxidase-conjugated goat anti-rabbit IgG (1:10000, Jackson ImmunoResearch, West Grove, PA, USA) or rabbit anti-goat IgG (1:10000, Jackson ImmunoResearch) at RT for 1 hour. Protein bands were detected using an enhanced chemiluminescence kit (ECL prime, GE Healthcare, Chicago, IL, USA) and visualized using an exposure and quantitation system (LAS-3000 mini, FUJI film, Tokyo, Japan). As a normalization control, the membranes were reprobed for 3-phosphate dehydrogenase (GAPDH) and exposed to polyclonal rabbit antibody against GAPDH (1:1000, Cell Signaling, Danvers, MA, USA).
Statistical analysis
All experiments were repeated two or three times with similar results (n = 4–5 per group). Statistical analysis was performed by applying a one-way ANOVA with the Bonferroni correction or the Student’s t-test. Data are presented as mean ± SD. Results were considered significant at P < 0.05. A two-way ANOVA was used to evaluate effects of pretreatment with mixed gases for different durations on cell death; a significant interaction was interpreted by a subsequent simple-effects analysis with the Student’s t-test.
Results
Protective effect of H2 pretreatment against H2O2-induced cell death
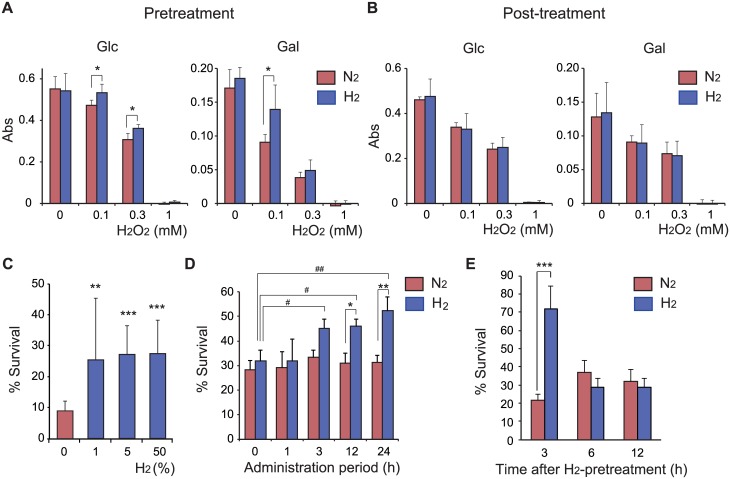
To investigate the molecular mechanisms underlying the physiological function of H2, we used human neuroblastoma SH-SY5Y cells because several lines of evidence indicate that treatment with H2 effectively protects against neuronal damage in vivo [3]. To prevent an accidental change in the O2 concentration, which would strongly affect cellular signaling and cell fate, we established a new cell culture system under strict gas control and carefully monitored the concentrations of H2 and O2 in the medium (Fig 1). SH-SY5Y cells were cultured in medium containing either Glc or Gal. Substituting Gal for Glc in cell culture media enhances mitochondrial metabolism [16]. Pretreatment of cells with 50% H2 gas for 18 h in both Glc- and Gal-containing media suppressed H2O2-induced cell death (Fig 2A), whereas post-treatment did not (Fig 2B). The protective effect of pretreatment was dose-dependent, and H2 concentrations of 1% and higher were significantly effective (Fig 2C). Pretreatment with 50% H2 for 3 h was sufficient to elicit the protective effect, whereas pretreatment for 1 h was not (Fig 2D). Cells were still protected against H2O2 toxicity at 3 h after the end of pretreatment with 50% H2, whereas after 6 h they were not (Fig 2E), indicating that the protective effects of pretreatment are transient in growing cultured cells.
Fig 2. Protective effect of H2 pretreatment against H2O2-induced cell death.
(A) For pretreatment with mixed gas, SH-SY5Y cells were incubated in culture medium containing either Glc or Gal under N2- or H2-mixed gas for 18 h. Immediately after the end of exposure to the mixed gas, the medium was replaced with fresh medium containing the indicated concentration of H2O2. Cells were further incubated in a conventional CO2 incubator for 18 h. (B) For post-treatment with mixed gases, culture medium containing either Glc or Gal was replaced with fresh medium containing the indicated concentration of H2O2. Cells were further incubated under an appropriate mixed gas. After the final incubation, cell viability was estimated by a modified 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrasodium bromide viability assay (A, B). (C) The protective effects of pretreatment with mixed gas containing different concentrations of H2 against 0.5 mM H2O2-induced cell death were examined. (D) The protective effects of pretreatment with N2- or H2-mixed gas for different durations against 0.5 mM H2O2-induced cell death were examined. Applying two-way ANOVA showed significant effects of mixed gas (P = 0.0017) and duration (P = 0.0315), however no interaction between them was observed (P = 0.2224). (E) After pretreatment with N2- or H2-mixed gas, culture medium was replaced with fresh medium, cells were incubated in a conventional CO2 incubator for the indicated duration, and then H2O2 (final 0.5mM) was added. Cells were further incubated for 18 h. All cells used in C—E were cultured in medium containing Glc. After the final incubation, cell viability was estimated by a two-color fluorescence cell viability assay and expressed as a percentage compared with cells not treated with H2O2 (considered as 100%) (C—E). *P < 0.05, **P < 0.01, ***P < 0.001 versus treatment with N2-mixed gas. #P < 0.05, ##P < 0.01 versus an administration period of 0 h.
Enhancement of mitochondrial activity by H2 treatment
We previously observed that H2 prevents the antimycin A (a mitochondrial respiratory complex III inhibitor)-dependent decline in ΔΨm [4]. We used the ΔΨm indicator JC-1 to determine the physiological changes of mitochondria in intact cells treated with 50% H2 for 18 h. H2 treatment significantly increased ΔΨm in both Glc- and Gal-containing media (Fig 3A). Furthermore, H2 treatment increased the accumulation of cellular ATP (Fig 3B), indicating that it activates OXPHOS and then enhances mitochondrial energy production. To confirm the activation of mitochondrial OXPHOS, we measured cellular O2 consumption by high-resolution respirometry. H2 treatment enhanced the O2 consumption rate in state 3 (Fig 3C). On the other hand, the mtDNA copy number relative to nuclear genes was not affected by H2 treatment (Fig 3D), indicating that the increase in oxygen consumption per cell was not due to a change in the mitochondrial copy number.
Fig 3. Enhancement of mitochondrial activities by H2 treatment.
(A) H2 treatment enhanced JC-1-indicated ΔΨm, which was expressed as the ratio of monomers to aggregates. (B) H2 treatment enhanced the accumulation of ATP, which was expressed as a percentage compared with cells not treated with mixed gases (considered as 100%). SH-SY5Y cells were incubated in culture medium containing either Glc or Gal under N2- or H2-mixed gas for 18 h. **P < 0.01, ***P < 0.001 (A, B). (C) H2 treatment enhanced the O2 consumption rate in state 3. O2 consumption was monitored with high-resolution respirometry. *P < 0.05. (D) The mtDNA copy number relative to nDNA in cells incubated under H2-mixed gas was quantified by real-time PCR analysis, and expressed relative to those in cells incubated under N2-mixed gas.
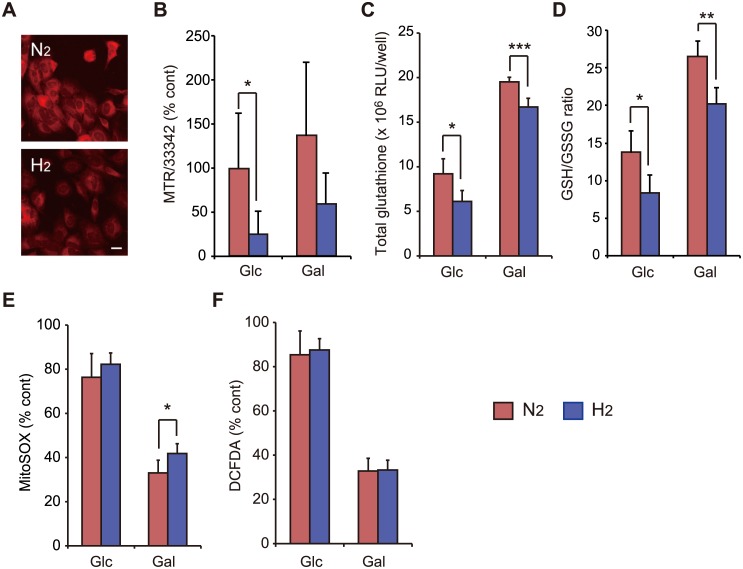
Induction of weak oxidative stress by H2 treatment
To monitor the effects of mitochondrial hyperactivity induced by H2 treatment on oxidative stress, we first used MTR. This dye contains a mildly thiol-reactive chloromethyl moiety, which keeps it associated with mitochondria after fixation [17]. H2 treatment attenuated staining with MTR, indicating that it decreased the thiol concentration in mitochondria (Fig 4A and 4B). H2 treatment decreased the total glutathione and GSH levels (Fig 4C and 4D), indicating that the decrease in the thiol concentration was at least partially dependent on that in GSH. H2 treatment significantly increased superoxide formation in cells cultured in Gal-containing medium (Fig 4E), whereas it did not increase the formation of DCFDA-indicated ROS (Fig 4F). Both the decrease in GSH and the increase in superoxide strongly suggest that H2 treatment induces oxidative stress in cells. However, H2-induced oxidative stress was too weak to affect cell survival (Fig 2A and 2B).
Fig 4. Induction of oxidative stress by H2 treatment.
SH-SY5Y cells were incubated in culture medium containing either Glc or Gal under N2- or H2-mixed gas for 18 h. (A, B) H2 treatment attenuated staining with MTR, which was expressed as a percentage compared with cells not treated with mixed gases (considered as 100%). The scale bar is 20 μm in (A). (C, D) H2 treatment decreased the total glutathione and GSH levels. (E) H2 treatment increased superoxide formation in cells cultured in Gal-containing medium, which was expressed as a percentage compared with cells not treated with mixed gases (considered as 100%). (F) H2 treatment did not increase DCFDA-indicated ROS, which was expressed as a percentage compared with cells not treated with mixed gases (considered as 100%). *P < 0.05, **P < 0.01, ***P < 0.001.
Induction of the anti-oxidative defense system by H2 treatment
Weak oxidative stress is expected to be associated with triggering of an adaptive response to stronger oxidative stress [18]. To investigate induction of the anti-oxidative system, we stained cells with an anti-Nrf2 antibody. H2 treatment induced translocation of the transcription factor Nrf2 into the nucleus (Fig 5A). We further measured the expression of anti-oxidative enzymes underlying the Nrf2 pathway by performing quantitative PCR. After H2 treatment, transcription of CAT, GPX1 and GSR genes increased significantly (Fig 5B). Western blot of cell extracts also revealed that H2 treatment resulted in an increase in HO-1, NQO1 and Nrf2 expressions (Fig 5C), indicating that weak oxidative stress induced by H2 treatment evokes an anti-oxidative defense system in SH-SY5Y cells.
Fig 5. The H2-induced anti-oxidative defense system.
(A) SH-SY5Y cells were stained with an anti-Nrf2 antibody. H2 treatment induced translocation of Nrf2 into the nucleus (arrow heads). The scale bar is 100 μm. (B) Cells were incubated in culture medium containing either Glc or Gal under N2- or H2-mixed gas for 18 h. The transcript levels of genes involved in the anti-oxidative defense system, including CAT, GCLC, GPX1, GSR, HO-1 and SOD2, were quantified by real-time PCR analysis coupled with reverse transcription of total RNA, and expressed relative to those in cells incubated under N2-mixed gas. (C) The expression levels of proteins involved in the anti-oxidative defense system, including γ-GCSc, HO-1, NQO1, Nrf2 and SOD2, were quantified by the intensity of representative immunoblots (n = 5 or 6, each), and expressed relative to those in cells incubated under N2-mixed gas. *P < 0.05, **P < 0.01. ***P < 0.001.
Discussion
Increasing evidence suggests that some natural products and synthetic drugs that improve our health may act via a characteristic process called hormesis, in which adaptive responses against cellular stress are activated [19, 20]. In the current study, we found that H2 pretreatment effectively protects against H2O2-induced neuronal damage in vitro; H2-induced slight activation of mitochondria accompanied by weak oxidative stress triggers adaptive responses against oxidative stress.
H2 selectively reduces the highly toxic ROS OH· and peroxynitrite, but not O2-·, H2O2, or nitric oxide [4]. The cellular toxicity of H2O2 is partially explained by the production of ·OH, which leads to alterations of lipids, proteins, and nucleic acids [21]. We previously observed that H2 reduces a large amount of ·OH produced by the Fenton reaction, irradiation, or sonication in vitro [4–6], strongly supporting the conclusion that a sufficient amount of H2 can efficiently moderate cellular oxidative damage induced by ·OH. However, treatment with 50% H2 gas after the addition of H2O2 (post-treatment) did not protect cells (Fig 2A and 2B). Because of the relatively low reactivity of H2 against ·OH [22], we speculate that the steady-state concentration of ·OH derived from exogenous H2O2 in the cell is too low to react with H2. On the other hand, pretreatment with H2 ameliorated H2O2-induced cell death. When H2O2 was added, no detectable amount of H2 remained in the cell (data not shown), suggesting that the pretreatment dose of H2 did not directly prevent H2O2-induced oxidative damage, but provoked an anti-oxidative defense system against H2O2 in our experiments.
The protective effect of H2 pretreatment was dose-dependent, and H2 concentrations of 1% and higher were significantly effective (Fig 2C). Inhalation of H2 gas is the simplest method to intake H2 and ameliorates acute diseases such as ischemia-reperfusion and graft injuries of several organs [1, 2]. The effective concentration of H2 in mixed gas is usually maintained between 1% and 4% [4, 23, 24]. On the other hand, drinking water saturated with H2 (1.6 ppm, saturated with 100% H2 gas) is safer and more convenient than inhaling H2 gas. After administration of HW containing a saturating amount of H2 (80%) with a feeding needle in mouse, the H2 concentration in the liver is immediately elevated, peaking at approximately 2% H2 [25]. These observations indicate that about a few percent of H2 is the physiologically active concentration in vivo.
H2 treatment significantly increased ΔΨm and the cellular ATP level, indicating that H2 treatment enhances mitochondrial energy production via activation of OXPHOS (Fig 3). This was supported by the observation that H2 treatment enhanced the O2 consumption rate. OXPHOS is regulated through respiratory control, allosteric regulation, and post-translational modifications [26]. Calcium is the strongest signal for mitochondrial activation [27]. Although the direct target molecule of H2 in physiological conditions remains to be identified, several potential effectors of H2 have been discussed, including cell signaling molecules and hormones that are responsible for preventing oxidative stress and inflammation. Recently, Iuchi et al. demonstrated that low concentrations (approximately 1%) of H2 modulate Ca2+ signal transduction [28], indicating that excessive calcium signaling enhances OXPHOS activity.
OXPHOS in a hyperactive state leads to hyperpolarization of ΔΨm, which causes the generation of excessive ROS [29]. H2 treatment attenuated staining with MTR after fixation (Fig 4A). Because the chloromethyl moiety of MTR is thiol-reactive, we speculated that H2 treatment decreases the thiol concentration in mitochondria. We then measured the intracellular concentration of GSH, which is the most abundant thiol inside the cell [30]. H2 treatment decreased the total amount of glutathione, concomitant with a lower GSH/GSSG ratio (Fig 4C and 4D). Finally, treatment with the selective reductant H2 enhanced the accumulation of the mitochondrial ROS O2-· (Fig 4E), indicating that H2 induces weak oxidative stress.
Increasing evidence indicates that transient exposure to low levels of ROS can protect neurons against subsequent exposure to a lethal level of oxidative stress [18]. The Keap1/Nrf2/ARE pathway is one of the molecular mechanisms underlying this adaptive response. Indeed, H2 treatment induced the translocation of Nrf2 into the nucleus and enhanced the transcription of CAT, GPX1 and GSR and the accumulation of HO-1, NQO1 and Nrf-2 (Fig 5). H2 pretreatment for more than 3 h was required to protect cells (Fig 2D). We speculated that exposure for 1 h was too short to induce oxidative stress sufficient to provoke an anti-oxidative defense system via transcriptional regulation.
In our experimental condition, a high dose of H2O2 was used to induce cell death, accompanied by a decrease in mitochondrial activity, which was not prevented by the post-treatment with H2 (Fig 2B). On the other hand, the post-treatment with H2 did not enhance H2O2-dependent cell death, indicating that H2-induced oxidative stress is negligible and very weaker than that induced by H2O2 during cell death. It was recently found that a low dose of H2O2 also plays a crucial role in the induction of hormesis [31], suggesting that the simultaneous treatment with H2 and a low dose of H2O2 may coordinately enhance a defense system against oxidative stress. Further studies will be required to elucidate the hormesis effect of H2 under weak oxidative stress.
With or without post-treatment with 0.3 mM H2O2 induce cell death. However, treatment with 50% H2 gas after the addition of H2O2 (post-treatment) did not protect cells (Fig 2A and 2B). Because of the relatively low reactivity of H2 against ·OH [22], we speculate that the steady-state concentration of ·OH derived from exogenous H2O2 in the cell is too low to react with H2.
After drinking of HW, hypoxia-reoxygenation-induced superoxide formation in a mouse brain slice is suppressed [32]. Noteworthy, there is no trace amount of H2 in the slice, indicating that HW induces anti-oxidation systems in the brain. We also found that preadministration of HW to mice before lipopolysaccharide injection prolongs survival and reduces oxidative stress in the liver, with increased expression of HO-1 and decreased expression of ET-1 [33].
In summary, H2 pretreatment prevented H2O2-induced cell death, enhanced mitochondrial activities, accompanied by an increased level of oxidative stress, and then induced expression of anti-oxidative enzymes. Based on H2-induced adaptive responses in vitro and in vivo, we now consider that H2 functions as a so-called mitohormetic effector against oxidative stress.
Acknowledgments
We thank Dr. Masashi Tanaka for his kind advice and Mr. Tetsuya Suzuki for technical support.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported in part by Japan Society for the Promotion of Science (JSPS) KAKENHI (https://www.jsps.go.jp/english/e-grants/) Grant Number 24500882 and 16H03267 for IO. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Ichihara M, Sobue S, Ito M, Ito M, Hirayama M, Ohno K (2015) Beneficial biological effects and the underlying mechanisms of molecular hydrogen—comprehensive review of 321 original articles. Med Gas Res 19(5):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ohta S (2015) Molecular hydrogen as a novel antioxidant: overview of the advantages of hydrogen for medical applications. Methods Enzymol 555:289–317. 10.1016/bs.mie.2014.11.038 [DOI] [PubMed] [Google Scholar]
- 3.Iketani M, Ohsawa I (2016) Molecular Hydrogen as a Neuroprotective Agent. Curr Neuropharmacol [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ohsawa I, Ishikawa M, Takahashi K, Watanabe M, Nishimaki K, Yamagata K, et al. (2007) Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat Med 13(6):688–694. 10.1038/nm1577 [DOI] [PubMed] [Google Scholar]
- 5.Terasaki Y, Ohsawa I, Terasaki M, Takahashi M, Kunugi S, Dedong K, et al. (2011) Hydrogen therapy attenuates irradiation-induced lung damage by reducing oxidative stress. Am J Physiol Lung Cell Mol Physiol 301(4):L415–426. 10.1152/ajplung.00008.2011 [DOI] [PubMed] [Google Scholar]
- 6.Igarashi T, Ohsawa I, Kobayashi M, Igarashi T, Suzuki H, Iketani M, et al. (2016) Hydrogen prevents corneal endothelial damage in phacoemulsification cataract surgery. Sci Rep 6:31190 10.1038/srep31190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chuai Y, Gao F, Li B, Zhao L, Qian L, Cao F, et al. (2012) Hydrogen-rich saline attenuates radiation-induced male germ cell loss in mice through reducing hydroxyl radicals. Biochem J 15;442(1):49–56. [DOI] [PubMed] [Google Scholar]
- 8.Oharazawa H, Igarashi T, Yokota T, Fujii H, Suzuki H, Machide M, et al. (2010) Protection of the retina by rapid diffusion of hydrogen:administration of hydrogen-loaded eye drops in retinal ischemia-reperfusion injury. Invest Ophthalmol Vis Sci 51(1):487–92. 10.1167/iovs.09-4089 [DOI] [PubMed] [Google Scholar]
- 9.Kawamura T, Huang CS, Peng X, Masutani K, Shigemura N, Billiar TR, et al. (2011) The effect of donor treatment with hydrogen on lung allograft function in rats. Surgery 150(2):240–249. 10.1016/j.surg.2011.05.019 [DOI] [PubMed] [Google Scholar]
- 10.Li J, Dong Y, Chen H, Han H, Yu Y, Wang G, et al. (2012) Protective effects of hydrogen-rich saline in a rat model of permanent focal cerebral ischemia via reducing oxidative stress and inflammatory cytokines. Brain Res 1486:103–111. 10.1016/j.brainres.2012.09.031 [DOI] [PubMed] [Google Scholar]
- 11.Hugyecz M, Mracskó E, Hertelendy P, Farkas E, Domoki F, Bari F (2011) Hydrogen supplemented air inhalation reduces changes of prooxidant enzyme and gap junction protein levels after transient global cerebral ischemia in the rat hippocampus. Brain Res 1404:31–38. 10.1016/j.brainres.2011.05.068 [DOI] [PubMed] [Google Scholar]
- 12.Shimada S, Wakayama K, Fukai M, Shimamura T, Ishikawa T, Fukumori D, et al. (2016) Hydrogen Gas Ameliorates Hepatic Reperfusion Injury After Prolonged Cold Preservation in Isolated Perfused Rat Liver. Artif Organs [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 13.Kawamura T, Wakabayashi N, Shigemura N, Huang CS, Masutani K, Tanaka Y, et al. (2013) Hydrogen gas reduces hyperoxic lung injury via the Nrf2 pathway in vivo. Am J Physiol Lung Cell Mol Physiol 304(10):L646–656. 10.1152/ajplung.00164.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robinson BH, Petrova-Benedict R, Buncic JR, Wallace DC (1992) Nonviability of cells with oxidative defects in galactose medium: a screening test for affected patient fibroblasts. Biochem Med Metab Biol. 48(2):122–126. [DOI] [PubMed] [Google Scholar]
- 15.Ohsawa I, Takamura C, Morimoto T, Ishiguro M, Kohsaka S (1999) Amino-terminal region of secreted form of amyloid precursor protein stimulates proliferation of neural stem cells. Eur J Neurosci. 11(6):1907–1913. [DOI] [PubMed] [Google Scholar]
- 16.Aguer C, Gambarotta D, Mailloux RJ, Moffat C, Dent R, McPherson R, et al. (2011) Galactose enhances oxidative metabolism and reveals mitochondrial dysfunction in human primary muscle cells. PLoS One 6(12):e28536 10.1371/journal.pone.0028536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chazotte B (2011) Labeling mitochondria with MitoTracker dyes. Cold Spring Harb Protoc 2011(8):990–992. 10.1101/pdb.prot5648 [DOI] [PubMed] [Google Scholar]
- 18.Texel SJ, Mattson MP (2010) Impaired adaptive cellular responses to oxidative stress and the pathogenesis of Alzheimer's disease. Antioxid Redox Signal 14(8):1519–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schieber M, Chandel NS (2014) ROS function in redox signaling and oxidative stress. Curr Biol 24(10):R453–462. 10.1016/j.cub.2014.03.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ristow M, Zarse K (2010) How increased oxidative stress promotes longevity and metabolic health: The concept of mitochondrial hormesis (mitohormesis). Exp Gerontol 45(6):410–418. 10.1016/j.exger.2010.03.014 [DOI] [PubMed] [Google Scholar]
- 21.Halliwell B (1987) Oxidants and human disease: some new concepts. FASEB J 1(5):358–364. [PubMed] [Google Scholar]
- 22.Ohno K, Ito M, Ichihara M, Ito M (2012) Molecular hydrogen as an emerging therapeutic medical gas for neurodegenerative and other diseases. Oxid Med Cell Longev 2012:353152 10.1155/2012/353152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yonamine R, Satoh Y, Kodama M, Araki Y, Kazama T (2013) Coadministration of hydrogen gas as part of the carrier gas mixture suppresses neuronal apoptosis and subsequent behavioral deficits caused by neonatal exposure to sevoflurane in mice. Anesthesiology 118(1):105–113. 10.1097/ALN.0b013e318275146d [DOI] [PubMed] [Google Scholar]
- 24.Hayashida K, Sano M, Kamimura N, Yokota T, Suzuki M, Ohta S, et al. (2014) Hydrogen inhalation during normoxic resuscitation improves neurological outcome in a rat model of cardiac arrest independently of targeted temperature management. Circulation 130(24):2173–2180. 10.1161/CIRCULATIONAHA.114.011848 [DOI] [PubMed] [Google Scholar]
- 25.Kamimura N, Nishimaki K, Ohsawa I, Ohta S (2011) Molecular hydrogen improves obesity and diabetes by inducing hepatic FGF21 and stimulating energy metabolism in db/db mice. Obesity (Silver Spring) 19(7):1396–1403. [DOI] [PubMed] [Google Scholar]
- 26.Hüttemann M, Helling S, Sanderson TH, Sinkler C, Samavati L, Mahapatra G, et al. (2012) Regulation of mitochondrial respiration and apoptosis through cell signaling: cytochrome c oxidase and cytochrome c in ischemia/reperfusion injury and inflammation. Biochim Biophys Acta 1817(4):598–609. 10.1016/j.bbabio.2011.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patergnani S, Suski JM, Agnoletto C, Bononi A, Bonora M, De Marchi E, et al. (2011) Calcium signaling around Mitochondria Associated Membranes (MAMs). Cell Commun Signal 9:19 10.1186/1478-811X-9-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iuchi K, Imoto A, Kamimura N, Nishimaki K, Ichimiya H, Yokota T, et al. (2016) Molecular hydrogen regulates gene expression by modifying the free radical chain reaction-dependent generation of oxidized phospholipid mediators. Sci Rep 6:18971 10.1038/srep18971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seppet E, Gruno M, Peetsalu A, Gizatullina Z, Nguyen HP, Vielhaber S, et al. (2009) Mitochondria and energetic depression in cell pathophysiology. Int J Mol Sci 10(5):2252–2303. 10.3390/ijms10052252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Circu ML, Aw TY (2008) Glutathione and apoptosis. Free Radic Res. 42(8):689–706. 10.1080/10715760802317663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ludovico P, Burhans WC (2014) Reactive oxygen species, ageing and the hormesis police. FEMS Yeast Res 14(1):33–39. 10.1111/1567-1364.12070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sato Y, Kajiyama S, Amano A, Kondo Y, Sasaki T, Handa S, et al. (2008) Hydrogen-rich pure water prevents superoxide formation in brain slices of vitamin C-depleted SMP30/GNL knockout mice. Biochem Biophys Res Commun 375(3):346–350. 10.1016/j.bbrc.2008.08.020 [DOI] [PubMed] [Google Scholar]
- 33.Iketani M, Ohshiro J, Urushibara T, Takahashi M, Arai T, Kawaguchi H, et al. (2016) Preadministration of hydrogen-rich water protects against lipopolysaccharide-induced sepsis and attenuates liver injury. Shock [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.