Abstract
Objectives:
Demand for dental care is expected to outpace supply through 2025. The objectives of this study were to determine the extent of pediatric dental care shortages in Georgia and to develop a general method for estimation that can be applied to other states.
Methods:
We estimated supply and demand for pediatric preventive dental care for the 159 counties in Georgia in 2015. We compared pediatric preventive dental care shortage areas (where demand exceeded twice the supply) designated by our methods with dental health professional shortage areas designated by the Health Resources & Services Administration. We estimated caries risk from a multivariate analysis of National Health and Nutrition Examination Survey data and national census data. We estimated county-level demand based on the time needed to perform preventive dental care services and the proportion of time that dentists spend on pediatric preventive dental care services from the Medical Expenditure Panel Survey.
Results:
Pediatric preventive dental care supply exceeded demand in Georgia in 75 counties: the average annual county-level pediatric preventive dental care demand was 16 866 hours, and the supply was 32 969 hours. We identified 41 counties as pediatric dental care shortage areas, 14 of which had not been designated by the Health Resources & Services Administration.
Conclusions:
Age- and service-specific information on dental care shortage areas could result in more efficient provider staffing and geographic targeting.
Keywords: pediatric dental care shortage areas, caries risk, national guidelines
Dental caries was named the most prevalent unmet health need among US children during 1993-1996.1 Almost 25% of US children living in poverty had untreated caries.2 Untreated dental caries can lead to problems with eating, speaking, and learning.3 Although preventive dental care (ie, pit-and-fissure sealants4 and topical fluoride5) is highly effective in preventing caries, <9% of low-income children received at least 1 of these services in 2009.6 Increasing the use of preventive dental care among low-income children is a health goal of Healthy People 2020.7
Use of dental care depends on demand and supply.8 Geographic regions that do not have sufficient supply to satisfy pediatric demand for preventive dental care are referred to as pediatric preventive dental care shortage areas (hereinafter, dental care shortage areas). Demand is influenced by the cost of services, personal income, perceived need for care, and professional guidelines for the recommended and frequency of services.8–10 The most precise estimates of dental care demand are based on specific dental procedures; such estimates provide details on quantity and delivery time.8
Dental care supply is typically measured by the number of dentists or workforce hours. Measuring supply in this way, however, may not accurately capture data on the supply of dental care to Medicaid-eligible children; many dentists do not accept Medicaid patients because of the high administrative costs and low reimbursement rates.11–13
Demand for dental care is expected to outpace supply through 2025.14 Contributing factors include population growth and increased access to dental insurance through health care reform.15–18 The Health Resources & Services Administration (HRSA) predicts that every state will face a shortage by 2025,14 suggesting that use of preventive dental care could remain low. Local strategies to increase supply include allowing dental hygienists or therapists to provide preventive services without a dentist’s supervision in public health or school settings, providing federal grants to health centers that offer dental care, increasing Medicaid reimbursements, offering federal assistance for dental school loans for dentists who locate in dental care shortage areas, and offering I-1 visas to international providers who practice in underserved areas.14
We estimated supply and demand for pediatric preventive dental care for small areas (ie, county and census tracts) using data from Georgia. We used need, as measured by recommended frequencies for receipt of preventive dental care in professional guidelines,19 as a proxy for demand. It is important to note, however, that demand depends on many factors, especially cost. Finally, we compared counties identified as dental care shortage areas by our methods with counties designated by HRSA as dental health professional shortage areas (HPSAs). Several problems have been identified with the HRSA designation methods.20 For example, some designated HPSAs no longer meet criteria for being an HPSA and yet still receive HPSA benefits. Furthermore, HRSA methods do not account for certain types of providers, such as primary care physicians.
Our approach differed from previous research in estimating dental care shortage areas15,21 in that we estimated supply and demand for specific services for a specific population. We believe that our study is the first to estimate county-level demand and supply for preventive dental care hours. These estimates are sufficiently precise to determine where to locate community programs and implement policies to increase the use of preventive dental care among high-need children. Although we piloted our approach for children in Georgia, the proposed methods can be applied to other states and age groups.
Methods
We estimated caries risk for 2.5 million Georgia children aged 0-18 in 2010 using logistic regression analysis. We estimated pediatric preventive dental care demand based on the time needed to provide recommended dental procedures. We estimated pediatric preventive dental care supply based on the location of providers and the time available to provide pediatric preventive dental care services. We determined dental care shortage areas based on the difference between available supply and demand. We categorized counties as rural or urban to identify geographic disparities.22 Because this study did not include human subjects, it was considered exempt from institutional review board review.
Estimated Caries Risk
The guidelines for caries risk assessment specify 3 categories of risk based on a child’s sociodemographic characteristics, behavior, and clinical indicators, as well as professional judgment.19,23 Because these guidelines do not provide a standardized case definition for each risk category and because census data do not include data on some of the risk factors, we estimated 2 levels of caries risk based on available census data.
We used data from the oral examination component of the 2001-2012 National Health and Nutrition Examination Survey24 to classify children as high risk if they were aged <6 years and had at least 1 tooth surface with caries (treated or untreated) or if they were aged ≥6 years and had ≥3 tooth surfaces with caries. To identify sociodemographic variables that predicted a child’s risk, we used a quasibinomial logistic regression model for children aged <6 years that fit the dichotomous outcome of caries versus no caries and a quasi-Poisson model for children aged ≥6 years that fit the count variable of number of tooth surfaces with caries. We estimated the prevalence of high-risk patients using a microsimulation model that generated virtual populations of children for each census tract based on 2010 US Census data.25 We applied the age-appropriate regression model to each virtual patient to determine risk and obtain the prevalence of high-risk children in each census tract. We used the Wald χ2 test, with P < .01 considered significant.
Estimated Pediatric Preventive Dental Care Demand
Pediatric preventive dental care demand is the total number of minutes required to provide preventive dental procedures at their recommended frequency annually. We used recommended procedures, which vary by age group (0-3, 4-5, 6-7, and 8-18 years) and caries risk, from the American Academy of Pediatric Dentistry guidelines.19 We estimated dental care demand per child (in minutes) for each age group stratified by caries risk. We estimated pediatric preventive dental care demand per county by multiplying per-child estimates for each age and risk group by the number of corresponding children living in that county, which we obtained from 2010 US Census data.26 We converted pediatric preventive dental care demand into procedure minutes using published data on procedure times.27
Estimating Pediatric Preventive Dental Care Supply
To estimate the time allocated to pediatric dental care for general and pediatric dentists, we first used national data to estimate the percentage of pediatric and general dentist time allocated to pediatric preventive dental care and then multiplied these percentages by average annual work hours. Finally, we multiplied these values by the corresponding number of general and pediatric dentists in each Georgia county and then summed them across provider types to obtain pediatric supply per county.
Estimating Percentage Hours Allocated to Pediatric Preventive Dental Care
We used data from the Medical Expenditure Panel Survey28 to estimate the percentage of total dental hours spent on pediatric preventive dental care services. We first obtained frequencies for diagnostic and preventive procedures (eg, examinations, cleanings, x-rays, fluoride applications, and sealants) and restorative and treatment procedures (fillings, crowns, root canals, extractions, bridges, dentures, and whitening) for children (by age group) and adults (aged ≥19). We estimated the time allocated to preventive and treatment services provided to children and adults by multiplying procedure frequencies by their respective service times, which were obtained from a published study27 and expert opinion from the Georgia Department of Public Health and the Division of Oral Health at the Centers for Disease Control and Prevention. Finally, we divided time spent on pediatric preventive dental services by total time spent on pediatric and adult preventive and treatment services. For general dentists, this value was 22%. We calculated the percentage of pediatric dentist hours available for child preventive services in a similar manner, with the exception that times for adult services were not included. This value was 84%.
Estimating Total Dental Care Hours per Provider
Based on the 2010 Survey of Dental Practice,29 male and female dentists work an average of 35.2 and 33.6 hours per week, respectively, for 49 weeks each year, which translates to 1714 hours per dentist per year. By multiplying annual hours per dentist by percentage time allocated to pediatric dental care, we estimated the hours allocated to pediatric dental care to be 377 for general dentists and 1440 for pediatric dentists. To account for dental hygiene support, we assumed that dental hygienists had the same pediatric dental care caseload of a dental provider and that each dentist had 2 hygienists under his or her supervision.30 After including dental hygiene hours, we estimated pediatric dental care hours to be 1131 hours per general dentist and 4319 hours per pediatric dentist.
Estimating Number of Dental Providers
We obtained providers’ practice location addresses and specialties from 2 data sources: the 2015 National Plan and Provider Enumeration System31 data set and the Georgia Board of Dentistry roster for licenses expiring March 2015.32 We used the roster as the initial supply base, and we used the data set to link the National Provider Index with a taxonomy code to records in the roster. Dental care supply consisted of dentists (codes 1223G0001X, 1223P0221X, and 122300000X) and dental hygienists (code 124Q00000X). From these data, we identified all providers who delivered preventive care to children.
Estimated Pediatric Preventive Dental Care Shortage Areas
For each Georgia county, we estimated the ratio of pediatric demand to supply. We designated a county as a dental care shortage area if this value exceeded 2. We chose this value because national data indicate that approximately 50% of children aged 0-18 use dental services at least once in a year.28 Finally, we compared counties identified as dental care shortage areas by our methods with counties designated by HRSA as HPSAs.33
Results
Of 2 489 727 children in Georgia, we estimated that 349 060 (95% CI, 315 946-382 173) were at high risk for dental caries in 2015 (Table). The per-county prevalence of children at high risk for dental caries by census tract ranged from 8.1% (95% CI, 7.8%-8.3%) to 36.6% (95% CI, 35.1%-38.4%; Figure 1). Each variable in the final logistic regression analysis was significant at P < .05.
Table.
Estimated annual pediatric preventive dental care demand per child, measured in minutes, by age and risk group, Georgia, 2015a
| Age, y | Dental Care Demand per Child per Year, minb | |
|---|---|---|
| Low-Risk Groupc | High-Risk Groupc | |
| 0-3 | 39.7 | 79.4 |
| 4-5 | 80.7 | 155.6 |
| 6-7 | 60.8 | 121.6 |
| 8-18 | 51.6 | 103.2 |
aData sources: 2010 US Census data26 and 2001-2012 National Health and Nutrition Examination Survey data.24
bAnnual pediatric preventive dental care demand per child per year was measured in minutes by using (1) caries risk estimated from a multivariate analysis of National Health and Nutrition Examination Survey data, (2) recommended procedures (by age and risk) by the American Academy of Pediatric Dentistry, and (3) service time for each procedure based on published studies.
cAge and risk groups were defined by the American Academy of Pediatric Dentistry guidelines.19
Figure 1.
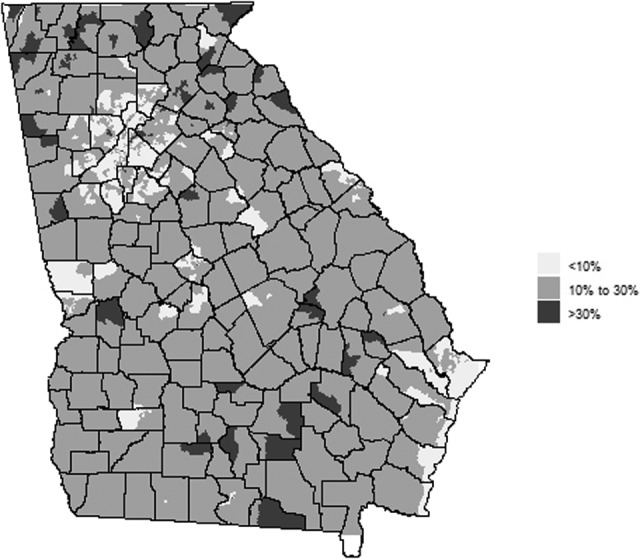
Estimated percentage of children at high risk of dental caries, by census tract, Georgia, 2015. The values range from 8.1% to 36.6%. Percentages were calculated by creating logistic regression models that predicted whether a child was at high risk for having caries according to demographic data in the National Health and Nutrition Examination Survey and then simulating the population of the census tract with 2010 US Census data. Data sources: 2010 US Census data26 and 2001-2012 National Health and Nutrition Examination Survey.24
We estimated total demand for pediatric preventive dental care for Georgia to be 2.7 million hours. The county-level pediatric preventive dental care demand ranged from 395 to 251 920 hours, with a mean of 16 866 hours (median = 5996). We estimated the pediatric preventive dental care supply for Georgia to be 5.2 million hours. The county-level pediatric preventive dental care supply ranged from 0 to 913 181 hours, with a mean of 32 696 hours (median = 5652). Twenty-one counties had no pediatric preventive dental care supply hours because they had no practicing dentists (Figure 2).
Figure 2.
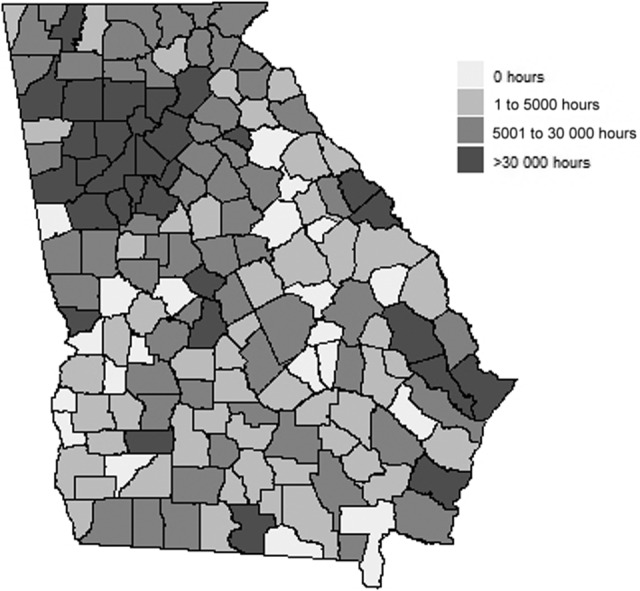
Estimated pediatric preventive dental care supply, in hours per year, by county, Georgia, 2015. Data sources: 2015 National Plan and Provider Enumeration System31 and 2015 Board of Dentistry roster from the Georgia Dental Association.32 The Board of Dentistry roster was used as the initial supply base. The National Plan and Provider Enumeration System data set was used to associate National Provider Index and a taxonomy code to each record in the roster, which allowed for the selection of only those dentists who provided preventive dental care services.
The pediatric preventive dental care supply exceeded demand in 75 counties, 37 of which were urban. Our methods identified 41 counties as pediatric dental care shortage areas, of which 25 were rural. For these counties, we estimated that it would take 46 908 additional supply hours per year to meet pediatric demand. If we classified any county where pediatric preventive dental care demand exceeded supply as a dental care shortage area, then 84 counties would qualify and the additional needed supply hours would be 241 748.
Of the 159 counties in Georgia, 100 were not designated as dental care shortage areas by HRSA or by our method. Of the 59 counties designated as a dental care shortage area by either method, 27 were designated as dental care shortage areas by both methods. We found that 32 counties differed in designation between the 2 methods (Figure 3); 14 were designated by our method only and 18 were designated by HRSA only. For these 18 counties designated as dental care shortage areas by HRSA, we estimated that none had pediatric preventive dental care demand greater than the available supply.
Figure 3.
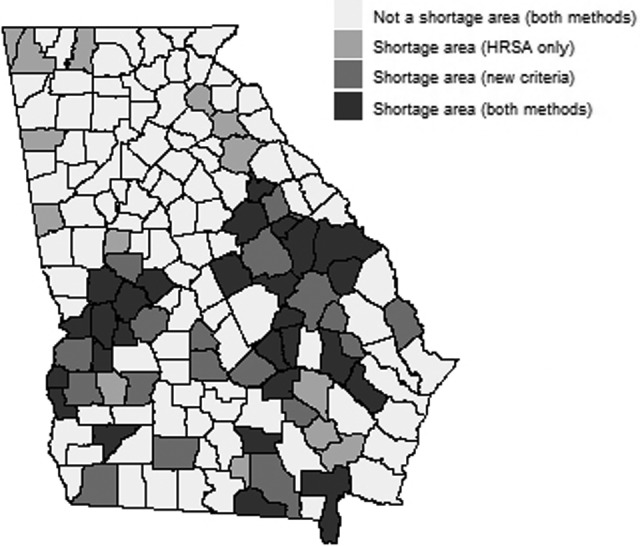
Designation of dental care shortage areas in counties differentiated by how shortage areas were determined, Georgia, 2015. Dental care shortage areas were defined in 3 ways: (1) by the Health Resources & Services Administration (HRSA) criteria, which are based primarily on supply factors without the consideration of primary care physicians20; (2) by criteria based on both supply and demand factors adjusted by caries for pediatric preventive dental care; and (3) by using both methods. Data source: Health professional shortage areas from HRSA.33
Discussion
Our findings suggest a poor distribution of pediatric preventive dental care in Georgia. Although for the state overall, supply of pediatric preventive dental care exceeded demand, demand was more than double the supply in 41 counties. Among children living in dental care shortage areas, those enrolled in Medicaid may have even greater barriers in accessing care than privately insured children, because only 28% of dentists in Georgia accept Medicaid.34 Strategies that could increase access to pediatric preventive dental care in these counties include implementing school-based dental sealant programs, as recommended by the Community Preventive Services Task Force,35 and increasing primary care providers’ provision of fluoride varnish to children aged ≤5 years, as recommended by the US Preventive Services Task Force.36 The state could also consider allowing dental hygienists to provide pediatric preventive dental care in schools without supervision by a dentist. Studies indicate that this policy would increase program efficiency and reach.37 States that allow insurers to directly reimburse hygienists increase annual use of hygienists by 3% to 4%.38 Furthermore, the success of dental schools in placing graduates in rural areas varies widely,39 possibly because of differences in recruitment strategies and loan-forgiveness policies.
Our methods can be used to identify strategies to increase the use of preventive dental care among children enrolled in Medicaid and the Children’s Health Insurance Program. Strategies designed to increase the demand for dental care (eg, increasing the income eligibility threshold or conducting oral health literacy campaigns) could be more effective in counties where supply exceeds demand or is close to demand than in counties with sufficient supply. Conversely, in pediatric dental care shortage areas, implementing strategies to incentivize providers to locate there or increasing Medicaid reimbursements40 may be effective.
We found similarities between the HRSA model and our model. Both models prioritize (1) counties with a large number of low-income children, an explicit HRSA criterion and a predictor of risk in our model and (2) counties with fewer dental providers compared with the average. A key difference is that we focused on specific services (preventive) for a specific population (children). Because pediatric preventive dental care services can be provided by auxiliary, such as dental hygienists or pediatricians, we weighted dental auxiliaries more heavily than HRSA does when we estimated dental care supply.
One interesting question is whether the increased specificity of our model provides useful information beyond the HRSA criteria. A 2012 study of dental capacity in Georgia found that 64 counties were pediatric dental care shortage areas according to the definition set by HRSA.41 Our methods identified 50 of these counties as pediatric dental care shortage areas. Identifying these areas is important because children and adults are likely to be targeted at different venues by dentists with different specialties, and having information about dental care shortage areas may allow for effective staffing and program targeting. Using our methods requires analytic capacity that some states may not possess; however, it would likely offer a higher return on investment for services based on surveillance (eg, school-based sealant programs) in (1) states that have not recently evaluated whether designated dental care shortage areas still meet the HRSA criteria or (2) states with surveillance data indicating rates of untreated decay or sealant prevalence among children that are higher or lower than the national average.
Although this analysis was largely conducted at the county level, the methods can be used to generate estimates at more local levels, such as ZIP code areas and census tracts. These levels can be important if specific targeting of resources is required, such as locating school-based sealant programs or providing oral health capacity at a federally qualified health center.
Limitations
This study had several limitations. First, our model (and the HRSA model) did not account for differences in policies between Medicaid and private dental insurance. Our model underestimated supply in areas with high Medicaid enrollment. That factor is important because dental supply available to Medicaid children relative to supply available to non-Medicaid children may decrease if Medicaid reimbursement rates or policies are lower or more restrictive than private insurance rates and policies. Second, professional guidelines on types and frequency of preventive dental services may not accurately measure demand. Demand for preventive dental care can also be influenced by the cost of care, income, and a person’s valuation or knowledge about oral health and the benefits of prevention. The cost for preventive dental care services may be close to zero for many children because pediatric preventive dental care services are an essential health benefit in the Affordable Care Act6; if so, demand would be underestimated by our approach.
Third, we obtained parameters on the effect of sociodemographic factors on caries risk and proportion of time spent on pediatric preventive dental care services relative to other services from national data and thus did not account for factors that could be specific to Georgia, leading to a potential error on demand. Fourth, dental procedure times were based on dated standards updated with expert opinion; inaccurate procedure times would lead to an error in the estimated supply. Fifth, county boundaries used in the analysis were defined for political reasons and did not represent true dental markets, although the analysis can be applied at the census tract level. Finally, there was no gold standard to determine how well our model or the HRSA model identified dental care shortage areas. As a result, we could compare findings between the models, but we could not identify the better model.
Conclusion
More than 25% of counties in Georgia had pediatric preventive dental care demand at least twice the available dental supply. The more detailed information on pediatric dental care shortage areas by age and service category provided by our model as compared with that defined by the HRSA criteria could result in more efficient provider staffing and geographic targeting of preventive dental care for school-based sealant programs or the provision of dental services through federally qualified health centers.
Acknowledgments
We thank Carol Smith, in the Oral Health Prevention Program at the Georgia Department of Public Health, for her engagement in this research.
Authors’ Note: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the National Science Foundation (CMMI-0 954 283). Dr Serban was also supported by the Coca Cola Early Professorship Chair, and Dr Griffin was supported by the Virginia C. and Joseph C. Mello Professorship Chair.
References
- 1. Newacheck PW, Hughes DC, Hung YY, et al. The unmet health needs of America’s children. Pediatrics. 2000;105(4, pt 2):989–997. [PubMed] [Google Scholar]
- 2. National Center for Health Statistics. Health, United States, 2015: With Special Feature on Adults Aged 55-64. Hyattsville, MD: National Center for Health Statistics; 2015. https://www.cdc.gov/nchs/data/hus/hus15.pdf. Accessed December 23, 2016. [Google Scholar]
- 3. National Institute of Dental and Craniofacial Research. Oral Health in America: A Report of the Surgeon General. Rockville, MD: US Department of Health and Human Services; 2000. https://www.nidcr.nih.gov/DataStatistics/SurgeonGeneral/Documents/hck1ocv.@www.surgeon.fullrpt.pdf. Accessed December 23, 2016. [Google Scholar]
- 4. Ahovuo-Saloranta A, Hiiri A, Nordblad A, et al. Pit and fissure sealants for preventing dental decay in the permanent teeth of children and adolescents. Cochrane Database Syst Rev. 2004;(3):CD001830. [DOI] [PubMed] [Google Scholar]
- 5. Marinho VC, Higgins JP, Logan S, et al. Topical fluoride (toothpastes, mouthrinses, gels or varnishes) for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003;(4):CD002782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Griffin SO, Barker LK, Wei L, et al. Use of dental care and effective preventive services in preventing tooth decay among US children and adolescents—Medical Expenditure Panel Survey, United States, 2003-2009 and National Health and Nutrition Examination Survey, United States, 2005-2010. MMWR Morb Mortal Wkly Rep. 2014;63(2):54–60. [PubMed] [Google Scholar]
- 7. US Department of Health and Human Services. Healthy People 2020. https://www.healthypeople.gov. Accessed December 23, 2016. [DOI] [PubMed]
- 8. Sintonen H, Linnosmaa I. Economics of dental services In: Culyer AJ, Newhouse JP, eds. Handbook of Health Economics. Vol 1, pt A Amsterdam, Netherlands: Elsevier; 2000:1251–1296. [Google Scholar]
- 9. Heft MW, Gilbert GH, Shelton BJ, et al. Relationship of dental status, sociodemographic status, and oral symptoms to perceived need for dental care. Community Dent Oral Epidemiol. 2003;31(5):351–360. [DOI] [PubMed] [Google Scholar]
- 10. Bell JF, Huebner CE, Reed SC. Oral health need and access to dental services: evidence from the National Survey of Children’s Health, 2007. Matern Child Health J. 2012;16(suppl 1):27–34. [DOI] [PubMed] [Google Scholar]
- 11. US General Accounting Office. Oral health: dental disease is a chronic problem among low-income populations. Report to Congressional requesters. http://www.gao.gov/new.items/he00072.pdf. Published 2000. Accessed December 23, 2016.
- 12. Seale NS, Casamassimo PS. Access to dental care for children in the United States: a survey of general practitioners. J Am Dent Assoc. 2003;134(12):1630–1640. [DOI] [PubMed] [Google Scholar]
- 13. Buchmueller TC, Orzol S, Shore-Sheppard LD. The effect of Medicaid payment rates on access to dental care among children. Am J Health Econ. 2015;1(2):194–223. [Google Scholar]
- 14. Bureau of Health Workforce. National and State-Level Projections of Dentists and Dental Hygienists in the US, 2012-2025. Washington, DC: US Department of Health and Human Services; 2015. https://bhw.hrsa.gov/sites/default/files/bhw/nchwa/projections/nationalstatelevelprojectionsdentists.pdf. Accessed December 23, 2016. [Google Scholar]
- 15. Beazoglou T, Bailit H, Myna V, et al. Supply and demand for dental services: Wisconsin 2010-2020. Report to the Wisconsin Dental Association. http://www.wda.org/wp-content/uploads/2012/04/Supply-and-Demand_Final-Report.pdf. Published 2010. Accessed December 23, 2016.
- 16. Nasseh K, Vujicic M. Dental care utilization rate highest ever among children, continues to decline among working-age adults. Health Policy Institute research brief. http://www.ada.org/∼/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_1014_4.ashx. Published 2014. Accessed December 23, 2016.
- 17. Meyerhoefer CD, Zuvekas SH, Manski R. The demand for preventive and restorative dental services. Health Econ. 2014;23(1):14–32. [DOI] [PubMed] [Google Scholar]
- 18. Vujicic M, Yarbrough C, Nasseh K. The effect of the Affordable Care Act’s expanded coverage policy on access to dental care. Med Care. 2014;52(8):715–719. [DOI] [PubMed] [Google Scholar]
- 19. American Academy of Pediatric Dentistry. Guideline on periodicity of examination, preventive dental services, anticipatory guidance/counseling, and oral treatment for infants, children, and adolescents. Pediatr Dent. 2013;35(5):E148–E156. [PubMed] [Google Scholar]
- 20. US Government Accountability Office. Health professional shortage areas: problems remain with primary care shortage area designation system: report to Congressional committees. http://www.gao.gov/assets/260/252841.pdf. Published 2006. Accessed December 23, 2016.
- 21. Munson B, Vujicic M. Supply of dentists in the United States is likely to grow. Health Policy Institute research brief. http://www.ada.org/∼/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_1014_1.ashx. Published 2014. Accessed December 23, 2016.
- 22. Georgia Department of Community Health. An overview of the State Office of Rural Health. https://dch.georgia.gov/sites/dch.georgia.gov/files/imported/vgn/images/portal/cit_1210/49/40/70650185StateOfficeRuralHealthFY12.pdf. Published 2012. Accessed December 23, 2016.
- 23. American Dental Association. Oral health topics: caries risk assessment and management. http://www.ada.org/en/member-center/oral-health-topics/caries-risk-assessment-and-management. Published 2016. Accessed December 23, 2016.
- 24. Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. https://www.cdc.gov/nchs/nhanes/index.htm. Accessed January 26, 2017.
- 25. Davila-Payan C, DeGuzman M, Johnson K, et al. Estimating prevalence of overweight or obese children and adolescents in small geographic areas using publicly available data. Prev Chronic Dis. 2015;12:E32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. US Census Bureau. Table PCT3: sex by age. http://factfinder2.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t. Published 2015. Accessed December 23, 2016.
- 27. Woodward GL, Csima A, Leake JL, et al. Estimation of procedure times in a publicly funded dental programme. Community Dent Health. 1995;12(3):155–160. [PubMed] [Google Scholar]
- 28. Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. http://meps.ahrq.gov/mepsweb. Accessed December 23, 2016.
- 29. American Dental Association. 2010 Survey of Dental Practice: Characteristics of Dentists in Private Practice and Their Patients. Chicago, IL: American Dental Association; 2012. [Google Scholar]
- 30. US Bureau of Labor Statistics. Occupational employment statistics. https://www.bls.gov/oes. Accessed January 26, 2017.
- 31. Centers for Medicare & Medicaid Services. National Plan and Provider Enumeration System (NPPES) downloadable file. http://download.cms.gov/nppes/NPI_Files.html. Accessed December 23, 2015.
- 32. Georgia Board of Dentistry. Roster request form—dentistry. https://gbd.georgia.gov/documents/applications-and-forms. Published 2015. Accessed July, 2016.
- 33. Health Resources & Services Administration. Health professional shortage areas (HPSAs). https://bhw.hrsa.gov/shortage-designation/hpsas. Accessed January 26, 2017.
- 34. American Dental Association. Oral health care system: Georgia. http://www.ada.org/en/∼/media/ADA/Science%20and%20Research/HPI/OralHealthCare-StateFacts/Georgia-Oral-Health-Care-System.pdf. Accessed December 23, 2016.
- 35. The Community Guide. Dental caries (cavities): school-based dental sealant delivery programs. https://www.thecommunityguide.org/oral/schoolsealants.html. Published 2013. Accessed December 23, 2016.
- 36. Moyer VA. US Preventive Services Task Force. Prevention of dental caries in children from birth through age 5 years: US Preventive Services Task Force recommendation statement. Pediatrics. 2014;133(6):1102–1111. [DOI] [PubMed] [Google Scholar]
- 37. Scherrer CR, Griffin PM, Swann JL. Public health sealant delivery programs: optimal delivery and the cost of practice acts. Med Decis Making. 2007;27(6):762–771. [DOI] [PubMed] [Google Scholar]
- 38. Wing C, Marier A. Effects of occupational regulations on the cost of dental services: evidence from dental insurance claims. J Health Econ. 2014;34:131–143. [DOI] [PubMed] [Google Scholar]
- 39. Vujicic M. Where do dental school graduates end up locating? J Am Dent Assoc. 2015;146(10):775–777. [DOI] [PubMed] [Google Scholar]
- 40. Decker SL. Medicaid payment levels to dentists and access to dental care among children and adolescents. JAMA. 2011;306(2):187–193. [DOI] [PubMed] [Google Scholar]
- 41. Georgia Health Policy Center. A Study of Georgia’s Dental Workforce 2012. Atlanta, GA: Georgia State University; 2012. [Google Scholar]


