Abstract
Background:
Rehabilitation after hospital stay implies several benefits for patients with chronic obstructive pulmonary disease (COPD); still few patients are referred and participate in rehabilitation programs. We conducted a case study to investigate the effects of interventions targeting the referral, uptake, and completion for a program of early rehabilitation in the primary health-care sector.
Methods:
We undertook targeted initiatives to make patients participate in an individualized rehabilitation program with gradual increased intensity. After discharge, primary care COPD nurses and physiotherapists guided patients through progressing exercises in small groups online. Patients proceeded to class-based exercises, patient education and/or leisure activities, or continued telerehabilitation. We evaluated the effects of the intervention by assessing referral rates, completion, and readmission.
Results:
Sixteen (23% of discharged patients) patients were referred to rehabilitation. In comparison, only 1 (0.8%) in 131 patients from Vejle hospital was referred to Vejle hospital. Twelve patients completed rehabilitation, all having severe COPD. All started the program within 2 weeks and proceeded to the online-guided exercises within 4 weeks. Study data showed that after 30 days, 1 (6.3%) of the 16 patients in the rehabilitation program had been readmitted compared to 8 (14.8%) of 55 patients who were not referred. After 90 days, 2 (12.5%) and 11 (20.0%) patients were readmitted, respectively. The readmission rate showed a nonsignificant decline in patients participating in rehabilitation.
Conclusion:
This case study showed that the referral rate of patients with COPD to early municipal rehabilitation is extremely low without a targeted effort and still insufficient in spite of a focused intervention. We showed that completion of a municipal rehabilitation program shortly after discharge is possible even for patients with severe COPD. The findings from our pilot study can guide further investigations into the effect of implementation strategies for handovers between health-care sectors to secure early-onset rehabilitation of patients with COPD.
Keywords: rehabilitation, COPD, referral rates, readmission, patient satisfaction
Background
Exacerbations of chronic obstructive pulmonary disease (COPD) are common and have a profound influence on the health status of patients. Repeated exacerbations are associated with increased mortality,1 reduced quality of life,2 and accelerated decline in lung function.1,3,4 Moreover, exacerbations of COPD cause frequent and prolonged hospital admissions,1 potentially initiating a vicious circle of inactivity, conditional decline, and repeated exacerbations.5
To prevent this vicious circle, a newly published Danish national guideline6 recommends to start rehabilitation during the first 4 weeks after discharge. Yet, rehabilitation of patients with COPD is often delayed or not carried out at all.7
Implementing clinical guidelines is generally challenging8 and more so in the management of COPD compared to other chronic conditions.9 As a result, rates of completion of pulmonary rehabilitation are among the lowest of evidence-based services for patients with COPD.7,10
The deteriorated clinical state of patients after an exacerbation, disease severity, and comorbidity are often indicated as reasons for patients to decline rehabilitation.10,11 Moreover, provider-related and organizational factors can be barriers to early rehabilitation. For example, the reluctance of clinicians to refer patients, lack of belief in the evidence for rehabilitation, or practical problems with referrals can all hinder early rehabilitation.10-13 Addressing such barriers when implementing recommendations of early rehabilitation is vital.
Overall, there is a need for new knowledge on how to overcome demonstrated obstacles and incorporate the resources of patients. Professionals should acknowledge psychological aspects such as fears, concerns, and need for motivational support of patients. Tailoring rehabilitation programs to the needs of patient and planning for time and travel constraints can facilitate implementation.10,14-20
Thus, we conducted a case study to investigate the effects of interventions targeting the referral, uptake, and completion for a program of early rehabilitation in the primary health-care sector.
Methods
Setting
We conducted this interventional case study in the Region of Southern Denmark that covers a fifth of Denmark (1.2 million citizen). Health-care coverage in Denmark is universal, all citizens have free access, and it is free of charge. The study was from the outset planned to involve 2 specialized pulmonary medical wards at Odense University Hospital (OUH) location, Svendborg, and Vejle Hospital and 2 rehabilitation departments (the municipalities of Faaborg-Midtfyn and Vejle). The regional center for quality improvement acted as the coordinator in the study. Both medical wards occupy specialists in pulmonary medicine and see patients in the hospital as well as in outpatient clinics. The municipalities in the region are primarily responsible for rehabilitation of patients with COPD and receive referrals from the hospital departments and general practitioners.
Study Population
All patients living in the 2 municipalities with a diagnosis of COPD and hospitalized for an exacerbation at OUH, Svendborg, and Vejle Hospital from December 2014 to June 2015 were potentially eligible for inclusion. Based on registry data from the equivalent period the previous year, we expected discharge of approximately 175 patients with COPD in the period to the 2 municipalities and thus possible candidates for referral to early-onset rehabilitation.
The Situation Prior to the Study
Prior to the publication of the national guideline, physicians in OUH, Svendborg, and Vejle Hospitals decided about rehabilitation during a planned outpatient visit about a month after a discharge from hospital. This routine is not compatible with implementation of the recommendation regarding early-onset rehabilitation. Likewise, the rehabilitation programs in the municipalities also did not support the concept of initiating rehabilitation shortly after discharge. Therefore, the ongoing routines had to be revised in order to implement the new guideline.
Odense University Hospital, Svendborg, and the municipality of Faaborg-Midtfyn agreed to change the procedures of referral and the rehabilitation program accordingly. In Vejle, the municipality managed to establish a program for early rehabilitation, but Vejle Hospital did not succeed in changing the referral routines. Consequently, the municipality of Vejle and the Vejle Hospital could not act as active participant in the intervention but instead we converted the site into a control setting with unchanged routines.
Interventions to Improve Referral and Uptake Into the Program
Due to habits following the former routines, we anticipated clinicians to be reluctant to refer patients to early rehabilitation. We planned new and simpler referral procedures to encourage staff to refer patients at the time of discharge to rehabilitation in the municipality. For educational purposes, we also passed on information on the new clinical guideline and the content of the municipality program (see Table 1). Physicians decided at discharge whether to refer patients to rehabilitation in the municipality based on the criteria of “unsuitability” (eg severe comorbidity, patient motivation).
Table 1.
Overview of Interventions, Target Groups, and Expected Effects.
| Problem | Interventions to Initiate Early Rehabilitation | Main Target Group for Intervention | Purpose of Intervention | Expected Effect | |
|---|---|---|---|---|---|
| Hospital | Few referrals | Simplification of referral to rehabilitation in municipality | Leaders, keypersons, local champions, clinicians | Transparency of referral pathway | Increase referrals |
| Dissemination of guidelines and the evidence behind | Leaders, keypersons, local champions, clinicians | Increase knowledge | |||
| Information on content of municipality rehabilitation | Clinicians | Increase knowledge | |||
| Patient handout | Patients, relatives, clinicians | Increase knowledge, motivation | |||
| Municipality | Insufficient uptake | Early contact by municipality nurse | Patients | Reassurance, motivation | Increase uptake |
| Low completion rate | Individualization of rehabilitation trajectory | Patients | Reassurance, motivation, confidence | Increase completion | |
| Telerehabilitation | Patients | Reassurance, motivation, confidence, support |
We also prepared a new handout for patients at discharge to inform and motivate them to participate in the rehabilitation program. The implementation process involved key persons and local champions to ensure communication of the new routine to staff involved in the referrals of patients.
Interventions to Improve Completion of the Program
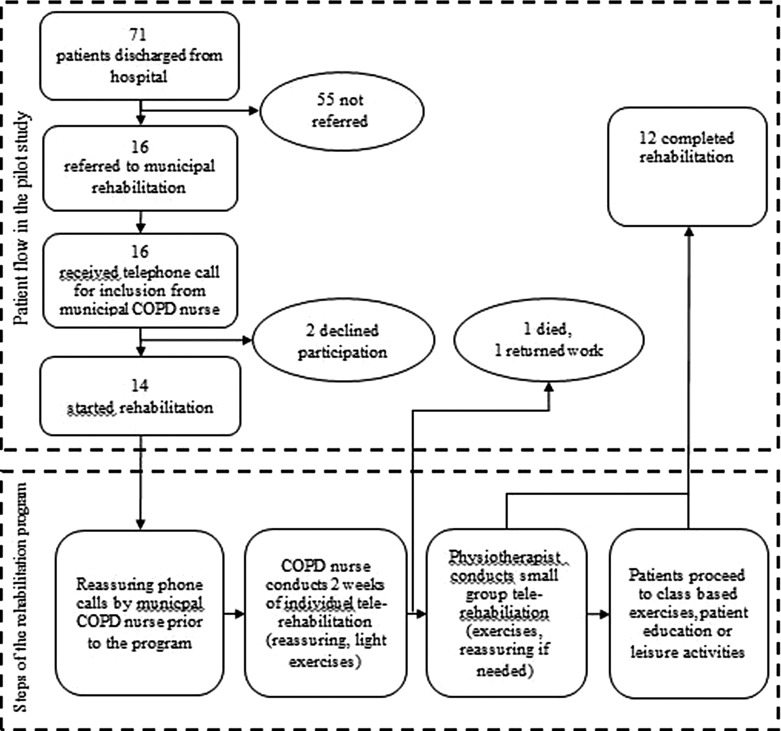
During the first week after discharge, a municipal-employed COPD nurse contacted referred patients to inform about the rehabilitation program and to initiate contact with the patient by offering the opportunity of reassuring phone calls. If the patient agreed to participate in the program, a technician installed a computer in the patient’s home to be used for telerehabilitation. The rehabilitation program in the municipality contained elements, which allowed for individualized rehabilitation trajectories of gradual increase in intensity. Depending on the individual demand, the COPD nurse had frequent online conversations with the patient followed by few tailored physical and guided exercises. After 2 weeks, a physiotherapist took over and guided patients online through individualized exercises in small groups of 3 to 4. The patients could still contact the nurse if needed (see the lower part of Figure 1). Rehabilitation continued with class-based exercises, patient education and/or leisure activities in the municipality, or continued telerehabilitation with increasing intensity of the exercises.
Figure 1.
Overview of the inclusion of patients in the pilot study and the elements of the municipal rehabilitation program.
Collection of Data on Referral and Completion Rates
We used data from national registries.21 We collected data from the National Patient Registry22 on all patients with a COPD diagnosis (ICD-10 codes J44.0-J44.9) from Faaborg-Midtfyn and Vejle municipalities who were discharged during mid-December 2014 to mid-June 2015. The first COPD admission/discharge in the inclusion period served as the index admission/index discharge. We registered readmission rates for 30 and 90 days based on readmissions within 0 to 90 days from the index discharge date. We counted patients with several admissions up to 90 days for COPD as multiple readmissions. We identified patients using their unique civil person registry identification number (CPR-number).23 The following rates were determined:
The proportion of discharged patients referred from hospital to municipal rehabilitation.
The proportion of referred patients declining inclusion in the rehabilitation program.
The proportion of patients participating actively in the program within 4 weeks after discharge.
The proportion of patients completing the program.
The rate of readmission to hospital after the rehabilitation program.
Ethics
Patients gave individual written consent for the use of their CPR-number for identification. The Regional Data Protection Agency gave approval to the study (id number: 15/36088). We informed the Council of Ethics about the study, and patients signed informed consent forms before the collection of data.
Results
During the study period, 71 patients living in the municipality of Faaborg-Midtfyn were discharged from hospital after an admission for an exacerbation. Sixteen (23%) of them were referred to municipal rehabilitation. In comparison, 1 (0.8%) of 131 patients from Vejle Hospital was referred to Vejle Hospital. No follow-up was carried out for this 1 patient.
After initial contact from the municipality COPD nurse, 2 patients declined to participate, leaving 14 patients for inclusion (see the upper part of Figure 1). One patient dropped out after a few weeks to resume work and 1 patient died. The remaining 12 patients completed the rehabilitation program. All 12 patients had severe COPD (grades 4 or 5) according to the Medical Research Council Dyspnea Scale.6 They all started the individualized program within 2 weeks and exceeded to the online-guided physical exercises in small groups within 4 weeks of discharge. Although readmission was not the focus of the study, data show that after 30 days, 1 (6.3%) of the 16 patients in the rehabilitation program had been readmitted compared to 8 (14.8%) of 55 patients who were not referred. After 90 days, 2 (12.5%) and 11 (20.0%) patients were readmitted, respectively (see Table 2). The numbers from patients not referred to rehabilitation are in line with the percentage of readmissions from the comparison group in Vejle of 13.7% at 30 days and 22.0% at 90 days. Although there are differences in referral percentage between the referred and nonreferred groups, these differences were nonsignificant (P = .67) nor there were differences between the rehabilitated group and the comparison group from Vejle (P = .69). To calculate the P values, we used Fisher exact test.
Table 2.
Characteristics of Patients Who Participated in the Rehabilitation Program in Faaborg-Midtfyn Municipality.
| Patients Referred (n = 16) | Patients Not Referred (n = 55) | |
|---|---|---|
| Median age (range) | 66.5 (49-90) | 78.0 (51-91) |
| COPD severity, MRCa grade (range) | 4 (2-5) | b |
| Median years of disease duration (range) | 9 (1-40) | b |
| Median number of hospitalizations for COPD (range) | 5 (1-25) | b |
| Initiation of information and nurse-guided individual telerehabilitation within 1 week | 14 | b |
| Initiation of physio-guided telerehabilitation in small groups within 4 weeks | 14 | b |
| Number of 30-day readmissionsc (percentage) | 1 (6.3%) | 8 (14.5%) |
| Number of 90-day readmissionsc | 2 (12.5%) | 11 (20.0%) |
Abbreviation: COPD, chronic obstructive pulmonary disease.
aMedical Research Council.
bInformation not available through registry data (consent was not possible to contain due to ethics).
cBased on all 16 patients in the study.
Discussion
In this study, we tried to address known challenges of implementing early rehabilitation.10,11,14,16,24 We focused especially on referral procedures to increase the rates of referrals and to avoid drop-offs after enrollment by establishment of an individualized municipal rehabilitation program. The results of the study showed that the rate of referrals to the rehabilitation program was negligible in the control setting (Vejle) but higher than in most other studies in Faaborg-Midtfyn.15,25 Nevertheless, even in this municipality, only a quarter of eligible patients were referred.
We tried to address a variety of factors and involved relevant stakeholders, which probably contributed to the higher referral rate to the rehabilitation program in the intervention setting in this study. Still, a majority of the patients were not referred. Earlier studies show that the reasons for not referring patients often are a complex combination of patient- and context-related factors.24,26 Probably some of these factors were not addressed rigorously enough in this pilot study.
The limited interest at the site converted into control setting could indicate that we were not able to convince leaders and staff in the appropriateness and benefits of referring patients to the municipality rehabilitation program. The targeted factors may not have been enough to encourage health-care staff to follow new routines. Perhaps, more involvement and education needs to be performed before physicians become aware of the potential benefits of early-onset rehabilitation, thereby being able to demonstrate a sufficiently enthusiastic attitude and belief in such programs.20,27
Studies have demonstrated that patients with COPD will not always accept and adhere to rehabilitation programs shortly after discharge.27,28 Some feel too ill or disabled to participate and others lack belief in the benefit of the programs.18 Therefore, motivating patients for rehabilitation at discharge is crucial and potentially not optimally addressed in this study. Another reason for noncompliance might be poor timing of introducing patients to rehabilitation programs at the time point of discharge.
These experiences lead us to hypothesize that successful uptake of patients cannot be obtained by focusing alone on optimizing and refining existing referral procedures. Probably, innovative approaches to the handover process between secondary and primary health care are needed. Such novel approaches should embrace a handover that is agreed upon by all stakeholders. We believe that rehabilitation shortly after discharge needs to be individualized and appropriate to each patient traveling across health-care settings. Patients’ concerns and wishes need to be taken into account whenever possible. Furthermore, we think that a predefined and theory-based implementation strategy potentially could create the foundation for dissemination of a useful pathway securing early rehabilitation.
The results from the study indicate that once enrolled, adherence to the rehabilitation program in Faaborg-Midtfyn was high. Participating patients, many with severe degrees of dyspnea, completed the rehabilitation and few patients were readmitted to the hospital. The slowly increasing intensity of the actual program and the reassuring effect of the initial telecommunication with the nurse could be an important element for adhering to the program. These factors are in line with previous studies.29,30
Conclusion
In conclusion, the results from this case study showed that the referral rate of patients with COPD to early municipal rehabilitation is extremely low without a targeted effort and still insufficient in spite of a focused intervention. On the other hand, we showed that completion of a municipal rehabilitation program shortly after discharge is possible even for patients with severe COPD. The findings from our pilot study can guide further investigations into the effect of implementation strategies for handovers between health-care sectors to secure early-onset rehabilitation of patients with COPD.
Acknowledgments
The authors wish to thank Ole Bruun Rasmussen, MD, OUH, Svendborg, for the initial contact to the medical ward and support throughout the study. The authors acknowledges the medical ward at OUH, Svendborg, for referral contribution, the rehabilitation department of Faaborg/Midtfyn municipality for helping with the data collection, and patients for participating in the interviews.
Author Biographies
Lars Morsø, Physiotherapist, MPH, PhD, is a fulltime researcher at the Regional Centre for Quality, Southern Denmark and is affiliated to the University of Southern Denmark. Besides working on improvement science research on various chronic diseases, e.g. chronic obstructive pulmonary disease he has done comprehensive work in the field of low back pain. He is appointed to the review committee of the Danish Physiotherapy Association's research foundation and he is involved in the revision of the Regional Danish Management Guidelines on low back pain.
Morten Sall Jensen, Cand. Scient. Med, PhD stud. He is currently doing his PhD work at the Centre for Quality in the field of the economical burden of low back pain. Morten S Jensen has specialized in economical analysis in health care utilities.
Christian von Plessen, MD, PhD, is director Center for Quality, Region of Southern Denmark and associate professor at Institute for Regional Health Research, University of Southern Denmark. He is an internist and respiratory care specialist and an IHI improvement advisor. He has led quality improvement programs in Norwegian and Danish hospitals. His research interests are patient safety and resilience, system integration and coproduction of health care service.
Peter Qvist, MD, is a specialist in internal medicine and medical gastroenterology. He is former leader of the Danish national quality program ‘The Good Medical Department’. He is associate professor at the University of Southern Denmark until October 2016. Presently attached to the Centre for Quality in the Region of Southern Denmark working primarily with organizational aspects of care for patients with chronic diseases.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Suissa S, Dell’Aniello S, Ernst P. Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax. 2012;67(11):957–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Spencer S, Jones PW. Time course of recovery of health status following an infective exacerbation of chronic bronchitis. Thorax. 2003;58(7):589–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Seemungal TA, Wedzicha JA. Acute exacerbations of COPD: the challenge is early treatment. COPD. 2009;6(2):79–81. [DOI] [PubMed] [Google Scholar]
- 4. Vestbo J, Hurd SS, Agusti AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. [DOI] [PubMed] [Google Scholar]
- 5. Williams V, Bruton A, Ellis-Hill C, McPherson K. The importance of movement for people living with chronic obstructive pulmonary disease. Qual Health Res. 2011;21(9):1239–1248. [DOI] [PubMed] [Google Scholar]
- 6. National Clinical guideline for rehabilitation of patients with chronic obstructive pulmonary disease. The Danish Health Board. 2014. Web site http://www.sst.dk. Accessed June 3, 2014.
- 7. Johnston K, Grimmer-Somers K. Pulmonary rehabilitation: overwhelming evidence but lost in translation? Physiother Can. 2010;62(4):368–373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Grol R, Wensing M. What drives change? Barriers to and incentives for achieving evidence-based practice. Med J Aust. 2004;180(suppl 6):S57–S60. [DOI] [PubMed] [Google Scholar]
- 9. Ofman JJ, Badamgarav E, Henning JM, et al. Does disease management improve clinical and economic outcomes in patients with chronic diseases? A systematic review. Am J Med. 2004;117(3):182–192. [DOI] [PubMed] [Google Scholar]
- 10. Benzo R, Wetzstein M, Neuenfeldt P, McEvoy C. Implementation of physical activity programs after COPD hospitalizations: lessons from a randomized study. Chron Respir Dis. 2015;12(1):5–10. [DOI] [PubMed] [Google Scholar]
- 11. Fischer MJ, Scharloo M, Abbink JJ, et al. Participation and drop-out in pulmonary rehabilitation: a qualitative analysis of the patient’s perspective. Clin Rehabil. 2007;21(3):212–221. [DOI] [PubMed] [Google Scholar]
- 12. Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: global burden of disease study. Lancet (London, England). 1997;349(9064):1498–1504. [DOI] [PubMed] [Google Scholar]
- 13. Seymour JM, Moore L, Jolley CJ, et al. Outpatient pulmonary rehabilitation following acute exacerbations of COPD. Thorax. 2010;65(5):423–428. [DOI] [PubMed] [Google Scholar]
- 14. Arnold E, Bruton A, Ellis-Hill C. Adherence to pulmonary rehabilitation: a qualitative study. Respir Med. 2006;100(10):1716–1723. [DOI] [PubMed] [Google Scholar]
- 15. Fischer MJ, Scharloo M, Abbink JJ, et al. Drop-out and attendance in pulmonary rehabilitation: the role of clinical and psychosocial variables. Respir Med. 2009;103(10):1564–1571. [DOI] [PubMed] [Google Scholar]
- 16. Garrod R, Marshall J, Barley E, Jones PW. Predictors of success and failure in pulmonary rehabilitation. Eur Respir J. 2006;27(4):788–794. [DOI] [PubMed] [Google Scholar]
- 17. Harris D, Hayter M, Allender S. Improving the uptake of pulmonary rehabilitation in patients with COPD: qualitative study of experiences and attitudes. Br J Gen Pract. 2008;58(555):703–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Keating A, Lee A, Holland AE. What prevents people with chronic obstructive pulmonary disease from attending pulmonary rehabilitation? A systematic review. Chron Respir Dis. 2011;8(2):89–99. [DOI] [PubMed] [Google Scholar]
- 19. Overington JD, Huang YC, Abramson MJ, et al. Implementing clinical guidelines for chronic obstructive pulmonary disease: barriers and solutions. J Thorac Dis. 2014;6(11):1586–1596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Perez X, Wisnivesky JP, Lurslurchachai L, Kleinman LC, Kronish IM. Barriers to adherence to COPD guidelines among primary care providers. Respir Med. 2012;106(3):374–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sortso C, Thygesen LC, Bronnum-Hansen H. Database on Danish population-based registers for public health and welfare research. Scand J Public Health. 2011;39(suppl 7):17–19. [DOI] [PubMed] [Google Scholar]
- 22. Lynge E, Sandegaard JL, Rebolj M. The Danish national patient register. Scand J Public Health. 2011;39(suppl 7):30–33. [DOI] [PubMed] [Google Scholar]
- 23. Pedersen CB. The Danish Civil Registration System. Scand J Public Health. 2011;39(suppl 7):22–25. [DOI] [PubMed] [Google Scholar]
- 24. Troosters T, Hornikx M, Demeyer H, Camillo CA, Janssens W. Pulmonary rehabilitation: timing, location, and duration. Clin Chest Med. 2014;35(2):303–311. [DOI] [PubMed] [Google Scholar]
- 25. Puhan MA, Gimeno-Santos E, Scharplatz M, Troosters T, Walters EH, Steurer J. Pulmonary rehabilitation following exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2011(10):CD005305. [DOI] [PubMed] [Google Scholar]
- 26. Johnston KN, Young M, Grimmer KA, Antic R, Frith PA. Barriers to, and facilitators for, referral to pulmonary rehabilitation in COPD patients from the perspective of Australian general practitioners: a qualitative study. Prim Care Respir J. 2013;22(3):319–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Johnston K, Grimmer-Somers K, Young M, Antic R, Frith P. Which chronic obstructive pulmonary disease care recommendations have low implementation and why? A pilot study. BMC Res Notes. 2012;5:652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Johnston KN, Young M, Grimmer-Somers KA, Antic R, Frith PA. Why are some evidence-based care recommendations in chronic obstructive pulmonary disease better implemented than others? Perspectives of medical practitioners. Int J Chron Obstruct Pulmon Dis. 2011;6:659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Paneroni M, Colombo F, Papalia A, et al. Is telerehabilitation a safe and viable option for patients with COPD? A feasibility study. COPD. 2015;12(2):217–225. [DOI] [PubMed] [Google Scholar]
- 30. Stickland M, Jourdain T, Wong EY, Rodgers WM, Jendzjowsky NG, Macdonald GF. Using Telehealth technology to deliver pulmonary rehabilitation in chronic obstructive pulmonary disease patients. Can Respir J. 2011;18(4):216–220. [DOI] [PMC free article] [PubMed] [Google Scholar]