Abstract
Objective
The purpose of this study was to examine the safety and efficacy of a high-intensity progressive rehabilitation protocol (HI) beginning 4 days after total knee arthroplasty (TKA) compared to a low-intensity (LI) rehabilitation protocol.
Methods
One hundred sixty-two participants (aged 63±7 years; 89 females) were randomized to either the HI group or LI group after TKA. Key components of the HI intervention were the utilization of progressive resistance exercises and a rapid progression to weight-bearing exercises and activities. Both groups were treated in an outpatient setting 2-3 times per week for 11 weeks (26 total sessions). Outcomes included the stair climbing test (SCT) (primary outcome), timed-up-and-go (TUG) test, 6-minute walk (6MW) test, the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Short-Form 12 (SF-12), knee ROM, quadriceps and hamstring strength, and quadriceps activation. Outcomes were assessed preoperatively and at 1, 2, 3 (primary end point), 6, and 12 months postoperatively.
Results
There were no significant differences between groups at 3 or 12 months in SCT, TUG, 6MW, WOMAC scores, knee ROM, quadriceps and hamstrings strength, quadriceps activation, or adverse event rates. By 12 months, outcomes on the 6MW, TUG, WOMAC, SF-12, quadriceps and hamstring strength, and quadriceps activation had improved beyond baseline performance in both groups.
Conclusion
Both the HI and LI interventions were effective in improving strength and function after TKA. High-intensity progressive rehabilitation is safe for individuals after TKA. However, its effectiveness may be limited by arthrogenic muscular inhibition in the early postoperative period.
Over 700,000 total knee arthroplasties (TKAs) are performed each year in the United States to alleviate pain and disability associated with knee osteoarthritis (OA), with 3.5 million per year expected by 2030.(1) Total knee arthroplasty reduces pain and improves self-reported function compared to pre-operative levels, but post-operative deficits in quadriceps strength (41% weaker), walking distance (28% less) and stair climbing speed (105% slower) persist after TKA compared to healthy adults. (2, 3) These findings suggest that current rehabilitation does not adequately target the impairments that lead to long-term deficits in functional mobility after TKA.
Although some studies suggest that rehabilitation after TKA has no long-term benefit, (4) emerging evidence suggests that more intensive rehabilitation, using progressive resistance exercise (PRE) and functional strengthening, may substantially improve patient function without compromising safety. (5–7) The greatest amount of strength and functional performance loss occurs in the first month after TKA, and therefore, early initiation of PRE and functional strengthening might help limit the extent of this loss (2); however, there has been only one randomized controlled trial that examined the effect of PRE initiated in the first week after TKA. Jakobsen et al (8) found that the addition of a resisted leg extension and leg press exercise did not lead to improved outcomes after TKA. However, the PRE intervention was limited to only two exercises, which failed to target all the major muscle groups of the lower extremity. In addition, the control group performed higher-level functional-based activities, such as stair-climbing and sit to stands, which may have led to a similar training effect and limited differences between groups.
Therefore, the purpose of this study was to evaluate the safety and efficacy of a high-intensity (HI) progressive rehabilitation program consisting of PRE targeting all major lower extremity muscle groups and a rapid progression to weight-bearing functional, balance, and agility exercises. We compared the HI program to a lower intensity (LI) intervention that had an initial focus on isometrics and active range of motion (ROM) exercise with a slower progression to weight-bearing exercise and activities as compared with LI. Our hypothesis was that the HI intervention would be as safe as the LI intervention and lead to superior outcomes in functional performance, self-reported function, quadriceps and hamstring strength, and quadriceps activation in both the short-term (3-month follow-up, end of intervention) and long-term (12-month follow-up).
Patients and Methods
Study design and patients
This was a randomized, double-blinded, controlled trial to evaluate the safety and efficacy of the HI intervention compared to the LI intervention. Patients were consecutively recruited by 9 participating orthopedic surgeons from 4 institutions from August 2011 to November 2014. Patients were included if they were awaiting a primary, unilateral TKA secondary to knee osteoarthritis (OA) and aged 50 to 85 years. Exclusion criteria were:1) current smoker, 2) current cancer treatment, 3) uncontrolled diabetes (hemoglobin A1c level <7.0), 4) body mass index (BMI) greater than 40 kg/m2, 5) neurological, vascular, or cardiac problems that limited function, 6) discharge to location other than home after surgery (e.g. skilled nursing facility), 7) severe contralateral knee OA (> 5/10 pain with stair climbing) or other orthopedic conditions that limited function and necessitated alternative concurrent intervention (e.g. severe lumbar spinal stenosis, severe hip or ankle OA). Informed consent was obtained from all participants. The study was approved by the University of Colorado Multiple Institutional Review Board and registered at ClinicalTrials.gov (NCT01537328).
Randomization and blinding
Eligible patients were randomly assigned to either the HI intervention arm or LI intervention arm. Randomization was carried out using a computer-generated allocation table and included stratification for sex and clinical site with random block sizes within each stratum. Patients and evaluators were both blinded to group assignment. Patients were blinded by being informed that they were participating in one of two interventions, both of which were commonly utilized in practice, and it was unknown if one was superior to the other. It was not possible to blind treating therapists to the interventions.
Procedures
All patients were assessed 1 to 2 weeks preoperatively and at 1, 2, 3, 6, and 12 months postoperatively at the Clinical Translational Research Center of the University of Colorado. The surgical technique and implant selection were based on surgeon preference. All components were cemented and the operations were performed via a medial parapatellar or mid-vastus approach, using either posterior stabilized or cruciate-retaining fixed or mobile bearing components. The patella was resurfaced in all instances. Following surgery, all patients received inpatient physical therapy twice daily prior to discharge.
Interventions
The HI and LI interventions were initiated 4.2 ± 1.2 (mean ± sd) days after surgery and took place at 4 different outpatient rehabilitation facilities in the Denver metro area. All patients were seen 3 times per week for the first 6 weeks and 2 times per week over the next 5 weeks. Testing sessions replaced a therapy session in weeks with a postoperative assessment for a total of 26 visits over 11 weeks. Treatment sessions averaged 45 minutes in length for both groups. Details on physical therapist selection, training, and fidelity oversight can be found in Appendix A.
Both the HI intervention and LI interventions included the following: education on healing after TKA, appropriate activities, pain, swelling, and wound management; training on transfers, gait (including assistive device progression), and stair climbing; up to 15 minutes per session of knee ROM and manual therapy techniques (9) focusing on restoration of knee range of motion; and a home exercise program (HEP) (Appendices B-D). Home exercise programs were based upon the exercises completed within clinical treatment sessions and prescribed to be completed twice daily for the first 4 weeks, once daily for weeks 5-6, and every other day on non-therapy days for the remainder of treatment.
HI Intervention
The HI intervention was a high-intensity, progression-based, rehabilitation program based on prior research (5, 6) and consisted of several domains: a warm-up; PRE targeting the ankle plantar flexors, quadriceps, hamstrings, and hip abductors, adductors, extensors and flexors; bilateral and unilateral weight-bearing functional exercises; balance exercises; agility exercises; and activity prescription. All PRE was performed for 2 sets of 8 repetitions and based on an 8-repetition maximum. All patients were prescribed a walking program as a part of their home exercise program at the beginning of rehabilitation with instructions to build up to 30 min of continuous walking 5 days per week. Once 30 minutes of walking was achieved, patients were allowed to progress into other cardiovascular activities such as swimming, cycling, elliptical machine, and stair climbing machine depending on their preferred mode of exercise.
LI Intervention
The LI intervention was a time-based rehabilitation program that was developed from the synthesis of previously published rehabilitation programs (10–13), chart reviews, therapist observation and interviews with treating therapists examining treatment preferences. Key differences from the HI program were: 1) an initial focus on isometric and ROM exercise for the first 4 weeks 2) a slower transition to weight-bearing exercises 3) less progression in difficulty of weight-bearing exercises 4) no resistance beyond body weight or elastic bands 5) restricted activity outside of ADLs for the first 4 weeks gradually building to 30 min by the end of therapy (restricted to walking and low-resistance cycling). Modalities (ice or heat depending on time point and patient preference) were added to the clinic treatment program for the LI group to account for the added treatment time to deliver the PRE intervention in the HI group.
Outcome measures
The primary outcome measure was the time required to ascend and descend a flight of 12 stairs (17.1 cm step height) as measured by the Stair Climbing Test (SCT) at the 3-month post-operative time point (end of intervention). The SCT was chosen as the primary outcome because stair climbing performance is the single largest residual deficit after TKA with 75% of patients reporting difficulty negotiating stairs years after TKA. (14) In addition, the SCT has been shown to be reliable and responsive to change. (15)
Secondary outcomes included measures of functional performance, health status questionnaires, knee range of motion (ROM), muscle strength, and quadriceps central activation. Secondary functional performance measures included the Timed “Up & Go” (TUG) test (16) and 6-minute Walk (6MW) test (17). The Physical Component Score (PCS) and Mental Component Score (MCS) of the 12-item Short-Form Health Survey questionnaire (SF-12) was utilized to assess global health status.(7) The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) was used to evaluate self-reported knee pain, stiffness, and function. (19) Active knee ROM was measured in the supine position with a long-arm goniometer. (20) Maximal voluntary isometric contraction (MVIC) of the quadriceps and hamstring muscles were measured at 60° of knee flexion utilizing a HUMAC NORM electromechanical dynamometer (CSMi, Stoghton, MA) and normalized to the participants body mass using methods previously described. (21) Voluntary activation of the quadriceps muscle was assessed using the doublet interpolation technique during quadriceps MVIC testing as previously described. (21)
Adherence
Therapist adherence for both groups was tracked using weekly chart reviews of all patient treatments and completion of a standardized fidelity checklist. Home exercise adherence was tracked with logs completed weekly by the patient and reviewed by the treating therapist to ensure accuracy of completion. Adherence was averaged over the course of treatment. The Physical Activity Scale for the Elderly (PASE) (22) was utilized as a secondary measure of home exercise adherence because activity prescriptions differed by group in the initial postoperative period. The PASE was collected at all testing sessions.
Adverse events
The incidence of musculoskeletal injury, falls, knee manipulation, and failure to attain at least 110° of active knee flexion were all tracked throughout the intervention period, and reviewed annually by the safety officer to determine the safety of both interventions. Musculoskeletal injuries were defined as a medically-diagnosed musculoskeletal injury that was related to the intervention and required at least a 1-week suspension of the intervention (other than ROM exercises).
Sample size
Based upon data from prior research, (6,21,23) we expected that the difference between groups at 3 months on the SCT would be 4.7 ± 8.1 seconds (mean ± SD). We determined that a sample size of 130 patients (65/group) would provide 90% power to detect differences at least this great between groups using a 2-sided, 2-group t-test at an α-level of 0.05. We enrolled 162 individuals in the study to allow for a 20% loss to follow-up.
Statistical analysis
The difference between the groups in the primary outcome measure, change in SCT at 3 months, was tested using an analysis of covariance model (ANCOVA); the 3-month change from baseline was regressed on sex, clinic site, and baseline SCT performance. Differences at three months of intervention in secondary outcomes (TUG, 6MW, WOMAC, SF12, knee ROM, quadriceps and hamstrings strength, and quadriceps activation) were analyzed utilizing the same method. Differences between groups at other time points (1,2, 6, and 12 months) were estimated using a repeated-measures maximum likelihood, cell means model using linear contrasts to estimate change from baseline and between-group differences in the outcome of interest; the 3-month comparisons from this model were used as a sensitivity analysis for the effect of missing data in the primary analysis. Explanatory variables included treatment group, sex, clinic site, and the baseline outcome measure. Differences in adherence between groups were estimated using an independent samples t-test, with the exception of the PASE, for which a repeated-measures maximum likelihood, cell means model was used. Another sensitivity analysis was done by adding PASE or HEP compliance to the outcomes models. Differences in the frequency of adverse events between groups were estimated using a Fisher's exact test for equal proportions. SAS version 9.3 (SAS Institute Inc, Cary, NC) was utilized for all statistical analyses. All analyses followed the intent-to-treat principle. A 2-sided p value of 0.05 without adjustment for multiple comparisons was designated a priori for statistical significance.
Results
Participant flow and characteristics
A total of 1358 individuals were assessed for eligibility in the study. One hundred sixty-two individuals (aged 63±7 years; 89 females) were randomized to either the HI intervention (n=84) or LI intervention (n=78). The patient flow diagram is shown in Figure 1. Baseline characteristics of the patients who were randomized to the intervention were similar between groups and are shown in Table 1.
Figure 1.
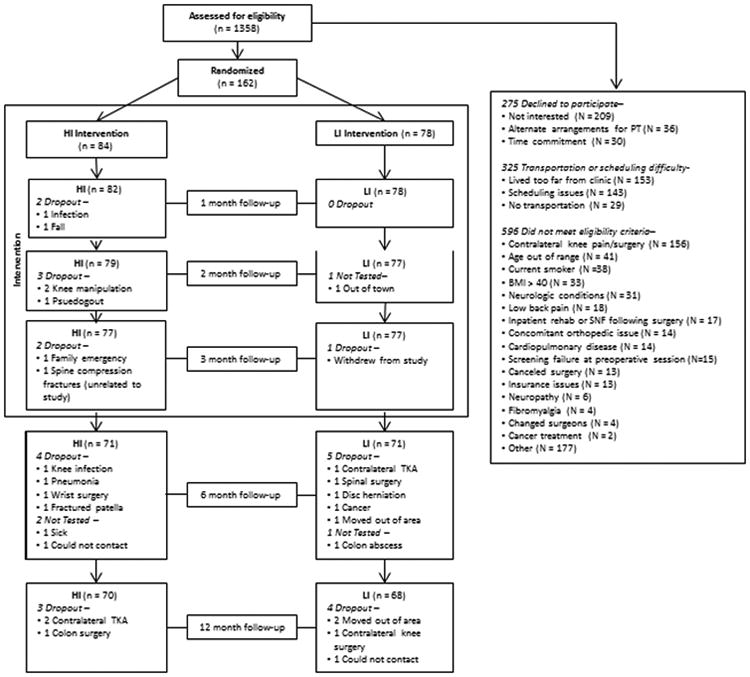
Table 1. Baseline characteristics.
| Characteristics | HI Group N=84 | LI Group N= 78 |
|---|---|---|
| Sex – Men, no. (%) | 39 (46) | 34 (44) |
| Age (years) | 63 (8) | 64 (7) |
| BMI (kg/m2) | 31 (5) | 30 (5) |
| Stair Climbing Test (s) | 17.20 (8.64) | 16.41 (7.99) |
| Timed-Up-and-Go Test (s) | 9.00 (2.91) | 8.87 (2.46) |
| 6-minute Walk Test (m) | 455 (106) | 466 (99) |
| WOMAC | 34 (13) | 33 (15) |
| SF-12 Physical Component Scale | 36 (9) | 37 (9) |
| SF-12 Mental Component Scale | 54 (9) | 54 (10) |
| Knee Extension (°) | 1 (4) | 0 (4) |
| Knee Flexion (°) | 126 (10) | 126 (11) |
| Quadriceps Strength (Nm/kg) | 1.18 (0.54) | 1.24 (0.49) |
| Hamstring Strength (Nm/kg) | 0.73 (0.32) | 0.75 (0.29) |
| Quadriceps Activation (%) | 70.9 (16.8) | 72.3 (14.2) |
All values are mean ± standard deviation except for sex which is reported in number of individuals and percent. Negative values of knee extension represent hyperextension. HI=High-intensity group. LI= Low-intensity group. BMI=body mass index. WOMAC=Western Ontario and McMaster Universities Osteoarthritis Index. SF-12=Short-form 12.
At the 3-month time point, 91% of the HI group and 99% of the LI group had completed the intervention and follow-up testing. At the 12-month time point, 83% of the HI group and 87% of the LI group had completed follow-up testing.
Outcome measures
The change from baseline in primary and secondary outcomes and the difference between groups at 3 months are shown in Table 2. Outcomes by group on all measures over time are shown in Table 3.
Table 2. Adjusted mean differences between groups in change from baseline at 3 months.
| Outcome | HI Group Mean (SEM) | LI Group Mean (SEM) | Point Estimate (95% CI) | p-value |
|---|---|---|---|---|
| Stair Climbing Test (s) | -3.89 (0.35) | -3.28 (0.36) | -0.61 (-1.56, 0.35) | 0.21 |
| Timed-Up-and-Go Test (s) | -1.35 (0.14) | -1.01 (0.14) | -0.34 (-0.71, 0.04) | 0.08 |
| 6-minute Walk Test (m) | 38.83 (7.18) | 23.39 (7.48) | 15.45 (-4.51, 35.40) | 0.13 |
| WOMAC | -19.60 (1.02) | -19.48 (1.05) | -0.12 (-2.94, 2.70) | 0.93 |
| SF-12 Physical Component Scale | 9.82 (0.93) | 6.80 (0.99) | 3.02 (0.39, 5.65) | 0.02 |
| SF-12 Mental Component Scale | 2.56 (0.76) | 3.57 (0.80) | -1.00 (-3.14, 1.14) | 0.36 |
| Knee Extension (°) | -0.61 (0.30) | -0.35 (0.31) | -0.26 (-1.09, 0.56) | 0.53 |
| Knee Flexion (°) | -1.93 (0.93) | -2.10 (0.96) | 0.17 (-2.40, 2.73) | 0.90 |
| Quadriceps Strength (Nm/kg) | 0.02 (0.04) | -0.05 (0.04) | 0.08 (-0.03, 0.18) | 0.14 |
| Hamstrings Strength (Nm/kg) | 0.03 (0.02) | -0.00 (0.02) | 0.03 (-0.03, 0.09) | 0.28 |
| Quadriceps Activation (%) | 11.70 (1.53) | 8.52 (1.60) | 3.18 (-1.07, 7.43) | 0.14 |
Reported means are change from baseline adjusting for baseline, sex, and clinical site. Negative values of knee extension represent hyperextension. HI=High-intensity group. LI= Low-intensity group. WOMAC=Western Ontario and McMaster Universities Osteoarthritis Index. SF-12=Short-form 12.
Table 3. Adjusted mean outcomes by group over time.
| Time Point | Baseline | 1 Month | 2 Months | 3 Months | 6 month | 12 month | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Outcome | HI Group N Mean (SD) |
LI Group N Mean (SD) |
HI Group N Mean (SD) |
LI Group N Mean (SD) |
HI Group N Mean (SD) |
LI Group N Mean (SD) |
HI Group N Mean (SD) |
LI Group N Mean (SD) |
HI Group N Mean (SD) |
LI Group N Mean (SD) |
HI Group N Mean (SD) |
LI Group N Mean (SD) |
| Stair Climbing Test (s) | 84 17.20 (8.64) | 78 16.41 (7.99) | 82 24.93 (12.39) | 78 24.42 (8.51) | 79 15.16 (5.78) | 77 15.27 (4.67) | 77 13.02 (4.62) | 77 13.60 (3.58) | 71 11.78 (4.29) | 71 12.15 (3.30) | 70 11.40 (3.62) | 67 11.77 (3.15) |
| Timed-up- and-Go Test (s) | 84 9.00 (2.91) | 78 8.87 (2.46) | 82 10.84 (4.16) | 78 10.48 (2.60) | 79 8.36 (2.42) | 77 8.27 (1.67) | 77 7.58 (1.82) | 77 7.98 (1.58) | 71 7.33 (1.60) | 71 7.48 (1.45) | 71 7.36 (1.77) | 67 7.44 (1.50) |
| 6-minute Walk Test (m) | 84 454.6 (105.7) | 77 466.5 (98.7) | 82 392.4 (100.4) | 78 374.4 (87.33) | 79 467.7 (96.6) | 77 465.6 (84.3) | 77 493.7 (92.4) | 76 478.7 (82.7) | 71 520.3 (91.1) | 71 511.7 (77.7) | 69 531.7 (98.9) | 67 513.6 (78.4) |
| WOMAC | 84 34.24 (13.15) | 77 33.32 (15.00) | 78 29.27 (11.64) | 76 30.13 (12.30) | 77 19.34 (10.56) | 74 19.57 (11.24) | 72 14.49 (8.98) | 75 14.55 (8.38) | 66 8.97 (7.27) | 67 10.60 (9.45) | 62 6.69 (7.75) | 62 7.16 (6.28) |
| S-12 PCS | 83 36.12 (9.44) | 74 36.50 (8.75) | 78 33.23 (8.81) | 73 33.07 (7.83) | 76 40.63 (8.01) | 75 39.15 (8.72) | 75 45.92 (7.96) | 75 43.09 (9.40) | 71 50.84 (6.23) | 68 49.02 (7.37) | 67 51.59 (8.33) | 61 50.07 (7.16) |
| SF-12 MCS | 83 54.15 (9.49) | 74 53.64 (9.81) | 78 51.83 (9.99) | 73 50.51 (9.59) | 76 56.30 (8.74) | 75 56.69 (8.50) | 75 56.73 (7.29) | 75 57.05 (6.86) | 71 55.76 (7.26) | 68 56.64 (6.20) | 67 55.76 (6.48) | 61 57.83 (3.58) |
| Knee Extension (°) | 84 0.69 (3.97) | 78 0.15 (3.69) | 82 1.83 (2.91) | 78 2.45 (2.60) | 79 0.85 (2.92) | 77 0.82 (2.25) | 77 -0.09 (2.97) | 77 0.06 (2.37) | 71 -1.38 (1.66) | 71 -0.90 (2.62) | 71 -2.18 (2.43) | 67 -1.76 (2.28) |
| Knee Flexion (°) | 84 125.54 (10.24) | 78 125.76 (10.95) | 82 108.10 (15.12) | 78 110.83 (10.81) | 79 119.25 (10.75) | 77 120.10 (9.38) | 77 123.79 (9.10) | 77 123.71 (8.97) | 71 127.10 (6.57) | 71 127.45 (7.88) | 71 129.28 (8.89) | 67 128.27 (8.61) |
| Quadriceps Strength (Nm/kg) | 84 1.18 (0.54) | 78 1.24 (0.49) | 81 0.75 (0.32) | 77 0.80 (0.34) | 78 1.07 (0.38) | 77 1.07 (0.38) | 77 1.21 (0.42) | 76 1.15 (0.40) | 71 1.35 (0.46) | 71 1.35 (0.40) | 70 1.42 (0.47) | 67 1.43 (0.44) |
| Hamstrings Strength (Nm/kg) | 84 0.73 (0.32) | 78 0.75 (0.29) | 81 0.56 (0.24) | 77 0.57 (0.22) | 78 0.68 (0.25) | 77 0.70 (0.23) | 77 0.76 (0.28) | 76 0.74 (0.26) | 71 0.80 (0.29) | 71 0.80 (0.27) | 70 0.84 (0.31) | 67 0.85 (0.29) |
| Quadriceps Activation (%) | 74 70.86 (16.80) | 71 72.27 (14.17) | 68 72.45 (17.02) | 62 73.14 (20.25) | 66 80.65 (13.60) | 64 80.34 (16.96) | 67 82.77 (10.78) | 63 79.94 (13.78) | 61 80.87 (12.01) | 62 82.92 (9.55) | 62 83.39 (11.73) | 59 83.73 (10.12) |
| PASE | 84 150.77 (96.32) | 76 153.84 (97.21) | 77 83.42 (55.80) | 75 76.25 (48.15) | 76 136.53 (90.63) | 74 131.96 (80.03) | 75 168.51 (103.36) | 75 162.48 (86.87) | 63 169.59 (80.67) | 60 171.98 (81.12) | 45 208.23 (89.51) | 47 166.48 (74.74) |
All values are adjusted for baseline, sex, and clinical site. Negative values of knee extension represent hyperextension. HI=High-intensity group. LI= Low-intensity group. WOMAC=Western Ontario and McMaster Universities Osteoarthritis Index. SF-12=Short-form 12. PASE=Physical Activity Scale for the Elderly.
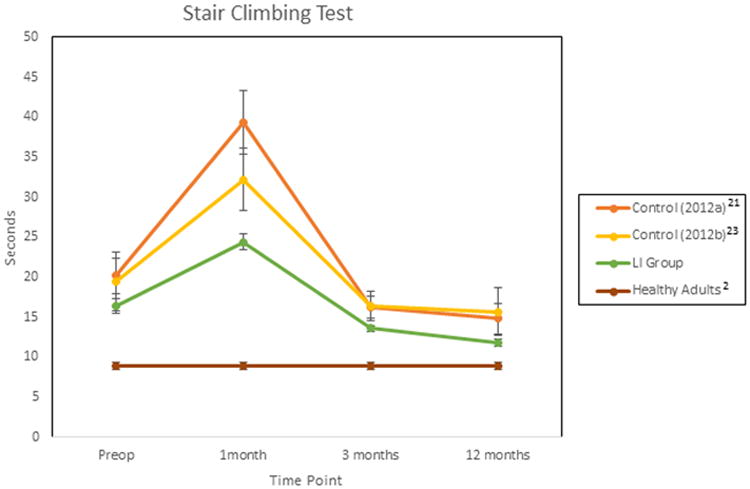
Primary outcome
There were no differences between groups in SCT change from baseline at the 3-month time point (p=0.21, 95% CI: -1.56, 0.35). Furthermore, there were no differences between groups on SCT performance at any time point (all p > 0.05). Both groups recovered to baseline SCT performance by the 2-month time point (p>0.05). By 12 months, SCT performance improved from baseline by 5.42 sec in the HI group (p <0.001, 95% CI: -7.03, -3.81) and 4.36 sec in the LI group (p <0.001, 95% CI: -6.01, -2.70).
Missing data
The primary analysis evaluated the 3-month change from baseline in an ANCOVA model, where the outcome is not defined when either baseline or a 3-month outcome is missing. Only 8 participants did not provide 3-month data (7 HI, 1 LI). As a sensitivity analysis, conclusions based on a longitudinal model, using all available data, were compared to the conclusions drawn from the ANCOVA using 154 complete cases; they were not different.
Secondary outcomes
There were no differences between groups in changes from baseline to 3 months on the TUG, 6MW, WOMAC, MCS, knee ROM, strength, or quadriceps activation (all p>0.05). The HI group had a 3-point greater improvement from baseline compared to the LI group on the PCS (p=0.02, 95% CI: 0.39, 5.65). However, this was not significant in the longitudinal model (p=0.06). There were no differences between groups on the TUG, WOMAC, MCS, PCS, knee ROM, strength or quadriceps activation at 1, 2, 6, and 12 months (all p>0.05). The HI group walked 29 meters farther on the 6MW test at 1-month compared to the LI group (p=.002, 95% CI: 11, 47), but distances were similar at all other time points (p>0.05). The WOMAC and quadriceps activation recovered to baseline performance in both groups by 1-month (both p>0.05). The TUG, 6MW, PCS, and MCS recovered to baseline levels in both groups by 2 months (all p>0.05). Knee ROM and quadriceps and hamstring strength recovered to baseline levels in both groups by 3 months (all p>0.05). By 12 months, outcomes on the 6MW, TUG, WOMAC, PCS, quadriceps and hamstring strength, and quadriceps activation had improved beyond baseline performance (all p<0.05). In a sensitivity analysis, the effect of home exercise adherence was not associated with the outcomes (p>0.05), but PASE activity was associated with SCT outcomes at 1 and 3 months (p=0.03 and 0.06 respectively) and quadriceps strength at 3 months (p=0.05). Adding the PASE to the outcomes models did not change the conclusions regarding group differences.
Adherence
Therapist treatment adherence with the intervention protocol was 96.4 ± 3.5% (mean ± sd) for the HI group and 96.8 ± 3.1% for the LI group. There was no difference between groups for therapist treatment adherence (p=0.46, 95% CI: -1.4, 0.7). Patient HEP adherence was 76 ± 0.2 % for the HI group and 83 ± 0.2 % for the LI group. Home exercise program adherence was significantly different between groups with the HI group completing 7.7% less of their assigned home exercises (p=0.04, 95% CI: -14.9, -0.5). There was no difference between groups at any time point in the PASE (all p >0.05).
Adverse events
A total of 7 adverse events occurred in the HI group (8.3% of participants) and 8 adverse events occurred in the LI group (10.2% of participants) during the intervention (Table 4). There was no difference between groups in the frequency of musculoskeletal injuries, knee ROM limitation, knee manipulation, or falls (all p>0.05).
Table 4. Adverse events by group.
| Adverse Events | HI Group (n=84) | LI Group (n=78) | p-value |
|---|---|---|---|
| Musculoskeletal Injuries (n) | 0 | 1 | 0.48 |
| Restricted Knee ROM (n) | 3 | 3 | 1.00 |
| Knee Manipulation (n) | 3 | 1 | 0.62 |
| Falls (n) | 1 | 3 | 0.35 |
| Total | 7 | 8 | 0.78 |
HI=High-intensity. LI=Low-intensity
Discussion
The HI program was safe to utilize in individuals after TKA. However, it did not lead to superior results compared to the LI program in the short or long term. Failure of the HI intervention to achieve superior outcomes compared to the LI intervention as hypothesized could be related to several key factors. The first factor to consider is that both the HI program and LI program were progressive in nature and it is possible that the loads imposed by the LI exercise program were similar to the average loads imposed by the HI program depending on patient progression through the HI program. Because the programs were fundamentally different in terms of exercise selection, it is not possible to make a direct comparison between programs in terms of the absolute amount of work patients completed during clinical treatment. One of the key differences between the HI and LI programs was the inclusion of a PRE program in the HI group, which targeted lower extremity musculature. Jakobsen et al (8) found that the addition of a leg extension exercise and leg press exercise (both utilized in this study) did not improve outcomes compared to a program which did not utilize these exercises. The authors attributed the lack of effect to arthrogenic muscular inhibition (AMI) which is a decrease in the neural drive to the quadriceps muscle which prevents it from being fully activated. AMI has been linked to knee pain, swelling, inflammation, and structural damage all of which are present after TKA. (24) AMI may have prevented patients from achieving the necessary intensity needed to stimulate muscle hypertrophy and improve functional performance. Moreover, Hurley et al (25) reported that individuals who had large activation deficits following knee injury did not respond to intensive rehabilitation. In the current study, quadriceps activation levels in the HI group were 72% at one month and remained below normal (26) throughout the intervention time period. Decreased activation may have limited gains from PRE. Future research should examine how different levels of activation failure prior to and following TKA affect recovery, and if alternate intervention strategies, such as neuromuscular electrical stimulation, could be more effective for individuals with larger activation deficits in the initial postoperative period. Moreover, future studies will need to evaluate whether PRE utilized with a different dosage, intensity, and/or timing could lead to superior long-term results. For example, Bieler et al (27) recently demonstrated that a 12-week high-intensity resistance training program initiated 8 weeks after anterior cruciate ligament reconstruction led to superior results compared to a low-intensity program. Two trials are currently underway that are examining if a high-intensity PRE intervention delivered after the initial post-operative period after TKA is more effective at this time point. (28, 29)
A second factor to consider regarding the lack of difference in outcomes between interventions is the influence of care pathway on recovery. Both the HI and LI programs appeared to be superior to previous studies of individuals after TKA. Jakobsen et al (8) reported that knee extension strength decreased by 10.6% compared to preoperative levels and active knee flexion was 109° at 6 months in the progressive strength training group. In the current study, knee extension strength increased by 14.4% compared to preoperative levels and knee flexion was 127° at 6 months in the HI group. Functional performance on the 6MW test was similar between studies, but the Jakobsen study did not evaluate activities that demand greater quadriceps strength such as stair climbing.(31) Patients typically recover to baseline levels of function following TKA but do not improve beyond baseline performance.(2) In the current study, SCT, 6MW, and TUG tests all improved to significantly greater levels beyond pre-surgical levels. Comparing the SCT times and time course of recovery from the current control group (LI group) to prior control groups from our laboratory that had identical inclusion criteria and testing methods as the current study (21, 23) revealed substantial differences between groups (Figure 2 (Appendix E). On average, in the present study, SCT improved more quickly and to a greater extent. In the current study, subjects went directly from the acute setting to outpatient rehabilitation and were seen 3 times a week for 6 weeks and then 2 times a week for 5 weeks. In contrast, subjects in our previous studies were treated in the home health setting 3 times a week for 2 weeks and then in outpatient clinics 2 times a week for 6 weeks. Jakobsen et al also utilized a twice weekly dose for 8 weeks but delivered all care in the outpatient setting. Care pathways and volume of therapy have been shown to be related to outcomes following TKA. For example, Brennan et al (30) found that the number of days from inpatient discharge to outpatient therapy was significantly related to outcomes indicating greater time spent in the home health setting led to poorer outcomes. Additionally, they found that greater number of visits in outpatient therapy led to better pain and functional outcomes. Future studies should determine optimal care pathways for individuals after TKA and explore the impact of volume and timing on recovery.
Figure 2.
The final factor to consider is the impact of adherence on the results. Therapist adherence with the protocol was excellent, but home exercise adherence was 7.7% lower in the HI group than the LI group (p=0.04). Additionally, the PASE scores between groups should have differed in the initial post-operative periods (1 month and 2 months) because activity prescriptions were different between groups. However, PASE scores did not differ between groups throughout the intervention (p>0.05). This suggests that the LI group may have completed more home exercise and engaged in more physical activity than was prescribed, which may have reduced the observed differences between groups. In the sensitivity analysis, PASE activity was associated with SCT outcomes at 1 and 3 months (p=0.03 and 0.06 respectively) and quadriceps strength at 3 months (p=0.05). However, adding the PASE to the outcomes models did not change the conclusions regarding group differences. It should be noted that there is some question as to the validity of the PASE in individuals after TKA compared to accelerometers and that the PASE may not accurately quantify physical activity. (31) Future trials should utilize accelerometers to quantify activity levels in the perioperative period as well as to study the relationship between physical activity and the recovery of physical performance because information on this relationship is currently lacking.
A limitation of this study was that treating therapists could not be blinded to the interventions they were providing. However, steps were taken to minimize contamination across interventions. A secondary limitation was that treatment exposure could not be precisely quantified, except by the amount of therapy received, so the true extent to which the HI and LI approaches differed could not be determined.
In conclusion, the HI intervention was safe to utilize however it did not lead to superior outcomes compared to the LI intervention. The effectiveness of the HI intervention may have been limited by arthrogenic inhibition. Both the HI and LI interventions led to improved strength and functional performance in the long-term.
Significance and Innovations.
The high-intensity intervention was safe and did not lead to an increase in adverse events or compromise knee range of motion compared to the low-intensity intervention.
Arthrogenic muscular inhibition in the early postoperative period could have limited the efficacy of the progressive resistive exercise component.
This study utilized a higher volume of therapy delivered only in the outpatient setting and outcomes from both groups were superior to results in prior studies on rehabilitation after TKA.
Acknowledgments
We would like to acknowledge the following individuals for their contributions to this clinical trial: John Kittelson, Margaret Schenkman, Krista Sanchez, Roger Paxton, Josh Winters, Michelle Reynolds, Tawnya Downing, Brian Loyd, Allison Gustavson, Jennifer Palmer, Jennifer Ivey, Derick Levy, Lucas Armstrong, Kurt Schulze, Michelle Kochanek, Susan Geidt, Lisa Bradford, Casey McNitt, Susan Ducklow, Dan Hartman, Lindsay Fairchild, Karen Backstrom, Marisa Peyerl, Patrick Kollmyer, Kevin Johnson, Keri Windels, Casey Stoneberger, Mitzy Burden, Kendall Slutzky, Roseann Johnson, the Colorado Joint Replacement Staff, and the patient participants.
Grant Funding Sources: NIH R01-HD065900, Colorado CTSI (UL1 TR000154), NIH T32 AG00279, and the Foundation for Physical Therapy Promotion of Doctoral Studies (PODS) I and II Scholarships
Appendix A
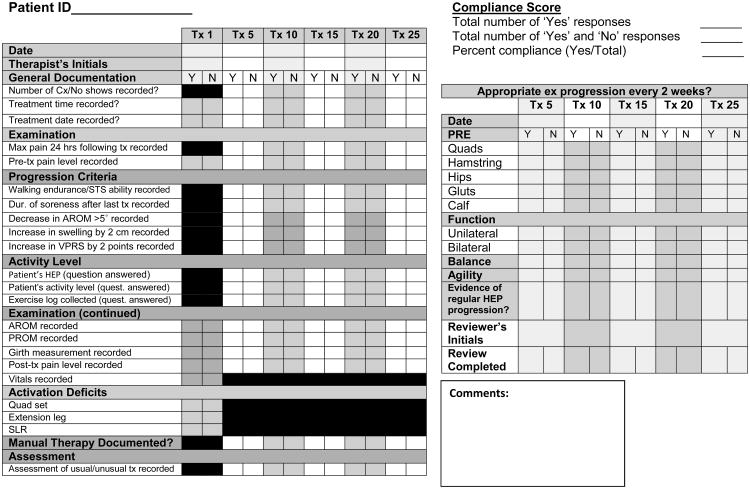
Therapist selection, training, and procedural reliability (continued) High Intensity Group Detailed Procedural Reliability Checklist.
Appendix B
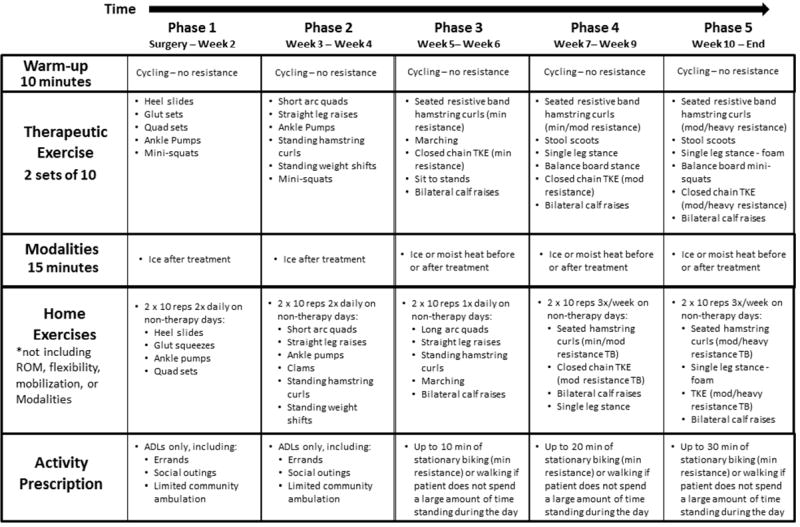
High Intensity Exercise Progression (performance-based).

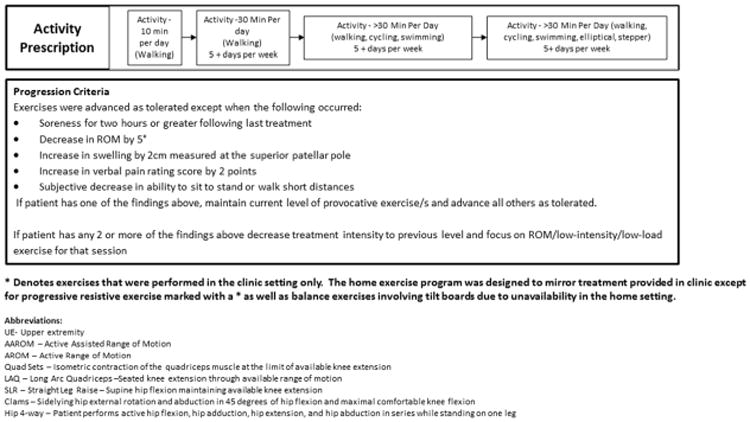
Appendix C
Low-Intensity Exercise Progression (time-based).
- Minimal resistance/Thin = Theraband brand Yellow
- Moderate resistance/Medium = Theraband brand Red
- Heavy resistance/Heavy = Theraband brand Green/Blue
Abbreviations:
Quad Sets– Isometric contraction of the quadriceps muscle at the limit of available knee extension
Shor Arc Quads –Supine active knee extension over a bolster
Straight Leg Raise–Supine hip flexion maintaining available knee extension
TKE –Terminal Knee Extensions- Standing resisted end range knee extension
Stool Scoots – Seated forward and backward propulsion on a stool designed to target hamstrings and quadriceps. Progressed by increasing resistance (friction from change in surface or with an elastic band)
Appendix D
Elements included in Both Programs.
| Common Clinical Treatments Between Both Programs | ||
|---|---|---|
|
| ||
| Manual Therapy | Education | Functional Training |
|
| ||
|
|
|
| *If indicated based upon clinical exam | ||
| Common Home Exercises Between Both Programs | |
|---|---|
|
| |
| Range of Motion | Flexibility |
|
|
|
| |
Appendix E
Baseline Characteristics of Current Control Group Compared to Prior Control Groups with Identical Inclusion Criteria.
| Characteristics | LI Group N= 78 | Control Group (2012a)21 N=31 | Control Group (2012b)23 N=22 |
|---|---|---|---|
| Sex – Men, no. (%) | 34 (44) | 15 (48) | 12 (55) |
| Age (years) | 64 (7) | 65 (8) | 64 (8) |
| BMI (kg/m2) | 30 (5) | 31 (4) | 31 (5) |
| Stair Climbing Test (s) | 16.4 (8.0) | 20.2 (12.3) | 19.4 (17.2) |
| 6-minute Walk Test (m) | 466 (99) | 434 (99) | 435 (148) |
| WOMAC | 33 (15) | 42 (14) | 41 (17) |
| Knee Extension (°) | 0 (4) | 1.5 (4.0) | 2 (8) |
| Knee Flexion (°) | 126 (11) | 119 (13) | 119 (16) |
| Quadriceps Strength (Nm/kg) | 1.24 (0.49) | 1.32 (0.49) | 1.37 (0.56) |
| Hamstring Strength (Nm/kg) | 0.75 (0.29) | 0.72 (0.26) | 0.80 (0.24) |
| Quadriceps Activation (%) | 72.3 (14.2) | 75.5 (19.0) | 74.6 (15.7) |
All values are mean ± standard deviation except for sex which is reported in number of individuals and percent. Negative values of knee extension represent hyperextension. LI= Low-intensity group. BMI=body mass index. WOMAC=Western Ontario and McMaster Universities Osteoarthritis Index.
Footnotes
Conflict of Interest Statement: None of the authors have any conflicts of interests to report
References
- 1.Kurtz S. Projections of Primary and Revision Hip and Knee Arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg Am. 2007;89:780. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Bade MJ, Kohrt WM, Stevens-Lapsley JE. Outcomes Before and After Total Knee Arthroplasty Compared to Healthy Adults. J Orthop Sports Phys Ther. 2010;40:559–567. doi: 10.2519/jospt.2010.3317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walsh M, Woodhouse LJ, Thomas SG, Finch E. Physical Impairments and Functional Limitations: A Comparison of Individuals 1 Year After Total Knee Arthroplasty With Control Subjects. Phys Ther. 1998;78:248–258. doi: 10.1093/ptj/78.3.248. [DOI] [PubMed] [Google Scholar]
- 4.Artz N, Elvers KT, Lowe CM, Sackley C, Jepson P, Beswick AD. Effectiveness of physiotherapy exercise following total knee replacement: systematic review and meta-analysis. BMC Musculoskelet Disord. 2015;16:15. doi: 10.1186/s12891-015-0469-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Petterson SC, Mizner RL, Stevens JE, Raisis L, Bodenstab A, Newcomb W, et al. Improved function from progressive strengthening interventions after total knee arthroplasty: A randomized clinical trial with an imbedded prospective cohort. Arthritis Rheum. 2009;61:174–183. doi: 10.1002/art.24167. [DOI] [PubMed] [Google Scholar]
- 6.Bade MJ, Stevens-Lapsley JE. Early high-intensity rehabilitation following total knee arthroplasty improves outcomes. J Orthop Sports Phys Ther. 2011;41:932–941. doi: 10.2519/jospt.2011.3734. [DOI] [PubMed] [Google Scholar]
- 7.Jakobsen TL, Husted H, Kehlet H, Bandholm T. Progressive strength training (10 RM) commenced immediately after fast-track total knee arthroplasty: is it feasible? Disabil Rehabil. 2012;34:1034–1040. doi: 10.3109/09638288.2011.629019. [DOI] [PubMed] [Google Scholar]
- 8.Jakobsen TL, Kehlet H, Husted H, Petersen J, Bandholm T. Early progressive strength training to enhance recovery after fast-track total knee arthroplasty: a randomized controlled trial. Arthritis Care Res. 2014;66:1856–1866. doi: 10.1002/acr.22405. [DOI] [PubMed] [Google Scholar]
- 9.Hengeveld E. Maitland's Peripheral Manipulation: Management of Neuromusculoskeletal Disorders. 5. Edinburgh: Churchill Livingstone; 2013. [Google Scholar]
- 10.Frost H, Lamb SE, Robertson S. A randomized controlled trial of exercise to improve mobility and function after elective knee arthroplasty. Feasibility, results and methodological difficulties. Clin Rehabil. 2002;16:200–209. doi: 10.1191/0269215502cr483oa. [DOI] [PubMed] [Google Scholar]
- 11.Moffet H, Collet JP, Shapiro SH, Paradis G, Marquis F, Roy L. Effectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: a single-blind randomized controlled trial1. Arch Phys Med Rehabil. 2004;85:546–556. doi: 10.1016/j.apmr.2003.08.080. [DOI] [PubMed] [Google Scholar]
- 12.Kramer JF, Speechley M, Bourne R, Rorabeck C, Vaz M. Comparison of clinic- and home-based rehabilitation programs after total knee arthroplasty. Clin Orthop. 2003:225–234. doi: 10.1097/01.blo.0000063600.67412.11. [DOI] [PubMed] [Google Scholar]
- 13.Minns Lowe CJ, Barker KL, Dewey M, Sackley CM. Effectiveness of physiotherapy exercise after knee arthroplasty for osteoarthritis: systematic review and meta-analysis of randomised controlled trials. BMJ. 2007;335:812. doi: 10.1136/bmj.39311.460093.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB. Does total knee replacement restore normal knee function? Clin Orthop. 2005:157–165. doi: 10.1097/01.blo.0000150130.03519.fb. [DOI] [PubMed] [Google Scholar]
- 15.Kennedy DM, Stratford PW, Wessel J, Gollish JD, Penney D. Assessing stability and change of four performance measures: a longitudinal study evaluating outcome following total hip and knee arthroplasty. BMC Musculoskelet Disord. 2005;6:3. doi: 10.1186/1471-2474-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39:142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 17.Steffen TM, Hacker TA, Mollinger L. Age- and Gender-Related Test Performance in Community-Dwelling Elderly People: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and Gait Speeds. Phys Ther. 2002;82:128–137. doi: 10.1093/ptj/82.2.128. [DOI] [PubMed] [Google Scholar]
- 18.Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 20.Norkin CC, White DJ. Measurement of Joint Motion : A Guide to Goniometry, 4th Edition. 4. Philadelphia: F.A. Davis Company; 2009. [Google Scholar]
- 21.Stevens-Lapsley JE, Balter JE, Wolfe P, Eckhoff DG, Kohrt WM. Early Neuromuscular Electrical Stimulation to Improve Quadriceps Muscle Strength After Total Knee Arthroplasty: A Randomized Controlled Trial. Phys Ther. 2012;92:210–226. doi: 10.2522/ptj.20110124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Washburn RA, Smith KW, Jette AM, Janney CA. The physical activity scale for the elderly (PASE): Development and evaluation. J Clin Epidemiol. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 23.Stevens-Lapsley JE, Bade MJ, Shulman BC, Kohrt WM, Dayton MR. Minimally Invasive Total Knee Arthroplasty Improves Early Knee Strength But Not Functional Performance: A Randomized Controlled Trial. J Arthroplasty. 2012;27:1812–1819.e2. doi: 10.1016/j.arth.2012.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rice DA, McNair PJ. Quadriceps Arthrogenic Muscle Inhibition: Neural Mechanisms and Treatment Perspectives. Semin Arthritis Rheum. 2010;40:250–266. doi: 10.1016/j.semarthrit.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 25.Hurley MV, Jones DW, Newham DJ. Arthrogenic quadriceps inhibition and rehabilitation of patients with extensive traumatic knee injuries. Clin Sci Lond Engl 1979. 1994;86:305–310. doi: 10.1042/cs0860305. [DOI] [PubMed] [Google Scholar]
- 26.Roos MR, Rice CL, Connelly DM, Vandervoort AA. Quadriceps muscle strength, contractile properties, and motor unit firing rates in young and old men. Muscle Nerve. 1999;22:1094–1103. doi: 10.1002/(sici)1097-4598(199908)22:8<1094::aid-mus14>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 27.Bieler T, Aue Sobol N, Andersen LL, Kiel P, Løfholm P, Aagaard P, et al. The Effects of High-Intensity versus Low-Intensity Resistance Training on Leg Extensor Power and Recovery of Knee Function after ACL-Reconstruction. BioMed Res Int. 2014;2014:1–11. doi: 10.1155/2014/278512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Piva SR, Moore CG, Schneider M, Gil AB, Almeida GJ, Irrgang JJ. A randomized trial to compare exercise treatment methods for patients after total knee replacement: protocol paper. BMC Musculoskelet Disord. 2015;16:303. doi: 10.1186/s12891-015-0761-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin CWC, March L, Crosbie J, Crawford R, Graves S, Naylor J, et al. Maximum recovery after knee replacement--the MARKER study rationale and protocol. BMC Musculoskelet Disord. 2009;10:69. doi: 10.1186/1471-2474-10-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brennan GP, Fritz JM, Houck LT, CKM, Hunter SJ. Outpatient Rehabilitation Care Process Factors and Clinical Outcomes Among Patients Discharged Home Following Unilateral Total Knee Arthroplasty. J Arthroplasty. 2015;30:885–890. doi: 10.1016/j.arth.2014.12.013. [DOI] [PubMed] [Google Scholar]
- 31.Bolszak S, Casartelli NC, Impellizzeri FM, Maffiuletti NA. Validity and reproducibility of the Physical Activity Scale for the Elderly (PASE) questionnaire for the measurement of the physical activity level in patients after total knee arthroplasty. BMC Musculoskelet Disord. 2014;15:1. doi: 10.1186/1471-2474-15-46. [DOI] [PMC free article] [PubMed] [Google Scholar]