Abstract
An 81‐year‐old female patient was admitted to our institute because of abnormal X‐ray results. Chest computed tomography showed a 7.7 × 5.3 cm mass located in the left lower lobe and multiple swollen lymph nodes. 18F‐fluorodeoxyglucose‐positron emission tomography indicated high standard uptake values in the mass and swollen lymph nodes. The patient was diagnosed with stage cT3N2M0‐IIIA squamous cell carcinoma. Although the patient had multiple lymph node metastases and severe obstructive pulmonary function, four cycles of platinum doublet chemotherapy were initially performed and no side effect greater than grade 3 was experienced. As the lung cancer was downstaged to ycT2aN0M0‐IB and pulmonary function had improved, a bronchodilating preparation, an uneventful left lower lobectomy, and a lymphadenectomy were performed. The patient was discharged 39 days after surgery and exhibited good health for a year at pathological stage ypT1aN0M0‐IA (Ef2).
Keywords: Chemotherapy, octogenarian, salvage treatment
Introduction
Several phase III randomized trials have demonstrated favorable results of salvage surgery after chemotherapy for advanced N2‐stage IIIA primary lung cancer compared with surgery alone.1, 2 Radical surgery for lung cancer in octogenarians has increasingly been performed recently in Japan.3 We report a case of successful salvage surgery after chemotherapy in an octogenarian cN2‐stage IIIA primary lung cancer patient.
Case report
An 81‐year‐old female patient with good performance status and without signs of senility was admitted as a result of an abnormal chest X‐ray, which showed a mass over 7 cm in diameter in the left lower field (Fig 1a). Chest computed tomography (CT) indicated swelling in multiple lymph nodes and 18F‐fluorodeoxyglucose‐positron emission tomography (FDG‐PET) displayed high standard uptake values (Fig 2a,b). A diagnosis of stage cT3N2M0‐IIIA primary squamous cell lung cancer was made (Fig 3a). Because of the multiple lymph node metastases (numbers 7, 10, and 11) and severe obstructive pulmonary function (vital capacity 1.69L [74.1%], forced expiratory volume in 1 second [FEV 1] 870 mL, FEV 1/forced vital capacity [FVC] 55.4%), four cycles of chemotherapy (carboplatin AUC 5, 290 mg/body day 1, tegafur‐gimeracil‐oteracil potassium [S‐1], 80 mg/body days 1–14) were performed each month and no side effects over grade 3 were observed. After chemotherapy, the main tumor had shrunk to 4.7 × 2.6 cm and the size and shape of the lymph nodes had decreased to within normal range. FDG‐PET showed diminished standard uptake values, resulting in stage ycT2aN0M0‐IB (Figs 1b, 2c,d). Good physical capacity was maintained and respiratory function was improved with a bronchodilating preparation (vital capacity 2.37L [106.8%], FEV 1 1220 mL, FEV1/FVC 56.0%); therefore, a left lower lobectomy, and a lymphadenectomy were performed uneventfully. Pathological findings revealed that the viable tumor was 1.4 cm in diameter (Ef2), staged as ypT1aN0M0‐IA (Fig 3b–d). Although the ambulatory patient was discharged 39 days after surgery because of rehabilitation and therapy for allergic bronchopulmonary aspergillosis, she was good in health with the same pretreatment and preoperative performance status, and did not experience recurrence from initial therapy for over a year.
Figure 1.
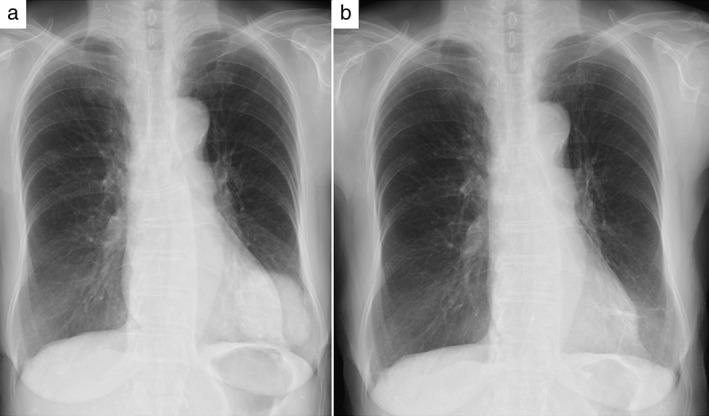
(a) Pre‐chemotherapy chest X‐ray shows a mass in the left lower field. (b) Post‐chemotherapy chest X‐ray shows the reduced mass.
Figure 2.
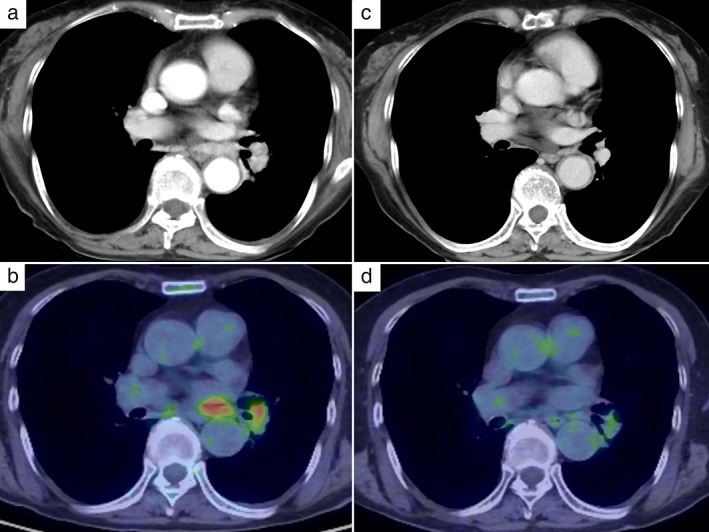
(a,b) Enhanced computed tomography and 18F‐fluorodeoxyglucose‐positron emission tomography pre‐chemotherapy shows multiple swollen hilar lymph nodes and high standard uptake values. (c,d) Computed tomography and 18F‐fluorodeoxyglucose‐positron emission tomography post‐chemotherapy shows reduced lymph nodes and decreased standard uptake values.
Figure 3.
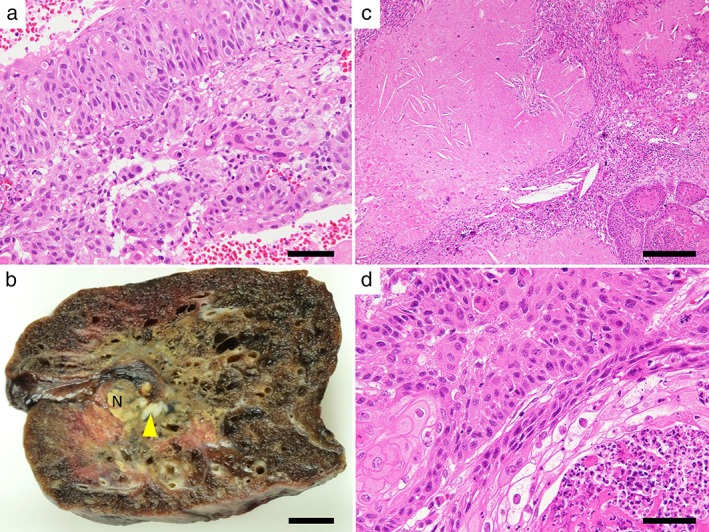
Macroscopic and microscopic view of the lung cancer. (a) A needle biopsy specimen before chemotherapy showed invasive keratinizing squamous cell carcinoma. Bar = 50 μm. (b) Resected specimen. The tumor had an irregular margin, approximately 1.4 × 1.0 cm, which mostly consisted of collapsed lung parenchyma with fibrosis and necrosis. The yellow granular appearance is a result of tumor necrosis (N). Arrowhead indicates a small focus of residual tumor. Bar = 1 cm. (c) Tumor necrosis with cholesterin clefts and ghost cells. Bar = 200 μm. (d) Residual squamous cell carcinoma with neutrophil inflammation. Bar = 50 μm.
Discussion
The age of lung cancer patients has been higher on average recently, and in Japan, after consideration of comorbidity, performance status, and mental state, greater numbers of octogenarians have undergone radical surgery, similar to treatment methods applied to younger generations.3 Surgical morbidity, mortality, and five‐year overall survival rates for octogenarians have been reported as 8.4–38.0%, 1.1–3.6%, and 27.0–65.9%, respectively.4, 5, 6, 7, 8 In a meta‐analysis of six eligible randomized studies, Berghmans et al. reported that a combination of induction chemotherapy and surgery was favorable to surgery alone (hazard ratio 0.69, 95% confidence interval 0.57–0.84).9 In our case, chemoradiation therapy was initially considered, but was felt to be an excessive burden considering the patient's age and frailty; therefore, radiation therapy was not performed. If chemotherapy could not be completed, radiation therapy might be added, depending on the case. Yoshioka et al. reported that patients with squamous cell carcinoma experienced longer median overall survival in a carboplatin plus S‐1 group than in a carboplatin‐paclitaxel group (14.0 vs. 10.6 months).10 The former group had a significantly better level of quality of life compared with the latter, including elderly patients.11
Elderly patients, especially octogenarians, are generally excluded from chemotherapy because of safety, considering their frailty. Only a few reports have evaluated the use and response of chemotherapy in the elderly population.12 The European Organization for Research and Treatment of Cancer and International Society for Geriatric Oncology recommend the use of carboplatin‐based doublets in fit elderly patients.13 National Comprehensive Cancer Network (NCCN) guidelines recommend platinum‐doublet chemotherapy in patients with good performance status, regardless of age.14 In our case, chemotherapy was performed because of the patient's physical tolerability. After the chemotherapy proved effective and the patients’ respiratory function improved, curative surgery was performed without any complications. Selected physically tolerable octogenarians could undergo invasive therapy, as is usually applied to younger generations, which might gain acceptable results. Further study is required to elucidate the feasibility and short and long term results of salvage surgery after chemotherapy in greater numbers of octogenarians with lung cancer.
Disclosure
No authors report any conflict of interest.
References
- 1. Nagai K, Tsuchiya R, Mori T et al. A randomized trial comparing induction chemotherapy followed by surgery with surgery alone for patients with stage IIIA N2 non‐small cell lung cancer (JCOG 9209). J Thorac Cardiovasc Surg 2003; 125: 254–60. [DOI] [PubMed] [Google Scholar]
- 2. Depierre A, Milleron B, Moro‐Sibilot D et al. Preoperative chemotherapy followed by surgery compared with primary surgery in resectable stage I (except T1N0), II, and IIIa non‐small‐cell lung cancer. J Clin Oncol 2002; 20: 247–53. [DOI] [PubMed] [Google Scholar]
- 3. Committee for Scientific Affairs, The Japanese Association for Thoracic Surgery , Masuda M et al. Thoracic and cardiovascular surgery in Japan during 2012: Annual report by The Japanese Association for Thoracic Surgery. (Published erratum appears in Gen Thorac Cardiovasc Surg 2015; 63: 120–2.) Gen Thorac Cardiovasc Surg 2014; 62: 734–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Port JL, Kent M, Korst RJ et al. Surgical resection for lung cancer in the octogenarian. Chest 2004; 126: 733–8. [DOI] [PubMed] [Google Scholar]
- 5. Mun M, Kohno T. Video‐assisted thoracic surgery for clinical stage I lung cancer in octogenarians. Ann Thorac Surg 2008; 85: 406–11. [DOI] [PubMed] [Google Scholar]
- 6. Okami J, Higashiyama M, Asamura H et al. Pulmonary resection in patients aged 80 years or over with clinical stage I non‐small cell lung cancer: Prognostic factors for overall survival and risk factors for postoperative complications. J Thorac Oncol 2009; 4: 1247–53. [DOI] [PubMed] [Google Scholar]
- 7. Fanucchi O, Ambrogi MC, Dini P et al. Surgical treatment of non‐small cell lung cancer in octogenarians. Interact Cardiovasc Thorac Surg 2011; 12: 749–53. [DOI] [PubMed] [Google Scholar]
- 8. Hino H, Murakawa T, Ichinose J et al. Results of lung cancer surgery for octogenarians. Ann Thorac Cardiovasc Surg 2015; 21: 209–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Berghmans T, Paesmans M, Meert AP et al. Survival improvement in resectable non‐small cell lung cancer with (neo)adjuvant chemotherapy: Results of a meta‐analysis of the literature. Lung Cancer 2005; 49: 13–23. [DOI] [PubMed] [Google Scholar]
- 10. Yoshioka H, Okamoto I, Morita S et al. Efficacy and safety analysis according to histology for S‐1 in combination with carboplatin as first‐line chemotherapy in patients with advanced non‐small‐cell lung cancer: Updated results of the West Japan Oncology Group LETS study. Ann Oncol 2013; 24: 1326–31. [DOI] [PubMed] [Google Scholar]
- 11. Okamoto I, Yoshioka H, Morita S et al. Phase III trial comparing oral S‐1 plus carboplatin with paclitaxel plus carboplatin in chemotherapy‐naïve patients with advanced non‐small‐cell lung cancer: Results of a west Japan oncology group study. J Clin Oncol 2010; 28: 5240–6. [DOI] [PubMed] [Google Scholar]
- 12. Sim SH, Kim YJ, Kim SH et al. Current status of chemotherapy use and clinical outcome in octogenarians with advanced non‐small cell lung cancer. J Cancer Res Clin Oncol 2015; 141: 1073–81. [DOI] [PubMed] [Google Scholar]
- 13. Pallis AG, Gridelli C, Wedding U et al. Management of elderly patients with NSCLC; updated expert's opinion paper: EORTC Elderly Task Force, Lung Cancer Group and International Society for Geriatric Oncology. Ann Oncol 2014; 25: 1270–83. [DOI] [PubMed] [Google Scholar]
- 14. Ettinger DS, Akerley W, Borghaei H et al. Non‐small cell lung cancer, version 2.2013. J Natl Compr Cancer Netw 2013; 11: 645–53. [DOI] [PubMed] [Google Scholar]


