Abstract
Introduction: Periosteal releasing incision (PRI) is nearly always essential to advance the flap sufficiently for a tension-free flap closure in bone augmentation procedures. However, hematoma, swelling, and pain are recognized as the main consequences of PRI with scalpel. The aim of this case series was to investigate the effectiveness of laser-assisted PRI in guided bone regeneration (GBR) procedure. In addition, postoperative hematoma, swelling, and pain and implant success were assessed.
Methods: Seventeen patients needed GBR were included in this study. Diode laser (940 nm, 2 W, pulse interval: 1 ms, pulse length: 1 ms, contact mode, 400-μm fiber tip) was used in a contact mode to cut the periosteum to create a tension-free flap. Facial hematoma, swelling, pain, and the number of consumed nonsteroidal anti-inflammatory drugs (NSAIDs) were measured for the six postoperative days. Six months after implant loading, implant success was evaluated.
Results: Minimal bleeding was encountered during the procedure. A tension-free primary closure of the flap was achieved in all cases. The clinical healing of the surgical area was uneventful. None of the patients experienced hematoma, ecchymosis, or intense swelling after surgery. The mean value of maximum pain (visual analogue scale – VAS) was 20.59 ± 12.10 mm (mild pain). Patients did not need to use NSAID after four postoperative days. All implants were successful and functional and none of them failed after 6 months of implant loading.
Conclusion: This study revealed the effectiveness of laser-assisted PRI in GBR procedure. This technique was accompanied with minimal sequelae at the first postoperative week. All implants were successful and no complication was noted during the course of this study.
Keywords: Laser ablation, Alveolar Bone, Augmentation, Postoperative Pain, Edema, Hemorrhage
Introduction
Guided bone regeneration (GBR) is a well-established method to augment the alveolar bone before or during implant placement.1,2 Tension-free primary closure of soft tissue flap is a prerequisite for successful GBR.3-5 On the other hand, failure to maintain primary closure usually results in flap dehiscence and membrane exposure and may lead to reduced quantity and quality of the regenerated bone.6 Periosteal releasing incision (PRI) is the most common method to ensure tension-free primary closure. Using this incision protocol has several benefits including being straightforward, predictable, and easy.7 However, especially in cases with major flap advancement, PRI with scalpel is usually accompanied with excessive bleeding during the procedure. This occurrence might impair visualization of the surgical field or lead to displacement of bone graft particles. Incidence of advanced arterial bleeding is another problem associated with scalpel PRI that needs prompt intervention. Scalpel PRI results in significant postoperative patient morbidity, as well. Facial hematoma and swelling after surgery could have a negative effect on patient’s quality of life.5 Several methods have been proposed to reduce postoperative sequelae. However, most of these techniques did not show beneficial effects.8-12 Although administration of corticosteroids to control postoperative sequelae is popular,13 there are serious concerns about their adverse impacts. The most potential side effects of corticosteroids are adrenal suppression, osteonecrosis, impaired wound healing, and increased risk of postoperative infection.14,15 Furthermore, use of corticosteroids is contraindicated in patients with hypertension, liver disease, diabetes, and hypothyroidism. These problems hinder the routine administration of corticosteroids for prevention of postoperative sequelae.
Over the past years, research has been developed regarding various applications of laser in oral surgical procedures. Laser surgery provides some advantages compared to scalpel surgery. These include easy ablation, better hemostasis, decontamination, as well as less surgical and postoperative pain.
To our knowledge, no study has been published on the clinical use of laser for PRI during bone augmentation procedure. Therefore, this case-series study is designed to assess the effectiveness of laser-assisted PRI in GBR procedure. In addition, degree of postoperative sequelae is evaluated.
Methods
Seventeen patients (8 males and 9 females, 31 to 65 years of age) requiring lateral ridge augmentation in the anterior maxilla for placement of dental implants participated. One defect in each patient was treated using GBR procedure. The ethical committee of Tehran University of Medical Sciences approved the study protocol (approval number: 179328). The study was conducted in accordance with Helsinki Declaration adopted by the 18th World Medical Assembly, Helsinki, Finland, 1964, and as revised by the 64th World Medical Assembly, Fontaleza, Brazil, 2013. Healthy nonsmoker subjects were enrolled in this study. Patients with the following criteria were excluded: general contraindication for bone augmentation procedure, implant surgeries, or laser treatment, the presence of infection at the site of surgery, and existence of swelling or pain at the time of surgery. Prior to surgery, verbal and written informed consent was obtained from each patient. One experienced surgeon performed all surgical procedures. Safety procedures associated with eye protection, smoke evacuator systems, etc. were established. Protective eyewear were used by the patient, surgeon, and assistant. Under local anaesthesia, a full-thickness mid-crestal incision was created in the keratinized gingiva using surgical blade. Then, two vertical releasing incisions were made on the buccal aspect: one mesial and one distal to the field of surgery. A full-thickness flap was elevated to the anterior nasal spine. A 940 nm diode laser (GaAlAs, ezLase, Biolase technology; Irvine, CA, USA) comprising of a 400-μm disposable tip was used in a contact mode with a setting of 2 W in pulse mode (pulse interval: 1 ms; pulse length: 1 ms) to cut the periosteum and create a tension-free flap (Figure 1). Care was taken to avoid any laser irradiation to the bone by aiming the laser beam nearly parallel to the buccal bone. Saline-moistened gauze was used to remove the carbonized layer, as needed. Screws were used to create and maintain a sufficient space for osteogenesis. After placement of demineralized freeze-dried bone allografts (Cenoboneâ, Tissue Regeneration Corporation, Kish, Iran) and resorbable membrane(Cenodermâ, thickness: 2 mm, Tissue Regeneration Corporation, Kish, Iran), internal mattress sutures were used to allow clinically passive primary closure of the buccal flap. Then, continuous mattress suture was used to close the margins of the flap. Postoperative protocol consisted of administration of amoxicillin (500 mg; T.I.D; 7 days), along with a nonsteroidal anti-inflammatory drug (NSAID, Gelofen, 400 mg; Jabber Ebne Hayyan, Tehran, Iran), and 0.2% chlorhexidine digluconate mouthwash (B.I.D; 14 days). NSAID was prescribed immediately after surgery and then upon patient discretion. Patients were asked to record the number of NSAID capsules consumed every day.
Figure 1.
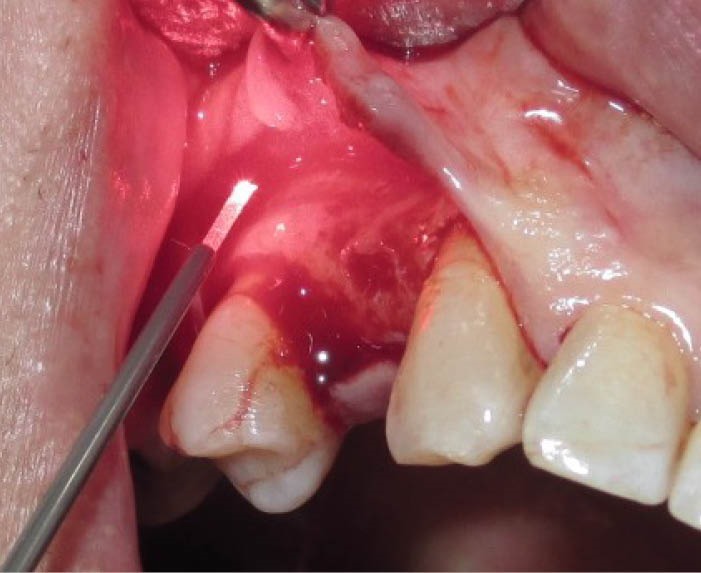
Periosteal Releasing Incision With Laser
An independent examiner assessed the degree of swelling and pain once daily for six postoperative days. All measurements were performed in the same time every day. Swelling on the operated side was graded as follows: 0 (none: no intraoral or extraoral swelling), 1 (mild: intraoral swelling confined to the surgical field), 2 (moderate: extraoral swelling in the surgical zone), or 3 (intense: extraoral swelling spreading beyond the surgical zone).16 Postoperative pain was measured using a visual analogue scale (VAS) ranging from zero for “no pain” to 100 mm for “the worst possible pain.” Pain intensity was classified into four categories: No pain (0 on the VAS), mild (1-35 mm), mild to moderate (36-50 mm), moderate (51-75 mm), and severe (76-100 mm).17
After 6 months, titanium implants (Implantium; Dentium, Suwon, Korea) were placed in the grafted sites. In order to verify whether there was any clinically detectable influence of laser on bone formation, success of dental implants were evaluated 6 months after loading based on Albrektsson criteria. These include lack of implant mobility as well as absence of x-ray radiolucency, and signs and symptoms such as pain, infections, neuropathies, and paresthesia.
Results
Minimal bleeding was observed during performing PRI with laser. A primary tension-free closure of the flap was obtained in all cases. The clinical healing of the surgical area was uneventful in all patients. Wound dehiscence or infection was not observed in any of the cases. Table 1 demonstrates the values of swelling and pain and the number of consumed nonsteroidal anti-inflammatory drugs (NSAIDs) in the first postoperative week. None of the patients experienced postoperative intense swelling (Table 2). The most degree of swelling was encountered in the third postoperative days (1.47 ± 0.50), which was subsequently subsided by the sixth day (Figure 2A).
Table 1. Degrees of Swelling and Pain and Number of Consumed NSAID During 6 Days After Surgery .
| Patient No. | Swelling | Pain (VAS) | No. of Consumed NASID | |||||||||||||||
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | |
| 1 | 1 | 1 | 1 | 1 | 1 | 0 | 34 | 25 | 15 | 10 | 0 | 0 | 2 | 1 | 1 | 0 | 0 | 0 |
| 2 | 1 | 1 | 1 | 0 | 0 | 0 | 30 | 21 | 10 | 5 | 0 | 0 | 2 | 1 | 2 | 0 | 0 | 0 |
| 3 | 1 | 2 | 2 | 1 | 1 | 0 | 27 | 10 | 5 | 5 | 0 | 0 | 2 | 1 | 1 | 0 | 0 | 0 |
| 4 | 1 | 2 | 2 | 2 | 2 | 1 | 43 | 19 | 15 | 9 | 0 | 0 | 3 | 2 | 2 | 2 | 0 | 0 |
| 5 | 1 | 2 | 2 | 2 | 1 | 0 | 35 | 15 | 5 | 5 | 5 | 0 | 3 | 1 | 1 | 1 | 0 | 0 |
| 6 | 1 | 1 | 1 | 1 | 0 | 0 | 40 | 20 | 20 | 10 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 |
| 7 | 1 | 2 | 1 | 1 | 0 | 0 | 20 | 10 | 4 | 0 | 0 | 0 | 1 | 1 | 1 | 2 | 0 | 0 |
| 8 | 1 | 1 | 2 | 1 | 1 | 0 | 25 | 5 | 3 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| 9 | 1 | 1 | 1 | 1 | 0 | 0 | 20 | 10 | 5 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 |
| 10 | 1 | 1 | 1 | 1 | 0 | 0 | 15 | 5 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| 11 | 1 | 1 | 2 | 2 | 1 | 0 | 12 | 5 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 |
| 12 | 1 | 2 | 2 | 1 | 1 | 1 | 10 | 5 | 0 | 0 | 0 | 0 | 4 | 1 | 0 | 0 | 0 | 0 |
| 13 | 1 | 1 | 2 | 1 | 0 | 0 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 14 | 1 | 1 | 2 | 1 | 1 | 0 | 7 | 7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 15 | 1 | 1 | 1 | 1 | 0 | 0 | 5 | 5 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| 16 | 1 | 1 | 1 | 1 | 0 | 0 | 10 | 6 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| 17 | 1 | 1 | 1 | 1 | 0 | 0 | 12 | 5 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
Abbreviations: NSAID, non-steroidal anti-inflammatory drug; VAS, visual analogue scale.
Table 2. Distribution of Swelling and Pain Scores During 6 days After Surgery .
| Swelling(n) | VAS(n) | ||||||||
| None | Mild | Moderate | Intense | 0 | 1-35 | 36-50 | 51-75 | 76-100 | |
| Day 1 | 0 | 17 | 0 | 0 | 0 | 15 | 2 | 0 | 0 |
| Day 2 | 0 | 12 | 5 | 0 | 1 | 16 | 0 | 0 | 0 |
| Day 3 | 0 | 9 | 8 | 0 | 7 | 10 | 0 | 0 | 0 |
| Day 4 | 1 | 13 | 3 | 0 | 11 | 6 | 0 | 0 | 0 |
| Day 5 | 9 | 7 | 1 | 0 | 16 | 1 | 0 | 0 | 0 |
| Day 6 | 15 | 2 | 0 | 0 | 17 | 0 | 0 | 0 | 0 |
Abbreviations: n, number of patients; VAS, visual analogue scale.
Figure 2.
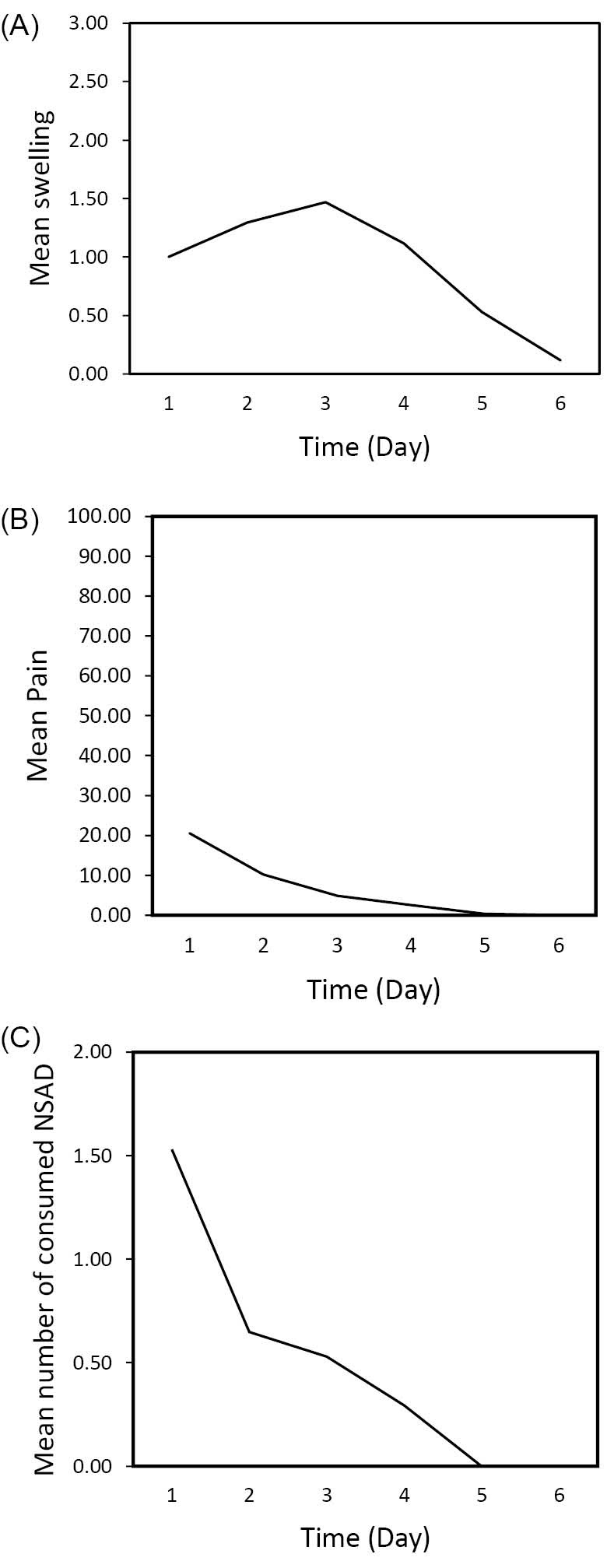
Mean Values of Postoperative Swelling (A), Pain (B), and Number of Consumed NSAIDs (C).
Due to administration of NSAID immediately after surgery, none of the patients experienced pain at that time. Maximal pain levels were noticed on the first postoperative day that was gradually resolved by the sixth day. The mean value of VAS at the first postoperative day was 20.59 ± 12.10 mm, which was considered as mild pain (Figure 2B).
The mean number of NSAIDs used by patients at the first postoperative day was 1.53 ± 1.04. None of the patients needed NSAID after the fourth day (Figure 2C).
All implants were successful and functional and none of them failed after 6 months of implant loading.
Discussion
To our knowledge, this is the first report on the utilization of laser for flap advancement in GBR procedure. The results of this clinical study showed significant effectiveness of diode laser for performing PRI without intra and postoperative complications. Using this device was accompanied with little bleeding during incision. This would be helpful, since direct visualization of the surgical field is important to ensure effectiveness of PRI. Moreover, postoperative sequelae like swelling and pain were slight to mild. Noteworthily, no negative impact on implant survival was observed in this study.
The effectiveness of PRI has been widely documented in the literature.3,7 The results of a study revealed that double vertical incisions could advance the flap length by 124.2% while after performing PRI, flap advancement of up to 171.3% was obtained. Therefore, PRI was considered as the key determinant for significant and predictable increased flap extension.18
Electric coagulator has been suggested as a tool to control the advanced bleeding during PRI.7,19 However, it should be noted that electrocautery causes intense heat-coagulation. The potential risk of thermal damage to the underlying bone and consequently incidence of bone necrosis and delayed wound healing is the major concern related to electrocautery.20
Over the last few years, a number of studies demonstrated the positive effects of low-level laser therapy (LLLT) on reduction of postoperative discomfort.10,12 Ozturan et al used Neodymium-Doped Yttrium Aluminium Garnet (Nd:YAG) laser (1064 nm, 0.5 W, 8 J/cm2, and 60 seconds, immediately after surgery) for LLLT after maxillary sinus lift procedure. They found that swelling and the oral health-related quality of life was significantly improved in the LLLT group compared to the control group. However, Nd:YAG laser was not effective in reducing pain level, when the above-mentioned parameters were used.21
Currently, laser-assisted surgery is a common practice for soft and hard tissue management. Due to several advantages, diode lasers are increasingly preferred within applications in soft tissue surgeries. Many surgeons prefer , and lower costs.22 Other beneficial properties of diode lasers include relative ease of soft tissue ablation, bactericidal effects, minimal wound contraction, and little postoperative pain.20
At the 940 nm wavelength, the diode laser is strongly absorbed in hemoglobin and water. Therefore, it could cut or ablate soft tissue and achieve sufficient hemostasis with minimum carbonization. Moreover, contact mode laser results in enhanced surgical precision and tactile feedback. Importantly, this wavelength provides adequate depth to seal the injured lymphatic vessels and nerve endings.23 It is assumed that this property might result in minimal postoperative edema and pain.24 We used laser in the pulsed mode, which prevents rapid temperature rise in the target tissue and provides time to the tissue to cool down. Modest collateral tissue damage as well as possible biostimulatory effect of laser in the surrounding tissue lead to proper wound healing.25
Yilmaz et al used diode laser (810 nm) for performing vestibular releasing incision during laterally positioned flap in root coverage procedure and reported positive clinical and aesthetic outcomes.26
In the present study, none of the patients experienced ecchymosis or intense swelling during the first postoperative week. Moreover, 8 out of 17 participants did not have extraoral swelling in this period. Kim et al reported that even without vertical releasing incisions, performing scalpel PRI resulted in some degree of facial swelling during the 2 weeks after bone augmentation surgery.19 Minimal postoperative edema was perhaps due to sealing of the lymphatic vessels by the laser.27,28
None of the patients included in this study perceived moderate or severe pain during the first postoperative week. Ogata et al used PRI with a scalpel during bone augmentation procedure, and reported that the average postoperative pain score in the first postoperative week was 37.5 mm.5 In the same period, the mean pain score perceived by the patients in this study was 6.42 mm.
Moreover, the results of this study demonstrated minimal need for NSAIDs in the postoperative period. Minimal pain experienced by the patients in this study could be due to the assumption that nerve endings seal during tissue incision by laser.29 Another reason for this finding could be due to the photobiomodulatory effect of laser. It is believed that during high-level laser irradiation, low-level laser is penetrated and scattered within the tissues surrounding the target zone and induce photobiostimulation.30
In the present report, no case with implant failure was observed. This could indicate that laser-assisted GBR did not have negative influence on the viability of the grafted sites.
The main limitation of this study is the lack of a control group. Future randomized clinical trials with longer follow-up are needed to verify the results of this study.
In conclusion, this investigation revealed that utilization of diode laser (940 nm) for performing PRI during GBR can be useful as it prevents excessive intraoperative bleeding and provides a good visualization of the surgical field. Moreover, postoperative swelling and pain of the patients undergone laser-assisted PRI was minimal.
Ethical Considerations
This study have been approved by ethical committee of Tehran University of Medical Sciences approved the study protocol (Approval number: 179328)
Conflict of Interests
The authors declare that they have no conflict of interest.
Acknowledgments
This study was fully supported by laser research center of dentistry, Tehran University of Medical Sciences. The authors thank for great help of this research center.
Please cite this article as follows: Moslemi N, Khorsand A, Torabi S, Shahnaz A, Soleimani Shayesteh Y, Fekrazad R. Periosteal releasing incision with diode laser in guided bone regeneration procedure: a case series. J Lasers Med Sci. 2016;7(4):259-264. doi:10.15171/jlms.2016.46.
References
- 1.Zitzmann NU, Scharer P, Marinello CP. Long-term results of implants treated with guided bone regeneration: a 5-year prospective study. Int J Oral Maxillofac Implants. 2001;16:355–366. [PubMed] [Google Scholar]
- 2.Blanco J, Alonso A, Sanz M. Long-term results and survival rate of implants treated with guided bone regeneration: a 5-year case series prospective study. Clin Oral Implants Res. 2005;16:294–301. doi: 10.1111/j.1600-0501.2005.01106.x. [DOI] [PubMed] [Google Scholar]
- 3.Greenstein G, Greenstein B, Cavallaro J, Elian N, Tarnow D. Flap advancement: practical techniques to attain tension-free primary closure. J Periodontol. 2009;80:4–15. doi: 10.1902/jop.2009.080344. [DOI] [PubMed] [Google Scholar]
- 4.Lee A, Brown D, Wang HL. Sandwich bone augmentation for predictable horizontal bone augmentation. Implant Dent. 2009;18:282–90. doi: 10.1097/id.0b013e3181ad8c6c. [DOI] [PubMed] [Google Scholar]
- 5.Ogata Y, Griffin TJ, Ko AC, Hur Y. Comparison of double-flap incision to periosteal releasing incision for flap advancement: a prospective clinical trial. Int J Oral Maxillofac Implants. 2013;28:597–604. doi: 10.11607/jomi.2714. [DOI] [PubMed] [Google Scholar]
- 6.Shaban M. Soft tissue closure over immediate implants: Classification and review of surgical techniques. Implant Dent. 2004;13:33–41. doi: 10.1097/01.id.0000116370.67314.c0. [DOI] [PubMed] [Google Scholar]
- 7.Romanos GE. Periosteal releasing incision for successful coverage of augmented sites A technical note. J Oral Implantol. 2010;36:25–30. doi: 10.1563/AAID-JOI-D-09-00068. [DOI] [PubMed] [Google Scholar]
- 8.Al-Khateeb TH, Nusair Y. Effect of the proteolytic enzyme serrapeptase on swelling, pain and trismus after surgical extraction of mandibular third molars. Int J Oral Maxillofac Surg. 2008;37:264–268. doi: 10.1016/j.ijom.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 9.Rana M, Gellrich NC, Joos U, Piffko J, Kater W. 3D evaluation of postoperative swelling using two different cooling methods following orthognathic surgery: a randomised observer blind prospective pilot study. Int J Oral Maxillofac Surg. 2011;40:690–696. doi: 10.1016/j.ijom.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 10.Gasperini G, Rodrigues de Siqueira IC, Rezende Costa L. Does low-level laser therapy decrease swelling and pain resulting from orthognathic surgery? Int J Oral Maxillofac Surg. 2014;43:868–873. doi: 10.1016/j.ijom.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 11.Klongnoi B, Kaewpradub P, Boonsiriseth K, Wongsirichat N. Effect of single dose preoperative intramuscular dexamethasone injection on lower impacted third molar surgery. Int J Oral Maxillofac Surg. 2012;41:376–379. doi: 10.1016/j.ijom.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Landucci A, Wosny AC, Uetanabaro LC, Moro A, Araujo MR. Efficacy of a single dose of low-level laser therapy in reducing pain, swelling, and trismus following third molar extraction surgery. Int J Oral Maxillofac Surg. 2016;45:392–398. doi: 10.1016/j.ijom.2015.10.023. [DOI] [PubMed] [Google Scholar]
- 13.Alcantara CE, Falci SG, Oliveira-Ferreira F, Santos CR, Pinheiro ML. Pre-emptive effect of dexamethasone and methylprednisolone on pain, swelling, and trismus after third molar surgery: a split-mouth randomized triple-blind clinical trial. Int J Oral Maxillofac Surg. 2014;43:93–98. doi: 10.1016/j.ijom.2013.05.016. [DOI] [PubMed] [Google Scholar]
- 14.Waldron NH, Jones CA, Gan TJ, Allen TK, Habib AS. Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis. Br J Anaesth. 2013;110:191–200. doi: 10.1093/bja/aes431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Esen E, Tasar F, Akhan O. Determination of the anti-inflammatory effects of methylprednisolone on the sequelae of third molar surgery. J Oral Maxillofac Surg. 1999;57:1201–6. doi: 10.1016/s0278-2391(99)90486-x. [DOI] [PubMed] [Google Scholar]
- 16.Penarrocha M, Garcia B, Marti E, Balaguer J. Pain and inflammation after periapical surgery in 60 patients. J Oral Maxillofac Surg. 2006;64:429–433. doi: 10.1016/j.joms.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 17.Miser AW, Dothage JA, Wesley RA, Miser JS. The prevalence of pain in a pediatric and young adult cancer population. Pain. 1987;29:73–83. doi: 10.1016/0304-3959(87)90180-1. [DOI] [PubMed] [Google Scholar]
- 18.Park JC, Kim CS, Choi SH, Cho KS, Chai JK, Jung UW. Flap extension attained by vertical and periosteal-releasing incisions: a prospective cohort study. Clin Oral Implants Res. 2012;23:993–998. doi: 10.1111/j.1600-0501.2011.02244.x. [DOI] [PubMed] [Google Scholar]
- 19.Kim Y, Kim TK, Leem DH. Clinical Study of a Flap Advancement Technique Without Vertical Incision for Guided Bone Regeneration. Int J Oral Maxillofac Implants. 2015;30:1113–1118. doi: 10.11607/jomi.3586. [DOI] [PubMed] [Google Scholar]
- 20.Ishikawa I, Aoki A, Takasaki AA, Mizutani K, Sasaki KM, Izumi Y. Application of lasers in periodontics: true innovation or myth? Periodontology 2000. 2009;50:90–126. doi: 10.1111/j.1600-0757.2008.00283.x. [DOI] [PubMed] [Google Scholar]
- 21.Ozturan S, Sirali A, Sur H. Effects of Nd:YAG laser irradiation for minimizing edema and pain after sinus lift surgery: randomized controlled clinical trial. Photomed Laser Surg. 2015;33:193–199. doi: 10.1111/j.1600-0757.2008.00283.x. [DOI] [PubMed] [Google Scholar]
- 22.El-Kholey KE. Efficacy and safety of a diode laser in second-stage implant surgery: a comparative study. Int J Oral Maxillofac Surg. 2014;43:633–638. doi: 10.1016/j.ijom.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 23.Parker S. Verifiable CPD paper: Laser-tissue interaction. Br Dent J. 2007;202(2):73–81. doi: 10.1038/bdj.2007.24. [DOI] [PubMed] [Google Scholar]
- 24.Sotoode SM, Azimi S, Taheri SA. et al. Diode laser in minor oral surgery: a case series of laser removal of different benign exophytic lesions. J Lasers Med Sci. 2015;6:133–138. doi: 10.15171/jlms.2015.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yogesh Doshi MS, Khandge N, Sanghavi A. Advantages of diode laser (940 nm) over surgical blade in management of ankyloglossia: a case report. J Oral Laser Appl. 2010;10:165–169. [Google Scholar]
- 26.Yilmaz E, Ozcelik O, Comert M. et al. Laser-assisted laterally positioned flap operation: a randomized controlled clinical trial. Photomed Laser Surg. 2014;32:67–74. doi: 10.15171/jlms.2015.08. [DOI] [PubMed] [Google Scholar]
- 27.Coleton S. Lasers in surgical periodontics and oral medicine. Dent Clin North Am. 2004;48:937–962. doi: 10.15171/jlms.2015.08. [DOI] [PubMed] [Google Scholar]
- 28.Parker S. Lasers and soft tissue: ‘loose’ soft tissue surgery. Br Dent J. 2007;202(4):185–191. doi: 10.1038/bdj.2007.128. [DOI] [PubMed] [Google Scholar]
- 29.Elanchezhiyan S, Renukadevi R, Vennila K. Comparison of diode laser-assisted surgery and conventional surgery in the management of hereditary ankyloglossia in siblings: a case report with scientific review. Lasers Med Sci. 2013;28:7–12. doi: 10.1007/s10103-010-0761-5. [DOI] [PubMed] [Google Scholar]
- 30.Aleksic V, Aoki A, Iwasaki K. et al. Low-level Er:YAG laser irradiation enhances osteoblast proliferation through activation of MAPK/ERK. Lasers Med Sci. 2010;25:559–569. doi: 10.1007/s10103-010-0761-5. [DOI] [PubMed] [Google Scholar]


