Abstract
Background and Aims:
Dexamethasone as an adjuvant to bupivacaine for supraclavicular brachial plexus (SCBP) block prolongs motor and sensory blockade. However, the effect of dexamethasone (8 mg) when added to levobupivacaine has not been well studied. This study was conducted to find out analgesic efficacy of dexamethasone as adjuvant to levobupivacaine in SCBP block.
Methods:
Ultrasound- guided SCBP block was given to sixty patients, randomly assigned into two groups. Group S (thirty patients) received 2 mL normal saline with 25 mL levobupivacaine (0.5%) and Group D (thirty patients) received 2 mL of dexamethasone (8 mg) with 25 mL of levobupivacaine (0.5%), respectively. Time for the first rescue analgesia, number of rescue analgesics required in 24 h and different block characteristics was assessed. Chi-square test and Student's t-test were used for statistical analysis.
Results:
Time for request of the first rescue analgesia was 396.13 ± 109.42 min in Group S and 705.80 ± 121.46 min in Group D (P < 0.001). The requirement for rescue analgesics was more in Group S when compared to Group D. The onset of sensory and motor block was faster in Group D when compared to Group S. The mean duration of sensory and motor block was significantly longer in Group D than Group S.
Conclusion:
The addition of dexamethasone to levobupivacaine in SCBP blockade prolonged time for first rescue analgesia and reduced the requirement of rescue analgesics with faster onset and prolonged duration of sensory and motor block.
Key words: Dexamethasone, levobupivacaine, supraclavicular brachial plexus
INTRODUCTION
Peripheral neural blockade is now a well-accepted component of post-operative pain management. Ultrasound-guided supraclavicular brachial plexus (SCBP) block provides not only intraoperative anaesthesia and post-operative analgesia but also reduce many complications like intravascular injection.[1]
Levobupivacaine has less systemic toxicity than bupivacaine.[2] Its limiting factors are late onset and limited duration of analgesia even when used with adjuvants like opioids that produce opioid-related side effects.[3] Studies have shown that dexamethasone can prolong the effect of regional anaesthesia.[4] Dexamethasone as an adjuvant may avoid opioid-related side effects. There is very limited literature available regarding the use of dexamethasone as an adjuvant to levobupivacaine. Hence, the study was designed to assess the analgesic efficacy of dexamethasone as an adjuvant to levobupivacaine in ultrasound-guided SCBP block.
The primary aim of the present study was to determine whether dexamethasone (8 mg) as adjuvant to levobupivacaine in ultrasound-guided SCBP block would delay the need for rescue analgesia and the number of rescue analgesia requirements in first 24 h after surgery. Effects on sensory or motor block characteristics were the secondary aims of the study.
METHODS
A randomised prospective study was conducted in a tertiary care hospital from January 2016 to June 2016 after approval of the Institutional Ethics Committee. Patients with American Society of Anesthesiologist Grade I or II status, between 16–65 years of either gender, posted for upper limb surgery were included in the present study. Patients who refused to give informed consent, obese and short neck patients, patients with coagulopathy, neuropathy or local infection at the site for block, those with a history of allergy to the study drug or of drug abuse and an anticipated operative time more than 2 h were excluded from the study.
Pre-anaesthetic evaluation was performed on the day before surgery. The procedure of block along with possible complications was explained to the patients, and written informed consent was obtained. All patients were given oral alprazolam 0.5 mg and ranitidine 150 mg on the night before the surgery, and were fasting overnight.
Sixty patients were divided randomly into two groups (Group S, n = 30 and Group D, n = 30) using a computer-generated programme. Assigned random group was enclosed in a sealed envelope to ensure concealment of allocation sequence. The anaesthesiologist who was not involved in the study, opened the envelope in operation theatre and prepared the drug accordingly. Observations were done by the anaesthesiologist who was blinded to the drug. Heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP), peripheral oxygen saturation (SpO2) and 3 lead electrocardiogram were monitored.
The SCBP block was performed using a portable ultrasound machine (Sonosite Micromaxx, Sonosite Inc., WA, USA) with a linear ultrasound transducer (8–13 MHz). Under all aseptic precautions with the patient in supine position, the affected arm adducted and head turned to the contralateral side, the brachial plexus was visualised by putting the transducer in the supraclavicular fossa behind the middle third of the clavicle. The plexus either appeared as a cluster of grapes (5–6 hypoechoic circles) or as 3 hypoechoic circles with the hyperechoic outer ring, located lateral and superior to subclavian artery between anterior and middle scalene muscles. The drug solution, based on group allocation was injected after negative aspiration to avoid accidental intravascular needle puncture and the spread of drug was observed in tissue planes. Distension of the brachial plexus sheath was considered as an indication of correct needle placement. Group S (30) received 25 mL 0.5% levobupivacaine plus 2 mL normal saline, and Group D (30) received 25 mL 0.5% levobupivacaine plus 2 mL Dexamethasone (8 mg) around the brachial plexus. Midazolam 0.05 mg/kg intravenous was administered after the block was given.
Sensory blockade was assessed by pinprick method at each minute after completion of the block. Block of the median and ulnar nerves were assessed by testing the palmar surfaces of the index and little finger, respectively, and the dorsal surface of thumb was used to test block of the radial nerve. Grading of sensory block was done as;[5] Grade 0: Normal sensation to pin prick. Grade 1: Dull sensation to pinprick. Grade 2: No sensation felt. Onset of sensory block was defined as the time interval between drug administration and onset of Grade 1 sensory block in the hand (3 nerve distribution). The full sensory block was defined as the complete loss of sensation to a pinprick. Duration of sensory block was defined as the time interval between the complete sensory block and the return of normal sensation.
Motor block was monitored by thumb adduction (ulnar nerve), thumb abduction (radial nerve), thumb opposition (median nerve) and flexion of elbow and pronation of forearm (musculocutaneous nerve) using a Lovett rating scale.[6] The onset of motor block was the time between completion of local anaesthetic injection and complete paralysis, and the duration of motor block was taken as the time interval from complete paralysis to complete recovery of motor function. The block was considered as failed block when at least two of the four nerves (radial, median, ulnar and musculocutaneous) were not affected even after 30 min after performing the block. As per complaint of surgeon and patient, the quality of the operative condition was monitored on the following scale: Grade 4: No complaint (excellent), Grade 3: Minor complaint (good), Grade 2: Complaint requiring analgesics (moderate) and Grade 1: Patient given general anaesthesia (unsuccessful).[5,6]
The performance of block, intra operative parameters and post-operative analgesia were monitored by an anaesthesiologist who was neither aware of group allocation nor involved in the drug preparation. Post-operative analgesia was monitored as per a numeric rating scale of 0–10 at every hour up to 24 hours.[6] If the numerical rating scale score was 5 or more, it was considered that analgesic action of the block had terminated, and injection tramadol 100 mg intravenously was given as rescue analgesia. Side effects such as nausea, vomiting, convulsion, dryness of mouth, respiratory problems, pneumothorax in intra-operative period and neuropathy in the post-operative period were noted. HR, SBP, DBP and SpO2 were recorded pre-operatively before drug administration, at 0 min (just after drug administration), 15 min, 30 min, 45 min, 60 min, 75 min, 90 min, 105 min, 120 min, 4 h, 8 h, 12 h and 24 h.
The mean onset time and duration of sensory and motor block were noted. The time for the first rescue analgesic, the total dose of rescue analgesic needed for first 24 h, all haemodynamic parameters (SBP, DBP, MAP and HR) and any other complication were also noted.
Sample size calculation was based on an initial pilot study involving ten patients with 'time needed for first rescue analgesic' as the primary end point of the study. Time to first analgesic request was 405.14 ± 110.35 min in levobupivacaine- saline group and 590.28 ± 115.64 min in levobupivacaine-dexamethasone group. With Ώ± error of 0.05 and power of the study (1− Ώ2) at 80%, to detect a minimum of 120 min difference in time needed for rescue analgesia between the two groups, the sample size was calculated to be approximately 28 in each group. We included thirty patients in each group to compensate for possible dropouts. The patients, who were part of the pilot study, were not included in the study. The patients' data and characteristics, the time of onset and duration of the block were categorised and analysed appropriately using student's unpaired t-test and Chi-square test. A P < 0.05 was considered as statistically significant and a P < 0.001 as statistically highly significant.
RESULTS
Block was successful in all the patients, and all the enrolled patients completed the study [Figure 1]. Demographic data such as age, sex, weight and duration of surgery between two groups were comparable [Table 1]. The request for first rescue analgesic was significantly earlier in Group S than Group D. [Table 2]. Figure 2 shows that in Group S, 80% of patients required three, and 20% of patients were given two rescue analgesic doses in the post-operative 24 h. In Group D, 60% of patients were given only one rescue analgesic dose and 30% of patients were given two, whereas only 10% of patients were given three rescue analgesic doses in the post-operative 24 h. This difference in both groups was statistically highly significant (P < 0.001).
Figure 1.
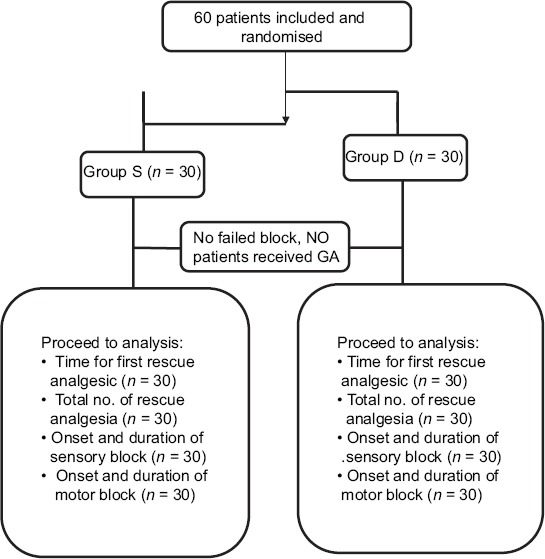
The patients enroled in the study and analysis
Table 1.
Demographic parameters
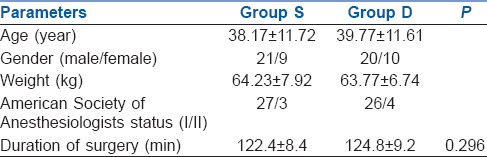
Table 2.
Brachial plexus block characteristics
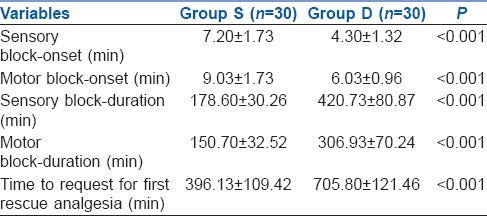
Figure 2.
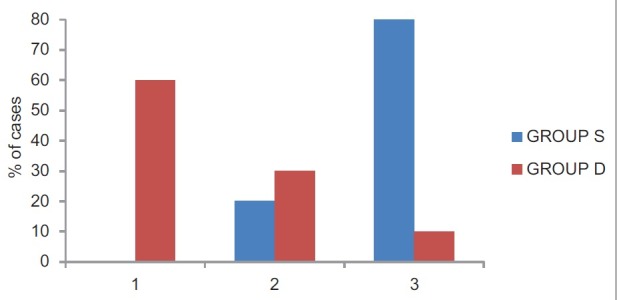
Number of rescue analgesics in post-operative for 24 h
In this study, the onset of motor and sensory block in Group S was delayed in comparison to Group D. This difference in both Group S and Group D was very highly significant (P < 0.001) [Table 2]. Duration of motor and sensory block in Group D was prolonged compared to Group S (P < 0.001) [Table 2].
There was no case of failed block or patchy block. None of the patients of either groups required supplemental analgesia or general anaesthesia. Qualities of the operative condition in both groups were excellent, and there was no statistically significant difference between two groups. Intra- and post-operative haemodynamic parameters were comparable between the two groups. There were no side effects during intra- and post-operative period.
DISCUSSION
While performing SCBP block by paraesthesia technique, many anaesthesiologists tend to use large volume (30–40 mL) of local anaesthetics to improve success rates and prolong sensory and motor block. However, this leads to complications such as phrenic nerve palsy and Horner's syndrome due to unusual spread, and also increases the chances of systemic local anaesthetic toxicity. Lower volume of local anaesthetics may produce either shorter duration of block or incomplete block. Ultrasound guided SCBP block enables adequate block with lower volume of local anaesthetic compared to blind techniques. Use of adjuvants such as dexamethasone may increase the duration of block without increasing the volume injected, and with minimal side effects.[7]
Many adjuvants to local anaesthetics such as clonidine, tramadol, dexmedetomidine and neostigmine have been studied in brachial plexus block, but each drug has its own side effects.[7] Recently, dexamethasone, a long-acting glucocorticoid has proven its efficacy as an adjuvant to local anaesthetics in brachial plexus block.[8] It produces vasoconstriction and reduces the absorption of local anaesthetics and thereby prolongs the action of local anaesthetics.[9] Many other studies reported the prolonged duration of sensory and motor block when dexamethasone was used as an adjuvant with bupivacaine and lignocaine in brachial plexus block, but they differed regarding the onset of sensory and motor block.[10,11,12,13] Effect of dexamethasone with bupivacaine was studied in interscalene block, and it was concluded that the sensory block was prolonged and use of opioid was reduced post-operatively using dexamethasone.[14] In our study we observed that adding dexamethasone (8 mg) to levobupivacaine not only delayed the time for the first rescue analgesic but also decreased the number of rescue analgesics required. In addition, there was early onset of sensory and motor effect, and also increased duration of block which might be due to the synergistic action of dexamethasone with levobupivacaine.
Low-dose dexamethasone (4 mg) was used as an adjuvant with (25 mL) levobupivacaine (0.5%) in SCBP block in a study concluded that it prolonged post-operative analgesia and delayed the first rescue analgesic request in comparison to levobupivacaine alone which was similar to our finding. However, in contrast to our study, it had no effect on the onset of block.[15] In a study comparing dexamethasone at different doses as an adjuvant to bupivacaine for SCBP block, it was observed that 1 mg and 2 mg of dexamethasone prolonged the sensory and motor block duration to same extent as 4 mg.[16] Addition of dexamethasone (8 mg) to 30 mL of ropivacaine (0.5%) in brachial plexus block prolonged motor and sensory blockade as compared to ropivacaine alone, but it had no effect on the onset of sensory and motor block.[17] A meta-analysis concluded that dexamethasone produced late onset of sensory and motor block with prolongation of motor block duration and that the smaller doses of dexamethasone (4-5mg) were as equally effective as higher doses of dexamethasone (8-10mg).[18] However, the meta-analysis did not analyse any study using dexamethasone (8 mg) with levobupivacaine in supraclavicular brachial plexus block. As far as time to first rescue analgesia was concerned, our study is in complete agreement with above studies.[15,16,17,18] but no agreement was found regarding the onset of block. In another study, the addition of 8 mg of dexamethasone to 30 mL of levobupivacaine reduced the onset of sensory and motor block and provided prolonged analgesia in supraclavicular brachial plexus block by paraesthesia technique.[19] In contrast to this study, 25 mL of levobupivacaine was deemed appropriate for our study in view of ultrasound guided SCBP block. In a comparative study of adjuvants such as midazolam and epinephrine, use of dexamethasone (8 mg) with bupivacaine (30 mL) not only produced rapid onset of sensory and motor block but also delayed the demand of rescue analgesia.[20] Both the above studies[19,20] were in complete agreement with ours. Studies were divided regarding the optimum dose of dexamethasone as an adjuvant to local anaesthetics and its impact on the onset of block. Furthermore, there were very few studies in the literature using 8 mg of dexamethasone with levobupivacaine in SCBP block. No significant side effects were reported in the literature using 8 mg of dexamethasone as an adjuvant in brachial plexus block. Hence, we have used 8 mg of dexamethasone to investigate its effect not only on duration but also on the onset of sensory and motor block.
Prolonged sensory and motor block following perineural administration of dexamethasone with (30–40 mL) of local anaesthetics may be due to the high volume of local anaesthetics.[21] In this study, we had used comparatively low volume (25 mL) of local anaesthetic in supraclavicular brachial plexus block suggesting that dexamethasone may have been responsible for the prolonged block
There are some concerns regarding the safety of perineural administration of dexamethasone. In animal studies on dexamethasone, blood flow to normal nerves was reduced for 4 h after topical application of intrafascicular injection of dexamethasone. This may produce harmful effects on nerve fibres, but there are no reports available regarding long-term effects on peripheral nerves.[22] The side effects associated with adjuvants such as clonidine, dexmedetomidine and opioids could be avoided using dexamethasone as an adjunct to levobupivacaine.[23] Systemic toxicity from a single dose of dexamethasone is unlikely. It is effective and widely administered intravenously by anaesthesiologists for prophylaxis against post-operative nausea and vomiting. Hence, dexamethasone may be a preferred adjuvant to levobupivacaine in comparison to others.
The limitation of the present study was that we did not study the incidence of steroid-induced hyperglycaemia and also long-term follow-up was not performed. Therefore, late onset neuropathy could not be detected. Hence, it is advisable to establish continuous follow-up for a longer period.
CONCLUSION
Dexamethasone (8 mg) when used as an adjuvant to 0.5% levobupivacaine for upper extremity surgeries under ultrasound-guided supraclavicular brachial plexus block delayed the time for the need of rescue analgesia and also decreased the dose requirement for the same. It produced faster onset of sensory and motor block and increased the duration of sensory and motor blockade.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Gupta K, Tiwari V, Gupta P, Pandey M, Singhol A, Shubham G, et al. Clonidine as adjunct for ultrasound guided supraclavicular brachial plexus block for upper extremity surgeries under tourniquet: A clinical study. J Anaesthesiol Clin Pharmacol. 2014;30:533–7. doi: 10.4103/0970-9185.142851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Movafegh A, Razazian M, Hajimaohamadi F, Meysamie A. Dexamethasone added to lidocaine prolongs axillary brachial plexus blockade. Anesth Analg. 2006;102:263–7. doi: 10.1213/01.ane.0000189055.06729.0a. [DOI] [PubMed] [Google Scholar]
- 3.Chen SY, Liu FL, Cherng YG, Fan SZ, Leighton BL, Chang HC, et al. Patient-controlled epidural levobupivacaine with or without fentanyl for post-cesarean section pain relief. Biomed Res Int. 2014;2014:965152. doi: 10.1155/2014/965152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cummings KC, 3rd, Napierkowski DE, Parra-Sanchez I, Kurz A, Dalton JE, Brems JJ, et al. Effect of dexamethasone on the duration of interscalene nerve blocks with ropivacaine or bupivacaine. Br J Anaesth. 2011;107:446–53. doi: 10.1093/bja/aer159. [DOI] [PubMed] [Google Scholar]
- 5.Tripathi A, Sharma K, Somvanshi M, Samal RL. A comparative study of clonidine and dexmedetomidine as an adjunct to bupivacaine in supraclavicular brachial plexus block. J Anaesthesiol Clin Pharmacol. 2016;32:344–8. doi: 10.4103/0970-9185.188819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Azimaraghi O, Marashi SM, Khazaei N, Pourhassan S, Movafegh A. The effect of adding sufentanil to 0.5% hyperbaric bupivacaine on duration of brachial plexus blockade in chronic opium abusers: A randomized clinical trial. Anesth Pain Med. 2015;5:e21960. doi: 10.5812/aapm.21960v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alarasan AK, Agrawal J, Choudhary B, Melhotra A, Uike S, Mukherji A. Effect of dexamethasone in low volume supraclavicular brachial plexus block: A double-blinded randomized clinical study. J Anaesthesiol Clin Pharmacol. 2016;32:234–9. doi: 10.4103/0970-9185.182108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Noss C, MacKenzie L, Kostash M. Dexamethasone- a promising adjuvant in brachial plexus anaesthesia? A systematic review. J Anesth Clin Res. 2014;5:421. [Google Scholar]
- 9.Bigat Z, Boztug N, Hadimioglu N, Cete N, Coskunfirat N, Ertok E. Does dexamethasone improve the quality of intravenous regional anesthesia and analgesia? A randomized, controlled clinical study. Anesth Analg. 2006;102:605–9. doi: 10.1213/01.ane.0000194944.54073.dd. [DOI] [PubMed] [Google Scholar]
- 10.Nigam R, Murthy M, Kosam D, Kujur AR. Efficacy of dexamethasone as an adjuvant to bupivacaine in supraclavicular brachial plexus block. J Evol Med Dent Sci. 2015;4:11157–63. [Google Scholar]
- 11.Biradar PA, Kaimar P, Gopalakrishna K. Effect of dexamethasone added to lidocaine in supraclavicular brachial plexus block: A prospective, randomised, double-blind study. Indian J Anaesth. 2013;57:180–4. doi: 10.4103/0019-5049.111850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saritas A, Sabuncu C. Comparison of clinical effects of prilocaine, dexamethasone added to prilocaine and levobupivacaine on brachial plexus block. J Pak Med Assoc. 2014;64:433–6. [PubMed] [Google Scholar]
- 13.Mamdouh LE, Ghada HA, Sherief ZI, Eldin AA, Tarek EA. Effect of addition of dexamethasone to low volumes of local anaesthetics for ultrasound-guided supraclavicular brachial plexus block. Menoufia Med J. 2015;28:928–34. [Google Scholar]
- 14.Vieira PA, Pulai I, Tsao GC, Manikantan P, Keller B, Connelly NR. Dexamethasone with bupivacaine increases duration of analgesia in ultrasound-guided interscalene brachial plexus blockade. Eur J Anaesthesiol. 2010;27:285–8. doi: 10.1097/EJA.0b013e3283350c38. [DOI] [PubMed] [Google Scholar]
- 15.Persec J, Persec Z, Kopljar M, Zupcic M, Sakic L, Zrinjscak IK, et al. Low-dose dexamethasone with levobupivacaine improves analgesia after supraclavicular brachial plexus blockade. Int Orthop. 2014;38:101–5. doi: 10.1007/s00264-013-2094-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu J, Richman KA, Grodofsky SR, Bhatt S, Huffman GR, Kelly JD, 4th, et al. Is there a dose response of dexamethasone as adjuvant for supraclavicular brachial plexus nerve block? A prospective randomized double-blinded clinical study. J Clin Anesth. 2015;27:237–42. doi: 10.1016/j.jclinane.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 17.Kumar S, Palaria U, Sinha AK, Punera DC, Pandey V. Comparative evaluation of ropivacaine and ropivacaine with dexamethasone in supraclavicular brachial plexus block for postoperative analgesia. Anesth Essays Res. 2014;8:202–8. doi: 10.4103/0259-1162.134506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knezevic NN, Anantamongkol U, Candido KD. Perineural dexamethasone added to local anesthesia for brachial plexus block improves pain but delays block onset and motor blockade recovery. Pain Physician. 2015;18:1–14. [PubMed] [Google Scholar]
- 19.Baloda R, Bhupal JP, Kumar P, Gandhi GS. Supraclavicular brachial plexus block with or without dexamethasone as an adjuvant to 0.5% levobupivacaine: A comparative study. J Clin Diagn Res. 2016;10:UC09–12. doi: 10.7860/JCDR/2016/18325.8048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El-Baradey GF, Elshmaa NS. The efficacy of adding dexamethasone, midazolam, or epinephrine to 0.5% bupivacaine in supraclavicular brachial plexus block. Saudi J Anaesth. 2014;8(Suppl 1):S78–83. doi: 10.4103/1658-354X.144083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Choi S, Rodseth R, McCartney CJ. Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: A systematic review and meta-analysis of randomized trials. Br J Anaesth. 2014;112:427–39. doi: 10.1093/bja/aet417. [DOI] [PubMed] [Google Scholar]
- 22.Mackinnon SE, Hudson AR, Gentili F, Kline DG, Hunter D. Peripheral nerve injection injury with steroid agents. Plast Reconstr Surg. 1982;69:482–90. doi: 10.1097/00006534-198203000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Tandoc MN, Fan L, Kolesnikov S, Kruglov A. Adjuvant dexamethasone with bupivacaine prolongs the duration of interscalene block: A prospective randomized trial. J Anaesth. 2011;25(5):704–09. doi: 10.1007/s00540-011-1180-x. [DOI] [PubMed] [Google Scholar]


