Abstract
Background:
Sepsis is the leading cause of mortality in the critically ill. Recently, it has been found in many studies that many trace elements and nutrients do have an effect on human body and if supplemented can improve the prognosis in patients with sepsis.
Aim and Objectives:
Primary objective: Whether low Vitamin D is associated with mortality. Secondary objective: To find out association of low Vitamin D levels and morbidity in terms of length of hospital and Intensive Care Unit (ICU) stay.
Subjects and Methods:
Following ethical approval, consent will be sought from either the patient or assent from a near relative. Successive patients admitted to the medical emergency and ICU at tertiary care health center who fulfill the following criteria for sepsis, within a 24 h time window, were included in the study.
Results:
Among 88 patients evaluated in our study 15 patients (18.2%) were found to have adequate Vitamin D levels and seven patients (8%) were found insufficient and rest 52 patients (73.9%) were found deficient in Vitamin D. Age of the patients ranged between 18 and 82 years with mean (±standard deviation) 45.02 ± 17.69 years. Mean Vitamin D level was found significantly higher among patients with positive outcome than those with unfavorable outcome (expiry) (t = 2.075, P = 0.04). On comparison of the length of hospital stay (morbidity) with Vitamin D levels, we found statistically significant inverse relation between Vitamin D levels and length of hospital stay.
Conclusion:
Vitamin D deficiency leads to increased risk of mortality in the critically ill along with prolonged hospital stay.
Keywords: Hospital stay, sepsis, Vitamin D deficiency
INTRODUCTION
Sepsis is the leading cause of mortality in the critically ill. Recent studies emphasize early classification and treatment is paramount to improving mortality rates.[1,2] Recently, it has been found in many studies that many trace elements and nutrients do have an effect on human body and if supplemented can improve the prognosis in patients with sepsis.[1,3] Although role of Vitamin D is vital in immune function and sepsis as suggested by many studies; this study is conducted to find out the correlation between Vitamin D and sepsis as well as to find out whether Vitamin D levels can be correlated with outcome of the patients in the form of mortality and discharge. This study is conducted also to find out whether levels of Vitamin D can be correlated with morbidity of the discharged patients in the form of hospital stay. The study also correlates levels of various sepsis biomarkers with Vitamin D levels to find out whether Vitamin D can be used as biomarker of sepsis.
SUBJECTS AND METHODS
The present study conducted in the Department of Medicine at tertiary care center in the Northern part of India, during 1 year from July 2013 to June 2014. Inclusion criteria: all adult patients admitted in Medical Emergency or in Intensive Care Unit (ICU) with features of sepsis, severe sepsis, or septic shock were enrolled. Exclusion criteria: pregnant and lactating mothers, postcardiopulmonary resuscitated patient, not giving consent, taking multivitamin, or food supplements which contain Vitamin D, malabsorption syndromes or patients with chronic diarrhea. Informed consent was taken from every patient before being included in the study. The study was approved by Local Ethical Committee.
Patient evaluation
Patients were evaluated on the basis of history, examination (general and systemic), and appropriate investigations were done (hemoglobin, total leukocyte count, differential leukocyte count, platelet count, hematocrit, fasting lipid profile, random blood sugar, pH, Na+, K+, ionic calcium, magnesium, phosphate, bicarbonate, serum urea, serum creatinine, glycated hemoglobin, fasting and postprandial blood sugar, liver function tests – serum bilirubin, serum glutamic oxaloacetic transaminases, serum glutamic pyruvic transaminases, serum protein, serum albumin, C-reactive protein (CRP), thyroid-stimulating hormone, T3, T4, serum lipase).
Additional tests were also done when needed like electrocardiography, to search for the source of infection (urine routine and microscopy and culture sensitivity, blood culture and sensitivity, sputum culture and sensitivity, X-ray chest). After initial patient evaluation and investigations, the patients were graded according to Glasgow coma scale (GCS) and Acute Physiology and Chronic Health Evaluation (APACHE) II scoring systems.
Statistical analysis
All categorical variables were expressed as percentages, and all continuous variables were expressed as mean ± standard deviation (SD). Categorical variables were compared using Fischer-exact test and Chi-square test, whichever is applicable. Continuous variables were compared using t-test and ANOVA as applicable. P <0.05 was considered statistically significant. Bivariate correlations were calculated using Pearson's correlation coefficient. Statistical analysis was performed using software SPSS version 17 (233, South Wacker Drive, 11th floor, Chicagon I)I.
RESULTS
A total of 91 patients were enrolled in the study, of which outcome could not be ascertained in 3 (3.3%). A total of 74 (81.3%) were discharged whereas 14 (15.4%) patients expired [Table 1].
Table 1.
Distribution of cases according to outcome (n=91)

Age of patients ranged from 18 to 82 years. Mean age of patients was 45.02 ± 17.69 years. Among patients who were discharged age of patients ranged from 18 to 82 years. Maximum were aged 20–30 years (21.6%) followed by those aged 51–60 years (20.3%), 31–40 years (18.9%), 41–50 years (8.1%), ≤20 years (8.1%), and >70 years (5.4%), respectively. Mean age of patients who were discharged was 45.26 ± 17.90 years [Table 2].
Table 2.
Age-wise distribution of cases with outcome (n=88)

Among patients who expired, age ranged from 18 to 70 years, maximum (n = 6; 42.9%) were aged 31–40 years followed by those aged 61–70 years (21.4%), ≤20 years and 51–60 years (14.3% each), and 21–30 years (7.1%). Mean age of patients who expired was 43.79 ± 17.13 years [Table 2]. Statistically, no significant association between age and outcome could be established (P = 0.326).
The majority of patients irrespective of outcome were males. In total, there were 53 (60.2%) males and 35 (39.8%) females. Male to female ratio of patients was 1.51:1. Statistically, there was no significant association between gender and outcome (P = 0.797) [Table 3].
Table 3.
Gender wise distribution of cases with outcome (n=88)

Mean APACHE II and Simplified Acute Physiology Score (SAPS) scores were higher among those who expired as compared to those who were discharged. However, statistically significant difference between two groups was observed for SAPS II only (P = 0.038). Mean GCS scores were higher in discharged patients as compared to those in expired patients, however, this difference was not significant statistically (P = 0.933) [Table 4 and Figure 1].
Table 4.
Association between severity scores and outcome (n=88)

Figure 1.

Various scoring system between discharged and expired group
The majority of patients, irrespective of outcome had Vitamin D deficiency. Although normal Vitamin D levels were observed in relatively higher proportion of patients who were discharged (20.3%) as compared to those who expired (7.1%) yet this difference was not significant statistically (P = 0.197) [Table 5 and Figure 2].
Table 5.
Association between Vitamin D levels and outcome (n=88)

Figure 2.

Scoring system in relation to Vitamin D level
However, mean Vitamin D levels were significantly higher in those who were discharged (18.22 ± 20.68) as compared to those who expired (6.57 ± 7.47) (P = 0.041) [Table 6].
Table 6.
Comparison of mean Vitamin D levels with outcome (n=88)

Mean APACHE II scores showed an incremental trend with increasing mean values in patients with deficiency to those with normal Vitamin D levels. Mean values were minimum among those with deficiency (15.79 ± 6.18) followed by those with insufficiency (16.57 ± 2.51) and those with normal Vitamin D levels (20.38 ± 8.46). Statistically, this difference among different Vitamin D levels was significant (P = 0.044) [Table 7].
Table 7.
Vitamin D levels and Acute Physiology and Chronic Health Evaluation II Scores, Simplified Acute Physiology Score II and Glasgow coma scale (n=89)

Mean SAPS II scores ranged from 33.71 ± 10.64 (insufficiency) to 35.63 ± 17.80 (normal). Mean scores were 34.29 ± 12.22 among those with deficiency. Statistically, the association between SAPS II scores and Vitamin D levels was not significant (P = 0.654) [Table 7].
Mean GCS scores ranged from 10.25 ± 4.37 (normal) to 11.86 ± 3.76 (insufficiency). Mean GCS score in patients with deficiency was 11.32 ± 4.76. Statistically, association between GCS and Vitamin D levels was not significant (P = 0.654) [Table 7].
Evaluation of a linear relationship between Vitamin D levels and GCS scores resulted in an inverse but weak, random natured, and nonsignificant correlation between two parameters (r = −0.027; P = 0.799) [Figure 3].
Figure 3.

Correlation between Vitamin D level and Glasgow coma scale
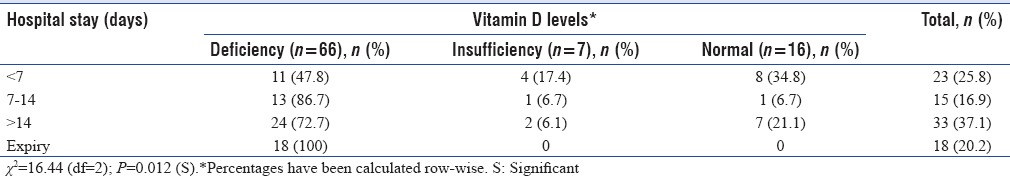
Evaluation of a linear relationship between Vitamin D levels and APACHE II scores resulted in a positive but weak, random natured, and nonsignificant correlation between two parameters (r = 0.150; P = 0.61) [Figure 4].
Figure 4.
Correlation between Vitamin D level and Acute Physiology and Chronic Health Evaluation
Evaluation of a linear relationship between Vitamin D levels and SAPS II scores resulted in an inverse but weak, random natured, and nonsignificant correlation between two parameters (r = −0.104; P = 0.332) [Figure 5].
Figure 5.

Correlation between Vitamin D level and Simplified Acute Physiology Score II score
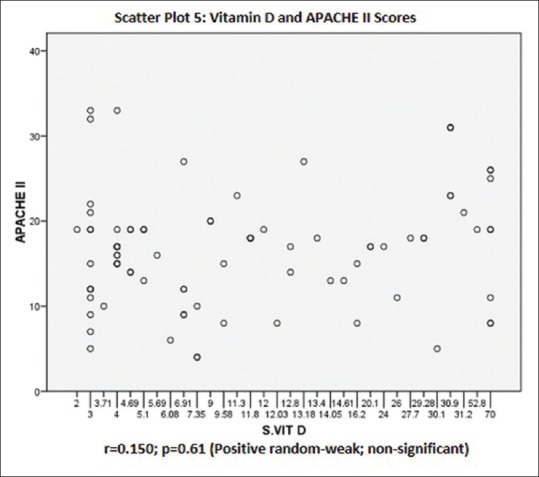
The proportion of those with normal Vitamin D levels was significantly higher in those with <7 days of hospital as compared to other groups. The proportion of patients with deficiency was lower in those who survived as compared to those who expired (P = 0.012) [Table 8].
Table 8.
Association between Vitamin D levels and hospital stay (n=89)
DISCUSSION
In this study, a total of 91 sepsis patients were enrolled among them three were excluded from the study due to the unknown outcome and finally study was conducted, and results analyzed based on data of 88 sepsis patients. The study was primarily aimed for correlating Vitamin D levels and sepsis severity as well as its outcome.
Among 88 patients whose outcome was known 74 (81.3%) were discharged and 14 (15.4%) expired; these results varied widely from the results of study carried out by Azim et al.[4] in which they included 158 sepsis patients from this study group 75 (47.46%) survived, and 83 (52.53%) expired. This variation in outcome can be attributed to many factors such as more severe cases included in their study or due to advancement and better understanding of the disease process and treatment with time. One possible reason can be more severe underlying disorders in patients included in their study apart from sepsis.
Among 88 patients included in our study we divided patients in three groups on the basis of Vitamin D levels: Deficient (serum Vitamin D level <20 ng/ml), insufficient (serum Vitamin D levels 20 to <30 ng/ml), sufficient (serum Vitamin D levels 30 ng/ml or more).[5]
Among 88 patients evaluated in our study 15 patients (18.2%) were found to have adequate Vitamin D levels and seven patients (8%) were found insufficient and rest 52 patients (73.9%) were found deficient in Vitamin D. In study carried out by Barnett et al.,[6] 120 patients of sepsis with acute lung injury were included among these patients 16 (13%) were found to be Vitamin D sufficient, 32 (27%) were found Vitamin D insufficient and rest 72 (60%) were found deficient in Vitamin D. They also had chosen similar cutoff values for deficiency, insufficiency, and sufficiency. There was little difference from Vitamin D levels from our study. This difference can be attributed to various factors including different ethnicity, nutritional status, hospital stay, and sun exposure. In another study carried out by Azim et al.[4] 31 (19.6%) patients were found Vitamin D sufficient and rest 127 (80.4%) were found either Vitamin D insufficient or deficient this prevalence of Vitamin D deficient is quite consistent with that found in our study.
As far as demographic characteristics of patients in our study is concerned; age of the patients ranged between 18 and 82 years with mean (±SD) 45.02 ± 17.69 years. In a study carried out by Jeng et al.[7] mean (± SD) of age was found to be 54 ± 17.1 among sepsis patients in ICU; the higher mean age can be due to higher low cutoff value taken for age or more number of extreme age adults.
Among evaluated patients 60.2% (53) were males and 39.8% (35) were females; this sex ratio is quite consistent with that in study of Azim et al.[4] In their study, they found that among 158 patients studied 97 (61.39%) were males and 61 (38.60%) were female patients.
In this study, we found that among Vitamin D sufficient patients there was higher percentage of discharge and lesser percentage of expiry, but this observation did not reach statistical significance (χ2 = 3.253, P = 0.197). In a study of Azim et al. they also could not find statistically significant correlation between Vitamin D levels and outcome. A study was carried out by Venkatram et al.[8] in which they considered >30 ng/dl of vitamin to be normal similar to our study. They found in their study that hospital mortality was significantly higher in Vitamin D deficient patients (P = 0.01); one of the important possible reasons for this difference can be that they included both sepsis and nonsepsis critically ill patients in their study.
A very important observation in our study worth consideration was that mean Vitamin D level was found significantly higher among patients with positive outcome than those with unfavorable outcome (expiry) (t = 2.075, P = 0.04).
In this study, we did not find any significant correlation between Vitamin D levels and lactate levels also we did not find statistically significant association between serum CRP and Vitamin D levels. Amer and Qayyum.[9] found in their study that there was statistically significant inverse relation between 25(OH) D at levels <21 ng/ml and CRP but at the level >21 ng/ml they found that higher Vitamin D levels were associated with higher levels of sepsis. They concluded from their study that the role of Vitamin D supplementation to reduce inflammation is beneficial only among those with lower serum Vitamin D levels.
In our study, we divided discharged patients into three groups on the basis of length of their hospital stay <7 days, 7–14 days, and >14 days.
On comparison of the length of hospital stay (morbidity) with Vitamin D levels, we found statistically significant inverse relation between Vitamin D levels and length of hospital stay. They concluded that proportion of those with normal Vitamin D levels was significantly higher in patients with <7 days of hospital stay as compared to other groups (χ2 = 16.44, P = 0.012). Amrein et al.[10] studied the association between length of hospital stay and effect of Vitamin D supplementation. They concluded that the median length of hospital stay was not significantly different between groups for Vitamin D versus placebo (20.1 vs. 19.3 days).
CONCLUSION
Sepsis is a leading cause of morbidity and mortality worldwide. A large chunk of our population is either deficient or insufficient as regards Vitamin D reserves. This was shown to have negative impact on inpatient morbidity, mortality as well as markers of severity of sepsis in the patients. This highlights the importance of the need for adequate Vitamin D supplementation in the population in general. Further studies are needed to demonstrate whether Vitamin D supplementation in patients of sepsis would affect the course during hospitalization and alter the morbidities experienced by the Vitamin D deficient patients suffering from sepsis.
Limitation of study
Cross-section single center study, small number of subjects.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bikle D. Nonclassic actions of Vitamin D. J Clin Endocrinol Metab. 2009;94:26–34. doi: 10.1210/jc.2008-1454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh J, Agrawal A, Gutch M, Consul S, Mahdi AA, Singh A, et al. Incidence of adrenal insufficiency and its relation to mortality in patients with septic shock. Afr J Med Health Sci. 2014;13:80–4. [Google Scholar]
- 3.Holick MF. Vitamin D status: Measurement, interpretation, and clinical application. Ann Epidemiol. 2009;19:73–8. doi: 10.1016/j.annepidem.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Azim A, Ahmed A, Yadav S, Baronia AK, Gurjar M, Godbole MM, et al. Prevalence of Vitamin D deficiency in critically ill patients and its influence on outcome: Experience from a tertiary care centre in North India (an observational study) J Intensive Care. 2013;1:14. doi: 10.1186/2052-0492-1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.White JH. Vitamin D metabolism and signaling in the immune system. Rev Endocr Metab Disord. 2012;13:21–9. doi: 10.1007/s11154-011-9195-z. [DOI] [PubMed] [Google Scholar]
- 6.Barnett N, Zhao Z, Koyama T, Janz DR, Wang CY, May AK, et al. Vitamin D deficiency and risk of acute lung injury in severe sepsis and severe trauma: A case-control study. Ann Intensive Care. 2014;4:5. doi: 10.1186/2110-5820-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jeng L, Yamshchikov AV, Judd SE, Blumberg HM, Martin GS, Ziegler TR, et al. Alterations in Vitamin D status and anti-microbial peptide levels in patients in the Intensive Care Unit with sepsis. J Transl Med. 2009;7:28. doi: 10.1186/1479-5876-7-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Venkatram S, Chilimuri S, Adrish M, Salako A, Patel M, Diaz-Fuentes G. Vitamin D deficiency is associated with mortality in the medical Intensive Care Unit. Crit Care. 2011;15:R292. doi: 10.1186/cc10585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amer M, Qayyum R. Relation between serum 25-hydroxyvitamin D and C-reactive protein in asymptomatic adults (from the continuous National Health and Nutrition Examination Survey 2001 to 2006) Am J Cardiol. 2012;109:226–30. doi: 10.1016/j.amjcard.2011.08.032. [DOI] [PubMed] [Google Scholar]
- 10.Amrein K, Schnedl C, Holl A, Riedl R, Christopher KB, Pachler C, et al. Effect of high-dose Vitamin D3 on hospital length of stay in critically ill patients with Vitamin D deficiency: The VITdAL-ICU randomized clinical trial. JAMA. 2014;312:1520–30. doi: 10.1001/jama.2014.13204. [DOI] [PubMed] [Google Scholar]


