ABSTRACT
The aim of this study was to report on the health inequalities facing stroke survivors with visual impairments as described in the current literature. A systemic review of the literature was conducted to investigate the potential health inequalities facing stroke survivors with subsequent visual impairments. A quality-of-evidence and risk-of-bias assessment was conducted for each of the included articles using the appropriate tool dependent on the type of article. Only four articles discussed health inequalities affecting stroke survivors with visual impairment specifically. A further 23 articles identified health inequalities after stroke, and 38 reported on health inequalities within the visually impaired UK or Irish population. Stroke survivors with visual impairment face inconsistency in eye care provision nationally, along with variability in the assessment and management of visual disorders. The subgroups identified as most at risk were females; black ethnicity; lower socioeconomic status; older age; and those with lower education attainment. The issue of inconsistent service provision for this population must be addressed in future research. Further research must be conducted in order to firmly establish whether or not stroke survivors are at risk of the aforementioned sociodemographic and economic inequalities.
KEYWORDS: Health inequalities, stroke, vision impairment
Background
Visual impairment is a common consequence of stroke, estimated to affect approximately 65% of stroke survivors.1 These include impairments of central vision (up to 70%); peripheral vision (up to 57%); ocular motility (up to 68%); and perceptual disorders including inattention (up to 80%).1,2 The resulting impact includes loss of confidence, mobility, and inability to return to work or driving.1,2
It is estimated that there are 111,000 new strokes in the United Kingdom (UK) every year.3 In 2009, stroke mortality rate in the UK was recorded at 53,000 per year, with premature death rates shown to be 3 times higher in the most economically deprived areas than the least deprived,3 largely due to the association of risk factors such as smoking, obesity, and poor diet.4 Preventable visual impairment is a significant public health issue, and sight loss is predicted to affect four million people in the UK by 2050 due to an increasing aging population and the association of visual loss with older age.5 Further to age and social deprivation, health inequalities of stroke and visual impairment may include gender, race, and educational attainment.
The reported economic cost of stroke between 2006 and 2007 in the UK was £4.5 billion.3 In addition, visual impairment was recorded to cost the UK £4.3 billion between 2009 and 2013, including the cost of resultant unemployment.5 Reducing health inequalities and lowering the rate of stroke and visual impairments by targeting the most affected groups could reduce this economic burden.5 The aim of this review is to report the health inequalities facing stroke survivors in the UK and Ireland with visual impairments as described in the current literature.
Methods
A systemic review of the literature was conducted to investigate the potential health inequalities facing stroke survivors with subsequent visual impairments. A quality-of-evidence and risk-of-bias assessment was conducted for each of the included articles using the appropriate tool dependant on the type of article.
Inclusion criteria for considering studies for this review
Types of studies
The following types of studies were included: randomised controlled trials, controlled trials, cohort studies, observational studies, and retrospective medical note reviews. Case reports were excluded due to the high risk of bias associated with these types of reports. Review articles were excluded, as the relevant articles from these review articles were extracted and discussed independently. All languages were included and translation obtained.
Types of participants
We included studies of adult participants (aged 18 years or over) diagnosed with a stroke or a visual impairment. Owing to limited literature, the visual impairments discussed did not necessarily result from a stroke itself but represented the same visual symptoms one may experience following a stroke.
Types of outcome and data
The outcomes collected were clinical improvement in visual functions, functional improvement in activities of daily living, and quality-of-life measures.
Search methods for identification of studies
We used systematic search strategies to search key electronic databases and contacted known experts in the field.
We searched the Cochrane Stroke Group Trials Register, the Cochrane Eyes and Vision Group Trials Register, and the following electronic bibliographic databases:
The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, latest issue)
MEDLINE (1950 to March 2016)
Embase (1980 to March 2016)
CINAHL (1982 to March 2016)
AMED (1985 to March 2016)
PsycINFO (1967 to March 2016)
Dissertations & Theses (PQDT) database (1861 to March 2016)
British Nursing Index (1985 to March 2016)
PsycBITE (Psychological Database for Brain Impairment Treatment Efficacy, www.psycbite.com)
In an effort to identify further published, unpublished, and ongoing trials, we
- Searched the following registers of ongoing trials:
- ClinicalTrials.gov (http://clinicaltrials.gov/)
- Current Controlled Trials (www.controlledtrials. com)
- Trials Central (www.trialscentral.org)
- Health Service Research Projects in Progress (wwwcf.nlm.nih.gov/hsr_project/home_ proj.cfm)
- National Eye Institute Clinical Studies Database (http://clinicalstudies.info.nih.gov/cgi /protinstitute.cgi?NEI.0.html)
Hand-searched the British and Irish Orthoptic Journal, Australian Orthoptic Journal, and proceedings of the European Strabismological Association (ESA), International Strabismological Association (ISA), International Orthoptic Association (IOA) (http://pcwww.liv.ac.uk/~rowef/index_files/Page646.htm), and Association for Research in Vision and Ophthalmology (www.arvo.org).
Performed citation tracking using Web of Science Cited Reference Search for all included studies.
Searched the reference lists of included trials and review articles about vision after acquired brain injury.
Contacted experts in the field (including authors of included trials, and excluded studies identified as possible preliminary or pilot work).
Search terms included a variety of Medical Subject Headings (MeSH) terms and alternatives in relation to stroke and visual conditions (Table 1).
Table 1.
Search terms.
| Cerebrovascular disorders/ | Eye Movements/ | Health inequality/ |
| Brain ischaemia/ | Eye/ | Health equity/ |
| Intracranial Arterial Disease | Eye Disease/ | Socioeconomic/ |
| Intracranial Arteriovenous Malformations/ | Visually Impaired Persons/ | Sociodemographic/ |
| “Intracranial Embolism and | Vision Disorders/ | Gender/ |
| Thrombosis*/ | Blindness/ | Male/ |
| Stroke/ | Diplopia/ | Female/ |
| Vision, Binocular/ | Age/ | |
| Vision, Monocular/ | Ethnicity/ | |
| Visual Acuity/ | Race/ | |
| Visual Fields/ | Transport/ | |
| Vision, Low/ | Education/ | |
| Ocular Motility Disorders/ | Occupation/ | |
| Blindness, Cortical/ | Access to services/ | |
| Hemianopsia/ | Access to care/ | |
| Abducens Nerve Diseases/ | ||
| Abducens Nerve/ | ||
| Oculomotor Nerve/ | ||
| Trochlear Nerve/ | ||
| Visual Perception/ | ||
| Nystagmus/ | ||
| Strabismus/ | ||
| Smooth pursuits/ | ||
| Saccades/ | ||
| Depth perception/ | ||
| Stereopsis/ | ||
| Gaze disorder/ | ||
| OR | OR | OR |
| AND | ||
Selection of studies
The titles and abstracts identified in the primary review were independently screened by both authors using the inclusion criteria discussed previously. Where it was not possible to establish if a study met these criteria from the title or abstract, the full paper was obtained. A secondary review of the full papers was then undertaken independently by the two authors to determine which studies should be included. In the case of disagreement for inclusion of studies, an option was available to obtain a third author opinion. In practice, this was not required, as no disagreements occurred for inclusion of papers.
Data extraction
A predesigned data extraction form was designed. Data were extracted and documented by one author (K.H.) and verified by another (F.R.).
Quality assessment
One author (K.H.) independently assessed the quality of the studies included in this review using the STROBE checklist. An adapted version of the STROBE statement was used to assess the quality of cross-sectional, cohort, and control studies. The STROBE statement covers 22 items from introduction, methods, results, and discussion.6 The adapted version of the STROBE statement used in this review included 18 items.
Results
The results of the literature search identified 189 articles reporting on worldwide health inequalities in stroke populations and populations with visual impairments (Figure 1). Only four were found that directly discussed health inequalities in stroke survivors with a visual impairment. However, a further 97 were found that discussed health inequalities in stroke populations only, and 88 were identified as reporting on health inequalities in populations with visual impairments, which could further identify possible inequalities facing stroke survivors with visual impairment. Collectively, these categories included:
Socioeconomic and income
Race/ethnicity
Gender
Age
Education level
Occupation
Transport
Access to services
Figure 1.
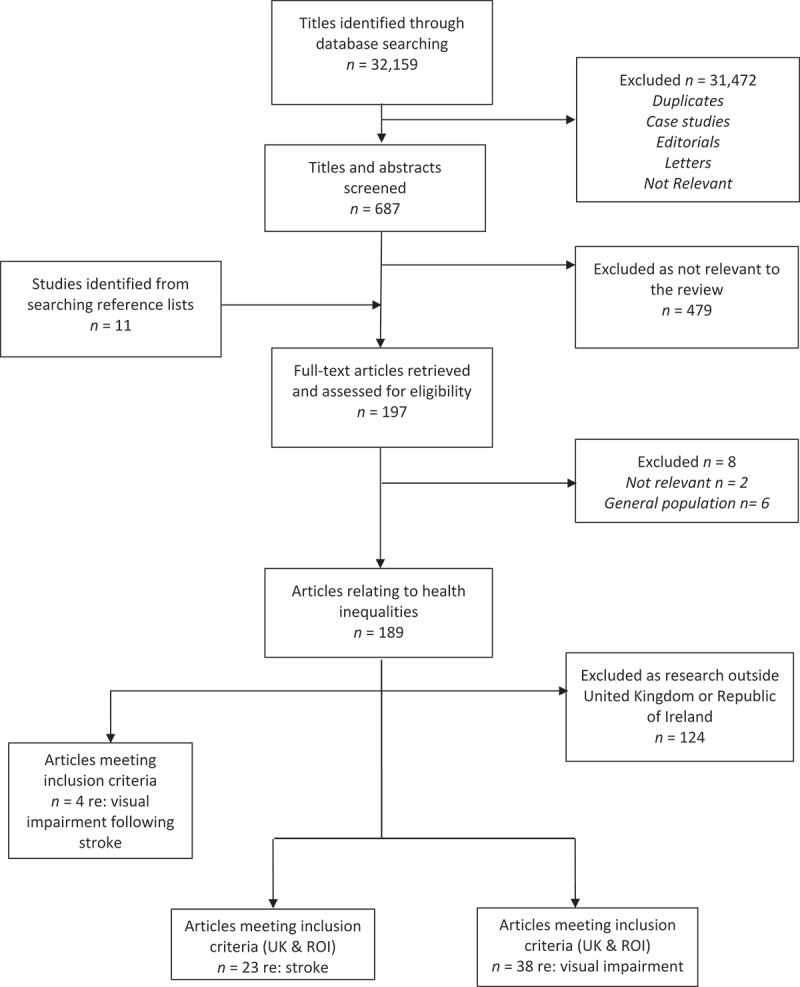
Flowchart of pathway for inclusion of articles.
The four articles directly discussing health inequalities in visually impaired stroke survivors were included in the review, two of which were UK studies and thus met the inclusion criteria. However, as both articles were co-written by one of the authors, all four articles were included in the review to address potential perceived bias. Consideration of the National Health Services in these countries (Australia and USA) was given to these two additional articles. Of the remaining 189 articles, only those reporting on population samples from the UK and republic of Ireland would be included in this review due to their direct relevance to our current health care system. After exclusion, the final numbers included four articles reporting on health inequalities due to post-stroke visual impairment, along with an additional 23 articles discussing stroke-related health inequalities only and a further 38 articles reporting on health inequalities in non-stroke populations with visual impairment.
Quality of the evidence
The majority of the included articles (n = 48) were of population-based studies (36 prospective, 10 retrospective, and 2 unclear), along with two surveys, three questionnaires, 11 retrospective medical note reviews or audits, and one article reporting on a series of prospective focus groups. A quality-of-evidence assessment was completed for each using the STROBE tool (Table 2). Evidence was deemed to be of good quality if the article reported ≥75% of the items on the relevant assessment checklist. Overall, 30 of the reported articles scored 100% in the quality-of-evidence assessment. The remaining 35 articles included in this review reported between 75% and 99% of the checklist items assessed and were deemed to have good quality. No article scored less than 75%.
Table 2.
Quality appraisal of papers using the STROBE checklist.
| Methods |
Results |
Discussion |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
Study design |
Participants |
Variables |
Data source |
Bias |
Study size |
Quantitative variables |
Statistical methods |
Participants |
Descriptive data |
Outcome data |
Main results |
Other analyses |
Key results |
Limitations |
Interpretation |
Generalisability |
| n | 4 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 |
| Acharya et al. 200958 | + | + | + | + | ? | + | + | + | + | + | + | + | + | + | + | + | + |
| Addo et al. 201119 | + | + | + | + | ? | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Bachmann et al. 200340 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Banerjee et al. 201031 | + | + | + | + | ? | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Bhopal et al. 201128 | + | + | + | + | + | + | + | + | ? | + | + | + | n/a | + | ? | + | + |
| Buch et al. 200544 | + | + | + | + | − | + | + | − | + | + | + | + | n/a | ? | + | + | ? |
| Busch et al. 200922 | + | + | + | + | ? | + | + | + | + | + | + | + | + | + | ? | + | + |
| Chaturvedi and Ben-Schlomo 199542 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Chen et al. 201417 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Chen et al. 201520 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Cookson et al. 201243 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Cooper et al. 200968 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Cox et al. 200465 | + | + | + | + | + | + | + | + | ? | + | + | − | n/a | + | − | + | + |
| Cumberland et al. 201671 | + | + | + | + | + | + | + | + | + | ? | + | + | + | + | + | + | + |
| Day et al. 201059 | + | + | + | + | ? | + | + | + | ? | + | + | + | + | + | + | + | + |
| Dickey et al. 201244 | + | + | + | + | + | + | ? | + | + | + | + | − | n/a | + | + | + | + |
| Fraser et al. 200160 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Gall et al. 201011 | + | + | + | + | − | + | + | + | + | + | + | + | + | + | + | + | + |
| Gallagher et al. 201173 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | − | + | + |
| Gulliford et al. 201045 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Hacker and Stanistreet 200467 | + | + | + | + | − | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Hajat et al. 200129 | + | + | + | + | ? | + | + | + | + | + | + | + | n/a | + | − | + | + |
| Hart et al. 200013 | + | + | + | + | ? | + | + | + | + | + | + | + | n/a | + | − | + | + |
| Heuschmann et al. 200815 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Jerath et al. 201112 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Keenan et al. 200746 | + | + | + | + | − | + | + | + | + | + | + | ? | n/a | + | + | + | + |
| Keenan et al. 200947 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Keenan et al. 201248 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Kerr et al. 201014 | + | + | + | + | ? | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Kliner et al. 201249 | + | + | + | + | − | + | + | + | − | − | + | + | n/a | + | + | + | + |
| Kunst et al. 199818 | + | + | + | + | + | ? | + | + | − | + | + | + | n/a | + | + | + | + |
| Lazzarino et al. 201133 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Leese et al. 200850 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Lockington et al. 201061 | + | + | + | + | + | − | + | + | + | ? | + | + | n/a | + | − | + | + |
| McCartney et al. 201521 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| McFadden et al. 200916 | + | + | + | + | + | ? | + | + | + | + | + | + | n/a | + | + | + | + |
| McKevitt et al. 200526 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Millett and Dodhia 200651 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Nessim et al. 201039 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Ng et al. 201057 | + | + | + | + | + | + | + | + | + | + | + | − | n/a | + | − | + | ? |
| Owen et al. 200652 | + | + | + | + | ? | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Owen et al. 200968 | + | + | + | + | + | + | + | + | + | + | − | + | n/a | + | + | + | + |
| Patel et al. 200736 | + | − | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Power et al. 200534 | + | + | + | + | + | ? | + | + | + | + | + | + | + | + | + | + | + |
| Putman et al. 200735 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Rahi et al. 200853 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Raine et al. 200932 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Redfern et al. 200222 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | − | + | + |
| Rowe 20107 | + | + | + | + | − | + | + | + | + | + | + | + | n/a | + | − | + | + |
| Rowe at al. 20158 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Sabates and Feinstein 200854 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Saidkasimova et al. 200962 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Scanlon et al. 200855 | + | + | + | + | ? | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Sherwin et al. 201266 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Shickle and Farragher 201537 | + | + | + | + | + | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Smeeton et al. 200730 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Sukumar et al. 200963 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Van der Pols et al. 199956 | + | + | ? | + | ? | + | + | + | + | + | + | + | n/a | + | − | + | + |
| Wallace et al. 200864 | + | + | + | + | − | + | + | + | + | ? | + | − | n/a | + | − | + | + |
| Wang et al. 201325 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Waqar et al. 201238 | + | + | + | + | + | + | + | − | + | + | + | + | n/a | + | + | + | + |
| Wolfe et al. 200224 | + | + | + | + | ? | + | + | + | + | + | + | + | + | + | ? | + | + |
| Wolfe et al. 200527 | + | + | + | + | − | + | + | + | + | + | + | + | n/a | + | + | + | + |
| Yip et al. 201370 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Yip et al. 201572 | + | + | + | + | + | + | + | + | + | + | + | + | + | + | − | + | + |
 = Not reported
= Not reported  = Unclear
= Unclear  = Reported
= Reported
Health inequalities affecting stroke survivors with visual impairment
The literature search identified just four articles reporting on health inequalities facing stroke survivors with visual impairment (Table 3). These discussed inequalities in service delivery and gender.
Table 3.
Articles reporting on health inequalities associated with stroke-related visual impairments.
| Article | Year/duration of research | Country of research | Study type | Population (n) | Aim |
|---|---|---|---|---|---|
| Rowe 20107 | 2007 | UK | Survey of stroke services—non-validated questionnaire | 134 stroke services | To determine the extent of Orthoptic involvement in stroke services throughout the UK and what constitutes a vision assessment |
| Rowe et al. 20158 | 2013 | UK | Online survey | 31 professional groups, 548 individuals | To explore care provision for post-stroke visual impairment and variations in the UK |
| Gall et al. 201011 | 1996–1999 | Australia | Population-based study | 1316 first ever stroke | To examine sex differences in presentation, severity, in-hospital treatment and early mortality in a cohort of first ever stroke patients |
| Women = 731 | |||||
| Men = 585 | |||||
| Jerath et al. 201112 | 2011 (data were collected in 1984–1989) | USA | Population-based study | 449 first ischaemic stroke | To investigate gender differences in presenting signs and symptoms of acute ischaemic stroke |
| Women = 268 | |||||
| Men = 181 |
Access to services
Rowe7 reported that only 45% of stroke units in the UK provide a vision service at the acute stage of stroke. This will result in many stroke survivors being mismanaged or even undiagnosed of their visual impairment. The health inequality was in the area of residence (hospital catchment area) and was dependent on where one had their stroke as to whether or not they received visual input with their stroke care.
In a more recent study, Rowe et al.8 identified further inequalities in stroke care when visual screening is undertaken. There is significant variability across the UK as to who performs the visual assessment, which tests are used, how visual impairments are managed, and when patients are referred to eye care services. Many orthoptists and occupational therapists (22%) reported using screening tools commonly based on patient reported signs and symptoms or observed signs alone. As many stroke survivors cannot report their visual impairment due to stroke-related speech difficulties and many visual problems will not elicit obvious signs, it is possible that few would be identified via this screening method.8,9 It has been suggested that national care pathways, such as the National Institute for Health and Care Excellence (NICE) pathways,10 to guide health care professionals would address the issue of variation in visual management and onward referral to eye services to allow all stroke survivors adequate and equitable care.8
Gender
Gall et al.11 reported that women were more likely to suffer visual field loss following stroke, whilst similar numbers of men and women suffered neglect. Moreover, the females in this study had a greater 28-day mortality due to their increased age and stroke severity. However, it should be noted that the data collection period for this study significantly predates the year of publication and may not be a true reflection of gender differences in the current population.
A more recent study reported that following stroke, men and women can present with very different symptoms,12 although the findings were not significant between either gender presenting with visual field loss, which differ from the findings by Gall et al.11 However, men more frequently reported traditional signs and symptoms of stroke, including the following visual impairments: visual hallucinations, photophobia, blurred vision, nystagmus, and diplopia. Women tended to present with non-traditional stroke symptoms such as fatigue and disorientation, which often resulted in delayed diagnosis and treatment. The authors urge health care professionals and women to become more aware of the presenting signs to reduce this inequality.12
Health inequalities affecting the general stroke population
Twenty-three articles were identified that discussed health inequalities facing stroke survivors without named visual impairments (Table 4). Health inequalities were reported from the following subcategories: race/ethnicity; gender; age; socioeconomic; education level; and access to stroke services.
Table 4.
Articles reporting on stroke-related health inequalities.
| Article | Year/duration of research | Country of research | Study type | Population (n) | Aim |
|---|---|---|---|---|---|
| Addo et al. 201119 | 2007–2009 | UK, England | Population-based stroke register | 3800 with first ever ischaemic stroke or primary intracerebral haemorrhage between 1995–2009 | To investigate time trends in receipt of effective stroke care and to determine factors associated with provision of care |
| Banerjee et al. 201031 | 2003–2007 | UK | Prospective database | 811 (stroke = 736) | To analyse differences between south Asian and white risk factor profile |
| Bhopal et al. 201228 | 2001–2008 | UK, Scotland | Retrospective cohort study | 4.65 million from census and stroke database | To show links of ethnic variations and stroke incidence |
| Busch et al. 200922 | 1995–2004 | UK, England (London) | Prospective, population-based study | 2874 first ever strokes | To investigate the frequency and determinants of return to paid work after stroke |
| Chen et al. 201417 | 1995–2011 | UK, England (London) | Retrospective analysis of prospectively collected data | 4398 first ever stroke | Assess the associations between SES and survival after stroke |
| Chen et al. 201520 | 1995–2011 | UK, England (London) | Retrospective analysis of prospectively collected data | 2104 alive at 3 months post stroke | To assess the association between SES and functional impairment post stroke in relation to age, sex phenotype differences |
| Hajat et al. 200129 | 1995–1998 | UK, England | Prospective population-based study | 1254 first ever stroke | To establish the frequency of cardiovascular risk factors in patients with first-ever stroke—relationship with ethnicity |
| Hart et al. 200013 | Had been screened in 1972–1976 | UK, Scotland | Prospective questionnaire | 467 men and 535 women | Investigate stroke differentials by socioeconomic position in adulthood |
| Heuschmann et al. 200815 | 1995–2004 | UK, England | Prospective population-based study | 2874 first time stroke | Investigate trends in stroke incidence and modifiable risk factors between different ethnic groups |
| Kerr et al. 201114 | 2007–2008 | UK, Scotland | Prospective multi-centred observational study | 467 stroke and TIA (stroke = 313) | To determine whether low SES stroke/TIA patients have reduced health care access |
| Kunst et al. 199818 | 1980s | England, Wales, Ireland, Finland, Sweden, Norway, Denmark, France, Switzerland, Italy, Spain, Portugal, USA | Retrospective review of national longitudinal and cross-sectional studies | Number of participants not stated | To present an international overview of socioeconomic differences in stroke mortality |
| Men aged 30–64 with stroke | |||||
| Lazzarino et al. 201133 | 2006–2009 | UK, England | Not clear if data collected retrospectively or prospectively | 209,174 emergency admissions for stroke | To describe the use of brain scanning in English hospitals and identify patient groups being excluded from appropriate care |
| McCartney et al. 201421 | 1995–2003 | UK, England and Scotland | Retrospective review of 18 cohort studies (15 English and 3 Scottish) | 193,873 Pooled data from 18 cohorts | To what extent SES, behavioural, anthropometric, and biological explain high levels of mortality in Scotland compared to England |
| McFadden et al. 200916 | 1993–1997 and followed up until 2007 | UK, England | Prospective population study | 22,488 Followed up for stroke | To investigate the association between working social class and stroke incidence |
| 39-79 years old | |||||
| McKevitt et al. 200526 | 1995–2000 | UK, England | Population-based stroke register | 1635 first ever stroke | Investigate the associations between SES and provision of acute and long-term stroke care |
| Power et al. 200534 | Over 45 year period | UK | Prospective study (follow up of 45 years) | 11,855 Women aged 14–49 (stroke = 217 participants but discussed separately) | To see if women’s childhood socioeconomic position influenced their risk of mortality |
| Putman et al. 200735 | Not stated | 6 stroke rehab units in Europe: UK, Germany, Switzerland, Belgium | Prospective, multi-centre population-based | 419 first ever stroke aged 40–85 | Examine the impact of education and income on recovery after stroke |
| Raine et al. 200932 | 1995–2005 | UK, England | Cohort study using data from primary care database | 12,830 aged 50+ who suffered a stroke between 1995–2005 and survived for the first 30 days | To determine extent to which secondary drug prevention for stroke pts varies by sex age and SES |
| Redfern et al. 200222 | 1995–1998 | UK, England (London) | Prospective population-based study | 717 first ever stroke | Access to health care follow-up after stroke |
| Smeeton et al. 200730 | 1995–2004 | UK, England (London) | Prospective population-based study | 566 first ever stroke | To see if race varied with incidence of intracerebral haemorrhage or subarachnoid haemorrhage |
| Wang et al. 201325 | 1995–2010 | UK, England (London) | Prospective population-based study | 4245 first ever stroke | Investigate age and ethnic disparities in stroke incidence |
| Wolfe et al. 200224 | 1995–1998 | UK, England (London) | Population-based stroke register | 1254 first ever stroke | Identify sociodemographic differences in incidence of stroke |
| Wolfe et al. 200527 | 1995–2002 | UK, England (London) | Population-based stroke register with follow-up | 2321 first ever stroke | Identify ethnic differences in survival after stroke |
Socioeconomic
A number of studies (n = 4) discuss the relationship between poor socioeconomic status (SES) and increased risk of stroke,13–16 with one study showing that social deprivation resulted in nearly twice the risk of stroke.13 Some studies found that certain demographics were more affected by social status than others in relation to stroke outcomes.14,15,17
One study compared the effect of SES and stroke mortality across a number of countries including England, Wales, and Ireland; however, estimates were only possible for males aged 45–59.18 They concluded that SES played a significant role, with males of manual class having a significantly higher rate of stroke mortality than those of non-manual class. However, a more recent study found that females from lower SES were twice as likely to suffer a stroke.13 After adjustment for stroke risk factors, there was no longer a significant association with the male population. Furthermore, Chen et al.17 reported a significant association between lower SES and survival after stroke, but only for those of black ethnicity.
Various articles revealed that those form lower SES were less likely to receive adequate hospital care following stroke. It has been reported that persons of lower SES are less likely to receive brain imaging at the acute stage of stroke.14,19 Additionally, stroke survivors from lower SES were less likely to attend their hospital appointments.14 A further study investigating functional recovery post-stroke revealed those from socioeconomically deprived areas had significant functional impairment at 3 moths post-stroke compared with those of higher SES.20
However, a number of articles reported little or no relationship between social class and stroke-related health inequalities. McCartney et al.21 found a 42% increased rate of stroke mortality in Scotland compared with England but reported that socioeconomic characteristics accounted for only a quarter of this difference. They identified risk factors such as smoking as the main cause for the high stroke mortality rate in Scotland. Furthermore, Busch et al.22 found that SES did not impact on UK individuals’ chances of returning to work after stroke, whilst Redfern et al.23 found no socioeconomic inequalities relating to access of health care follow up after stroke. Although the primary factor affecting stroke outcome is likely related to risk factors as opposed to social position or area of residence, these risk factors are more commonly found in lower socioeconomic groups13,14 and, as such, infers a health inequality within this group
Race/ethnicity
Twelve articles discussed race/ethnicity inequalities in stroke populations. Stroke incidence is shown to be higher in some ethnic groups compared with others. Overall, the black population appears to be at a higher risk of stroke than white, Asian, or Hispanic populations.24 From 1995 to 2010, there was a significant decrease in stroke incidence in the white population but not in blacks.25 Black persons are more likely to be admitted to acute stroke units,19,26,27 although the reason behind this is unclear. McKevitt et al.26 suggested that one reason for this is that black minorities are more often admitted as a precaution because of their typical younger age compared with white populations, or because clinicians are now sensitised to the stroke risk profile in the black African and Caribbean populations.
Heuschmann et al.15 noted a decrease in stoke incidence for white males and females but not for black males. This finding that black males have an increased risk of stroke compared with black females was furthered by Bhopal et al.28 Furthermore, Busch et al.22 found the odds of black males returning to work following stroke were significantly less. Postulated reasons for this include an increased association with risk factors such as smoking and hypertension in the black population.29 It has been recommended that improved use of medication to control risk factors could address this, although further research into compliance and dose assessment is required.27
Some articles reported no association of race/ethnicity after stroke, or conversely, that whites were more at risk of health inequalities. Wolfe et al.27 found the white population to have poorer survival outcomes following stroke, whilst the black population over the age of 65 were more likely to survive a first-time stroke (57% survival rate at 5 years post-stroke compared with 36% in the white population). They suggest that the heightened risk factors in the UK white population of heart disease, transient ischaemic attacks (TIA), and atrial fibrillation outweighed the risk of hypertension and diabetes in the older UK black population. This concurs with the findings by Smeeton et al.,30 where only black Caribbean and Africans under the age of 65 had higher rates of hypertension, possibly explaining why older black persons were previously found to have better stroke outcomes.27
Redfern et al.23 found no association of any race in access to health care following stroke. The authors initially observed that higher rates of lacunar strokes and infarcts were in the Asian population, although this finding was not significant.31 Likewise, Chen et al.17 found an initial increase in risk of mortality after stroke within black Caribbean and Africans, but this was deemed not significant after adjustment for acute stroke care provisions.
Gender
Overall, there has been an equal decline in stroke incidence between both genders in the last 10 years.25 However, one study has reported a higher incidence of stroke within the female UK population.13 Furthermore, Chen et al.20 has shown that females have poorer functional recovery after stroke compared with men due to an increased risk of factors associated with social deprivation.20 Consequently, females have a lower chance of returning to work following a stroke.22 Hart et al.13 was unable to explain the finding of higher stroke risk in females from the most deprived groups but speculate alcohol consumption, poor diet, and lack of physical exercise as possible reasons.
Conversely, McFadden et al.16 found that social class played a significant role in increasing stroke incidence between both genders equally, although their smaller population size could limit the validity of their findings when compared with other studies.
Others found no significant differences between gender in respect to stroke incidence,31 access of stroke services,23 or access to secondary drug prevention for patients.32 One study has shown evidence of health inequalities within the male population in relation to stroke care provision.14 Kerr et al.14 found that men were less likely to be offered an electrocardiogram (ECG) following stroke. However, another study reported no differences between genders in relation to hospital admission or likelihood of receiving a brain scan.26 Yet, a more recent study reported that men were more likely than women to be selected for brain scanning after a stroke.33
Age
Four of the fifteen articles discussing age-related health inequalities found that older persons are at higher risk of stroke.24,25,27,31 Hajat et al.29 reported that increasing age correlated significantly with increased risk of infarction but not with haemorrhagic stroke, whilst a study investigating risk of stroke in females found that age was a significant factor of stroke mortality.34
Redfern et al.23 found stroke survivors over the age of 65 were less likely to be offered follow-up appointments. Although they could not provide an explanation for their findings, the authors speculate that health professionals may find it difficult to discuss lifestyle issues and behavioural risk factors with patients, meaning those most at risk don’t receive follow-up.23 Moreover, functional recovery after stroke is shown to be significantly worse in the older population (>65 years old).20,26 One study showed that the chances of returning to work decreased as age increased.22
An inequality was identified in relation to access to stroke services, as older patients (≥75) were less likely to receive brain imaging following stroke.19 This concurs with the findings from Lazzarino et al.33 that younger patients were more likely to be selected for brain imaging. Moreover, Raine et al.32 found that increasing age was significantly associated with reduced odds of receiving secondary preventative drugs after stroke. The odds increased from 26.4% for 50–59-year-olds to 15.6% in 80–89-year-olds, and just 4.2% for those aged >90.
However, a study by Banjeree et al.31 found that south Asians living in London were at an increased risk of stroke if aged ≤55 years. This is due to higher risk of diabetes in this younger population. This concurs with the findings by Wang et al.25 who noted a 40% reduction in stroke incidence from 1995 to 2010 in those >45 years old. However, there was no significant change in the 15–44-year-olds due to an increased rate of diabetes over this period. Additionally, Smeeton et al.30 found that the rate of hypertension in black populations <65 years old reportedly increased between 1995 and 2004, subsequently increasing the incidence of stroke.
It has been further suggested that socioeconomic factors play a role in the association between age and stroke incidence. It was found that stroke survivors in lower socioeconomic groups were of younger age,14 which could indicate poorer health outcomes from a younger age for those living in more deprived areas of the UK.
Education
Only one article discussed education attainment and stroke-related health inequalities, concurring that a lower educational level is associated with poorer stroke recovery whilst in hospital.35 However, this was not significant for recovery following discharge. Additionally, a high level of education correlated with a higher Rivermead motor assessment score, which may suggest that those with a higher education will have a better functional outcome after stroke.35
Health inequalities affecting the visually impaired population
Thirty-eight articles reported on health inequalities associated with non-stroke-related visual impairments (Table 5). Visual impairments can arise form a wide range of possible diagnoses, including glaucoma, age-related macular degeneration (AMD) and cataracts, the symptoms of which can be compared with those caused by stroke. Potential health inequalities facing this population include gender; age; occupation; socioeconomic; education level; and transport.
Table 5.
Articles relating to vision impairment health inequalities.
| Article | Year/duration of research | Country of research | Study type | Population (n) | Aim |
|---|---|---|---|---|---|
| Acharya et al. 200958 | 2004–2005 | Scotland, UK | Retrospective medical note review | 240 with new exudative AMD | To evaluate the influence of socioeconomic factors on visual acuity (VA) at presentation in exudative age-related macular degeneration |
| Bachmann et al. 200340 | 1998–2000 | England, UK | Cross-sectional questionnaire survey | 770 diabetes | To investigate socioeconomic inequalities in diabetes complications and to examine factors that may explain these differences |
| Buch et al. 200544 | 2000–2001 | UK | Cross-sectional study | 11682 Patients who underwent retinal screening between 2000–2001 | To assess the coverage of a diabetes retinopathy screening service and identify characteristics associated with non-attendance |
| Chaturvedi and Ben-Schlomo 199542 | 1991–1992 | UK | Cross-sectional study | 140,049 patients from a GP surgery | To determine whether there are socioeconomic differences in the relationship between expressed need for possible surgical intervention and surgical provision |
| Cookson et al. 201243 | 2001–2008 | UK | Ecological study | 32,482 English small areas | To investigate whether there was any change between 2001 and 2008 in small-area socioeconomic equity in the utilisation of specialist care relative to need in the English NHS |
| All adults receiving non-emergency hospital care in the English NHS from 2001 to 2008 | |||||
| Cooper et al. 200968 | 1997–2007 | England, UK | Retrospective cross-sectional study | 427,277 elective knee replacement patients, | To determine whether waiting times occurred for certain key elective procedures |
| 406,253 elective hip replacement patients, | |||||
| 2,568,318 elective cataract repair patients | |||||
| Cox et al. 200565 | 2000–2001 | Scotland, UK | Cross-sectional study | 537 fracture patients aged 65 and over | To evaluate the current visual status and ophthalmic history of a sample of elderly patients with fractured neck of femur |
| Cumberland et al. 201671 | 2009–2010 | UK | Cross-section epidemiological study | 112,314 adults with low vision | To investigate the association of visual health with social determinants of general health and the association of visual health and health and social outcomes |
| Day et al. 201059 | 2002–2007 | UK, England (Leeds) | Equity profile mapping It is not a formal epidemiological survey | Estimate between 5963 and 6700 people with glaucoma in Leeds | Unclear To map an equity profile for glaucoma in Leeds but can be reused for other ophthalmic conditions in other UK locations |
| Dickey et al. 201244 | 1999–2008 | Scotland, UK | Analysis of nationwide survey | Not stated. Covers >5000 households in the UK | To examine how the introduction of free eye examinations in Scotland affected people’s use of eye care services |
| Gallagher et al. 201173 | Not stated | Ireland and Northern Ireland | 14 Focus groups | 121 urban and rural dwellers with visual impairment | Explore mobility and access to transport issues of people with visual impairment (differences in urban and rural) |
| Gulliford et al. 201045 | 2007–2009 | England, UK | Retrospective study | 31,484 subjects (59,495 appointments) | To quantify socioeconomic and ethnic inequalities in diabetes retinal screening |
| Hacker and Stanistreet 200467 | 2000–2001 | England, UK | Retrospective study | 4306 ophthalmology or orthopaedic waiting list patients (elective, first episodes) living within Health Authority boundaries | To investigate the extent to which equitable access is achieved in one routinely administered hospital waiting list system |
| Fraser et al. 200160 | 1996–1997 | UK | Prospective hospital based Case-control study | 220 glaucoma | To identify socioeconomic risk factors associated with glaucomatous visual field loss |
| Keenan et al. 200746 | 1960–2003 | England, UK | Retrospective audit | Hospital episodes of cataract admissions | To examine time trends and geographical variation in rates of cataract surgery |
| Keenan et al. 200947 | 1976–2004 | England, UK | Retrospective audit | Hospital episodes of annual trabeculectomy admissions | To examine trends over time and regional variation in rates of trabeculectomy in England |
| Keenan et al. 201248 | 1989–2009 | England, UK | Retrospective audit | Hospital episodes of annual treatment rates of intravitreal injections | To report on trends over time and, geographical variation in intravitreal injection rates in England |
| Kliner et al. 201249 | Unclear | England, UK | Ecological study | N = ? Diabetic retinopathy | To conduct an equity profile to identify inequity in eye health across Leeds and Bradford |
| Leese et al. 200850 | 2004–2006 | Scotland, UK | Population-based study | 15,150 patients with diabetic retinopathy | To identify criteria that affect uptake of diabetes retinal screening in a community screening program |
| Lockington et al. 201061 | 1994–2008 | Scotland, UK | Retrospective record review | 536 patients with choroidal melanoma | To audit the demographic characteristics of patients with choroidal melanoma |
| Millett and Dodhia 200651 | 2003 | England, UK | Cross-sectional study | Patients on a centralised disease register invited for screening N = 8061 | To assess uptake of the diabetes retinopathy screening programme in South East London and examine variation in attendance and screening outcomes |
| Nessim et al. 201039 | Unclear | England, UK | Retrospective case note reviews | 139 consecutive patients presenting with acute primary angle closure glaucoma | To investigate the association of social deprivation as a risk factor for acute primary angle closure in a UK urban population |
| Ng et al. 201257 | 2006 | Scotland, UK | Cross-sectional study | 48 patients with severe glaucoma and 74 patients with non-severe glaucoma | To evaluate the influence of socioeconomic factors on severity of glaucoma at presentation |
| Owen et al. 200652 | 1994–2003 | UK | Retrospective review | 131 general practices across the UK | To study trends in the prevalence of being treated for glaucoma and ocular hypertension and to examine factors determining treatment in 2002 |
| Owen et al. 200969 | 1993–2005 | UK | Retrospective medical note reviews | 5670 registered patients newly prescribed an ocular hypotensive drug | To examine trends and demographic factors affecting persistence with ocular hypotensive therapy |
| Patel et al. 200736 | 1998–2001 | UK | Questionnaire | 3652 (23 towns) Older Women aged 62–83 | To examine socioeconomic position and self-reported use of 6 preventative and therapeutic services including eye services |
| Rahi et al. 200853 | Unclear | UK | Cohort study | 9271 members of the 1958 British birth cohort | To investigate frequency of visual impairment due to undiagnosed RE and its associations with vision-related quality of life (VRQOL), general health and social circumstances |
| Sabates and Feinstein 200854 | 1991–2003 | UK | Analysis of data from national survey | Approx. 10,000 individuals | To investigate whether permanent and transitory income effects mask the impact of unobservable factors on the uptake of health check-ups in Britain |
| Saidkasimova et al. 200962 | 2007–2008 | Scotland, UK | Prospective, multi-centre population-based observational study | 572 patients with retinal detachment | To investigate any association between retinal detachment, macular status at presentation and deprivation |
| Scanlon et al. 200855 | 1998–2003 | England, UK | Cross-sectional | 13,304 patient records in data set 1. | To investigate socioeconomic variations in diabetes prevalence, uptake of screening for diabetic retinopathy, and prevalence of diabetic retinopathy |
| 10,312 patients with diabetic retinopathy in data set 2 | |||||
| Sherwin et al. 201266 | 2006 | England, UK | Prospective study | 4428 participants between 48 and 89 years old | To investigate the prevalence of, and demographic associations with, uncorrected refractive error (URE) in an older British population |
| Shickle and Farragher 201437 | 2011 | UK, England (Leeds) | Population based | 17,680 eye examinations taken from general ophthalmic services claim forms | To explore the geographical differences in the uptake of general ophthalmic services |
| Sukumar et al. 200963 | 1995–2005 | England, UK | Retrospective study | 113 glaucoma patients | To investigate the relationship between socioeconomic status and the extent of visual field loss in glaucoma and treated ocular hypertension patients at their first presentation to eye clinic |
| Van der Pols et al. 199956 | 1994–1995 | UK | Cross-sectional study | 1275 subjects with a successful measurement of distance visual acuity and no mental impairment | To investigate the time since a last eye test and relations to socioeconomic factors |
| Wallace et al. 200864 | 1990–1999 | UK | Retrospective case note review and a cross-sectional interview of 29 patients | 87 case notes and 29 patients registered blind with glaucoma were interviewed | To study patient characteristics and management profile in advanced glaucoma |
| Waqar et al. 201238 | 2009–2010 | England, UK | Retrospective study | 2137 patients who did not attend diabetic retinopathy screening | To ascertain the relationship between socioeconomic status and non-attendance alongside the role of geodemographic analysis in identifying reasons for non-attendance |
| Yip et al. 201370 | 2004–2011 | UK, England | Multi-centre prospective study | 8467 persons with completed eye examinations | Prospective investigation into the relationship between area deprivation and poor vision |
| Yip et al. 201472 | 2004–2011 | UK | Cross-sectional study within a longitudinal cohort study | 5344 pairs of fundus photos | Investigate relationship between area deprivation, SES, and AMD |
| AMD patients |
Socioeconomic
Patel et al.36 reported that British women from lower socioeconomic groups are less likely to have an optometry eye examination. The reason for this inequality is uncertain, but the authors postulate the cost of this service as the potential cause. Concurrently, Shickle and Farragher37 found that eye examinations were 71% more likely in the least deprived areas than in the most deprived areas, despite equal entitlement between groups.
A review investigating inequalities accessing eye services in the UK found an association poor SES and poor attendance of eye health services38–56; late stage of eye disease at presentation to eye services57–64; uncorrected refractive error65,66; increased waiting times for treatment67,68; and poor treatment compliance.64,69 Articles meeting the inclusion criteria have been extracted and evaluated in Tables 2 and 5. There was an equal split between articles reporting no association and those reporting a significant association between poor SES and access to eye services. The authors suggest that this is due to a number of the articles investigating access to eye services as a secondary research question70. Two further studies remarked that as eye care is the only fee-paying service in the UK, and the cost of using this service could explain this possible health inequality.36,37 One study proposed free universal public provision to tackle income effects in up taking health care.54
One article, reported an association between poor SES and reduced vision, which was not significant.71 They concluded that the true reason for this association was the higher rate of uncorrected refractive error within the manual working class groups. They recommended that targeting uncorrected refractive error within deprived areas may have the potential to reduce this inequality. An additional study concurred with these findings and reported uncorrected refractive error was associated with younger age, male sex, increased deprivation and non-white ethnicities.72
As noted previously with age-related inequalities, some ocular conditions are more prevalent in lower socioeconomic groups; namely, glaucoma and AMD.60,73 Those from lower SES groups have been reported to present with glaucoma at significantly later stages than those of higher SES,59,60 although Fraser et al.60 added that family history and time since last optometry visit also played a key role in this statistic. As mentioned previously, this places more deprived individuals at a significant disadvantage and at high risk of irreversible visual loss. Poor diet and increased rates of smoking and stress associated with lower SES are reportedly the cause of this progression of glaucoma.60 Day et al.59 concluded that it is not acceptable to rely on high-street opticians to detect glaucoma in these areas of high deprivation and recommended the development of outreach services to tackle this concerning issue.
Furthermore, Yip et al.73 reported higher levels of deprivation with AMD patients due to associated increased rates of smoking and lower levels of physical and academic education within this group. As smoking is a significant risk factor of AMD, they propose the potential lack of understanding regarding the risks of smoking suggested by the lower levels of education as the cause of this inequality.
Gender
Three articles discussing gender-related health inequalities and visual impairment reported that women were at a higher risk of visual impairment71–73 potentially due to the higher prevalence of particular ocular diseases within females. Yip et al.73 found a significant association of AMD prevalence within the female population only. The authors found that this risk was indirectly influenced by SES due to a mutual association of risk factors such as smoking and poor diet.73 Another study reported that more women were taking up eye examinations in Leeds (UK), indicating an increased prevalence of visual impairment within the female population,37 although this was not found to be statistically significant when compared to the male population utilising ophthalmic services.
Age
All of the articles reporting age-related health inequalities and visual impairment (n = 6) concluded that older age was significantly associated with greater health inequalities.36,37,59,72,73 Older persons with visual impairment living in deprived areas are significantly less likely to take up eye examinations, suggesting an association between inequalities of older age and low SES.37 Moreover, a study of solely female participants reported that women >65 years old and of manual social class were less likely to take up eye examinations in the UK.36 They postulate that the cost of having an eye assessment may be a determining factor for this group. Another study reported that participants of both genders in this same age group were 3 times more likely to be visually impaired than those under 65 years old.71
The prevalence of various ocular diseases has shown to increase with age.59,73 Day et al.59 conducted a study to map the profile of glaucoma in Leeds and found that older persons are accessing glaucoma services at a later stage. This highlights a potentially significant inequality, as late presentation of glaucoma can result in irreversible loss of the patients’ visual acuity.
Education
Four articles reported an association between lower levels of education attainment and higher rates of visual impairment.60,71,73 Two articles reported a connection between lower levels of education and lower SES, which has further been associated with reduced vision in these deprived groups.71,73 Yip et al.73 reported that those with A-levels were significantly less likely to develop AMD than those without O-levels due to a lack of education and understanding of health risk factors.
Fraser et al.60 found that those who left full-time education by age 14 were more likely to present to an optician with glaucoma at a later stage than those who carried on in full-time education; however, this association was not statistically significant.
Occupation
One study found an association with increased risk of unemployment in individuals with reduced vision, even in those with mildly reduced vision in one eye.72 Those with the most severe grade of visual impairment had 3 times the risk of unemployment. Visually impaired individuals who can work are more likely to have a lower-grade job and are associated with living in sheltered accommodation as a result of their visual impairment.72
Transport
One article was identified in the literature search that discussed transport issues for the visually impaired population.74 The authors identified a number of inequalities relating to mobility and access to transport services through focus groups. They discussed the difficulty of using buses, as wheelchairs were often not admitted on board whilst many sight-impaired persons required this service.74 Furthermore, the high cost of frequent taxis when transport by bus or train was not possible posed a further inequality. Moreover, when it is possible to use public transport, many visually impaired patients found this to be very stressful due to lack of confidence as a result of their sight impairment.74
Those living in rural areas are at a further disadvantage, as night buses are less available in those areas. When transport options are restricted, this results in increased dependency on family or friends to take them to appointments, which limits the patients’ access to medical, social, and rehabilitative services.74
Conclusion
Only two articles aimed to investigate health inequalities affecting stroke survivors in the UK with visual impairment. These identified significant inconsistency in eye care provision nationally, along with variability in the assessment and management of visual disorders. However, the authors recognise the potential perceived bias, as these articles were co-written by one of the authors. To reduce bias, the review was opened up to include international articles outside of the UK and Ireland, which discussed health inequalities due to post-stroke visual impairment, although the findings should be interpreted cautiously, as differences in ethnicity, lifestyle factors, and private health care systems in these countries could yield inequalities unlikely to be experienced in the UK. These additional two articles discussed gender inequalities in visually impaired stroke survivors; women are more likely to present with visual field loss, men more likely to present with ocular motility defects, and both have equal risk of neglect.11,12
Our review further identified the following stroke and visually impaired subgroups as most at risk of health inequalities in the UK and Ireland: lower SES, older age, females, and those with lower education attainment. Black ethnic groups have poorer stroke outcomes than whites and Asians, and Asians have poorer outcomes than whites. Health inequalities facing these populations range from likelihood of having a stroke or vision problem to limited access to health care resources. These findings highlight a requirement for further research in which to develop strategies to overcome these established inequalities. Many of the subcategories named are associated with one another, e.g., females’ increased risk of stroke due to their association with socioeconomic deprivation, which in turn is related to the increased rates of risk factors found in socially deprived areas (e.g., smoking). Therefore, the full trajectories of these inequalities should be considered when addressing these issues.
Stroke survivors often suffer from a wide range of visual deficits; however, there is a specific gap in the literature in relation to health inequalities facing this population. Due to this lack of research, it has often only been possible to speculate the potential inequalities; therefore, further research must be conducted in order to establish whether or not this population are at risk of the aforementioned sociodemographic and economic inequalities.
Funding Statement
This research is funded by the National Institute of Health Research (CLAHRC NWC). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the department of health.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the article.
Funding
This research is funded by the National Institute of Health Research (CLAHRC NWC).
The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the department of health.
References
- [1].Hepworth LR, Rowe FJ, Walker MF, Rockliffe J, Noonan C, Howard C, Currie J. Post-stroke visual impairment: a systematic literature review of types and recovery of visual conditions. Ophthalmol Res 2016;5:1–43. [Google Scholar]
- [2].Rowe FJ, Walker M, Rockliffe J, Pollock A, Noonan C, Howard C, Hepworth L, Glendinning R, Currie J. Care provision and unmet needs for post stroke visual impairment; United Kingdom: The Stroke Association and Thomas Pocklington Trust, 2013:1–48. [Google Scholar]
- [3].Scarborough P, Peto V, Bhatnagar P, Kaur A, Leal J, Luengo-Fernandez R, Gray A, Rayner M, Alleder S. Stroke Statistics. Oxford, UK: University of Oxford: Department of Public Health; 2009:1–107 [Google Scholar]
- [4].Lynch JW, Kaplan GA, Salonen JT.. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc Sci Med 1997;44:809–819. [DOI] [PubMed] [Google Scholar]
- [5].Access Economics Limited Future Sight Loss UK 1: Economic Impact of Partial Sight and Blindness in the UK Adult Population. London, UK: The Royal National Institute of Blind People; 2009. [Google Scholar]
- [6].Elm EV, Altman DG, Egger M, Pocok SJ, Gotzsche PC, Vandenbroucke JP.. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Prev Med 2007;45:247–251. [DOI] [PubMed] [Google Scholar]
- [7].Rowe FJ. Who sees visual impairment following stroke? Strabismus 2010;18:37–40. [DOI] [PubMed] [Google Scholar]
- [8].Rowe FJ, Walker M, Rockliffe J, Pollock A, Noonan C, Howard C, Glendinning R, Feechan R, Currie J. Care provision for poststroke visual impairment. J Stroke Cardiovasc Dis 2015;24:1131–1144. [DOI] [PubMed] [Google Scholar]
- [9].Rowe FJ. Accuracy of referrals for visual assessment in a stroke population. Eye 2011;25:161–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].National Institute for Health and Care Excellence NICE Pathways—mapping our guidance. https://pathways.nice.org.uk/. Published 2016. Accessed 3 March 2017.
- [11].Gall SL, Donnan G, Dewey HM, Macdonell R, Sturm J, Gilligan A, Srikanth V, Thrift AG. Sex differences in presentation, severity, and management of stroke in a population-based study. Neurology 2010;74:975–981. [DOI] [PubMed] [Google Scholar]
- [12].Jerath NU, Reddy C, Freeman WD, Jerath AU, Brown RD.. Gender differences in presenting signs and symptoms of acute ischemic stroke: a population-based study. Gender Med 2011;8:312–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Hart CL, Hole DJ, Davey Smith G.. The contribution of risk factors of stroke differnetials, by socioeconomic position in adulthood: the Renfrew/Paisley study. Am J Public Health 2000;90:1788–1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kerr GD, Higgins P, Walters M, Ghosh SK, Wright F, Langhorne P, Stott DJ. Socioeconomic status and transient ischaemic attack/stroke: a prospective observational study. Cerebrovasc Dis 2011;31:130–137. [DOI] [PubMed] [Google Scholar]
- [15].Heuschmann PU, Grieve AP, Toschke AM, Rudd AG, Wolfe CDA.. Ethnic group disparities in 10-year trends in stroke incidence and vascular risk factors: the South London Stroke Register (SLSR). Stroke 2008;39:2204–2210. [DOI] [PubMed] [Google Scholar]
- [16].McFadden E, Luben R, Wareham N, Bingham S, Khaw K-T.. Social class, risk factors, and stroke incidence in men and women: a prospective study in the European Prospective Investigation Into Cancer in Norfolk Cohort. Stroke 2009;40:1070–1077. [DOI] [PubMed] [Google Scholar]
- [17].Chen R, McKevitt C, Rudd AG, Wolfe CDA.. Socioeconomic deprivation and survival after stroke: findings from the Prospective South London Stroke Register of 1995 to 2011. Stroke 2014;45:217–223. [DOI] [PubMed] [Google Scholar]
- [18].Kunst AE, del Rios M, Groenhof F, Machenbach JP.. Socioeconomic inequalities in stroke mortality among middle aged men. Stroke 1998;29:2285–2291. [DOI] [PubMed] [Google Scholar]
- [19].Addo J, Bhalla A, Crichton S, Rudd AG, McKevitt C, Wolfe CDA.. Provision of acute stroke care and associated factors in a multiethnic population: prospective study with the South London Stroke Register BMJ 2011;342:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Chen R, Crichton S, McKevitt C, Rudd AG, Sheldenkar A, Wolfe CDA.. Association between socioeconomic deprivation and functional impairment after stroke: the South London Stroke Register. Stroke 2015;46:800–805. [DOI] [PubMed] [Google Scholar]
- [21].McCartney G, Russ TC, Walsh D, Lewsey J, Smith M, Davey Smith G, Stamatakis E, Batty GD. Explaining the excess mortality in Scotland compared with England: pooling of 18 cohort studies. J Epidemiol Community Health 2015;69:20–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Busch MA, Coshall C, Heuschmann PU, McKevitt C, Wolfe CDA.. Sociodemographic differences in return to work after stroke: the South London Stroke Register (SLSR). J Neurol Neurosurg Psychiatry 2009;80:888–893. [DOI] [PubMed] [Google Scholar]
- [23].Redfern J, McKevitt C, Rudd AG, Wolfe CDA.. Health care follow up after stroke: opportunities for secondary prevention. Fam Pract 2002;19:378–382. [DOI] [PubMed] [Google Scholar]
- [24].Wolfe CDA, Rudd AG, Howard R, Coshall C, Stewart J, Lawrence E, Hajat C, Hillen T. Incidence and case fatality rates of stroke subtypes in a multiethnic population: the south London stroke register. J Neurol Neurosurg Psychiatry 2002;72:211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Wang Y, Rudd AG, Wolfe CDA.. Age and ethnic disparities in incidence of stroke over time. The South London Stroke Register. Stroke 2013;44:3298–3304. [DOI] [PubMed] [Google Scholar]
- [26].McKevitt C, Coshall C, Tilling K, Wolfe C.. Are there inequalities in the provision of stroke care? Analysis of an inner-city stroke register. Stroke 2005;36:315–320. [DOI] [PubMed] [Google Scholar]
- [27].Wolfe CD, Smeeton NC, Coshall C, Tilling K, Rudd AG Survival differences after stroke in a multiethnic population: follow-up study with the South London Stroke Register. BMJ 2005;331:431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Bhopal RS, Bansal N, Fischbacher CM, Brown H, Capewell S.. Ethnic variations in the incidence and mortality of stroke in the Scottish Health and Ethnicity Linkage Study of 4.65 million people. Eur J Prev Cardiol 2012;19:1503–1508. [DOI] [PubMed] [Google Scholar]
- [29].Hajat C, Dundas R, Stewart JA, Lawrence E, Rudd AG, Howard R, Wolfe CDA. Cerebrovascular risk factors and stroke subtypes: differences between ethnic groups. Stroke 2001;32:37–42. [DOI] [PubMed] [Google Scholar]
- [30].Smeeton NC, Heuschmann PU, Rudd AG, McEvoy AW, Kitchen ND, Sarker SJ, Wolfe CD. Incidence of hemorrhagic stroke in black Caribbean, black African, and white populations: the South London Stroke Register, 1995–2004. Stroke 2007;38(:3133–3138. [DOI] [PubMed] [Google Scholar]
- [31].Banjeree S, Biram R, Chataway J, Ames D.. South Asian strokes: lessons from the St Mary’s Stroke Database. Q J Med 2010;103:17–21. [DOI] [PubMed] [Google Scholar]
- [32].Raine R, Wong W, Ambler G, Hardoon S, Petersen I, Morris R, Bartley M, Blane D. Sociodemographic variations in the contribution of secondary drug prevention to stroke survival at middle and older ages: cohort study. BMJ 2009;338:b1279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Lazzarino AI, Palmer W, Bottle A, Aylin P.. Inequalities in stroke patients’ management in English public hospitals: a survey on 200,000 patients. PLoS ONE 2011;6:(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Power C, Hypponen E, Smith GD.. Socioeconomic position in childhood and early adult life and risk of mortality: a prospective study of the mothers of the 1958 British birth cohort. Am J Public Health 2005;95:1396–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Putman K, De Wit L, Schoonacker M, Baert I, Beyens H, Brinkmann N, Dejaeger E, De Meyer AM, De Weerdt W, Feys H De Weerdt W, Jenni W, Kaske C, Leys M, Lincoln N, Schuback B, Schupp W, Smith B, Louckx F.. Effect of socioeconomic status on functional and motor recovery after stroke: a European multicentre study J Neurol Neurosurg Psychiatry 2007;78:539–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Patel R, Lawlor DA, Ebrahim S.. Socio-economic position and the use of preventive health care in older British women: a cross-sectional study using data from the British Women’s Heart and Health Study cohort. Fam Pract 2007;24:7–10. [DOI] [PubMed] [Google Scholar]
- [37].Shickle D, Farragher TM.. Geographical inequalities in uptake of NHS-funded eye examinations: small area analysis of Leeds, UK. J Public Health 2015;37:337–345. [DOI] [PubMed] [Google Scholar]
- [38].Waqar S, Bullen G, Chant S, Salman R, Vaidya B, Ling R.. Cost implications, deprivation and geodemographic segmentation analysis of non-attenders (DNA) in an established diabetic retinopathy screening programme. Diabetes Metab Syndr Clin Res Rev 2012;6:199–202. [DOI] [PubMed] [Google Scholar]
- [39].Nessim M, Denniston AK, Nolan W, Holder R, Shah P.. Research into Glaucoma and Ethnicity (ReGAE) 8: is there a relationship between social deprivation and acute primary angle closure? Br J Ophthalmol 2010;94:1304–1306. [DOI] [PubMed] [Google Scholar]
- [40].Bachmann MO, Eachus J, Hopper CD, Davey Smith G, Propper C, Pearson NJ, Williams S, Tallon D, Frankel S Socio-economic inequalities in diabetes complications, control, attitudes and health service use: a cross-sectional study. Diabet Med 2003;20:921–929. [DOI] [PubMed] [Google Scholar]
- [41].Buch HN, Barton DM, Varughese GI, Bradbury S, Scarpello JHB, Walker AB.. An assessment of the coverage of a district-wide diabetic retinopathy screening service. Diabet Med 2005;22:840–841. [DOI] [PubMed] [Google Scholar]
- [42].Chaturvedi N, Ben-Shlomo Y.. From the surgery to the surgeon: does deprivation influence consultation and operation rates? Br J Gen Pract 1995;45:127–131. [PMC free article] [PubMed] [Google Scholar]
- [43].Cookson R, Laudicella M, Donni PL.. Measuring change in health care equity using small-area administrative data—evidence from the English NHS 2001–2008. Soc Sci Med 2012;75:1514–1522. [DOI] [PubMed] [Google Scholar]
- [44].Dickey H, Ikenwilo D, Norwood P, Watson V, Zangelidis A.. Utilisation of eye-care services: the effect of Scotland’s free eye examination policy. Health Policy 2012;108:286–293. [DOI] [PubMed] [Google Scholar]
- [45].Gulliford MC, Dodhia H, Chamley M, McCormick K, Mohamed M, Naithani S, Sivaprasad S. Socio-economic and ethnic inequalities in diabetes retinal screening. Diabet Med 2010;27:282–288. [DOI] [PubMed] [Google Scholar]
- [46].Keenan T, Rosen P, Yeates D, Goldacre M.. Time trends and geographical variation in cataract surgery rates in England: study of surgical workload. Br J Ophthalmol 2007;91:901–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Keenan TDL, Salmon JF, Yeates D, Goldacre MJ.. Trends in rates of trabeculectomy in England. Eye 2009;23:1141–1149. [DOI] [PubMed] [Google Scholar]
- [48].Keenan TDL, Wotton CJ, Goldacre MJ.. Trends over time and geographical variation in rates of intravitreal injections in England. Br J Ophthalmol 2012;96:413–418. [DOI] [PubMed] [Google Scholar]
- [49].Kliner M, Fell G, Gibbons C, Dhothar M, Mookhtiar M, Cassels-Brown A.. Diabetic retinopathy equity profile in a multi-ethnic, deprived population in Northern England. Eye 2012;26:671–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Leese GP, Boyle P, Feng Z, Emslie-Smith A, Ellis JD.. Screening uptake in a well-established diabetic retinopathy screening program. The role of geographical access and deprivation. Epid Health Ser Res 2008;31:2131–2135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Millett C, Dodhia H.. Diabetes retinopathy screening: audit of equity in participation and selected outcomes in South East London. J Med Screen 2006;13:152–155. [DOI] [PubMed] [Google Scholar]
- [52].Owen CG, Carey IM, De Wilde S, Whincup PH, Wormald R, Cook DG.. The epidemiology of medical treatment for glaucoma and ocular hypertension in the United Kingdom: 1994 to 2003. Br J Ophthalmol 2006;90:861–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Rahi JS, Peckham CS, Cumberland PM.. Visual impairment due to undiagnosed refractive error in working age adults in Britain. Br J Ophthalmol 2008;92:1190–1194. [DOI] [PubMed] [Google Scholar]
- [54].Sabates R, Feinstein L.. Do income effects mask social and behavioural factors when looking at universal health care provision? Int J Public Health 2008;53:23–30. [DOI] [PubMed] [Google Scholar]
- [55].Scanlon PH, Carter SC, Foy C, Husband RFA, Abbas J, Bachmann MO.. Diabetic retinopathy and socioeconomic deprivation in Gloucestershire. J Med Screen 2008;15:118–121. [DOI] [PubMed] [Google Scholar]
- [56].Van der Pols JC, Thompson JR, Bates CJ, Pentice A, Finch S.. Is the frequency of having an eye test associated with socioeconomic factors? A national cross sectional study in British elderly. J Epidemiol Community Health 1999;53:737–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Ng WS, Agarwal PK, Sidiki S, McKay L, Townend J, Azuara-Blanco A.. The effect of socio-economic deprivation on severity of glaucoma at presentation. Br J Ophthalmol 2010;94:85–87. [DOI] [PubMed] [Google Scholar]
- [58].Acharya N, Lois N, Townend J, Zaher S, Gallagher M, Gavin M.. Socio-economic deprivation and visual acuity at presentation in exudative age-related macular degeneration. Br J Ophthalmol 2009;93:627–629. [DOI] [PubMed] [Google Scholar]
- [59].Day F, Buchan JC, Cassells-Brown A, Fear J, Dixon R, Wood F.. A glaucoma equity profile: correlating disease distribution with service provision and uptake in a population in Northern England, UK. Eye 2010;24:1478–1485. [DOI] [PubMed] [Google Scholar]
- [60].Fraser S, Bunce C, Wormald R, Brunner E.. Deprivation and late presentation of glaucoma: case-control study. BMJ 2001;322:639–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Lockington D, Chadha V, Russell H, Young D, Cauchi P, Kemp E.. Socioeconomic status and choroidal melanoma in Scotland. Arch Ophthalmol 2010;128:383–384. [DOI] [PubMed] [Google Scholar]
- [62].Saidkasimova S, Mitry D, Singh J, Yorston D, Charteris DG.. Retinal detachment in Scotland is associated with affluence. Br J Ophthalmol 2009;93:1591–1594. [DOI] [PubMed] [Google Scholar]
- [63].Sukumar S, Spencer F, Fenerty C, Harper R, Henson D.. The influence of socioeconomic and clinical factors upon the presenting visual field status of patients with glaucoma. Eye (Lond) 2009;23:1038–1044. [DOI] [PubMed] [Google Scholar]
- [64].Wallace EJ, Paterson H, Miller S, Sinclair A, Sanders R, Hinds A.. Patient profile and management in advanced glaucoma. Br J Vis Impair 2008;26:7–23. [Google Scholar]
- [65].Cox A, Blaikie A, MacEwen CJ, Jones D, Thompson K, Holding D, Sharma T, Miller S, Dobson S, Sanders R Visual impairment in elderly patients with hip fracture: causes and associations. Eye 2004;19:652–656. [DOI] [PubMed] [Google Scholar]
- [66].Sherwin JC, Khawaja AP, Broadway D, Luben R, Hayat S, Dalzell N, et al. Uncorrected refractive error in older British adults: the EPIC-Norfolk Eye Study. Br J Ophthalmol 2012;96:991–996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Hacker J, Stanistreet D.. Equity in waiting times for two surgical specialties: a case study at a hospital in the North West of England. J Public Health 2004;26:56–60. [DOI] [PubMed] [Google Scholar]
- [68].Cooper ZN, McGuire A, Jones S, Grand JL.. Equity, waiting times, and NHS reforms: retrospective study. BMJ 2009;339:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Owen CG, Carey IM, de Wilde S, Whincup PH, Wormald R, Cook DG.. Persistency with medical treatment for glaucoma and ocular hypertension in the United Kingdom: 1994–2005. Eye 2009;23:1098–1110. [DOI] [PubMed] [Google Scholar]
- [70].Knight A, Lindfield R.. The relationship between socio-economic status and access to eye health services in the UK: a systematic review. Public Health. 2015;129(2):94–102. [DOI] [PubMed] [Google Scholar]
- [71].Yip JLY, Luben R, Hayat S, Khawaja AP, Broadway DC, Wareham N, Khaw KT, Foster PJ. Area deprivation, individual socioeconomic status and low vision in the EPIC-Norfolk Eye Study. J Epidemiol Community Health 2013(0):1–7. doi: 10.1136/jech-2013-203265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Cumberland PM, Rahi JS, for the UKBE, Vision C Visual function, social position, and health and life chances: the UK Biobank Study. JAMA Ophthalmol 2016;134(9):959–66. [DOI] [PubMed] [Google Scholar]
- [73].Yip JLY, Khawaja AP, Chan MPY, Broadway DC, Peto T, Luben R, et al. Area deprivation and age related macular degeneration in the EPIC-Norfolk Eye Study. Public Health 2015;129:103–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Gallagher BAM, Hart PM, O’Brien C, Stevenson MR, Jackson AJ.. Mobility and access to transport issues as experienced by people with vision impairment living in urban and rural Ireland. Disabil Rehabil 2011;33:979–988. [DOI] [PubMed] [Google Scholar]


