Abstract
Zambia and other sub-Saharan nations suffer from a critical shortage of trained health-care professionals to combat the human immunodeficiency virus/acquired immunodeficiency syndrome crisis. The University of Maryland and the Zambian Ministry of Health have partnered over the past decade to develop health-care capacity among physicians, nurses, and community health workers. We describe novel interventions to train health-care workers at all levels and argue that our collaboration represents a successful model for such partnerships between western medical institutions and African governmental health agencies.
Perspective: The University of Maryland Baltimore–Zambian Ministry of Health Collaboration
From the initial announcement of the President's Emergency Plan for AIDS Relief (PEPFAR) to the current PEPFAR 3.0, a deficit persists in the number and capacity of clinicians needed to implement human immunodeficiency virus (HIV) care and treatment programs in sub-Saharan Africa. By 2002, Zambia had an adult HIV prevalence of 15.6%1 and an estimated 920,000 adults and children living with HIV.2 By 2005, the country had only 646 doctors in government facilities,3 and little expertise in HIV management. In response to this crisis, the University of Maryland Baltimore (UMB) has developed a model partnership with the Zambian Ministry of Health (MoH) to address the HIV epidemic by training and deploying health-care professionals to meet the health-care needs of Zambia.
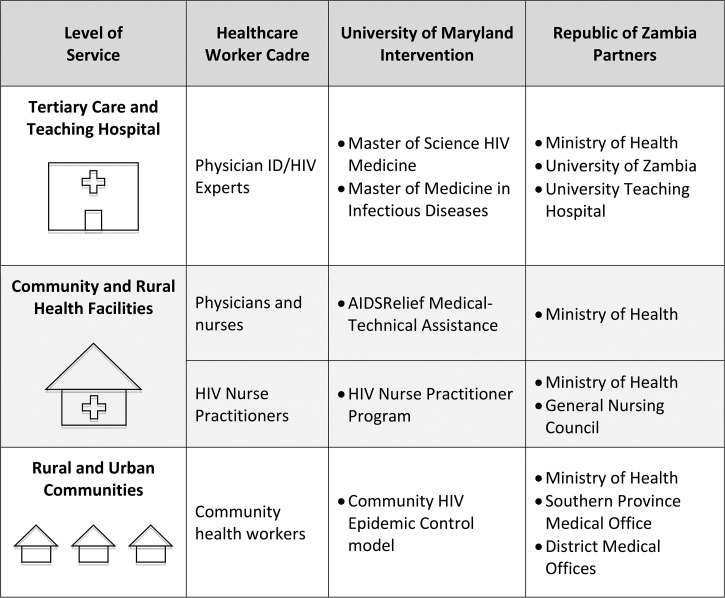
In 2006, Zambian President Levy Mwanawasa visited Baltimore to meet with Robert Gallo and Robert Redfield, cofounders of the UMB Institute of Human Virology. Together they envisioned overcoming the health workforce challenge in Zambia, and UMB embarked on a multipronged approach toward expanding health worker capacity using four strategies in phases: technical assistance and clinical mentorship, task shifting to nurses, advanced clinical training for doctors, and expansion of community health initiatives (Figure 1 ). UMB also temporarily embedded a Zambian U.S.-trained infectious disease physician in the MoH to support and advise on the national antiretroviral therapy (ART) program.
Figure 1.
Depiction of University of Maryland interventions with Zambian governmental partners to develop health-care worker capacity at all levels of health service delivery in Zambia. All interventions were funded by the U.S. Center for Disease Control and Prevention and the President's Emergency Plan for AIDS Relief.
Mentoring in the Clinic: AIDSRelief Medical–Technical Assistance
UMB started working in Zambia in 2004 with Catholic Relief Services under the AIDSRelief consortium to support rapid ART scale-up throughout the country. As the medical partner, UMB provided technical assistance and in-service clinical mentorship on ART, HIV testing and counseling, and maternal–infant HIV care for doctors, clinical officers, and nurses at 19 treatment sites. By 2012, AIDSRelief clinics had provided HIV care and treatment to over 96,000 patients in Zambia, including more than 60,000 enrolled on ART.4
Task Shifting to Nurses: Development of HIV Nurse Practitioner Program
To address the physician shortage, UMB partnered with the General Nursing Council (GNC) of Zambia and the University of Alabama in 2009 to create the HIV Nurse Practitioner (HNP) course, which trained nurses in HIV diagnosis, first-line ART initiation and monitoring, adherence counseling, and management of opportunistic infections.5 There was no precedent for this new cadre of health-care workers and the program initially faced resistance from physicians; this was overcome by working to present the concept of task shifting to all stakeholders, including the GNC, Health Professions Council of Zambia, Zambia Medicines Regulatory Authority, and the Medical Association of Zambia. Other challenges faced by the program included continued funding and identification of sufficient mentors but these were solved in time by commitments from MoH.
The 1-year curriculum developed by UMB and adapted by the GNC consists of 6 weeks of didactics and intensive mentorship, after which the nurses complete the course at their own facility under supervision, thus preventing health-care staff shortages during training. Begun in 2009, UMB sponsored 31 nurses in the first 3 years of the program; 24 still practice at their respective facilities while five now serve as mentors in the program. The program was then integrated into the University of Zambia (UNZA) School of Nursing and graduates continue to provide high-quality HIV care in clinics throughout Zambia.6 By 2015, 169 nurses had completed the HNP training, with 33 more enrolled in training. A recent evaluation demonstrates that the HNPs are viewed positively by their supervisors.7
Advanced Physician Education: Postgraduate Training in HIV Medicine and Infectious Diseases
With expansion of HIV care in the early 2000s, physician-level expertise was required to diagnose and treat seriously ill HIV-infected patients, manage rapidly growing populations on ART (including drug side effects, treatment failures, and drug resistance), and manage health service delivery and guide national policy. UMB partnered with the MoH, University Teaching Hospital (UTH) in Lusaka, UNZA School of Medicine, and the U.S. Centers for Disease Control and Prevention (CDC) in Zambia to create a program to train HIV physician specialists to provide expert HIV care and train other health-care workers. UMB developed the curricula for the course, worked with the UNZA Senate to approve the course and materials, and participated in selection of candidates from within the MOH, the military, and the private sector.
The postgraduate diploma in HIV Medicine started in 2008 as a 1-year course focused on advanced adult and pediatric HIV medicine, management of opportunistic infections, laboratory medicine, clinical teaching skills, and research design and implementation.8 The hallmark of the program was supervised clinical mentorship of trainees. UMB faculty provided clinical preceptorship on every outpatient and inpatient seen by the trainees. Together, UMB and UTH provided a robust teaching program that included journal clubs, case conferences, HIV treatment failure conferences, and research conferences. To recognize their expertise and enhance opportunities for career advancement, the course was extended to include a 6-month research component and the diploma program was elevated to a master of science in HIV Medicine (MSc. HIV) from UNZA. The diploma and MSc. HIV programs together trained 27 doctors, 24 of whom still work in HIV care in Zambia today. Former participants currently play key leadership roles in HIV treatment and policy in Zambia; 15 graduates work at the MoH while others are employed at CDC-Zambia, UNZA, UMB, and other governmental and nongovernmental institutions.
To address the broader burden of infectious diseases among HIV-infected and uninfected individuals alike, UMB recognized a need for higher level comprehensive infectious diseases expertise in Zambia. Thus, in 2012, UMB and UNZA created the master of medicine in infectious diseases (MMed ID) program to train doctors as specialists to provide and teach advanced HIV and infectious disease medicine. Although the MSc. HIV was an 18-month course focused on clinical care of HIV-infected patients, the MMed ID program is a comprehensive 5-year residency that includes training in internal medicine, infectious diseases, and advanced HIV medicine. UMB infectious diseases faculty, including a U.S.-trained Zambian national, reside full time in Zambia and provide clinical teaching and oversight of trainees; together they staff the infectious diseases consult service at UTH, seeing over 1,000 inpatient consultations per year. Along with MoH and other partners, UMB developed the Advanced Treatment Center for patients with complicated HIV, currently treating 312 patients on third-line ART. UMB faculty also teaches UNZA medical students HIV medicine and infectious diseases. The MMed ID program is now in its 4th year with the first cohort expected to graduate in 2017. Although it was argued that infectious disease medicine was adequately learned in internal medicine training and a separate MMed ID program was not necessary, this resistance was overcome by demonstrating the value of the infectious diseases team to patient management.
Increasing Community Clinical Capacity: The Community HIV Epidemic Control Model
As clinical, public health, and human rights arguments have aligned toward universal treatment, Zambia required novel methods of service delivery to achieve the UNAIDS goals of identifying 90% of persons with HIV, providing ART to 90% of known infected persons, and achieving viral suppression in 90% of those on ART. To meet the demands for more patients, higher retention, and better adherence, UMB developed the Community HIV Epidemic Control (CHEC) model that expands the HIV care continuum and task-shifts care into the community. CHEC community health workers (CHWs) offer door-to-door HIV testing, health assessment, adherence support, and personal health messaging. Each CHW is equipped with a tablet linked to the national electronic health record to enable reporting and long-term follow-up. The CHW immediately refers persons testing HIV-positive to a health-care facility, provides care navigation support, and ensures patients remain in care and adhere to treatment.
Since 2015, UMB has implemented the CHEC model in over 100 sites in Zambia, with more than 400 CHWs trained and deployed. In the 1st year of CHEC implementation, HIV testing increased 339%, from 21,051 to 71,289 clients; of these clients, 20,623 (28.9%) were tested in the community.
A Model for Effective Medical Partnership
By developing global partnerships, academic health centers such as UMB can play a unique role as incubators and innovators of novel interventions, and are poised to accelerate replication of proven solutions through research, education, and systems development. For diseases with existing highly effective prevention or treatment, such as HIV, expanded and strategic application of existing knowledge yield more immediate intermediate benefit than additional research.9 Medical education exchanges are increasingly common10 and can have a substantial benefit,11 but run the risk of limited skill transfer to the receiving country. If the needs of the host country are not the highest priority, we risk global health neocolonialism, garnering research grants and medical tourism from resource-limited health systems while draining talented health-care providers and researchers from the public sector.
The UMB-Zambian MoH partnership fosters a collaborative response to changing health needs, thereby assisting Zambia in achieving HIV epidemic control. Using a phased strategy, UMB and the MoH have partnered to train the health-care workforce to handle the challenges of an evolving epidemic. We propose that this model of collaborative education partnership represents a durable method for achieving high-quality health care and sustainable health systems in countries severely afflicted by HIV.
ACKNOWLEDGMENTS
We thank their collaborators at the Ministry of Health for their committed partnership over the past decade and the contributing faculty from the University of Maryland. We also thank the doctors, nurses, and community health workers of Zambia, whose dedication to the health of their fellow Zambians made this effort possible.
Footnotes
Authors' addresses: Cassidy W. Claassen and Lottie Hachaambwa, Institute of Human Virology, University of Maryland School of Medicine, Baltimore, MD, Maryland Global Initiatives Corporation, University of Maryland School of Medicine, Lusaka, Zambia, and Department of Medicine, University of Zambia School of Medicine, Lusaka, Zambia, E-mails: cclaassen@ihv.umaryland.edu and lhachaambwa@ihv.umaryland.edu. Dorcas Phiri, Maryland Global Initiatives Corporation, University of Maryland School of Medicine, Lusaka, Zambia, E-mail: dphiri@mgic.umaryland.edu. Douglas C. Watson, Department of Pediatrics, University of Maryland School of Medicine, Baltimore, MD, E-mail: dwatson@peds.umaryland.edu. Devang Patel, Deus Mubangizi, and Robert Redfield, Institute of Human Virology, University of Maryland School of Medicine, Baltimore, MD, E-mails: dpatel@ihv.umaryland.edu, dmubangizi@ihv.umaryland.edu, and rredfield@ihv.umaryland.edu. Christopher M. Bositis and Amy Bositis, Greater Lawrence Family Health Center, Lawrence, MA, E-mails: cbositis@glfhc.org and amy.bositis@glfhc.org. Peter Mwaba, Office of the Permanent Secretary, Ministry of Health, Lusaka, Zambia, E-mail: pbmwaba2000@gmail.com. Robb Sheneberger, Institute of Human Virology, University of Maryland School of Medicine, Baltimore, MD, and Maryland Global Initiatives Corporation, University of Maryland School of Medicine, Lusaka, Zambia, E-mail: rsheneberger@ihv.umaryland.edu.
References
- 1.Central Statistical Office, Central Board of Health, ORC Macro . Zambia Demographic and Health Survey 2001–2002. Calverton, MD: Central Statistical Office, Central Board of Health, and ORC Macro; 2003. [Google Scholar]
- 2.UNAIDS/WHO . Epidemiological Fact Sheet Zambia. Geneva, Switzerland: UNAIDS; 2004. [Google Scholar]
- 3.Ministry of Health . National Human Resources for Health Strategic Plan 2011–2015. Lusaka, Republic of Zambia: Ministry of Health; 2011. [Google Scholar]
- 4.AIDSRelief AIDSRelief Zambia Final Report 2004–2012: Catholic Relief Services. 2013. www.crs.org/sites/default/files/tools-research/aidsrelief_zambia_final.pdf Available at. Accessed July 15, 2016.
- 5.Msidi E, Sinkala M, Bositis A, Guberski T, Katayamoyo P, Menke J, Montesanti A, Morris M, Mwale A, Mwanahamunutu F, Mweemba P, Ngoma RW, Phiri D, Wilson CM, Wilson L. The Zambian HIV nurse practitioner diploma programme: preliminary outcomes. Int J Nurs Educ Scholarsh. 2011;8:1–19. [Google Scholar]
- 6.Mulenga UH, Chanda D, Gashongore I, Katayamoyo P, Masebe EM, Mukanyimi B, Mukupo F, Mulenga L, Mulenga PL, Musamba B, Mutemi D, Mwanahamuntul FH, Mwango A, Mweemba P, Phiri D, Wahila-N R, Wilson L. Follow-up evaluation of first two cohorts of graduates of the Zambian HIV nurse practitioner program. Int J Africa Nursing Sci. 2015;2:1–9. [Google Scholar]
- 7.McCullock D, Chanda D, Masebe E, Mwale A, Wahila R, Wilson L. Supervisors' perceptions regarding the Zambian HIV nurse practitioner program and integrating graduates into the Zambian health system: a descriptive cross-sectional survey. J Nurs Educ Pract. 2016;6:140–150. [Google Scholar]
- 8.Hachaambwa LM, Zachary D, Sikazwe I, Lakhi S, Sheneberger R. B103 the Zambian Medical Education Program. J Acquir Immune Defic Syndr. 2013;62:35. [Google Scholar]
- 9.Gopal S. Moonshot to Malawi. N Engl J Med. 2016;374:1604–1605. doi: 10.1056/NEJMp1601982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McKinley DW, Williams SR, Norcini JJ, Anderson MB. International exchange programs and U.S. medical schools. Acad Med. 2008;83:S53–S57. doi: 10.1097/ACM.0b013e318183e351. [DOI] [PubMed] [Google Scholar]
- 11.Bodnar BE, Claassen CW, Solomon J, Mayanja-Kizza H, Rastegar A. The effect of a bidirectional exchange on faculty and institutional development in a global health collaboration. PLoS One. 2015;10:e0119798. doi: 10.1371/journal.pone.0119798. [DOI] [PMC free article] [PubMed] [Google Scholar]