Abstract
This study was conducted to investigate the prevalence of Blastocystis spp. and its subtypes (STs) in North Cyprus; and to evaluate the presence of this parasite and its STs with respect to demographic, socioeconomic, and epidemiological factors, as well as gastrointestinal symptoms. Stool samples were collected from 230 volunteers. Each participant also filled out a questionnaire. The samples were examined microscopically by native-Lugol and trichrome methods and further tested by polymerase chain reaction (PCR) and sequencing. Prevalence of Blastocystis spp. infection was found to be 10.5%, 10.5%, and 27.8%, by direct microscopy, trichrome method, and PCR, respectively. No other parasites were detected in the specimens except Giardia spp. (n = 2; 0.8%) and Entamoeba coli (n = 1; 0.4%). The most common Blastocystis STs were ST3 (20; 31.2%), ST2 (18; 28.2%), ST1 (8; 12.5%), and ST4 (7; 11%); whereas other STs were identified as ST6 (3; 4.7%), ST7 (2; 3.2%), and non-ST (6; 9.4%). Presence of Blastocystis spp. and its STs was not significantly related to any of the demographic, socioeconomic, and epidemiological factors. Furthermore, no significant association of Blastocystis spp. and its STs with gastrointestinal symptoms was found. This study is the first investigation of the epidemiology of Blastocystis spp. in North Cyprus. Distribution of Blastocystis spp. and its STs among demographic, socioeconomic, and epidemiological factors showed complete homogeneity. Presence of the parasite and its STs was not significantly related with the gastrointestinal symptoms among symptomatic and asymptomatic individuals. These findings suggest that Blastocystis spp. may be part of the intestinal flora in humans.
Introduction
Blastocystis spp. is the most widespread protists in the gastrointestinal tract of humans and in a variety of animal species.1–4 The routes of transmission of Blastocystis spp. are similar to those of other enteric parasites: the organisms can be acquired via fecal-oral pathway through contaminated food and water or by exposure to animals.5 Based on the molecular analyses, Blastocystis spp. comprises at least 17 subtypes (STs) nine of which have been reported in humans.6–11 Pathogenesis of blastocystosis still remains uncertain, as the organisms can be found in both symptomatic and asymptomatic patients.6 It has been proposed that the pathogenesis of Blastocystis spp. might be dependent on certain STs12,13; however, recent epidemiological studies remain contradictory.14 Clinical features of blastocystosis include abdominal pain, flatulence, constipation, bloating, vomiting, and acute or chronic diarrhea.3,15
The prevalence of Blastocystis spp. varies between 0.5% and 23.1% in developed countries and 22.1% and 100.0% in developing countries.1,2,15–20 Generally, the high prevalence of infection is associated with demographic, socioeconomic, and epidemiological factors.1,15,21,22 Although a large number of studies on Blastocystis spp. have been published, information on the epidemiology and pathogenesis of the disease is still lacking.5 Likewise, the prevalence and epidemiological profile of blastocystosis in North Cyprus have not been evaluated before. Hence, the primary goal of the present study was to investigate the prevalence of Blastocystis spp. and its STs in North Cyprus. The secondary purpose of the study was to evaluate the presence of this parasite and its STs with respect to demographic, socioeconomic, and epidemiological data; and to determine their role in gastrointestinal symptoms.
Materials and Methods
Study area and population.
A total of 230 volunteers who were living in North Cyprus were enrolled in this epidemiological study. North Cyprus, an island country, is situated in the northeast of the Mediterranean Sea and has the typical hot and dry Mediterranean climate. The country is located in 34° and 36° northern latitudes, and 32° and 35° eastern longitudes. North Cyprus is a developing country with a population of 313,626. The economy of the country is mainly provided by the public sector, trade, tourism, and education.
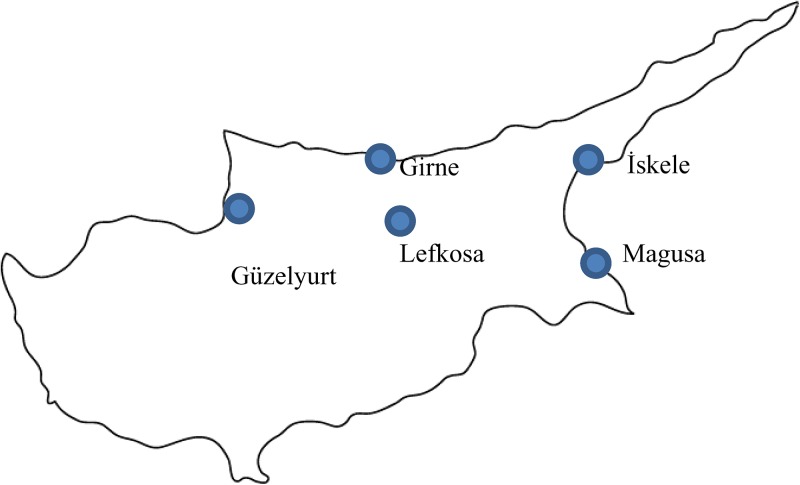
Stool samples were collected from both asymptomatic and symptomatic volunteers originating from main cities, Lefkosa, Girne, Guzelyurt, Iskele, Gazimagusa, and surrounding rural areas (Figure 1 ). The participants were preferably selected from adults and elderly individuals. Only one sample per participant was included in the study. The ethical approval for the study was obtained from the Clinical Research Ethics Board of Ankara Numune Training and Research Hospital, Turkey No/Year: E.Kurul-E-15-446/06.04.2015. Written informed consent was obtained from each participant. For the individuals under 18 years of age, the informed consent was collected from their parents.
Figure 1.
The cities where stool samples were collected for Blastocystis research, 2015, North Cyprus.
Questionnaire.
A standard questionnaire was applied to each participant to obtain a demographic (age, gender, marital status), socioeconomic (education, residence, occupation, economic income), and epidemiological (type of water supply, presence of domestic animals, travel history, general health conditions, presence of gastrointestinal symptoms such as abdominal pain, diarrhea, abdominal cramps, nausea, bloating, constipation) data.
Direct examination.
A total of 230 fresh human fecal samples were examined macroscopically in terms of consistency, and presence of pus, blood, and helminths. All samples were also examined microscopically by using both native-Lugol and trichrome-stained smears.23 Microscopic examination of the samples was performed double-blinded by two different experts.
Molecular assays.
For the molecular analysis of Blastocystis spp., two preservation techniques were used: conventional frozen stool (FS) and dried stool spots on filter paper (DSSFP) methods.24 DNA extraction was performed by following the manufacturer's protocol (EURx, GeneMATRIX Stool DNA Purification Kit, Gdansk, Poland). Briefly, a total of 70 mg from the fecal samples were used in each preservation method for the extraction of DNA with a final elution volume of 100 μL. For detection of small subunit rDNA gene (SSU-rDNA) of Blastocystis spp., primers BhRDr (GAGCTTTTTAACTGCAACAACG) and RD5 (ATCTGGTTGATCCTGCCAGT) were used in touch-down polymerase chain reaction (PCR) assay.24,25 Two microliters of DNA solution was added into the standard PCR mixture with a total volume of 25 μL. Sequencing of SSU-rDNA of the PCR products was analyzed by using the Blastocystis subtype (18S) and sequence typing database (MLST) (http://pubmlst.org/Blastocystis/) online software. Representative nucleotide sequences from this study were submitted to GenBank under accession numbers KY675320–KY675376.
Statistical analyses.
Statistical analyses were performed by using Stata software, version 21 (StataCorp, College Station, TX). The test was two sided, with a type I error set at α = 0.05. Association of Blastocystis spp. prevalence with demographic, socioeconomic, epidemiological, and clinical factors was evaluated by using Pearson χ2 test or Fisher's exact test. To test the distribution of Blastocystis STs according to demographic, socioeconomic, epidemiological, and clinical factors, the Wilcoxon signed-rank nonparametric test was used and P < 0.05 was considered statistically significant.
Results
General demographic, socioeconomic, and epidemiological information.
A total of 230 volunteers were enrolled in the study. Numbers of female and male participants were 143 (62.2%) and 87 (37.8%), respectively. Distribution of the individuals according to the age groups was nine (3.9%) for age 7–19, 76 (33%) for age 20–39, 90 (39.1%) for age 40–59, and 55 (24%) for age 60 and above. A minority of the participants (24%) were university graduates; however, most of the individuals (91.7%) had middle or high socioeconomic status. According to their occupational status, the study population was categorized as students/pupils (8.3%), officials (27.8%), housewives/retirees (40.9%), workers (7%), and self-used (16%). Rates of the urban and rural residents were 64.8% and 35.2%, respectively. Thirty-seven percent of the individuals owned domestic animals such as dog, cat, chicken, and bird. Additionally, most of the participants used treated drinking water (bottled water: 80.4%, tap water: 19.6%). The detailed demographic, socioeconomic, and epidemiological information of the volunteers were shown in Table 1.
Table 1.
Distribution of Blastocystis spp. prevalence according to demographic, socioeconomic, and epidemiological factors, North Cyprus, 2015
| Factors | Factors (n/%) | Blastocystis spp. positivity (n/%) | OR (95% CI) | P value |
|---|---|---|---|---|
| Gender | ||||
| Male | 87/37.8 | 24/27.6 | 1.0 (–) | – |
| Female | 143/62.2 | 40/27.9 | 0.981 (0.541–1.779) | 0.950 |
| Age groups | ||||
| 7–19 | 9/3.9 | 1/11.1 | 1.0 (–) | – |
| 20–39 | 76/33 | 27/35.5 | 0.227 (0.027–1.911) | 0.141 |
| 40–59 | 90/39.1 | 23/25.5 | 0.364 (0.043–3.071) | 0.335 |
| > 60 | 55/24 | 13/23.6 | 0.404 (0.046–3.537) | 0.399 |
| Educational level | ||||
| Lower than university | 175/76 | 53/30.3 | 1.0 (–) | – |
| University graduates | 55/24 | 11/20 | 1.738 (0.833–3.625) | 0.138 |
| Marital status | ||||
| Married | 183/80 | 56/30.6 | 1.0 (–) | – |
| Single | 47/20 | 8/17 | 2.15 (0.944–4.896) | 0.064 |
| Occupation | ||||
| Students | 19/8.3 | 4/21 | 1.0 (–) | – |
| Officials | 64/27.8 | 19/29.6 | 0.632 (0.185–2.153) | 0.460 |
| Housewives or retirees | 94/40.9 | 27/28.7 | 0.662 (0.201–2.175) | 0.494 |
| Workers | 16/7 | 4/25 | 0.800 (0.165–3.885) | 1.000 |
| Self-used | 37/16 | 10/27 | 0.720 (0.192–2.696) | 0.625 |
| Socioeconomic status | ||||
| Low | 19/8.3 | 6/31.6 | 1.0 (–) | – |
| Middle and high | 211/91.7 | 58/27.4 | 1.218 (0.442–3.354) | 0.703 |
| Traveling abroad | ||||
| Yes | 83/36 | 24/29 | 1.0 (–) | – |
| No | 147/64 | 40/27.2 | 1.088 (0.599–1.978) | 0.782 |
| Residence | ||||
| Urban | 149/64.8 | 41/27.5 | 1.0 (–) | – |
| Rural | 81/35.2 | 23/28.4 | 0.957 (0.524–1.748) | 0.887 |
| Domestic animal owners | ||||
| Yes | 85/37 | 29/34.1 | 1.0 (–) | – |
| No | 145/63 | 35/24.1 | 1.628 (0.904–2.930) | 0.103 |
| Source of water | ||||
| Tap water | 45/19.6 | 10/22.2 | (–) | – |
| Bottled water | 185/80.4 | 54/29.1 | 0.707 (0.404–1.239) | 0.225 |
CI = confidence interval; OR = odds ratio.
Prevalence of the intestinal parasitic infection.
In the macroscopic examination, 43 stool samples were noted to have watery appearance, whereas the remaining had normal consistency and color. Also, no pus, blood, and helminth were observed in the morphological evaluation of the specimens.
Blastocystis spp. was detected microscopically in the native-Lugol (n = 24; 10.5%) and trichrome-stained slides (n = 24; 10.5%). No other parasites were detected in the specimens except Giardia spp. (n = 2; 0.8%) and Entamoeba coli (n = 1; 0.4%). According to the PCR results, 49 (21.3%) and 58 (25.3%) specimens were found positive for Blastocystis spp. by FS and DSSFP methods, respectively. Total number of the PCR-positive specimens were noted to be 64 (27.8%) by the two methods.
Evaluation of Blastocystis spp. infection according to the risk factors and clinical symptoms.
Presence of Blastocystis spp. was not significantly related to gender, age, marital status, educational level, economic status, and occupation (Table 1). Association of Blastocystis spp. prevalence with the epidemiological factors such as travel history, residence, presence of domestic animals, and source of water was also not statistically significant (Table 1).
There was no statistical significance between Blastocystis spp. positivity and any of the gastrointestinal symptoms such as bloating, abdominal pain, abdominal cramps, constipation, diarrhea, and nausea (Table 2).
Table 2.
Distribution of Blastocystis spp. prevalence according to the gastrointestinal symptoms, North Cyprus, 2015
| Factors | Factors (n/%) | Blastocystis spp. positivity (n/%) | OR (95% CI) | P value |
|---|---|---|---|---|
| Abdominal pain | ||||
| Yes | 114/49.6 | 31/27.2 | 1.0 (–) | – |
| No | 116/50.4 | 33/28.4 | 0.939 (0.528–1.673) | 0.832 |
| Diarrhea | ||||
| Yes | 43/18.7 | 13/30.2 | 1.0 (–) | – |
| No | 187/81.3 | 51/27.2 | 1.156 (0.559–2.388) | 0.696 |
| Abdominal cramps | ||||
| Yes | 98/42.6 | 29/29.5 | 1.0 (–) | – |
| No | 132/57.4 | 35/26.5 | 1.165 (0.652–2.082) | 0.607 |
| Nausea | ||||
| Yes | 40/17.4 | 11/27.5 | 1.0 (–) | – |
| No | 190/82.6 | 53/27.8 | 0.980 (0.457–2.103) | 0.960 |
| Bloating | ||||
| Yes | 125/54.4 | 33/26.4 | 1.0 (–) | – |
| No | 105/45.4 | 31/29.5 | 0.856 (0.480–1.526) | 0.598 |
| Constipation | ||||
| Yes | 59/25.7 | 12/20.3 | 1.0 (–) | – |
| No | 171/74.3 | 52/30.4 | 0.584 (0.286–1.192) | 0.137 |
CI = confidence interval; OR = odds ratio.
Blastocystis suptyping and their association with risk factors.
To determine Blastocystis STs, PCR products of 64 positive stool samples were sequenced in one direction. The most common Blastocystis STs were found to be ST3, ST2, ST1, and ST4; whereas other STs were identified as ST6, ST7, and non-ST. The STs were not significantly related to any of the demographic, socioeconomic, and epidemiological factors (Table 3). Furthermore, no significant association was found between Blastocystis STs and the gastrointestinal symptoms (Table 4).
Table 3.
Distribution of Blastocystis subtypes according to demographic, socioeconomic, and epidemiological factors, North Cyprus, 2015
| Factors | Positive (n) | Non-ST (n) | ST1 (n) | ST2 (n) | ST3 (n) | ST4 (n) | ST6 (n) | ST7 (n) |
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Male | 24 | 4 | 1 | 5 | 10 | 2 | 2 | – |
| Female | 40 | 2 | 7 | 13 | 10 | 5 | 1 | 2 |
| P value | 0.317 | 0.655 | 0.180 | nc | 0.317 | 0.317 | nc | |
| Age groups (years) | ||||||||
| 0–19 | 1 | – | – | 1 | – | – | – | – |
| 20–39 | 27 | 2 | 6 | 9 | 7 | 3 | – | – |
| 40–59 | 23 | 2 | 1 | 6 | 10 | – | 2 | 2 |
| ≥ 60 | 13 | 2 | 1 | 2 | 3 | 4 | 1 | – |
| P value | 0.102 | 0.370 | 0.109 | 0.109 | nc | nc | nc | |
| Educational level | ||||||||
| Lower than university | 53 | 4 | 5 | 16 | 16 | 7 | 3 | 2 |
| University graduates | 11 | 2 | 3 | 2 | 4 | – | – | – |
| P value | 0.181 | 0.80 | 0.180 | 0.108 | nc | nc | nc | |
| Marital status | ||||||||
| Married | 56 | 6 | 6 | 15 | 19 | 6 | 3 | 1 |
| Single | 8 | – | 2 | 3 | 1 | 1 | – | 1 |
| P value | nc | 0.180 | 0.180 | 0.655 | 0.655 | nc | nc | |
| Occupation | ||||||||
| Students | 4 | – | 2 | 1 | – | 1 | – | – |
| Officials | 19 | 3 | 2 | 6 | 5 | 1 | 1 | 1 |
| Housewives or retirees | 27 | 2 | 2 | 7 | 9 | 5 | 2 | – |
| Workers | 4 | – | – | 1 | 3 | – | – | – |
| Self-used | 10 | 1 | 2 | 3 | 3 | – | – | 1 |
| P value | 0.593 | nc | 0.223 | 0.066 | 1.000 | 0.655 | nc | |
| Socioeconomic status | ||||||||
| Low income | 6 | – | 2 | 3 | – | – | 1 | – |
| Middle or high income | 58 | 6 | 6 | 15 | 20 | 7 | 2 | 2 |
| P value | nc | 0.180 | 0.180 | nc | nc | 0.655 | nc | |
| Traveling abroad | ||||||||
| Yes | 24 | – | 1 | 8 | 10 | 3 | 1 | 1 |
| No | 40 | 6 | 7 | 10 | 10 | 4 | 2 | 1 |
| P value | nc | 0.655 | 0.180 | nc | 0.655 | 0.180 | nc | |
| Residence | ||||||||
| Urban | 41 | 3 | 6 | 9 | 12 | 7 | 2 | 2 |
| Rural | 23 | 3 | 2 | 9 | 8 | – | 1 | – |
| P value | nc | 0.180 | nc | 0.180 | nc | 0.655 | nc | |
| Domestic animal owners | ||||||||
| Yes | 29 | 4 | 4 | 6 | 12 | 1 | 1 | 1 |
| No | 35 | 2 | 4 | 12 | 8 | 6 | 2 | 1 |
| P value | 0.120 | nc | 0.180 | 0.180 | 0.655 | 0.655 | nc | |
| Source of water | ||||||||
| Tap water | – | 2 | 3 | 4 | – | – | 1 | |
| Bottled water | 10 | 6 | 6 | 15 | 16 | 7 | 3 | 1 |
| P value | 54 | nc | 0.180 | 0.180 | 0.180 | nc | nc | nc |
nc = noncountable.
Table 4.
Distribution of Blastocystis subtypes according to the gastrointestinal symptoms, North Cyprus, 2015
| Symptoms | Positive (n) | Non-ST (n) | ST1 (n) | ST2 (n) | ST3 (n) | ST4 (n) | ST6 (n) | ST7 (n) |
|---|---|---|---|---|---|---|---|---|
| Abdominal pain | ||||||||
| Yes | 31 | 4 | 1 | 12 | 8 | 3 | 3 | – |
| No | 33 | 2 | 7 | 6 | 12 | 4 | – | 2 |
| P value | 0.317 | 1.000 | 0.180 | 0.180 | 0.317 | nc | nc | |
| Diarrhea | ||||||||
| Yes | 13 | 2 | – | 6 | 3 | 1 | 1 | – |
| No | 51 | 4 | 8 | 12 | 17 | 6 | 2 | 2 |
| P value | 0.655 | nc | 0.180 | 0.655 | 1.000 | 0.180 | nc | |
| Abdominal cramps | ||||||||
| Yes | 29 | 2 | 2 | 10 | 9 | 3 | 2 | 1 |
| No | 35 | 4 | 6 | 8 | 11 | 4 | 1 | 1 |
| P value | 0.655 | 0.655 | 0.180 | 0.180 | 1.000 | 0.180 | ||
| Nausea | ||||||||
| Yes | 11 | – | 1 | 3 | 3 | 3 | 1 | – |
| No | 53 | 6 | 7 | 15 | 17 | 4 | 2 | 2 |
| P value | nc | 0.655 | 0.317 | 0.317 | 0.317 | 0.180 | nc | |
| Bloating | ||||||||
| Yes | 33 | 3 | 4 | 9 | 11 | 3 | 2 | 1 |
| No | 31 | 3 | 4 | 9 | 9 | 4 | 1 | 1 |
| P value | 0.157 | 0.157 | 0.157 | 0.180 | 1.000 | 0.180 | 0.157 | |
| Constipation | ||||||||
| Yes | 12 | 0 | 3 | 2 | 5 | 2 | 0 | 0 |
| No | 52 | 6 | 5 | 16 | 15 | 5 | 3 | 2 |
| P value | 1.000 | 0.317 | 0.655 | 0.180 | 0.655 | 0.317 | 0.180 | |
nc = noncountable.
Discussion
Blastocystosis is commonly encountered especially in developing countries. The prevalence of Blastocystis spp. in developed countries such as Japan (0.5%)17 and Denmark (5.6%)18 is relatively low, with the exception of France (13.7–23.1%).20 On the contrary, generally higher rates are documented from developing countries including Libya (22.1%),15 Iran (26.9%),26 Turkey (15.2%),27 Brazil (17.8%),28 Egypt (33.3%),29 Philippines (12.9%),30 and Thailand (21%).31 The highest percentages of Blastocystis spp. positivity were detected in Senegal (100%),16 Qatar (71.1%),19 and Lebanon (63%).2
In our study, the prevalence of Blastocystis spp. infection was noted to be 24 (10.5%), 24 (10.5%), and 64 (27.8%), by direct microscopy, trichrome method, and PCR, respectively. Generally, stained and direct smear methods have lower sensitivity,32,33 while PCR was found to be the most effective diagnostic approach.25,34 Owing to the difficulty in collecting three consecutive stool samples, we obtained one specimen from each participant. This might have affected the diagnostic performance of microscopy resulting in lower positivity rates in our study. Furthermore, the reason of inconsistent results among different studies can be explained by the different diagnostic methods used: Abdulsalam and others,15 Belleza and others,30 and Yaicharoen and others31 used microscopy and culture, while our method was based on PCR.
In North Cyprus, generally, the population has middle or high socioeconomic status; service sector is dominated, and especially tourism is considered as a major source of income. In the community, adequate public services and infrastructures including health care are available. Public water system is often controlled and treated. Generally, the individuals consume treated and bottled water that is considered to be healthy and safe. The population has easy access to water supplies, which provides maintenance of hygienic conditions. Additionally, garbage and sewage are known to be exposed to proper treatment before discharged. These can explain the reason of relatively lower rates of Blastocystis spp. in North Cyprus compared with developing countries.
The prevalence of the intestinal parasitic infections could depend on demographic, socioeconomic, and epidemiological factors.35,36 In our study, Blastocystis spp. positivity was not significantly related to the age and gender of the participants. Several studies indicated that the prevalence of this protistan infection was significantly higher in males in comparison to females.15,28,37 On the contrary, no difference in the infection rates was documented between the genders by other studies.19,30,38 Previous publications reported high prevalence rates among individuals aged 5–59,30 in adults aged ≥ 18 years,15 and those aged 18–30 years31. Li and others demonstrated that individuals aged 60 years and above had the highest rate of Blastocystis spp. infection.9 However, other studies found no significant relation between the infection prevalence and age.38,39 These contradictory results can be explained by the local determinants such as the environmental conditions that affect the fecal-oral route of transmission among individuals of different ages and genders.15 On the other hand, number of the participants aged 7–19 years was low (3.9%), which might also have affected the results of statistical analyses in the current study.
Interestingly, our data revealed that the prevalence of Blastocystis spp. was higher in single individuals compared with married ones; however, there was no statistical significance between the infection rates and the marital status. Dagci and others also found no significant association between the marital status and the parasite prevalence.27
In the present study, the prevalence of Blastocystis spp. between the used and unemployed individuals was not statistically significant. In a previous report, due to the significantly higher rates in the used individuals than those of the unemployed subjects, Abdulsalam and others demonstrated that occupational status of the individuals was a risk factor for blastocystosis. The authors indicated that this result could be explained by the higher possibility of acquiring the infection at the work places through the food and environment.15 Also, Quihui and others found that children with unemployed and less educated mothers had a higher risk of parasitic infection.40
Studies showed that the low level of education was a significant risk factor for acquiring Blastocystis and other parasitic infections.15,26,35 Hygiene and sanitation are important factors for prevention and control of the communicable diseases. However, in our study, the relation between Blastocystis prevalence and educational levels was not statistically significant.
Previous studies indicated that poverty or low economic status significantly increased the prevalence of parasitic infections by enabling the active transmission within the community.26,35,40 In our study, most of the participants (91.7%) had middle or high socioeconomic status; however, the rate of blastocystosis was interestingly high (27.4%) in this group. In the low socioeconomic status group, infection rate was also found high (31.6%). Furthermore, no statistical significance was found between Blastocystis prevalence and the educational levels, which was contradictory to the previous studies.
Ingestion of contaminated water, particularly surface water (untreated), was indicated as a potential risk for the infection with Blastocystis.22,40,41 However, Abdulsalam and others and Osman and others detected no significant difference in the rates of blastocystosis between drinking treated and untreated water, and suggested that the level of contamination of groundwater by Blastocystis was likely to be low.2,15 In the present study, majority of the participants used bottled water (80.4%), and the remaining consumed tap water (19.6%), but no statistical difference was found in the infection rates between the two groups.
Blastocystosis is also regarded as a zoonosis. A high prevalence of this protist was detected in the feces of dogs (70%) and cats (67.3%).21 The individuals who are exposed to animals were shown to have significantly higher rates of blastocystosis.11,42 However, similar to our findings, a study found no statistical significance between the prevalence of blastocystosis and contact with animals.15 Previous studies indicated that factors associated with living in the rural regions significantly influence the prevalence of Blastocystis and other parasitic infections. Generally, this can be explained by the poor sanitary and hygiene conditions, effects of contaminated water supplies, exposure to soil, and absence of toilet facilities.1,43 On the contrary, Kiani and others found no statistical difference in blastocystosis rates between rural and urban residents,26 which support our results. In our study population, 36% of the individuals frequently traveled to Turkey and European countries. Our results showed that traveling history of the participants did not significantly influence the prevalence of blastocystosis. Unlike our findings, Jelinek and others suggested that Blastocystis hominis was related with the development of diarrhea in travelers returning from tropical countries.44
It is generally accepted that Blastocystis is noninvasive however, vacuolar form of the protist was shown to invade the lamina propria, submucosal and muscular layers of the intestine, leading to inflammation and active colitis in experimentally infected mice.45 Furthermore, the proteases of Blastocystis were suggested as a virulence factor that contributes to escape from the host immune response.46 Blastocystis spp. can be detected in both symptomatic and asymptomatic patients.6 Several studies suggested that the protist could be a potential pathogen in both immunocompetent and immunocompromised patients.47,48 A recent study indicated that Blastocystis was a common member of the intestinal flora in healthy people, and various STs of the protist could also colonize the gastrointestinal tract resulting in asymptomatic carriage.49 The most common symptoms of our study population were recorded as bloating, abdominal pain, abdominal cramps, constipation, diarrhea, and nausea. No significant association was found between the Blastocystis prevalence and development of the gastrointestinal symptoms. Our finding was inconsistent with those of previous studies in which significant relation was detected between blastocystosis and gastrointestinal symptoms in symptomatic individuals.1,2,15,37
In the present study, the most common Blastocystis STs were ST3, ST2, ST1, and ST4. Among these, only four STs (ST1, ST2, ST3, and ST4) are common throughout the world and their distribution also depends on geographic regions.6–8 In Turkey, the most predominant Blastocystis ST was documented as ST3, which was followed by ST1 and ST2.12,50,51 In the European countries, distribution of the STs tended to be similar to Turkey, and in addition, ST4 was commonly observed.8 On the contrary, ST5–ST9 were detected sporadically in humans.8,9 Several studies suggested that the gastrointestinal symptoms associated with Blastocystis spp. might be dependent on certain STs12,13; however, recent epidemiological studies14 remain contradictory. In the present study, Blastocystis STs also did not show significant correlation with the gastrointestinal symptoms. Similarly, the prevalence of Blastocystis STs was not found significantly associated with the demographic, socioeconomic, and epidemiological factors. Although there are limited data, Mattiucci and others demonstrated that ST3 and ST1 were significantly more prevalent in patients aged 15–50 years.52
Conclusion
This study is the first investigation of the prevalence and epidemiology of Blastocystis spp. in North Cyprus. Our results revealed high prevalence of Blastocystis spp. in the community; however, presence of the protist and its STs was not significantly related with the gastrointestinal symptoms among the symptomatic and asymptomatic individuals in North Cyprus. Interestingly, the distribution of Blastocystis spp. and its STs among demographic, socioeconomic, and epidemiological factors showed complete homogeneity. Taken together, these findings support the theory that Blastocystis spp. may be member of the intestinal flora in humans; nevertheless, further investigations are needed for elucidating the mechanisms of pathogenicity.
Supplementary Material
ACKNOWLEDGMENTS
We would like to thank BM Laboratory Company for the technical support.
Footnotes
Financial support: This study was funded by Hitit University Scientific Research Projects (grant no: TIP19002.15.003).
Authors' addresses: Ayse Seyer, Faculty of Health Sciences and School of Nursing, Girne Amerikan University, Kyrenia, North Cyprus, Cyprus, E-mail: ayseseyer@gau.edu.tr. Djursun Karasartova, Ayse Semra Güreser, and Ebru Turgal, Faculty of Medicine, Hitit University, Corum, Turkey, E-mails: jursuna11@gmail.com, semrakalay@yahoo.com, and eturgal@yahoo.com. Emrah Ruh and Turgut Imir, Faculty of Medicine, Near East University, Nicosia, North Cyprus, Cyprus, E-mails: emrahruh@gmail.com and turgut_imir@yahoo.com. Aysegul Taylan-Ozkan, Department of Medical Microbiology, Faculty of Medicine, Hitit University, Corum, Turkey, and Department of Medical Microbiology and Clinical Microbiology, Faculty of Medicine, Near East University, Nicosia, North Cyprus, Cyprus, E-mail: aysegultaylanozkan@hitit.edu.tr.
References
- 1.Nithyamathi K, Chandramathi S, Kumar S. Predominance of Blastocystis sp. 𝚤nfection among school children in Peninsular Malaysia. PLoS One. 2016;25:e0136709. doi: 10.1371/journal.pone.0136709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Osman M, El Safadi D, Cian A, Benamrouz S, Nourrisson C, Poirier P, Pereira B, Razakandrainibe R, Pinon A, Lambert C, Wawrzyniak I, Dabboussi F, Delbac F, Favennec L, Hamze M, Viscogliosi E, Certad G. Prevalence and risk factors for intestinal protozoan infections with Cryptosporidium, Giardia, Blastocystis and Dientamoeba among schoolchildren in Tripoli, Lebanon. PLoS Negl Trop Dis. 2016;10:e0004496. doi: 10.1371/journal.pntd.0004496. Erratum in: PLoS Negl Trop Dis 10: e0004643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wawrzyniak I, Poirier P, Viscogliosi E, Dionigia M, Texier C, Delbac F, Alaoui HE. Blastocystis, an unrecognized parasite: an overview of pathogenesis and diagnosis. Ther Adv Infect Dis. 2013;1:167–178. doi: 10.1177/2049936113504754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scanlan PD, Stensvold CR. Blastocystis: getting to grips with our guileful guest. Trends Parasitol. 2013;29:523–529. doi: 10.1016/j.pt.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 5.Tan KS, Mirza H, Teo JD, Wu B, Macary PA. Current views on the clinical relevance of Blastocystis spp. Curr Infect Dis Rep. 2010;12:28–35. doi: 10.1007/s11908-009-0073-8. [DOI] [PubMed] [Google Scholar]
- 6.Tan KS. New insights on classification, identification, and clinical relevance of Blastocystis spp. Clin Microbiol Rev. 2008;21:639–665. doi: 10.1128/CMR.00022-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stensvold CR, Suresh GK, Tan KS, Thompson RC, Traub RJ, Viscogliosi E, Yoshikawa H, Clark CG. Terminology for Blastocystis subtypes-a consensus. Trends Parasitol. 2007;23:93–96. doi: 10.1016/j.pt.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Alfellani MA, Stensvold CR, Vidal-Lapiedra A, Onuoha ES, Fagbenro-Beyioku AF, Clark CG. Variable geographic distribution of Blastocystis subtypes and its potential implications. Acta Trop. 2013;126:11–18. doi: 10.1016/j.actatropica.2012.12.011. [DOI] [PubMed] [Google Scholar]
- 9.Li LH, Zhang XP, Lv S, Zhang L, Yoshikawa H, Wu Z, Steinmann P, Utzinger J, Tong XM, Chen SH, Zhou XN. Cross-sectional surveys and subtype classification of human Blastocystis isolates from four epidemiological settings in China. Parasitol Res. 2007;102:83–90. doi: 10.1007/s00436-007-0727-0. [DOI] [PubMed] [Google Scholar]
- 10.Stensvold CR, Alfellani MA, Norskov-Lauritsen S, Prip K, Victory EL, Maddox C, Nielsen HV, Clark CG. Subtype distribution of Blastocystis isolates from synanthropic and zoo animals and identification of a new subtype. Int J Parasitol. 2009;39:473–479. doi: 10.1016/j.ijpara.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 11.Parkar U, Traub RJ, Vitali S, Elliot A, Levecke B, Robertson I, Geurden T, Steele J, Drake B, Thompson RC. Molecular characterization of Blastocystis isolates from zoo animals and their animal-keepers. Vet Parasitol. 2010;19:8–17. doi: 10.1016/j.vetpar.2009.12.032. [DOI] [PubMed] [Google Scholar]
- 12.Dogruman-Al F, Dagci H, Yoshikawa H, Kurt O, Demirel M. A possible link between subtype 2 and asymptomatic infections of Blastocystis hominis. Parasitol Res. 2008;103:685–689. doi: 10.1007/s00436-008-1031-3. [DOI] [PubMed] [Google Scholar]
- 13.Eroglu F, Genc A, Elgun G, Koltas IS. Identification of Blastocystis hominis isolates from asyptomatic and symptomatic patients by PCR. Parasitol Res. 2009;105:1589–1592. doi: 10.1007/s00436-009-1595-6. [DOI] [PubMed] [Google Scholar]
- 14.Clark CG, van der Giezen M, Alfellani MA, Stensvold CR. Recent developments in Blastocystis research. Adv Parasitol. 2013;82:1–32. doi: 10.1016/B978-0-12-407706-5.00001-0. [DOI] [PubMed] [Google Scholar]
- 15.Abdulsalam AM, Ithoi I, Al-Mekhlafi HM, Khan AH, Ahmed A, Surin J, Mak JW. Prevalence, predictors and clinical significance of Blastocystis sp. in Sebha, Libya. Parasit Vectors. 2013;8:86. doi: 10.1186/1756-3305-6-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.El Safadi D, Gaayeb L, Meloni D, Cian A, Poirier P, Wawrzyniak I, Delbac F, Dabboussi F, Delhaes L, Seck M, Hamze M, Riveau G, Viscogliosi E. Children of Senegal River Basin show the highest prevalence of Blastocystis sp. ever observed worldwide. BMC Infect Dis. 2014;25:164. doi: 10.1186/1471-2334-14-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horiki N, Maruyama M, Fujita Y, Yonekura T, Minato S, Kaneda Y. Epidemiologic survey of Blastocystis hominis infection in Japan. Am J Trop Med Hyg. 1997;56:370–374. doi: 10.4269/ajtmh.1997.56.370. [DOI] [PubMed] [Google Scholar]
- 18.Stensvold CR, Christiansen DB, Olsen KE, Nielsen HV. Blastocystis sp. subtype 4 is common in Danish Blastocystis-positive patients presenting with acute diarrhea. Am J Trop Med Hyg. 2011;84:883–885. doi: 10.4269/ajtmh.2011.11-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abu-Madi M, Aly M, Behnke JM, Clark CG, Balkhy H. The distribution of Blastocystis subtypes in isolates from Qatar. Parasit Vectors. 2015;17:465. doi: 10.1186/s13071-015-1071-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El Safadi D, Cian A, Nourrisson C, Pereira B, Morelle C, Bastien P, Bellanger AP, Botterel F, Candolfi E, Desoubeaux G, Lachaud L, Morio F, Pomares C, Rabodonirina M, Wawrzyniak I, Delbac F, Gantois N, Certad G, Delhaes L, Poirier P, Viscogliosi E. Prevalence, risk factors for infection and subtype distribution of the intestinal parasite Blastocystis sp. from a large-scale multi-center study in France. BMC Infect Dis. 2016;26:451. doi: 10.1186/s12879-016-1776-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duda A, Stenzel DJ, Boreham PF. Detection of Blastocystis sp. in domestic dogs and cats. Vet Parasitol. 1998;31:9–17. doi: 10.1016/s0304-4017(97)00224-0. [DOI] [PubMed] [Google Scholar]
- 22.Taamasri P, Mungthin M, Rangsin R, Tongupprakarn B, Areekul W, Leelayoova S. Transmission of intestinal blastocystosis related to the quality of drinking water. Southeast Asian J Trop Med Public Health. 2000;31:112–117. [PubMed] [Google Scholar]
- 23.Wheatley WB. A rapid staining procedure for intestinal amoebae and flagellates. Am J Clin Pathol. 1951;21:990–991. doi: 10.1093/ajcp/21.10_ts.990. [DOI] [PubMed] [Google Scholar]
- 24.Seyer A, Karasartova D, Ruh E, Gureser AS, Imir T, Taylan-Ozkan A. Is “dried stool spots on filter paper method (DSSFP)” more sensitive and effective for detecting Blastocystis spp. and their subtypes by PCR and sequencing? Parasitol Res. 2016;115:4449–4455. doi: 10.1007/s00436-016-5231-y. [DOI] [PubMed] [Google Scholar]
- 25.Scicluna SM, Tawari B, Clark CG. DNA barcoding of Blastocystis. Protist. 2006;157:77–85. doi: 10.1016/j.protis.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 26.Kiani H, Haghighi A, Rostami A, Azargashb E, Tabaei SJ, Solgi A, Zebardast N. Prevalence, risk factors and symptoms associated to intestinal parasite infections among patients with gastrointestinal disorders in Nahavand, Western Iran. Rev Inst Med Trop Sao Paulo. 2016;58:42. doi: 10.1590/S1678-9946201658042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dagci HO, Demirel M, Mandiracioglu A, Aydemir S, Saz U, Bart A, Van Gool T. Epidemiological and diagnostic features of Blastocystis infection in symptomatic patients in Izmir province, Turkey. Iran J Parasitol. 2014;9:519–529. [PMC free article] [PubMed] [Google Scholar]
- 28.Cabrine-Santos M, Cintra Edo N, do Carmo RA, Nascentes GA, Pedrosa AL, Correia D, Oliveira-Silva MB. Occurrence of Blastocystis spp. in Uberaba, Minas Gerais, Brazil. Rev Inst Med Trop Sao Paulo. 2015;57:211–214. doi: 10.1590/S0036-46652015000300005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rayan HZ, Ismail OA, El Gayar EK. Prevalence and clinical features of Dientamoeba fragilis infections in patients suspected to have intestinal parasitic infection. J Egypt Soc Parasitol. 2007;37:599–608. [PubMed] [Google Scholar]
- 30.Belleza ML, Cadacio JL, Borja MP, Solon JA, Padilla MA, Tongol-Rivera PN, Rivera WL. Epidemiologic study of Blastocystis infection in an urban community in the Philippines. J Environ Public Health. 2015;2015:894297. doi: 10.1155/2015/894297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yaicharoen R, Sripochang S, Sermsart B, Pidetcha P. Prevalence of Blastocystis hominis infection in asymptomatic individuals from Bangkok, Thailand. Southeast Asian J Trop Med Public Health. 2005;36((Suppl 4)):17–20. [PubMed] [Google Scholar]
- 32.Dogruman-Al F, Simsek Z, Boorom K, Ekici E, Sahin M, Tuncer C, Kustimur S, Altinbas A. Comparison of methods for detection of Blastocystis infection in routinely submitted stool samples, and also in IBS/IBD Patients in Ankara, Turkey. PLoS One. 2010;18:e15484. doi: 10.1371/journal.pone.0015484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Elghareeb AS, Younis MS, El Fakahany AF, Nagaty IM, Nagib MM. Laboratory diagnosis of Blastocystis spp. in diarrheic patients. Trop Parasitol. 2015;5:36–41. doi: 10.4103/2229-5070.149919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roberts T, Barratt J, Harkness J, Ellis J, Stark D. Comparison of microscopy, culture, and conventional polymerase chain reaction for detection of Blastocystis sp. in clinical stool samples. Am J Trop Med Hyg. 2011;84:308–312. doi: 10.4269/ajtmh.2011.10-0447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ostan I, Kilimcioglu AA, Girginkardesler N, Ozyurt BC, Limoncu ME, Ok UZ. Health inequities: lower socio-economic conditions and higher incidences of intestinal parasites. BMC Public Health. 2007;27:342. doi: 10.1186/1471-2458-7-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Okyay P, Ertug S, Gultekin B, Onen O, Beser E. Intestinal parasites prevalence and related factors in school children, a western city sample-Turkey. BMC Public Health. 2004;22:64. doi: 10.1186/1471-2458-4-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Al-Fellani MA, Khan AH, Al-Gazoui RM, Zaid MK, Al-Ferjani MA. Prevalence and clinical features of Blastocystis hominis infection among patients in Sebha, Libya. Sultan Qaboos Univ Med J. 2007;7:35–40. [PMC free article] [PubMed] [Google Scholar]
- 38.Khoshnood S, Rafiei A, Saki J, Alizadeh K. Prevalence and genotype characterization of Blastocystis hominis among the Baghmalek People in Southwestern Iran in 2013–2014. Jundishapur J Microbiol. 2015;18:e23930. doi: 10.5812/jjm.23930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.AbuOdeh R, Ezzedine S, Samie A, Stensvold CR, ElBakri A. Prevalence and subtype distribution of Blastocystis in healthy individuals in Sharjah, United Arab Emirates. Infect Genet Evol. 2016;37:158–162. doi: 10.1016/j.meegid.2015.11.021. [DOI] [PubMed] [Google Scholar]
- 40.Quihui L, Valencia ME, Crompton DW, Phillips S, Hagan P, Morales G, Díaz-Camacho SP. Role of the employment status and education of mothers in the prevalence of intestinal parasitic infections in Mexican rural schoolchildren. BMC Public Health. 2006;6:225. doi: 10.1186/1471-2458-6-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Abdulsalam AM, Ithoi I, Al-Mekhlafi HM, Ahmed A, Surin J, Mak JW. Drinking water is a significant predictor of Blastocystis infection among rural Malaysian primary schoolchildren. Parasitology. 2012;139:1014–1020. doi: 10.1017/S0031182012000340. [DOI] [PubMed] [Google Scholar]
- 42.Rajah Salim H, Suresh Kumar G, Vellayan S, Mak JW, Khairul Anuar A, Init I, Vennila GD, Saminathan R, Ramakrishnan K. Blastocystis in animal handlers. Parasitol Res. 1999;85:1032–1033. doi: 10.1007/s004360050677. [DOI] [PubMed] [Google Scholar]
- 43.Sungkar S, Pohan AP, Ramadani A, Albar N, Azizah F, Nugraha AR, Wiria AE. Heavy burden of intestinal parasite infections in Kalena Rongo village, a rural area in South West Sumba, eastern part of Indonesia: a cross sectional study. BMC Public Health. 2015;24:1296. doi: 10.1186/s12889-015-2619-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jelinek T, Peyerl G, Loscher T, von Sonnenburg F, Nothdurft HD. The role of Blastocystis hominis as a possible intestinal pathogen in travellers. J Infect. 1997;35:63–66. doi: 10.1016/s0163-4453(97)91025-2. [DOI] [PubMed] [Google Scholar]
- 45.Elwakil HS, Hewedi IH. Pathogenic potential of Blastocystis hominis in laboratory mice. Parasitol Res. 2010;107:685–689. doi: 10.1007/s00436-010-1922-y. [DOI] [PubMed] [Google Scholar]
- 46.Hameed DM, Hassanin OM, Zuel-Fakkar NM. Association of Blastocystis hominis genetic subtypes with urticaria. Parasitol Res. 2011;108:553–560. doi: 10.1007/s00436-010-2097-2. [DOI] [PubMed] [Google Scholar]
- 47.Ok UZ, Korkmaz M, Ok GE, Taylan Ozkan A, Unsal A, Ozcel MA. Cryptosporidiosis and blastocystosis in chronic renal failure [in Turkish] Turkiye Parazitol Derg. 1996;1:41–46. [Google Scholar]
- 48.Karasartova D, Gureser AS, Zorlu M, Turegun-Atasoy B, Taylan-Ozkan A, Dolapci M. Blastocystosis in post-traumatic splenectomized patients. Parasitol Int. 2016;65((6 Pt B)):802–805. doi: 10.1016/j.parint.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 49.Scanlan PD, Stensvold CR, Rajilić-Stojanović M, Heilig HG, De Vos WM. The microbial eukaryote Blastocystis is a prevalent and diverse member of the healthy human gut microbiota. FEMS Microbiol Ecol. 2014;90:326–330. doi: 10.1111/1574-6941.12396. [DOI] [PubMed] [Google Scholar]
- 50.Dogruman-Al F, Kustimur S, Yoshikawa H, Tuncer C, Simsek Z, Tanyuksel M, Araz E, Boorom K. Blastocystis subtypes in irritable bowel syndrome and inflammatory bowel disease in Ankara, Turkey. Mem Inst Oswaldo Cruz. 2009;104:724–727. doi: 10.1590/s0074-02762009000500011. [DOI] [PubMed] [Google Scholar]
- 51.Eroglu F, Koltas IS. Evaluation of the transmission mode of B. hominis by using PCR method. Parasitol Res. 2010;107:841–845. doi: 10.1007/s00436-010-1937-4. [DOI] [PubMed] [Google Scholar]
- 52.Mattiucci S, Crisafi B, Gabrielli S, Paoletti M, Cancrini G. Molecular epidemiology and genetic diversity of Blastocystis infection in humans in Italy. Epidemiol Infect. 2016;144:635–646. doi: 10.1017/S0950268815001697. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.