Abstract
Mumps, a highly contagious, viral disease continues to spread in India, despite the availability of an effective vaccine. On November 24, 2014, we came across a suspected case of mumps in a 6-year-old boy in a village of Bhusandapur sector in Odisha. We initiated an outbreak investigation using standard techniques outlined by the Centers for Disease Control and Prevention, Atlanta, GA. This uncovered a silent epidemic of 94 case patients (10% of the population) over a period of 16 weeks between August and December 2014, in a single village, which had gone completely unnoticed by the existing health-care system. Since the index case was one of the last case patients of the outbreak, investigation for immediate control was not a priority. Hence, we have used this exercise to describe the outbreak and identify causes that led to its nondetection. Age range of the case patients was between 2 and 40 years; 85 (90.4%) case patients were ≤ 15 years of age and 54 (57.4%) were females. Average duration of illness was 9 days. No child had received the mumps vaccine. The outbreak had led to a community expenditure of 538 USD. The exercise uncovered a number of weak links in the essential public health services within the health-care delivery system in the area.
Introduction
Mumps, a highly contagious viral disease, continues to spread in India, despite the availability of an effective vaccine.1 Although the disease is usually a self-limiting clinical condition mainly affecting children between 5 and 10 years of age, it can lead to serious complications such as meningitis (15%), pancreatitis (4%), and orchitis (20–30%) in postpubertal males, and encephalitis and abortions in pregnant women. It also results in significant loss of school days/working days; therefore, its prevention becomes imperative. Globally, 120 countries (62%) have included mumps vaccine in their national immunization schedule, but India is still not a member of this group.1,2
Other than vaccination, one of the prerequisites of a successful disease prevention and control program is a robust surveillance system. India has an Integrated Disease Surveillance Program (IDSP), a decentralized project through World Bank assistance operating for nearly a decade.3 However, since reporting of mumps under IDSP is optional, a large number of outbreaks due to mumps might go unnoticed. In the recent past, very few research studies investigating mumps outbreaks have been published from India.1 Thus, mumps-related disease burden data in India continue to be sketchy. If mumps is to be controlled, it is essential to detect the cases that occur, investigate, and report them. It is also imperative that health systems research be carried out at periodic intervals, so that specific weakness in the system can be detected and actions taken. Such improvements in the public health-care system would impact the control activities for other diseases too.
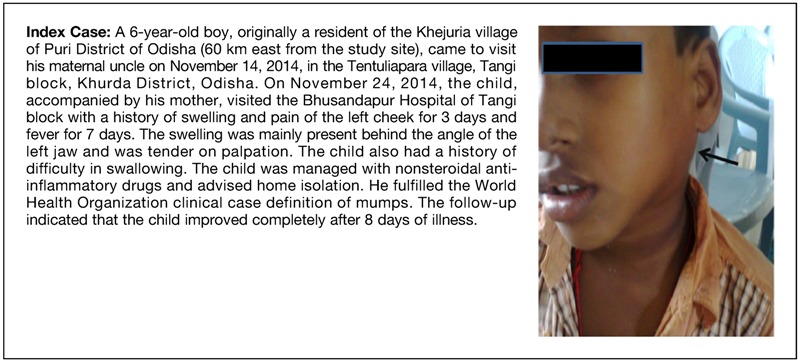
On November 24, 2014, we had a serendipitous encounter with a pediatric mumps case (Box 1) in our geriatric outpatient department at a rural primary health center (PHC). This prompted us to carry out a field inquiry in his village Tentuliapara. The village had 174 families and 946 people residing in overcrowded and poorly ventilated houses. We found clustering of similar case patients within the neighborhood during the preceding weeks, a phenomenon not recognized for nearly a decade, as per the local residents. The boy first brought the attention of the authors toward a waning, silent outbreak. Since he was a nonresident of the village, this set him up for infection late in the outbreak as a remaining, nonimmune person.
Box 1. Index case of mumps with swelling of the left cheek.
In this article, we describe the outbreak and the reasons for its late detection. We have carried out situation analysis by utilizing the essential public health services framework4 and also identified the degree of improvement needed in each of the service components. Thus, we have explored the opportunity to use the health systems research in guiding future disease control activities in the region.
Materials and Methods
Outbreak location.
The outbreak occurred in Tentuliapara village of Odisha state, which is one of the 29 states in India. Odisha has a population of 41.9 million and is divided into 30 districts which are further subdivided into 310 blocks for administrative purposes. Each block is subdivided into sectors and every sector has group of villages within it. Tangi, one of the 10 blocks in Khurda District is divided into six sectors, and each sector has a PHC. The village is in the Bhusandapur sector of Tangi block. The Department of Community and Family Medicine at the All India Institute of Medical Sciences, Bhubaneswar, has adopted PHC Bhusandapur for providing once a week chronic care services to the elderly population and supporting the community-based teaching and learning activity of undergraduate MBBS students. The sector covers 58 villages and a population of 57,000. The Bhusandapur PHC has one medical officer (MO) who sees about 60 patients every day and supervises seven frontline workers (FLWs) that include auxiliary nurse midwives (ANM) and multipurpose health workers. Every village is also served by an accredited social health activist (ASHA) worker who is in turn supervised by an ANM.
Clinical case definition.
For the purpose of the study, according to the World Health Organization (WHO) clinical case definition, a case of mumps was defined as “any person who had acute onset of unilateral or bilateral tender, self-limited swelling of the parotid or other salivary gland, lasting two or more days and without other apparent cause.”5 Case patients were permanently classified as clinical mumps cases due to unavailability of laboratory facilities in the region to isolate the mumps virus or demonstrate antibody levels.
Data collection.
Two doctors (authors) trained in public health contacted the local ANM and ASHA workers to prepare a spot map of the area for carrying out house-to-house epidemiological investigation between November 26 and December 31, 2014. The authors interviewed the FLWs working in this village to assess their knowledge about the epidemiology of mumps and the response of the health system during the mumps outbreak. They also interviewed the household respondents (immediate caregiver of case patients) to collect relevant information about every mumps case, using a pretested epidemiological case sheet. Data gathered included demographic details of the household, the onset of disease, its duration, sequence of appearance of symptoms, past mumps vaccination history, treatment history, travel history, past mumps infection, knowledge of prevention and control, and contact history with any case of mumps infection. To capture information about mumps-related complications, the authors depended upon retrospective disease history during the survey and passive surveillance throughout the investigation period, which was 5 weeks. No further follow-up was possible after the end of the study period. All case patients were line-listed and census data of all the family members were collected. A search for new case patients was done through home visits during the investigation period. We tried to understand the social spread among the case patients by asking the possible source of infection in the community and classifying the known source as either a family member or neighbor.
A spot map depicting the exact geographical distribution of mumps case patients was prepared. After completion of all the interviews, necessary health advice for prevention and control of mumps was provided to all the family members. Two suspected case patients detected during the course of the study were referred to the nearby health center. The investigating team was vigilant for 6 weeks after the last case was detected (longest incubation period of mumps being 3 weeks) to determine whether the outbreak had subsided.
Ethical considerations.
Verbal consent was taken from the participants prior to data collection, after explaining the purpose and nature of investigation. Confidentiality of the subjects was maintained. Approval of the institutional ethics board was not taken as it was an outbreak investigation.
Statistical analysis.
Data were entered and analyzed in Microsoft Excel 2013 (Microsoft Corporation, Redmond, WA). The outbreak has been described according to time, place, and person. Case patients beyond 15 years of age were classified as older individuals, considering the fact that it is primarily the disease of children below 15 years of age.
An epidemic curve was plotted to visualize the outbreak's magnitude and time trend. Categorical data were summarized using proportions; continuous data were summarized using means and standard deviations, median and interquartile range (IQR). Epidemiological links were derived through social links and respondents reported expected sources of infection in the neighborhood.
We also analyzed the health system using a framework for essential public health services/functions laid down by the Centers for Disease Control and Prevention, Atlanta, GA.4 Based on the information obtained during the interview of caregivers of case patients and FLWs, and observations carried out by the investigators during the survey, we developed a concept diagram to explain various factors responsible for the outbreak. We then grouped these factors under each of the 10 essential public health services/functions. Subsequently, we graded the level of improvement needed in each of these 10 functions using a color code, based on the findings of the study and consensus achieved after deliberation among the investigators using a marking scheme. Red (performance < 30%), yellow (performance ≥ 31%, < 50%), and green color (performance ≥ 51%) indicated maximal, moderate, and minimal improvement needed respectively, for each of the 10 functions within the framework.
Results
Our investigation revealed that 94 (9.9%) people in the village satisfied the clinical case definition of mumps during the outbreak period. Minimum and maximum ages of the case patients were 2 and 40 years, respectively. Nine case patients were women in the reproductive age group (25–40 years) and the rest were children below 15 years. Median age was 8 years (IQR: 5–10) Overall, 54 (57.4%) were females. All case patients except the index case were permanent resident of the village Tentuliapara.
The case patients reported with fever and predominantly bilateral parotid involvement (Table 1). Sixteen percent of the subjects had multiple salivary gland involvement for prolonged duration, of which 80% were older individuals. The mean duration of illness was 9.5 ± 1 days. None of the case patients reported any complications based on retrospective disease history at the time of the survey and also throughout the study period. Only 2% of the overall population could recollect past history of mumps in their childhood.
Table 1.
Clinical presentation of cases of mumps in Tentuliapara village, Bhusandapur, Tangi, Odisha, India, August–December 2014
| Symptoms | No. of case patients (%) N = 94 | Mean duration (days) ± standard deviation |
|---|---|---|
| Fever | 94 (100) | 5.02 ± 1.01 |
| Swelling of salivary glands | 94 (100) | 5.27 ± 0.69 |
| Parotid swelling | 93 (98.9) | |
| Unilateral | 24 (25.5) | – |
| Bilateral | 69 (73.4) | |
| Submandibular swelling | 16 (17.0) | – |
| Unilateral | 3 (3.2) | |
| Bilateral | 13 (13.8) | |
| Cough and cold | 88 (93.6) | 4.57 ± 1.2 |
| Difficulty in swallowing | 80 (85.1) | 4.41 ± 2.1 |
| Earache | 36 (38.3) | 1.84 ± 2.4 |
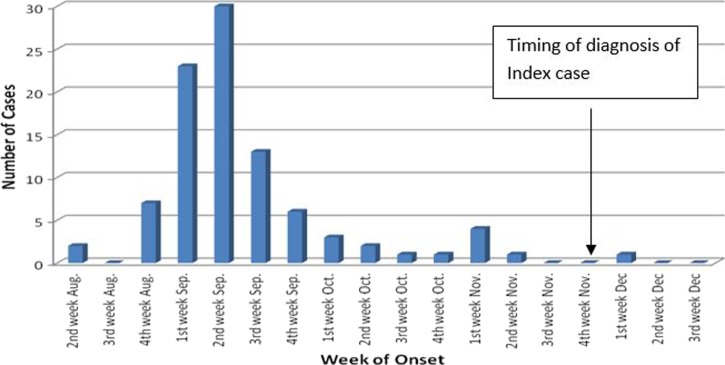
The disease outbreak had started around the second week of August 2014 and continued up to the first week of December 2014. The epidemic was at its peak during the second week of September. The distribution of case patients over time showed that the outbreak was continuous in nature and lasted for 16 weeks. Our index case (Box 1) had suffered during the downslope and the outbreak almost ended by that time (Figure 1 ).
Figure 1.
Outbreak of mumps in Tentuliapara village, Bhusandapur, Tangi, Odisha, India, August–December 2014 (epidemic curve by weekly intervals).
Most case patients had clustered around the two ends of the village. These were the locations having households with large joint families and a large number of susceptible children (Figure 2 ). Proportionately, more females were affected (57.4%) and females also had a higher attack rate (12.3/100 people). All case patients above 15 years of age were the caregivers of the children (mothers). As expected, the 5- to 10-year age group had the greatest number of cases (48% cases). Among children (< 15 years), one of five boys and one of three girls each were found to be sick with mumps indicating an explosive spread of this virus in this age group. (Table 2).
Figure 2.
Cases of mumps by households in Tentuliapara village, Bhusandapur, Tangi, Odisha, India, August–December 2014.
Table 2.
Attack rates by age and sex at Tentuliapara village, Bhusandapur, Tangi, Odisha, India, August–December 2014
| Age groups (years) | Male | Female | Total | Age-wise percentage distribution of mumps cases (%) | Total attack rate (%) | ||||
|---|---|---|---|---|---|---|---|---|---|
| No. of mumps cases | Total population | Attack rate (%) | No. of mumps cases | Total population | Attack rate (%) | No. of mumps cases | |||
| < 2 | 0 | 15 | 0.00 | 2 | 16 | 12.50 | 2 | 2 | 6.45 |
| 2–5 | 9 | 22 | 40.91 | 18 | 30 | 60.00 | 27 | 29 | 51.92 |
| 5–10 | 25 | 62 | 40.32 | 20 | 51 | 39.22 | 45 | 48 | 39.82 |
| 10–15 | 6 | 50 | 12.00 | 5 | 46 | 10.87 | 11 | 12 | 11.46 |
| > 15 | 0 | 350 | 0.00 | 9 | 305 | 2.95 | 9 | 10 | 1.37 |
| Total | 40 | 499 | 8.02 | 54 | 448 | 12.05 | 94 | 100 | 9.93 |
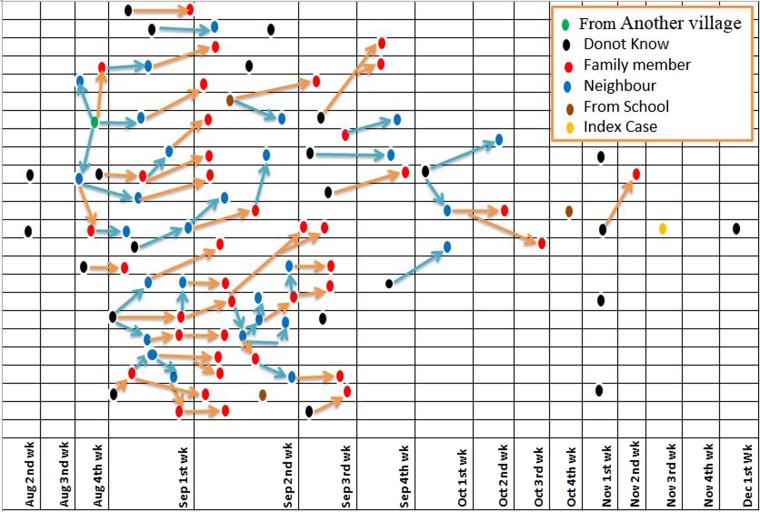
We could trace the epidemiological link in 72 case patients. Of these, 54% seemed to have contracted the illness from within the home environment. Here, the rate of exposure could be higher due to overcrowding and the joint family settings. The rest either acquired the illness while playing in the community (39%) or in the school settings (7%) (Figure 3 ).
Figure 3.
Epidemiological links of mumps outbreak in Tentuliapara village, Bhusandapur, Tangi, Odisha, India, August–December 2014.
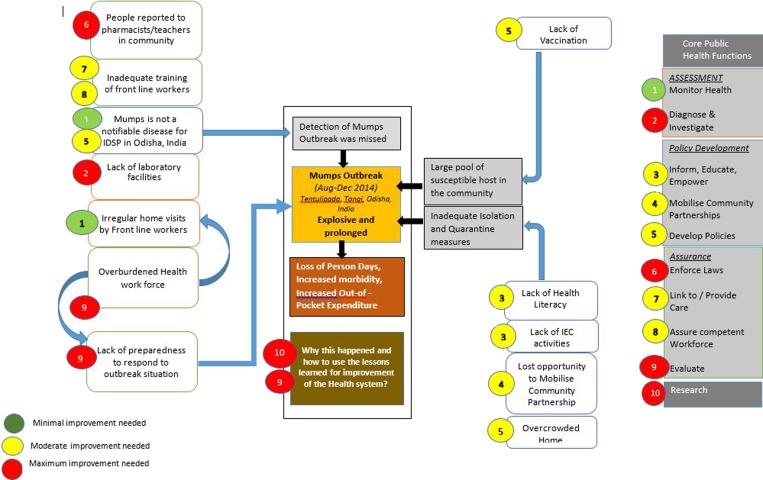
The policy development component of essential public health services was assessed by studying the treatment-seeking behavior of the case patients, which is reflective of the information, education and empowerment functions, and community-mobilizing activities (Figure 4 ). Of the 94 case patients, 51 (54%) reported to a MBBS doctor for treatment and spent an average of Rs 365 (∼6 USD) for treatment that lasted for around 6 days. Four of five such case patients were seen in a public health facility within 1 km (31 case patients) to 12 km (11 case patients) radius. Of the rest, 25 case patients (27%) were treated by a resident pharmacist from the Bhusandapur PHC during odd hours and this cost them average Rs 420 (∼7 USD) as he mainly prescribed costly antibacterial agents. Others sought advice from school teachers or unqualified practitioners (quacks). Eighty case patients (85%) were prescribed drugs from the allopathic system of medicine followed by homeopathic in nine case patients (10%) to gain relief from the symptoms. The remaining five case patients (5%) resorted to a local home remedy in the form of applying “banyan tree oil,” “salt and oil,” etc.
Figure 4.
Concept diagram depicting factors responsible for the mumps outbreak within the framework of the Essential Public Health Services in Tentuliapara village, Bhusandapur, Tangi, Odisha, India, August–December 2014.
We tried to find out whether the adult family members in the village knew about the various measures that could be undertaken to either contain the spread of the illness or prevent it. Only 64 (37%) of 174 people available for interview knew the importance of isolation, but they also expressed that in an overcrowded setting of their village it was impossible to prevent children from mixing with each other and none were aware about mumps vaccine. Understandably, in the absence of inclusion of mumps vaccine in the national immunization schedule, the coverage of mumps vaccination was zero.
The assessment domain of the essential public health services framework was analyzed by obtaining information through interviews of FLWs. The village health worker claimed that they had not seen any case of mumps in the village for nearly a decade. However, the very deficiency of surveillance as elaborated further in this article would argue against the reliability of any FLW to have appropriately recognized the disease. The FLWs were unaware of the explosive spread of mumps as they had not regularly visited the houses during the peak of the epidemic due to time constraints and work overload. They had also ignored the few sporadic cases that came to their notice as they were not aware that it was an outbreak-prone condition. According to them, antibiotics were the mainstay of treatment and that this illness usually occurred during the summer season. They were not aware of the mumps vaccine and felt that perhaps the measles vaccine could also protect from mumps. There were no facilities in any of the public health centers in the state of Odisha for confirming the existence of mumps using either serology or virus isolation techniques.
Under IDSP, usually a rapid response team stationed at district level carries out an immediate outbreak investigation to control further spread and prevent recurrence of outbreaks. Here, as mumps was never reported through the existing IDSP surveillance system, no such response was possible.
Discussion
The epidemiology of mumps during this outbreak was similar to that reported elsewhere in India1 and during the prevaccination era in developed countries.2
The fact that five generations of transmission had already occurred and the epidemic was almost over by the time it was detected implies that most of the key components of the essential public health services were hampered. Since the outbreak was missed by the existing health system in the area, we decided to identify the factors that led to its nondetection and assess the level of health system preparedness to deal with such situations in the future. These factors have been presented as a concept diagram (Figure 4) within the framework of 10 essential public health services used internationally to assess the performance of public health systems.4
The P form3 under IDSP that captures information on various epidemic-prone diseases does not include mumps. However, this list can be extended based on the requirements of individual states. The IDSP unit in Odisha has not included mumps in their P form, which was one of the most important reasons why this outbreak was perhaps missed as it was not perceived to be a notifiable disease. Further, the FLWs were not adequately trained in the epidemiology of mumps due its low priority, and therefore they never attempted to either investigate or notify the outbreak. Their lack of knowledge stopped a series of activities that could have been initiated to control the outbreak, namely, organize community efforts to mitigate the situation, sustain information education communication activities to promote effective isolation and quarantine, prevent case patients from visiting unqualified practitioners, opting for mumps vaccine for the susceptible contacts, etc. This perpetuated the transmission cycle. Besides these, overcrowding and unhygienic surroundings made matters worse.
Countries using the mumps vaccine in their national immunization schedules have demonstrated reduction in attack rates due to mumps (< 5%).6 A single dose of measles, mumps, and rubella vaccine (MMR) vaccine can be administered to a susceptible during an outbreak.7 The cost of one MMR dose is around Rs 76.5 (1.2 USD).8 We found that the entire community spending as out-of-pocket expenditure during this outbreak was around Rs 34,275.9 (538 USD). Instead, if they had purchased the vaccine, the cost for the entire community could have dropped by 35%. Currently, in India, there are mixed opinions regarding inclusion of mumps vaccine in the national immunization schedule.1,9–11 However, these decisions have to be based on reliable surveillance data, capturing the true disease burden. Reliability of the data generated through IDSP, in its current format, is highly questionable and its improvement is possible only through health systems research.12,13 Unless notification of mumps is made mandatory and data are analyzed as per WHO guidelines for surveillance of mumps, it is difficult to determine the cost-effectiveness of MMR vaccination or any other public health intervention.4
We could not do any laboratory confirmation of mumps infection due to lack of facilities in the public sector in Odisha. In India, very few public health facilities routinely process samples for presence of mumps virus. In a study by Mishra and others, genotyping and subtyping of mumps virus isolates during an outbreak investigation in Chandigarh revealed circulation of subtype G2 of genotype G in the community.14 Creating such infrastructure which is locally accessible is necessary to further strengthen the surveillance activities.
There is a shortage of competent health workforce, particularly in rural areas throughout India as well in Odisha.15–19 As per the Indian Public Health Standards, a PHC MO is expected to see around 40 patients daily and each PHC should cater to a population of up to 30,000.20 Only then can one expect the MO to devote at least two additional hours per day, twice in a week for field duties and monitoring. At our study site, the doctor saw 60 patients per day and had scanty staff for double the population expected to be served for providing community-based public health services. Thus, the MO was clearly overburdened and could not devote sufficient time for training and preparing his team for averting or managing outbreaks. Similarly, the FLWs were engaged in multiple programs that included preventive and curative service delivery, maintenance of records, administrative matters, etc., and are seldom able to effectively carry out surveillance activities in their catchment area. Health systems research, use of time-motion studies, and effective applications of health management principles could possibly resolve some of these issues.21,22
In our study area, due to the unavailability of 24 × 7 medical care, 43% of people had to depend on pharmacists, school teachers, or unqualified practitioners for dealing with mumps. This trend is worrisome and might need a multipronged approach, including filling up of vacant posts in the PHC, enforcements of laws to prevent unqualified practitioners from misleading people, training of FLWs in prehospital care and appropriate referral, improving the health literacy of the community members, mobilizing partnerships with self-help groups for promoting healthy behavior, etc.
Nearly 57% of case patients visited a medical doctor during this outbreak. Even then the system could not recognize the outbreak. The existing health information management system (HIMS) especially for surveillance of communicable disease in most parts of India including Odisha is in stage 1, that is, paper-based collection of data and reporting of aggregate data which are not amenable for any detailed and prompt analysis required for timely action. At times, the health workers are required to collect up to 3,000 data points of questionable quality, with manual entry across seven layers of government.23 Since analysis is manual, it is not amenable to trend analysis. For effective monitoring and evaluation of health programs, major reform in the HIMS in India is necessary.24 This would include transition to higher stages of HIMS by simplifying indicators and reducing duplication (stage 2), electronic storage and reporting (stage 3), introduction of operational information technology systems as a source of data for health information system (stage 4), and finally achievement of an end state of a fully comprehensive and integrated national health information system (stage 5).
Conclusions
Important lessons could be learned about the health system through this outbreak investigation. There is a need to improve the surveillance mechanism for better evidence generation and timely action, and to influence the policy decision of including MMR in the national immunization schedule. Continuous campaigning to improve the health literacy, particularly by engaging community partners will help reduce the burden of frontline health workers. Optimum utilization of management principles in health will improve the work efficiency. Besides, training of all involved in the surveillance system to deal with outbreaks and prevent their occurrence is of utmost importance. The Essential Public Health Service framework has enabled us to categorize the deficiencies in the health system effectively. The identification of level of improvement needed in each of the service areas might further prompt appropriate intervention to strengthen the health system and reduce the number of occurrences of various outbreaks in the future. However, the success of such analysis remains to be seen.
ACKNOWLEDGMENTS
The American Society of Tropical Medicine and Hygiene (ASTMH) assisted with publication expenses.
Footnotes
Authors' addresses: Sourabh Paul, Preetam B. Mahajan, Jyotiranjan Sahoo, Vikas Bhatia, and Sonu H. Subba, Department of Community and Family Medicine, All India Institute of Medical Sciences, Bhubaneswar, India, E-mails: drsourabh82@gmail.com, preetam3879@gmail.com, dr.jyotiranjan@gmail.com, drbhatiav@yahoo.com, and sonuhsubba2016@gmail.com.
References
- 1.Vashishtha VM, Yadav S, Dabas A, Bansal CP, Agarwal RC, Yewale VN, Thacker N, Kamath SS, Mehta PJ. IAP position paper on burden of mumps in India and vaccination strategies. Indian Pediatr. 2015;52:505–514. doi: 10.1007/s13312-015-0666-2. [DOI] [PubMed] [Google Scholar]
- 2.Galazka AM, Robertson SE, Kraigher A. Mumps and mumps vaccine: a global review. Bull World Health Organ. 1999;77:3–14. [PMC free article] [PubMed] [Google Scholar]
- 3.NCDC, DGHS, MOHFW, GOI Integrated Disease Surveillance Programme. 2005. www.idsp.nic.in Available at. Accessed June 25, 2015.
- 4.Centers for Disease Control and Prevention National Public Health Performance Standards (NPHPS) 2013. http://www.cdc.gov/nphpsp/essentialServices.html Available at. Accessed June 25, 2015.
- 5.World Health Organization WHO-Recommended Surveillance Standard of Mumps. 2008. http://www.who.int/immunization/monitoring_surveillance/burden/vpd/surveillance_type/passive/mumps_standards/en/ Available at. Accessed June 25, 2015.
- 6.Dayan GH, Rubin S. Mumps outbreaks in vaccinated populations: are available mumps vaccine effective enough to prevent outbreaks? Clin Infect Dis. 2008;47:1458–1467. doi: 10.1086/591196. [DOI] [PubMed] [Google Scholar]
- 7.Public Health Agency of Canada The National Advisory Committee on Immunization. Canadian Immunization Guide. 7th edition. 2006. http://publications.gc.ca/collections/Collection/HP40-3-2006E.pdf Available at. Accessed June 26, 2015.
- 8.Med India Network for Health Drug “Measles, Mumps, and Rubella Vaccine” Price List. 2015. http://www.medindia.net/drug-price/measles-mumps-and-rubella-mmr-vaccine/morupar.htm Available at. Accessed June 26, 2015.
- 9.Bhatnagar N, Kaur R, Gupta M. Introducing combined measles, mumps and rubella vaccine in Chandigarh, India: issues and concerns! Indian Pediatr. 2014;51:441–443. doi: 10.1007/s13312-014-0428-6. [DOI] [PubMed] [Google Scholar]
- 10.Gupta SK, Sosler S, Haldar P, Hombergh HVN, Bose AS. Introduction strategy of a second dose measles containing vaccine in India. Indian Pediatr. 2011;48:379–382. doi: 10.1007/s13312-011-0066-1. [DOI] [PubMed] [Google Scholar]
- 11.Ministry of Health and Family Welfare, Government of India Minutes and Recommendations of National Technical Advisory Group on Immunization (NTAGI) 2008. http://mohfw.nic.in/WriteReadData/l892s/8706936084National%20Technical%20Advisory%20Group%20on%20Immunization%20(NTAGI)%20minutes%20of%20meeting%20NEW.pdf Available at. Accessed June 26, 2015.
- 12.Iyer V, Azhar GS, Choudhury N, Dhruwey VS, Dacombe R, Upadhyay A. Infectious disease burden in Gujarat (2005–2011): comparison of selected infectious disease rates with India. Emerg Health Threats J. 2014;7:1–8. doi: 10.3402/ehtj.v7.22838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumar A, Goel MK, Jain RB, Khanna P. Tracking the implementation to identify gaps in integrated disease surveillance program in a block of district jhajjar (Haryana) J Family Med Prim Care. 2014;3:213–215. doi: 10.4103/2249-4863.141612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mishra B, Pujhari SK, Dhiman V, Mahalakshmi P, Bharadwaj A, Pokhrel S, Sharma D, Sharma M, Bhatia D, Ratho RK. Genotyping and subtyping of mumps virus isolates from the Indian subcontinent. Arch Virol. 2013;158:2359–2363. doi: 10.1007/s00705-013-1717-4. [DOI] [PubMed] [Google Scholar]
- 15.Rao M, Rao KD, Kumar AK, Chatterjee M, Sundararaman T. Human resources for health in India. Lancet. 2011;377:587–598. doi: 10.1016/S0140-6736(10)61888-0. [DOI] [PubMed] [Google Scholar]
- 16.Rao KD, Bhatnagar A, Berman P. So many, yet few: human resources for health in India. Hum Resour Health. 2012;10:1–9. doi: 10.1186/1478-4491-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hazarika I. Health workforce in India: assessment of availability, production and distribution. WHO South-East Asia J Public Health. 2013;2:106–112. doi: 10.4103/2224-3151.122944. [DOI] [PubMed] [Google Scholar]
- 18.Garg S, Singh R, Grover M. India's health workforce: current status and the way forward. Natl Med J India. 2012;25:111–113. [PubMed] [Google Scholar]
- 19.Health Nutrition Population, World Bank Health Worker Attitudes toward Rural Service in India: Results from Qualitative Research. 2010. http://siteresources.worldbank.org/HEALTHNUTRITIONANDPOPULATION/Resources/2816271095698140167/HealthWorkerAttitudesTowardRuralServiceinIndia.pdf Available at. Accessed June 25, 2015.
- 20.National Health Mission, Directorate General of Health Services Ministry of Health and Family Welfare Government of India Indian Public Health Standards (IPHS) Guidelines for Primary Health Centers Revised 2012. 2012. http://nrhm.gov.in/nhm/nrhm/guidelines/indian-public-health-standards.html Available at. Accessed June 25, 2015.
- 21.Columbia Global Centers|South Asia, Columbia University Improving the Performance of Accredited Social Health Activists in India. Working Paper No. 1. 2011. http://globalcenters.columbia.edu/files/cgc/pictures/Improving_the_Performance_of_ASHAs_in_India_CGCSA_Working_Paper_1.pdf Available at. Accessed June 25, 2015.
- 22.Finkler SA, Knickman JR, Hendrickson G, Lipkin M, Jr, Thompson WG. A comparison of work-sampling and time-and-motion techniques for studies in health services research. Health Serv Res. 1994;28:577–597. [PMC free article] [PubMed] [Google Scholar]
- 23.Vital Wave Consulting Health Information Systems in Developing Countries. A Landscape Analysis. 2009. http://www.minsa.gob.pe/ogei/conferenciaops/Recursos/43.pdf Available at. Accessed June 25, 2015.
- 24.World Health Organization Health Metrics Network. Country Health Information Systems a Review of the Current Situation and Trends. 2011. www.who.int/healthmetrics/news/chis_report.pdf Available at. Accessed June 25, 2015.