Abstract
Pellagra is a deficiency of niacin or its amino acid precursor, tryptophan, which presents with the classic four Ds: the characteristic dermatitis, diarrhea, dementia, and eventually death if left untreated. The incidence of pellagra is quite rare presently because of increased awareness and strategies such as vitamin fortification. However, the deficiency is still present in cultures that rely on maize as their primary source of sustenance. We report a recent outbreak in a catchment area in Kasese, Malawi, of 691 cases of pellagra which were successfully treated with niacin supplementation. We present this short report to highlight the importance of educating providers of at-risk populations about this diagnosis and to consider solutions for these populations to prevent further deficiencies.
Introduction
Pellagra is a deficiency of niacin and/or tryptophan, the amino acid precursor to niacin. The signs and symptoms form the classic four Ds: dermatitis, diarrhea, dementia, and death. First described in the eighteenth century, pellagra was a deadly disease that affected both developing and developed countries.1 With further understanding of the pathophysiology of pellagra in the twentieth century and vitamin fortification endeavors in the United States2 and internationally,3 this deficiency is rarely seen presently. Sporadic cases have been reported in the last few decades often relating to alcoholism,4,5 tuberculosis therapy,6 or malabsorption disorders7; however, several areas of the world continue to have outbreaks of the deficiency. The populations that are at the greatest risk are those that rely on unfortified Indian corn, or maize, as their primary food source. Examples in the literature describe these outbreaks in places such as Malawi, Mozambique, and Angola5,8,9 in the past; however, an outbreak of pellagra in Malawi in a non-refugee population has not been reported in the literature in over 20 years. We report an outbreak of 691 patients in the Kasese catchment area in Malawi.
Report of Cases
Between July 2015 and April 2016, a total of 691 patients presented to a local Kasese catchment area clinic in Malawi with the chief complaint of a rash in sun-exposed areas. The catchment clinic serves approximately 30,000 people, primarily of the Chichewa tribe. The rash was most commonly present on the arms bilaterally, around the neck, and on the lower legs. Examples of the rash are shown in Figures 1 –
Figure 2.
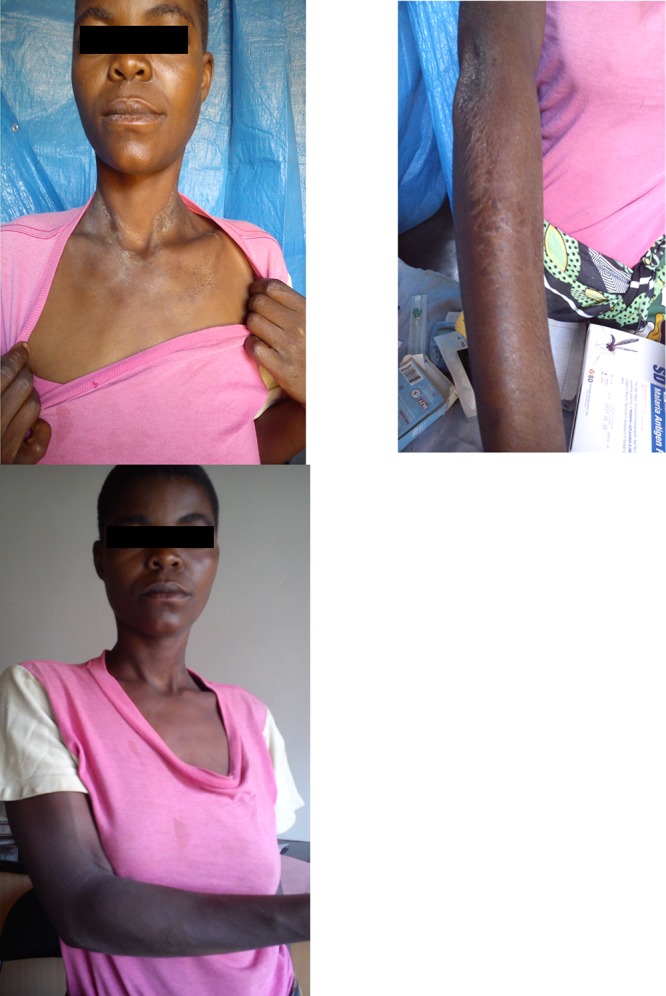
Female patient from Kasese catchment area with pellagra dermatitis of the forearm and neck (top) and after treatment with niacin (bottom).
3 . Providers at the clinic described the sudden occurrence of the rash as an outbreak, as approximately one in 10 patients were observed as having the rash during that time. Many of the patients had been treated for eczema in the past, but clinicians had not routinely seen rashes of this severity. The majority of patients complained of diarrhea, often preceding the rash. A small group of patients was affected only by lip ulcerations and/or glossitis. The patients had no history of concurrent rheumatologic or neurologic symptoms. Approximately 60% of the patients were female and 96% of the affected patients were over the age of 15. The majority of the patients were in extreme poverty and from remote tribal areas.
Figure 1.
Female patient from the Kasese catchment area with pellagra dermatitis of neck (left) and after treatment with niacin supplementation (right).
Figure 3.
Male patient from the Kasese catchment area with pellagra dermatitis of the forearm and neck (left) and after treatment with niacin supplementation (right).
Initially, these patients were treated with a generic emulsifying skin ointment with little improvement. After seeking input with colleagues in Malawi and the United States, pellagra was finally considered as a possible diagnosis. A treatment program was started in October 2015 in which patients were empirically treated with a vitamin B complex multivitamin containing 20 mg niacin given once or twice daily for 30 days. After the treatment period, the vast majority of the patients had complete resolution of the rash and associated symptoms. The small minority of patients that did not respond in the first 30 days responded well after continued vitamin therapy. In addition to vitamin supplementation, the patients were educated on the diagnosis and methods to increase the content of niacin in their diet.
Discussion
An outbreak of 691 cases of pellagra occurred in a Kasese catchment area beginning in July 2015. The clinical signs and symptoms and complete therapeutic response to treatment with niacin supplementation confirmed the diagnosis. In the patients described, their dermatitis matched the description of the characteristic skin rash in pellagra: a symmetrical erythematous rash in sun-exposed areas, most commonly the dorsal portions of hands and forearms, the feet and legs, forehead, upper neck, nose, and cheeks.3 Associated symptoms such as diarrhea, stomatitis, and cheilosis were also present in the Malawi patients and are commonly seen in pellagra. The diagnosis was confirmed by the significant clinical improvement reported in almost all patients after weeks of niacin supplementation.
Pellagra can be either primary or secondary with primary being most commonly associated with recent outbreaks in sub-Saharan Africa.8,9 Primary pellagra is because of a diet that is deficient in niacin or tryptophan whereas, secondary pellagra tends to occur when adequate quantities of niacin are present, but other conditions result in interference with absorption or processing. The highest incidences of primary pellagra are in geographic locations where Indian corn or maize is the dietary staple,10 and Malawi is one of the highest maize consuming countries in the world.11 The Malawian diet consists of little other alternative sources of niacin. Secondary causes are much less common and normally require parenteral rather than oral niacin supplementation, thus primary pellagra is much more likely in these cases.
One can question then, why did these patients suddenly present in 2015 and in such great numbers? Changes in diet have been a cause of outbreaks in Malawi in the past,8 however, no particular change was reported in these patients. Seat and others described similar outbreaks of pellagra in Angola from 1999 to 2004 which suggested that the difficulty of surveying and educating the population for pellagra leaves many cases of subclinical or clinical pellagra undiagnosed and untreated.9 Humanitarian efforts are impossible in many rural areas of Angola because of road access and safety issues, further complicating treatment and diagnostic efforts. One could speculate that this would explain the issue in the Malawi patient population described in this report, as many patients are from remote areas and the rash was not identified as pellagra until further inquiry was sought. The clinicians in the area had not seen pellagra in this sector of Malawi for many decades. At the outset, many clinicians mistook the rash for eczema and were unsuccessfully treating it with topical steroids. At the time of publication, the true cause of the outbreak is unknown and additional investigations will be needed to determine its exact cause. Additionally, clinicians will need to be educated about the typical signs and symptoms so that early recognition and intervention can occur.
For this patient population, treatment options are a primary concern at this time. Vitamin supplementation with niacin 100–300 mg daily in divided doses for children and 300–500 mg daily in divided doses for adults is an effective option that has been used in African outbreaks in the past.8,9 The recommended treatment is 300 mg of niacin daily for adults divided into 2–3 doses per day with 15 mg of niacin daily as maintenance dose daily after treatment.1 This method of treatment may not be sustainable for in Malawi as vitamin supplements are expensive, especially for these extremely impoverished areas. The distribution of the supplements is also an issue as the Kasese clinic serves a very large catchment area and would require great effort in ensuring continual supplementation. Alternative methods for increasing available niacin in the patients' diet are thus important to consider. Three possible solutions have been discussed with the clinicians at the Kasese clinic: fortification, diet diversification, and maize processing with alkaline hydrolysis.
Fortification endeavors have solved the issue of pellagra globally and was even recommended by the World Health Organization to African authorities in the 1970s.3 On further investigation of fortification in Malawi, it was found that many shopping centers in rural areas of Malawi near the affected patients do have commercially packaged maize flour that is fortified with niacin. However, most of the maize flour is processed within the household individually with whole maize that is unenriched. The expense of purchasing processed and fortified flour makes this solution difficult for many of the poorer Malawian people. For those who can afford it, it has been recommended that they consume the fortified flour to increase their daily niacin allowance.
A second solution would be to diversify the Malawian diet and educate the people on what foods to eat in addition to maize to increase the amount of niacin in their diet. Foods such as legumes, meat, eggs, fish, and milk are niacin rich and can help patients obtain the required daily allowance of niacin.10 This solution may be problematic in the more remote areas of the catchment area, especially in the dry season from April to November, where alternative food sources are especially scarce. But for those who can afford or obtain additional food types, it is important that the population is educated on adding niacin-rich foods to their diet.
The final solution involves altering the processing of maize with alkaline hydrolysis that increases the niacin content available for absorption. Cultures in Mexico and Central America have termed this process as nixtamalization where maize flour is washed with an alkaline solution such as limewater.12 The niacin, which is normally tightly bound to the maize, is released via alkaline hydrolysis, increasing the amount of available niacin by up to 3-fold.13 As a result, pellagra is rarely seen in Latin America, despite maize being the primary food source.14,15 Additionally, limewater is extremely cheap and effective, which would be ideal for the patient population described and can be performed in the remote areas with ease. The viability of this method will depend on adequate education in the maize processing techniques. Additionally, local sources of culturally acceptable foods high in B vitamins should be sought and promoted in the population affected.
These cases highlight the need for a concerted effort to educate the local tribes to help the population and clinic providers identify signs of pellagra and recommend potential treatment options, including the consideration of dietary changes in both content and processing. These cases also serve a point to consider the need for further nutritional surveillance in any maize-consuming country, as the diagnosis of pellagra continues to go unnoticed in many areas of the world.
Footnotes
Authors' addresses: George Matapandeu, Orant Charities, Primary Care Clinic, Kasese, Dowa, Malawi, E-mail: georgematapandeu@gmail.com. Samuel H. Dunn and Patti Pagels, Department of Family and Community Medicine, University of Texas Southwestern, Dallas, TX, E-mails: samuel.dunn@utsouthwestern.edu and patti.pagels@utsouthwestern.edu.
References
- 1.Hegyi J, Schwartz RA, Hegyi V. Pellagra: dermatitis, dementia, and diarrhea. Int J Dermatol. 2004;43:1–5. doi: 10.1111/j.1365-4632.2004.01959.x. [DOI] [PubMed] [Google Scholar]
- 2.Rajakumar K. Pellagra in the United States: a historical perspective. South Med J. 2000;93:272–277. http://www.jmcgowan.com/pellagra.pdf Available at. [PubMed] [Google Scholar]
- 3.World Health Organization . Pellagra and Its Prevention and Control in Major Emergencies. Geneva, Switzerland: World Health Organization; 2000. WHO/NHD. 00.10. [Google Scholar]
- 4.Klauder JV, Winkelman NW, Wolff B. Pellagra among chronic alcoholic addicts: a clinical and laboratory study. J Am Med Assoc. 1928;90:364–371. [Google Scholar]
- 5.Segula D, Banda P, Mulambia C, Kumwenda JJ. Case report: a forgotten dermatological disease. Malawi Med J. 2012;24:19–20. http://www.ncbi.nlm.nih.gov/pubmed/23638264 Available at. Accessed May 2, 2016. [PMC free article] [PubMed] [Google Scholar]
- 6.Darvay A, Basarab T, McGregor JM, Russell-Jones R. Isoniazid induced pellagra despite pyridoxine supplementation. Clin Exp Dermatol. 1999;24:167–169. doi: 10.1046/j.1365-2230.1999.00444.x. http://www.ncbi.nlm.nih.gov/pubmed/10354170 Available at. Accessed May 3, 2016. [DOI] [PubMed] [Google Scholar]
- 7.Lu J-Y, Yu C-L, Wu M-Z. Pellagra in an immunocompetent patient with cytomegalovirus colitis. Am J Gastroenterol. 2001;96:932–934. doi: 10.1111/j.1572-0241.2001.03659.x. [DOI] [PubMed] [Google Scholar]
- 8.Malfait P, Moren A, Dillon JC, Brodel A, Begkoyian G, Etchegorry MG, Malenga G, Hakewill P. An outbreak of pellagra related to changes in dietary niacin among-Mozambican refugees in Malawi. Int J Epidemiol. 1993;22:504–511. doi: 10.1093/ije/22.3.504. [DOI] [PubMed] [Google Scholar]
- 9.Seal AJ, Creeke PI, Dibari F, Cheung E, Kyroussis E, Semedo P, van den Briel T. Low and deficient niacin status and pellagra are endemic in postwar Angola. Am J Clin Nutr. 2007;85:218–224. doi: 10.1093/ajcn/85.1.218. [DOI] [PubMed] [Google Scholar]
- 10.Bogan KL, Brenner C. Nicotinic acid, nicotinamide, and nicotinamide riboside: a molecular evaluation of NAD+ precursor vitamins in human nutrition. Annu Rev Nutr. 2008;28:115–130. doi: 10.1146/annurev.nutr.28.061807.155443. [DOI] [PubMed] [Google Scholar]
- 11.Ranum P, Pena-Rosas JP, Garcia-Casal MN. Global maize production, utilization, and consumption. Ann N Y Acad Sci. 2014;1312:105–112. doi: 10.1111/nyas.12396. [DOI] [PubMed] [Google Scholar]
- 12.Caballero-Briones F, Iribarren A, Peña JL, Castro-Rodríguez R, Oliva AI. Recent advances on the understanding of the nixtamalization process. Sociedad Mexicana de Ciencia de Superficies y de Vacio. 2000;10:20–24. [Google Scholar]
- 13.Haytowitz D, Ahuja J, Showell B, et al. USDA National Nutrient Database for Standard Reference, release. 2015. p. 27.https://www.ars.usda.gov/ARSUserFiles/80400525/Data/SR27/sr27_doc.pdf Available at. Accessed January 23, 2017.
- 14.Miller SJ. Nutritional deficiency and the skin. J Am Acad Dermatol. 1989;21:1–30. doi: 10.1016/s0190-9622(89)70144-4. http://www.ncbi.nlm.nih.gov/pubmed/2663932 Available at. Accessed May 3, 2016. [DOI] [PubMed] [Google Scholar]
- 15.Brenton BP. Pellagra and nutrition policy lessons from the Great Irish Famine to the new South Africa. Nutr Anthropol. 1998;22:1–11. [Google Scholar]




