Abstract
Despite a decrease in incidence, smoking remains the most serious public health problem worldwide. Identification of the factors contributing to changes in willingness to quit smoking may aid the development of strategies that encourage smoking cessation. Pooled cross-sectional data from 11,924 smokers from the Korean National Health and Nutrition Examination Survey II–V were analyzed. The stages of change in smoking cessation were categorized as pre-contemplation, contemplation, and preparation. Baseline characteristics, socioeconomic factors, quality of life, psychological status, and smoking-related factors were compared between groups. The smokers were grouped as follows: 32.4% pre-contemplation, 54.4% contemplation, and 13.1% preparation. The proportion of smokers in the pre-contemplation group decreased (from 37.4% to 28.4%) from 2001 to 2012, while the proportion in the preparation group increased (from 6.4% to 18.1%). Compared with the preparation group, after adjusting for confounding factors, the pre-contemplation group was older [≥65 years-old; odds ratio (OR) = 1.40], more often single (OR = 1.38), less educated (elementary school or lower; OR = 1.93), less physically active in terms of walking (OR = 1.38) or performing strengthening exercises (OR = 1.61), smoked more heavily (≥20 cigarettes per day; OR = 4.75), and had a lower prevalence of chronic disease (OR = 0.76). Moreover, smokers who had never received education on smoking cessation were less willing to quit than those who had (OR = 0.44). In Korean smokers, the stages of change for smoking cessation were associated with age, education, marital status, chronic diseases, physical activity, and participation in smoking cessation programs.
Introduction
Smoking is the leading cause of a number of preventable diseases such as chronic obstructive pulmonary disease, cardio-cerebrovascular disease, and malignancy. In the United States, estimates show that tobacco contributes to approximately 480,000 premature deaths and costing approximately 289 billion dollars annually owing to direct healthcare expenditure and loss of productivity [1, 2]. Despite declines in the prevalence of current smoking, the annual burden of smoking-attributable mortality in the United States has remained above 400,000 for more than a decade and currently is estimated to be about 480,000 with millions more living with smoking-related diseases [2]. Furthermore, due to the slow decline in the prevalence of current smoking, the annual burden of smoking-attributable mortality can be expected to remain at high levels for decades into the future, with 5.6 million youth currently 0 to 17 years of age projected to die prematurely from a smoking-related illness [2]. Annual smoking-attributable economic costs in the United States estimated for the years 2009–2012 were between 289–332.5 billion dollars, including 132.5–175.9 billion dollars for direct medical care of adults, 151 billion dollars for lost productivity due to premature death estimated from 2005–2009, and 5.6 billion dollars (in 2006) for lost productivity due to exposure to secondhand smoke [2].
A diversity of individual and public-based interventions aimed at smoking cessation have been developed and implemented. The Transtheoretical Model (TTM) proposed by DiClemente et al. and Prochaska et al. allows the examination of behavior associated with willingness to quit smoking with a view to developing stage-matched interventions in the United States [3–5]. The TTM can be applied to assess behavior change and provides strategies to guide the individual through the “stages of change” to action and maintenance [6]. Several health behaviors that have been applied by the TTM include smoking cessation, exercise adoption, dietary fat reduction, mammography compliance, and reduced sun exposure and alcohol consumption [6–11].
According to the TTM, smokers are classified into one of three stages of change: pre-contemplation, contemplation, or preparation [3, 12]. The stages have been redefined since they were first conceived [13]. In order to design interventions for smoking cessation, information on the distribution and characteristics of smokers in each stage is required. The stage of change is also a useful predictor of smoking cessation and intermediate indicator of movement toward smoking cessation [14, 15].
Several national, cross-sectional studies have been reported on the relationship of basic demographic or socioeconomic factors with smoking cessation [7, 10, 16–19]. Besides their inconsistent results, only few studies included various factors related to socio-economic status, health status, psychosocial attributes, and smoking-related factors together in the analysis [10]. In these studies, factors such as age, marital status, socio-economic position, health status, and smoking characteristics were analyzed [7, 10, 16–19]. In the study of prospective cohort study for Taiwanese, demographic factors and mortality were analyzed but socioeconomic factors were not included [11]. Several studies reported that physical activity may be related to tobacco use [20, 21]. However, the study which investigated the relationships between the physical activity and willingness to smoking cessation were scarce.
The aim of this study was to determine the distributions of smokers in the three stages of change in smoking cessation and to evaluate the factors contributing to changes in willingness to quit smoking in a large representative sample of the Korean population.
Materials and methods
Study population
We used data from the Korean National Health and Nutrition Examination Survey II–V (KHANES) to classify the three stages of change. KNHANES I–VII is an ongoing cross-sectional survey of the civilian, conducted by the Korea Centers for Disease Control [22]. The methodology of the survey is as follows in brief: A stratified multistage clustered probability design was used to select a representative sample of civilian, non-institutionalized Koreans. KNHANES I, II, III were conducted in 1998, 2001, and 2005, respectively whereas KNHANES IV (2007–2009), V (2010–2012), VI (2013–2015), and VII (2016–2018, still in progress) were conducted continuously throughout the year and contained a larger number of participants. The survey is composed of a health interview, a nutrition survey, and a health examination survey (S1, S2 and S3 Tables). Data were collected by household interviews, and standardized physical examinations and analysis of fasting blood samples were performed in mobile health examination centers [23]. After registering personal information and signing a pledge of confidentiality, anyone can download the raw data from the KNHANES website [22]. Among the subjects who participated in the survey between 2001 and 2012, we identified 11,924 smokers aged ≥20 years who reported their readiness to quit smoking. Smokers were defined by those who replied positively to the following question: “Do you smoke?”
The Korea Centers for Disease Control and Prevention obtained written and informed consent from all participants, and the Institutional Review Board of Severance Hospital approved this study protocol (4-2014-0397).
Measures
We used data relating to two questions from the KNHANES questionnaire to classify the stages of change in smoking cessation:
-
Q1Have you made a 24-hour quit attempt in the previous 12 month?
-
1)Yes
-
2)No
-
1)
-
Q2Are you planning to quit smoking within the next 1 to 6 months?
-
1)Thinking of quitting smoking within the next month
-
2)Thinking of quitting smoking within the next 6 months
-
3)Thinking of quitting smoking at some point, but not within the next 6 months
-
4)Absolutely not thinking of quitting smoking
-
1)
The stages of change were defined as follows: pre-contemplation included smokers who responded to question 2 with answer 4; preparation included smokers who responded to question 2 with answer 1 and question 1 with answer 1; and contemplation included the rest.
The stages of change in smoking cessation were compared in relation to age, sex, body mass index, socioeconomic characteristics (household income, education defined by the highest level of schooling, occupation, and marital status), underlying diseases (hypertension, cardiovascular disease, and diabetes mellitus (DM)), pulmonary function test, quality of life (as assessed via the EuroQol five dimensions questionnaire (EQ-5D) questionnaire), psychological status, smoking-related factors (amount, duration, anti-smoking policy, and attendance at smoking cessation programs), alcohol use (ever-drinker; drinking more than once a month), and physical activity.
Physical activity was defined as follows. Intense physical activity included activities such as jogging, mountain climbing, cycling, swimming rapidly, playing soccer, basketball, jump rope, squash, or a tennis match of singles, at least 20 minutes, 3 times a week. Moderate physical activity included activities such as swimming slowly, playing a tennis match of doubles, volleyball, badminton, or table tennis. Muscle strengthening exercises included activities such as pushup, sit-up, dumbbell or barbell exercise, or exercising on the horizontal bar.
Statistical analysis
Categorical variables were analyzed by using the chi-square test, and continuous variables were analyzed by using analysis of variation. Change in proportion of precontemplation, contemplation, and preparation stages over the years was tested for trend with the linear-by-linear association method. Multinomial logistic regression analysis was performed for variables that showed significance in univariate analysis to identify factors that influence the stages of change in smoking cessation. Pre-contemplation and contemplation groups were compared with the preparation group. The results are described as odds ratio (OR) with 95% confidence intervals. Statistical analysis was performed by using SAS Enterprise Guide version 9.4 (SAS Institute Inc., Cary, NC, USA). For missing data, the pairwise deletion method was used, and a P-value <0.05 was deemed to be statistically significant in the analysis.
Results
Baseline characteristics
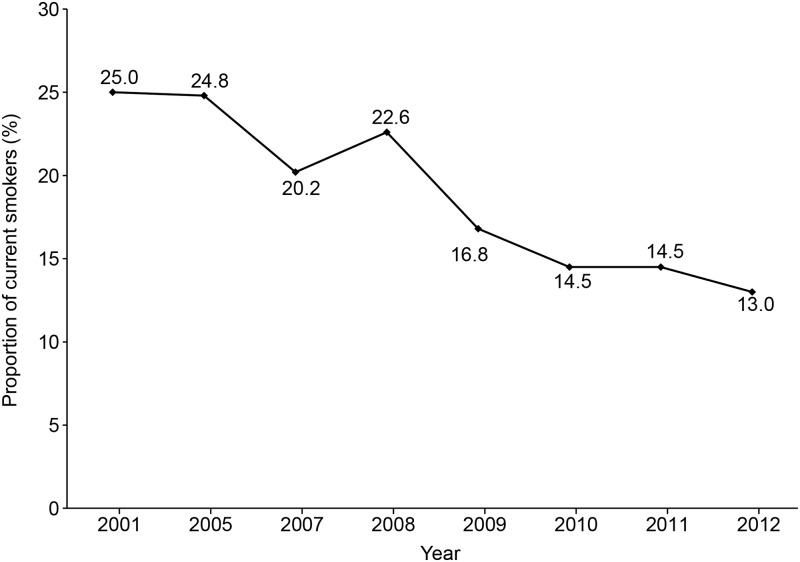
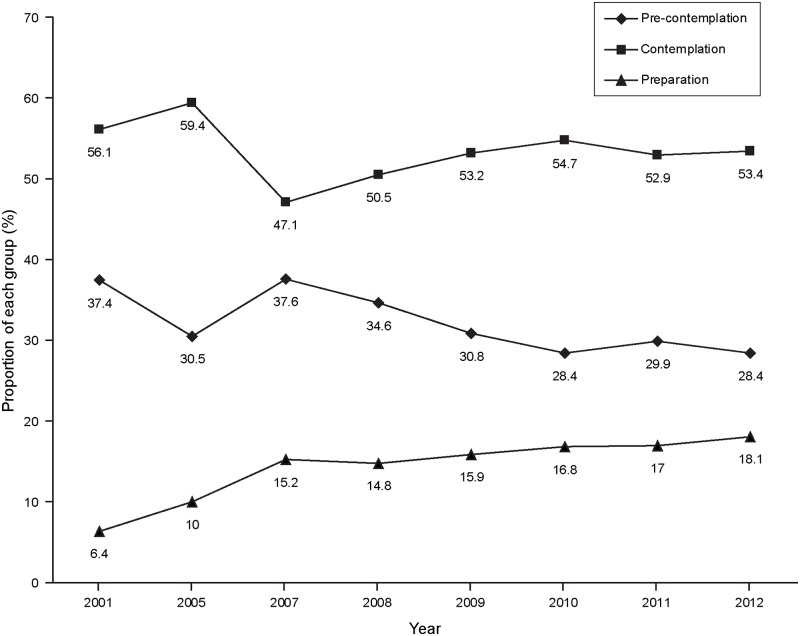
The study included 11,924 smokers and the proportion of current smokers decreased from 2001 to 2012 (from 25.0% to 13.0%; Fig 1). Among the smokers, 32.4%, 54.4%, and 13.1% were in pre-contemplation group, contemplation group, and preparation group, respectively. While the proportion of smokers in the pre-contemplation group decreased from 2001 to 2012 (from 37.4% to 28.4%; Ptrend < 0.001), the proportion in the preparation group increased (from 6.4% to 18.1%; Ptrend < 0.001)(Table 1, Fig 2).
Fig 1. Annual percentages of current smokers in each year from 2001 to 2012.
Table 1. Percentage of the pre-contemplation, contemplation, and preparation group for each yeara.
| Year | No. | Pre-contemplation | Contemplation | Preparation |
|---|---|---|---|---|
| 2001 | 2496 | 934 (37.4) | 1401 (56.1) | 161 (6.5) |
| 2005 | 2089 | 639 (30.5) | 1241 (59.4) | 209 (10.1) |
| 2007 | 585 | 220 (37.6) | 276 (47.2) | 89 (15.2) |
| 2008 | 1494 | 517 (34.6) | 755 (50.6) | 222 (14.8) |
| 2009 | 1661 | 512 (30.8) | 884 (53.3) | 265 (15.9) |
| 2010 | 1331 | 379 (28.5) | 728 (54.7) | 224 (16.8) |
| 2011 | 1223 | 366 (29.9) | 648 (53.0) | 209 (17.1) |
| 2012 | 1045 | 297 (28.4) | 558 (53.4) | 190 (18.2) |
a Data are presented as numbers (percentages)
Fig 2. Annual percentages of the pre-contemplation, contemplation, and preparation groups in each year from 2001 to 2012.
The demographic and clinical characteristics of the study population are shown in Table 2. Compared with the contemplation and preparation groups, the pre-contemplation group was older (48.4 years vs. 42.2 years and 44.4 years; P <0.001), and a larger proportion was unemployed or had a blue collar job and was in the lowest household income level bracket (25.4% vs. 16.5% and 17.3%; P <0.001) and the lowest education level bracket (26.9% vs. 12.4% and 14.2%; P <0.001). The pre-contemplation group had a higher prevalence of hypertension and DM, and a lower prevalence of cardiovascular disease. Moreover, the pre-contemplation group more often had an obstructive pattern in a pulmonary function test than did the preparation group.
Table 2. Baseline characteristics of the pre-contemplation, contemplation, and preparation groupsa.
| Baseline characteristics | Total No. (n = 11924) |
Pre-contemplation (n = 3864) |
Contemplation (n = 6491) |
Preparation (n = 1569) |
P-value |
|---|---|---|---|---|---|
| Age, yrs | 48.4±16.2 | 42.2±13.9 | 44.4±15.3 | <0.001 | |
| <45 | 6584 | 1747 (45.2) | 3955 (60.9) | 882 (56.2) | <0.001 |
| 45–64 | 3808 | 1341 (34.7) | 1991 (30.7) | 476 (30.3) | |
| ≥65 | 1532 | 776 (20.1) | 545 (8.4) | 211 (13.5) | |
| Sex | 0.02 | ||||
| Male | 10338 | 3316 (85.8) | 5679 (87.4) | 1343 (85.6) | |
| Female | 1586 | 548 (14.2) | 812 (12.6) | 226 (14.4) | |
| BMI, kg/m2 b | 23.5±3.4 | 23.7±3.3 | 23.8±3.3 | 0.005 | |
| Household income | <0.001 | ||||
| 1st quartile (lowest) | 2260 | 951 (25.4) | 1043 (16.5) | 266 (17.3) | |
| 2nd quartile | 3172 | 1024 (27.4) | 1722 (27.1) | 426 (27.5) | |
| 3rd quartile | 3165 | 912 (24.5) | 1811 (28.6) | 442 (28.7) | |
| 4th quartile (highest) | 3022 | 850 (22.7) | 1762 (27.8) | 410 (26.5) | |
| Education | <0.001 | ||||
| Elementary school or lower | 2051 | 1028 (26.9) | 802 (12.4) | 221 (14.2) | |
| Middle school | 1350 | 511 (13.4) | 680 (10.6) | 159 (10.2) | |
| High school | 4855 | 1439 (37.6) | 2769 (42.9) | 647 (41.4) | |
| College/university or higher | 3585 | 849 (22.1) | 2200 (34.1) | 536 (34.2) | |
| Occupation | <0.001 | ||||
| White collar jobc | 4606 | 1228 (32.0) | 2728 (42.3) | 650 (41.7) | |
| Blue collar jobd or unemployed | 7243 | 2620 (68.0) | 3726 (57.7) | 907 (58.3) | |
| Marriage | 0.001 | ||||
| Singlee | 2840 | 973 (26.5) | 1552 (25.6) | 315 (21.6) | |
| Married | 8361 | 2699 (73.5) | 4518 (74.4) | 1144 (78.4) | |
| Underlying diseasef | |||||
| Hypertension | 1403 | 507 (17.3) | 680 (13.3) | 216 (15.4) | <0.001 |
| Dyslipidemia | 554 | 144 (4.9) | 313 (6.1) | 97 (6.8) | 0.071 |
| Cerebral vascular accident | 160 | 66 (2.2) | 73 (1.4) | 21 (1.4) | 0.083 |
| Cardiovascular disease | 178 | 58 (1.9) | 78 (1.5) | 42 (2.9) | 0.001 |
| Pulmonary tuberculosis | 497 | 163 (5.5) | 250 (4.9) | 84 (5.9) | 0.469 |
| Asthma | 391 | 136 (4.6) | 199 (3.9) | 56 (3.9) | 0.563 |
| Diabetes mellitus | 669 | 242 (8.2) | 320 (6.2) | 107 (7.6) | 0.017 |
| Chronic renal failure | 25 | 8 (0.2) | 15 (0.2) | 2 (0.1) | 0.855 |
| Bronchiectasis | 17 | 3 (0.1) | 11 (0.3) | 3 (0.3) | 0.423 |
| Depression | 1048 | 329 (8.5) | 552 (8.5) | 167 (10.6) | 0.02 |
| Pulmonary function test | <0.001 | ||||
| FEV1/FVC <70% | 848 | 326 (22.4) | 386 (16.1) | 136 (17.8) | |
| FEV1/FVC ≥70% | 3767 | 1128 (77.6) | 2010 (83.9) | 629 (82.2) |
a Categorical variables were analyzed by using the chi-square test, and continuous variables were analyzed by using analysis of variation. Data are presented as numbers (percentages) and ± values are means±standard deviation.
b n = 3288 in the pre-contemplation group, n = 4432 in the contemplation group, and n = 1442 in the preparation group
c White collar jobs include administrators, experts, and office workers.
d Blue collar jobs include farmers, fishermen, and other manual workers.
e Single includes divorced, separated, and never-married subjects.
f n = 2930 in the pre-contemplation group, n = 5090 in the contemplation group, and n = 1408 in preparation group except for depression. All the underlying diseases were diagnosed by a medical provider.
BMI, body mass index; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity.
Quality of life and psychological status
Table 3 shows data relating to quality of life, as assessed via the EQ-5D questionnaire, and the psychological status of the three groups. Compared with the contemplation and preparation groups, the pre-contemplation group had more problems with mobility, self-care, usual activities, and pain/discomfort. More smokers in the pre-contemplation group reported a lack of stress. However, a larger proportion of smokers in this group had experienced suicidal ideation within the past year (19.3% vs. 16.0% and 16.1%; P = 0.001).
Table 3. Quality of life and psychological status in the pre-contemplation, contemplation and preparation groupsa.
| Variables | Total No. (n = 11924) |
Pre-contemplation (n = 3864) |
Contemplation (n = 6491) |
Preparation (n = 1569) |
P-value |
|---|---|---|---|---|---|
| EQ-5Db | |||||
| Mobility | |||||
| No problems | 8300 | 2470 (84.4) | 4595 (90.5) | 1235 (88.0) | <0.001 |
| Problemsc | 1104 | 455 (15.6) | 480 (9.5) | 169 (12.0) | |
| Self-care | |||||
| No problems | 9074 | 2784 (95.2) | 4940 (97.4) | 1350 (96.2) | <0.001 |
| Problemsd | 329 | 140 (4.8) | 135 (2.6) | 54 (3.8) | |
| Usual activities | |||||
| No problems | 8643 | 2607 (89.1) | 4746 (93.5) | 1290 (91.9) | <0.001 |
| Problems | 761 | 318 (10.9) | 329 (6.5) | 114 (8.1) | |
| Pain/discomfort | |||||
| No problems | 7364 | 2221 (75.9) | 4029 (79.4) | 1114 (79.3) | 0.001 |
| Problems | 2038 | 703 (24.1) | 1045 (20.6) | 290 (20.7) | |
| Anxiety/depressione | |||||
| No problems | 8252 | 2543 (86.9) | 4488 (88.5) | 1221 (86.9) | 0.068 |
| Problems | 1145 | 381 (13.1) | 581 (11.5) | 183 (13.1) | |
| Stress | |||||
| Yes | 8144 | 2361 (80.6) | 4544 (89.3) | 1239 (88.0) | <0.001 |
| No | 1284 | 569 (19.4) | 546 (10.7) | 169 (12.0) | |
| Suicidal ideation within past 1 yr | 1611 | 566 (19.3) | 817 (16.0) | 228 (16.1) | 0.001 |
| Suicidal attempt within past 1 yr | 124 | 44 (1.1) | 63 (0.9) | 17 (1.1) | 0.015 |
| Psychiatric counseling within past 1 yrb | 162 | 51 (1.7) | 85 (1.6) | 26 (1.8) | 0.897 |
a Categorical variables were analyzed by using the chi-square test. Data are presented as numbers (percentages).
b n = 2930 in the pre-contemplation group, n = 5090 in the contemplation group, and n = 1408 in the preparation group
c People who have difficulty with walking.
d People who have difficulty with dressing or taking a bath.
e The Anxiety and depression are based on self-report about their general mood.
Smoking, alcohol, and physical activity
Table 4 shows data relating to smoking history, alcohol use, and physical activity. Compared with the contemplation and preparation groups, the pre-contemplation group smoked more cigarettes per day and had smoked for a longer time. Smokers in the pre-contemplation group were more often permitted to smoke in the workplace (79.8% vs. 72.7% and 68.8%; P = 0.013) or at home (77.8% vs. 66.4% and 60.0%; P <0.001) and to be never-drinkers (5.7% vs. 3.3% and 3.0%; P <0.001). They less often experienced smoking cessation education within past 1year (7.3% vs. 12.4% and 16.4%; P <0.001) and exercised or performed physical activity.
Table 4. Smoking, alcohol use, and physical activity between the pre-contemplation, contemplation and preparation groupsa.
| Variables | Total No. (n = 11924) |
Pre-contemplation (n = 3864) |
Contemplation (n = 6491) |
Preparation (n = 1569) |
P-value |
|---|---|---|---|---|---|
| Smoking history | |||||
| No. of cigarettes smoked per dayb | 16.9±9.2 | 15.2±8.0 | 12.1±8.1 | <0.001 | |
| <10 | 2293 | 589 (15.3) | 1153 (17.8) | 551 (35.1) | <0.001 |
| 10–19 | 4473 | 1263 (32.7) | 2637 (40.6) | 573 (36.5) | |
| ≥20 | 5155 | 2010 (52.1) | 2700 (41.6) | 445 (28.4) | |
| Duration of smoking, monthsb | 288±196.1 | 216.1±151.9 | 212.1±173.1 | <0.001 | |
| Attempt smoking cessationc | |||||
| For oneselfd | 4426 | 640 (76.1) | 3051 (84.1) | 735 (84.8) | <0.001 |
| For otherse | 912 | 201 (23.9) | 579 (15.9) | 132 (15.2) | |
| Anti-smoking policy at workplacef | |||||
| Yes | 339 | 69 (20.2) | 227 (27.3) | 43 (31.2) | 0.013 |
| No | 971 | 273 (79.8) | 603 (72.7) | 95 (68.8) | |
| Anti-smoking policy at homeg | |||||
| Yes | 631 | 140 (22.2) | 411 (33.6) | 80 (40.0) | <0.001 |
| No | 1423 | 490 (77.8) | 813 (66.4) | 120 (60.0) | |
| Existence of a regular smoker at homef | 3018 | 1063 (36.2) | 1648 (32.3) | 307 (21.8) | <0.001 |
| Smoking cessation education experience within past 1 yrg | 7339 | 167 (7.3) | 478 (12.4) | 197 (16.4) | <0.001 |
| Alcohol usef | |||||
| Ever-drinkerh | 9049 | 2763 (94.3) | 4921 (96.6) | 1365 (96.9) | <0.001 |
| Never-drinker | 379 | 167 (5.7) | 169 (3.3) | 43 (3.0) | |
| Physical activityf | |||||
| Number of days of intense physical activityi (per week) | |||||
| None | 5882 | 2009 (68.5) | 3058 (60.0) | 815 (57.8) | <0.001 |
| One day or more | 3543 | 921 (31.4) | 2031 (39.9) | 592 (42.1) | |
| Number of days of moderate physical activityj (per week) | |||||
| None | 5268 | 1832 (62.4) | 2700 (53.0) | 738 (52.4) | <0.001 |
| One day or more | 4154 | 1098 (37.4) | 2389 (46.9) | 669 (47.6) | |
| Number of days of walking (per week) | |||||
| None | 1247 | 522 (17.8) | 565 (11.1) | 160 (11.3) | <0.001 |
| One day or more | 8179 | 2408 (82.2) | 4524 (88.9) | 1247 (88.6) | |
| Number of days of muscle strengthening exercisesk (per week) | |||||
| None | 6604 | 2226 (75.9) | 3519 (69.1) | 859 (61.0) | <0.001 |
| One day or more | 2822 | 704 (24.0) | 1570 (30.9) | 548 (38.9) | |
a Categorical variables were analyzed by using the chi-square test, and continuous variables were analyzed by using analysis of variation. Data are presented as numbers (percentages) and ± values are means±standard deviation.
b n = 3862 in the pre-contemplation group, n = 6491 in the contemplation group, and n = 1569 in the preparation group
c n = 841 in the pre-contemplation group, n = 3630 in the contemplation group, and n = 867 in the preparation group
d Self-awareness or concern for their own health.
e Concern or request from other people.
f n = 2930 in the pre-contemplation group, n = 5089 in the contemplation group, and n = 1407 in the preparation group
g n = 2291 in the pre-contemplation group, n = 3849 in the contemplation group, and n = 1199 in the preparation group
h Drinking more than once a month
i Intense physical activity includes activities such as jogging, mountain climbing, cycling, swimming rapidly, playing soccer, basketball, jump rope, squash, or a tennis match of singles, at least 20 minutes, 3 times a week.
j Moderate physical activity includes activities such as swimming slowly, playing a tennis match of doubles, volleyball, badminton, or table tennis
k Muscle strengthening exercises include activities such as pushup, sit-up, dumbbell or barbell exercise, or exercising on the horizontal bar
Multivariate analysis
Multivariate analysis was performed for variables that showed significance in univariate analysis (Table 5). Relative to the preparation group, the pre-contemplation group was older (≥65 years of age; OR = 1.40), less educated (elementary school or lower; OR = 1.93), more often single (OR = 1.38) and anxious or depressed (OR = 0.75), smoked more heavily (≥20 cigarettes per day; OR = 4.75), and had a lower level of physical activity in terms of walking (OR = 1.38) or performing strengthening exercises (OR = 1.61) and a lower prevalence of chronic diseases (hypertension, DM, or cardiovascular disease)(OR = 0.76). Moreover, smokers without smoking cessation education experience within past 1 year were less willing to quit smoking (OR = 0.44). Compared with the preparation group, the contemplation group contained more women (OR = 0.79), heavy smokers (OR = 2.98), and single individuals (OR = 1.26), fewer individuals with previous chronic disease (OR = 0.82), and fewer physically active individuals (OR = 1.42), and fewer individuals with smoking cessation education experience within past 1 year (OR = 0.70).
Table 5. Multivariate analysis for factors associated with stage of change in smoking cessationa.
| Variables | Pre-contemplation (n = 2025) |
Contemplation (n = 3338) |
|---|---|---|
| Demographic factors | ||
| Age, yr | ||
| 45–64 (vs. <45) | 1.10 (0.90–1.34) | 1.02 (0.85–1.23) |
| ≥65 (vs. <45) | 1.40 (1.03–1.89) | 0.77 (0.58–1.03) |
| Sex (male vs. female) | 0.83 (0.64–1.07) | 0.79 (0.63–0.99) |
| Underlying diseases | ||
| Chronic diseasee (vs. none) | 0.76 (0.63–0.93) | 0.82 (0.68–0.98) |
| Depression (vs. none) | 0.81 (0.61–1.08) | 1.03 (0.79–1.35) |
| Social factors | ||
| Household income | ||
| 1st quartile (vs. 4th quartile) | 1.03 (0.78–1.36) | 0.94 (0.72–1.22) |
| 2nd quartile (vs. 4th quartile) | 0.93 (0.75–1.17) | 0.84 (0.69–1.03) |
| 3rd quartile (vs. 4th quartile) | 0.86 (0.69–1.07) | 0.91 (0.75–1.10) |
| Education | ||
| Elementary school or lower (vs. college/university or higher) | 1.93 (1.42–2.63) | 0.93 (0.70–1.25) |
| Middle school (vs. college/university or higher) | 1.44 (1.07–1.94) | 0.87 (0.66–1.15) |
| High school (vs. college/university or higher) | 1.24 (1.01–1.53) | 0.94 (0.79–1.13) |
| Occupation | ||
| White collar jobb (vs. blue collar jobc or unemployed) | 0.96 (0.79–1.16) | 0.94 (0.79–1.11) |
| Marital status | ||
| Singled (vs. married) | 1.38 (1.12–1.70) | 1.26 (1.04–1.53) |
| Smoking and alcohol related factors | ||
| No. of cigarettes smoked per day | ||
| 10–19 (vs. <10) | 2.59 (2.10–3.20) | 2.21 (1.84–2.65) |
| ≥20 (vs. <10) | 4.75 (3.82–5.93) | 2.98 (2.46–3.62) |
| Never-drinker (vs. ever drinkerf) | 1.38 (0.91–2.10) | 1.32 (0.88–1.99) |
| Life style factors | ||
| Suicidal ideation within past 1 yr (vs. none) | 1.20 (0.95–1.52) | 1.08 (0.87–1.35) |
| Smoking cessation education experience within past 1yr (vs.none) | 0.44 (0.34–0.56) | 0.70 (0.57–0.86) |
| Number of days of walking exercise (per week) | ||
| None (vs. 1 day or more) | 1.38 (1.11–1.72) | 1.01 (0.82–1.25) |
| Number of days of strengthening exerciseg (per week) | ||
| None (vs. 1 day or more) | 1.61 (1.35–1.01) | 1.42 (1.22–1.66) |
| EQ-5D | ||
| Mobility, problemsh (vs. no problems) | 0.91 (0.67–1.23) | 0.92 (0.69–1.24) |
| Self-care, problemsi (vs. no problems) | 0.85 (0.54–1.32) | 0.93 (0.60–1.43) |
| Usual activities, problems (vs. no problems) | 1.04 (0.71–1.52) | 0.96 (0.67–1.39) |
| Pain/discomfort, problems (vs. no problems) | 1.06 (0.84–1.33) | 1.05 (0.84–1.30) |
| Anxiety/depression, problems (vs. no problems) | 0.75 (0.56–0.99) | 0.81 (0.62–1.05) |
a Multinomial logistic regression analysis was performed to identify factors that influence the stages of change in smoking cessation. Pre-contemplation and contemplation groups were compared with the preparation group. Data are presented as odds ratios (95% confidence intervals) compared with the preparation group (n = 1063).
b White collar job includes administrators, experts, and office workers.
c Blue collar job includes manual workers such as farmers, fishermen, and others.
d Single includes divorced, separated, and never married subjects.
e Chronic disease includes hypertension, diabetes mellitus, or cardiovascular accident.
f Drinking more than once a month.
g Muscle strengthening exercises include activities such as pushup, sit-up, dumbbell or barbell exercise, or exercising on the horizontal bar.
h People who have difficulty with walking.
i People who have difficulty with dressing or taking a bath.
EQ-5D, EuroQol five dimensions questionnaire
Discussion
This study demonstrated significant associations between the stages of change in smoking cessation in the Korean population and the following: age, education level, marital status, cardiovascular disease, amount of smoking, physical activity, and education regarding smoking cessation. Our study population comprised 32.4% in the pre-contemplation group, 54.4% in the contemplation group, and 13.1% in the preparation group. While the proportion of smokers in the pre-contemplation group decreased from 2001 to 2012, the proportion in the preparation group increased.
The stages of change have been redefined since their conception was first introduced in 1984 [3, 12]. Initially, there were five stages (pre-contemplation, contemplation, action, maintenance, and relapse) [5, 9]. Preparation was added by DiClemente et al. in 1991 [3], and smokers were then divided into three groups of pre-contemplation, contemplation, or preparation groups [3, 7, 11, 12, 17]. In those studies, relapse was considered as an event that terminates the other phases prompting a cyclical movement back through the initial stages, not a different stage [3, 7, 10–12, 17]. We used data from the KNHANES to classify the three stages of change, in accordance with previous reports as follows: the pre-contemplation stage includes smokers who do not seriously consider quitting within the next 6 months, and the preparation stage includes smokers who “intend to quit” or “seriously think about quitting” in the next 30 days and have made a 24-hour quit attempt in the previous 12 months. The rest were classified as the contemplation stage [3, 7, 11, 12, 17].
Distribution of smokers according to stages of change for smoking cessation
The distribution of smokers according to stages of change for smoking cessation has been investigated in a number of countries at different times with different definition of stage of change. Mbulo et al. used Global Adult Tobacco Survey data to categorize smokers into different stages of change [7]. In this paper, most smokers across all countries were in the pre-contemplation stage, followed in order by the contemplation stage and the preparation stage [7]. Wewers et al. reported that 59.1%, 33.2%, and 7.7% of American respondents were in the pre-contemplation, contemplation, and preparation stages, respectively, in 1992–1993 [18]. Subsequent surveys in the United States showed similar distributions in 1995–1996 and 1998–1999 [18]. In thet study by Cambell et al. between 2003–2004, 39.6%, 43.4%, and 13.9% of 594 Australians were assigned to the pre-contemplation, contemplation, and preparation groups, respectively; these values are similar to those in our study of the Korean population [16]. Daoud et al. reported that 61.8%, 23.8%, 14.4% were in the pre-contemplation, contemplation stage, and preparation stage, respectively, among Arab men between 2012–2013 [10]. The preparation group showed the least proportion of less than 15% in all studies. However, different distributions between studies might be attributed to differences in definition, race, culture, study duration, and local anti-smoking policies [7, 16, 18]. Wewers et al used similar definitions that we did while Cambell et al. and Daoud et al. used broader definition for preparation group. Moreover, the age was limited to less than 65 years old in the study of Daoud et al. [7, 16, 18].
To promote public health, the Korean government implemented various anti-smoking services and policies after the National Health Promotion Act was announced in 1995 [24, 25]. These include the designation of public places as non-smoking areas and the curtailment of cigarette advertisements. A nationwide smoking cessation program was introduced in 253 health centers in 2005, and free nicotine replacement therapy and individual counseling were provided. In addition, small-scaled nationwide quitline smoking cessation services were initiated in 2006, and the price of cigarettes was increased nearly twofold in 2015. These efforts might be related with augmenting the smoker’s willingness to quit smoking in Korea.
Factors associated with the stages of change in smoking cessation
Most of the studies that examined the demographic and socioeconomic factors associated with the stages of change in smoking cessation reported socioeconomic status as significant [17–19]. According to age-stratified analyses, smoking characteristics such as number of cigarettes smoked, duration of smoking, and age at smoking onset were also related to the stages of change [17]. Our study provides further evidence that as levels of education and income increase, the proportion of smokers in the pre-contemplation group decreases, and the proportions in the contemplation and preparation groups increase. Moreover, those who had smoked for a longer time and who smoked more cigarettes per day were more likely to be in the pre-contemplation group. Among the smokers who attempted to quit, more attempted for themselves than for others, although more smokers in the pre-contemplation group attempted to quit for others. In this context, being single was another important factor influencing the stage of change in smokers.
Psychiatric disorders, such as major depressive disorders and anxiety disorders, are known to increase the risk of smoking and decrease the likelihood of quitting [26–28].: Stanton et al. reported that conditions such as anxiety, depression, and substance abuse were related to higher tobacco use, although proportion of cigarette smoking declined significantly over time among adults with no chronic condition [29]. Anxiety, stressful life events, and social support were psychological factors relevant to the stages of changes, as reported by Daoud et al. [10]. In our study, although the proportion of people diagnosed with depression was lower in the pre-contemplation group, levels of suicidal ideation and attempted suicide were higher. According to the EQ-5D questionnaire, smokers in the pre-contemplation group were less anxious and depressed; however, this questionnaire might be too simplistic to accurately evaluate the severity and type of anxiety or depression. Moreover, those with a low level of physical activity, which is associated with an increased likelihood of depression, were less willing to quit [30]. In the study of Loprinzi et al. maintenance of regular physical activity among young daily smokers may help to facilitate smoking cessation [31]. However, the relationship between physical activity and willingness to quit smoking has not been evaluated clearly.
Progression through the stages of change in smoking cessation requires changes in knowledge, attitude, and beliefs in regard to smoking, particularly for those who are unwilling to attempt quitting [16]. Our study suggests that additional effort is required for the elderly, those with a lower level of education or exercise, those without chronic disease or smoking cessation education experience, those who are single or anxious/depressed, or those who smoked more heavily in pre-contemplation stage. In comtemplation stage, additional effort is required for women, heavy smokers, singles, those without chronic disease, those without smoking cessation education experience, or those with low levels of exercise. Both individual and public health approaches are needed to increase quitting rates. On an individual level, clinicians can encourage smokers to quit by presenting the potential benefits of quitting, the harmful effects of smoking, and the coping strategies for barriers to quitting [32, 33]. Education in regard to smoking cessation was strongly associated with change in our study. Similarly, the stages of change were related to knowledge of the hazards of smoking and a positive attitude toward smoking prevention in a study of current smokers by Daoud et al. [10] and to smoking-related thoughts such as the pros and cons of smoking, the temptation to smoke, and the ability to resist smoking in a study of Taiwanese male smokers by Luh et al. [11]. However, all smokers coming for smoking cessation programs are not ready for action and they should be grouped according to which stage of change they are in. The interventions vary according to smoker’s individual stages and using the ten processes of change previously presented could help to identify strategies specific to each stage leading to individualized approach [5, 34]. Public health approaches include increases in cigarette taxes, ban smoking in public places, smoking cessation campaigns with prohibition of tobacco advertising, and the placement of warnings or pictures on cigarettes products [35]. According to our analysis, anti-smoking policies in the workplace and at home have led to smokers to become more willing to quit.
Unlike previous studies, we considered marital status, anti-smoking policies in the workplace and smoke-free rules in homes, anti-smoking education, psychological status, physical activity, and quality of life in our analyses. The information obtained will facilitate the development of interventions that encourage progression through the stages of change in smoking cessation and will allow strategies to be tailored to the characteristics of the smoker.
Limitations
This study has several limitations. First, it was a cross-sectional and observational study, and thus it is difficult to clarify the cause-and-effect relationships between the associated factors and the stages of change in smoking cessation. However, the large study population might compensate for the methodological bias. Moreover, data for multiple years were integrated in one data set, but adjustment of years of survey did not show differences. Longitudinal cohort study is warranted to overcome this limitation. Second, data on smokers who had since quit were not available; this information is important in identifying the type of smokers that will actually quit. However, the aim of this study was to evaluate the factors that contribute to changes in the willingness of smokers to stop smoking, and this analysis was accomplished by comparing pre-contemplation, contemplation, and preparation groups. Third, the questions related with stage of change in smoking cessation in this study are not exactly in accord with previous traditional criteria [3, 36]. KNHANES is designed to assess the health and nutritional status of Koreans, so other previous definitions which can be applied with questions in KNHANES were searched and used in this study [3, 11, 12, 17]. Owing to differences in the definition of the stages of change, it may be difficult to directly compare the results of all relevant studies. Fourth, the level of nicotine dependence is an important factor in smoking cessation, and there are commonly used measures of nicotine dependence such as Fagerström Tolerance Questionnaire, Fagerström Test for Nicotine Dependence and Heaviness of Smoking Index. [37–39] Although the number of cigarettes per day is an important indicator for nicotine dependence, other variables related to nicotine dependence scales were not available in the KNHANES. Lastly, we used the pairwise deletion method to deal with missing data, so each computed statistic may be based on a different subset of cases. However, the missing number in the final model was 1135 (9.5% of total population), and the distributions of the important variables were not significantly different between total population and subpopulation in the final model.
Conclusions
In conclusion, relative to the preparation group, the pre-contemplation group was older, less educated, more often single and anxious or depressed, smoked more heavily, and had a lower level of physical activity in terms of walking or performing strengthening exercises and a lower prevalence of chronic diseases (hypertension, DM, or cardiovascular disease). Moreover, smokers without smoking cessation education experience within past 1 year were less willing to quit smoking. Compared with the preparation group, the contemplation group contained more women, heavy smokers, and single individuals. Moreover, fewer smokers in the contemplation group had chronic diseases, were physically active, and experienced smoking cessation education within past 1 year. Future interventions to encourage smokers to move from the pre-contemplation to contemplation and preparation stages of smoking cessation should take these factors into consideration.
Supporting information
(DOC)
(DOC)
(DOC)
Acknowledgments
This study was supported by a faculty research grant of Yonsei University College of Medicine for (6-2014-0158). We thank to all members of the Korean Smoking Cessation Study Group: Jae Jeong Shim (Korea University), Tae Hoon Jung (Kyoungpook National University), Yeong Hun Choe (Chonbuk National University), Hyo-Jeong Lim (Veterans Health Service Medical Center), Yong C. Lee(Chonbuk National University), Jinyoung An (Chungbuk National University), Kyeong-Cheol Shin (Yeungnam University), Jae Woo Jung (Chung-Ang University), Yeon Mok Oh (Univeristy of Ulsan), Hyoung Kyu Yoon (Catholic University of Korea), Ki Uk Kim (Pusan National University), Yu-Il Kim (Chonnam National University), Yu Jin Kim (Gachon University), Jae Yeol Kim (Chung-Ang University), Ju Ock Kim (Chungnam National University), Huijung Kim (Wonkwang University), Ju Ock Na (Soonchunhyang University), Jeong-Seon Ryu (Inha University), Won-Yeon Lee (Yonsei University), Myung Jae Park (KyungHee University), Young Sik Park (Seoul National University), Joo Hun Park (Ajou University), Hye Jung Park (Yonsei University), Ji Young Seo (Sungkyunkwan University), and Choon Hee Sohn (Dong-A University)
Abbreviations
- BMI
body mass index
- EQ-5D
EuroQol five dimensions questionnaire
- FEV1
forced expiratory volume in 1 second
- FVC
forced vital capacity
- KNHANES
Korean National Health and Nutrition Examination Survey
- OR
odds ratio
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by a faculty research grant from Yonsei University College of Medicine (6-2014-0158). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Jamal A, Agaku IT, O'Connor E, King BA, Kenemer JB, Neff L. Current cigarette smoking among adults—United States, 2005–2013. MMWR Morb Mortal Wkly Rep. 2014;63(47):1108–12. Epub 2014/11/27. [PMC free article] [PubMed] [Google Scholar]
- 2.National Center for Chronic Disease P, Health Promotion Office on S, Health. Reports of the Surgeon General. The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2014.
- 3.DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS. The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. Journal of consulting and clinical psychology. 1991;59(2):295–304. Epub 1991/04/01. [DOI] [PubMed] [Google Scholar]
- 4.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change. Applications to addictive behaviors. Am Psychol. 1992;47(9):1102–14. Epub 1992/09/01. [DOI] [PubMed] [Google Scholar]
- 5.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. Journal of consulting and clinical psychology. 1983;51(3):390–5. Epub 1983/06/01. [DOI] [PubMed] [Google Scholar]
- 6.Laforge RG, Velicer WF, Richmond RL, Owen N. Stage distributions for five health behaviors in the United States and Australia. Preventive medicine. 1999;28(1):61–74. Epub 1999/02/12. 10.1006/pmed.1998.0384 [DOI] [PubMed] [Google Scholar]
- 7.Mbulo L, Palipudi KM, Nelson-Blutcher G, Murty KS, Asma S. The Process of Cessation Among Current Tobacco Smokers: A Cross-Sectional Data Analysis From 21 Countries, Global Adult Tobacco Survey, 2009–2013. Prev Chronic Dis. 2015;12:E151 Epub 2015/09/18. 10.5888/pcd12.150146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cahill K, Lancaster T, Green N. Stage-based interventions for smoking cessation. Cochrane Database Syst Rev. 2010; (11):Cd004492. Epub 2010/11/12. [DOI] [PubMed] [Google Scholar]
- 9.Prochaska JO, DiClemente CC, Velicer WF, Ginpil S, Norcross JC. Predicting change in smoking status for self-changers. Addictive behaviors. 1985;10(4):395–406. Epub 1985/01/01. [DOI] [PubMed] [Google Scholar]
- 10.Daoud N, Hayek S, Sheikh Muhammad A, Abu-Saad K, Osman A, Thrasher JF, et al. Stages of change of the readiness to quit smoking among a random sample of minority Arab male smokers in Israel. BMC Public Health. 2015;15:672 Epub 2015/07/17. 10.1186/s12889-015-1950-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luh DL, Chen HH, Liao LR, Chen SL, Yen AM, Wang TT, et al. Stages of change, determinants, and mortality for smoking cessation in adult Taiwanese screenees. Prev Sci. 2015;16(2):301–12. Epub 2014/02/08. 10.1007/s11121-014-0471-5 [DOI] [PubMed] [Google Scholar]
- 12.Etter JF, Sutton S. Assessing 'stage of change' in current and former smokers. Addiction (Abingdon, England). 2002;97(9):1171–82. Epub 2002/08/30. [DOI] [PubMed] [Google Scholar]
- 13.Etter JF, Perneger TV. A comparison of two measures of stage of change for smoking cessation. Addiction (Abingdon, England). 1999;94(12):1881–9. Epub 2000/03/16. [DOI] [PubMed] [Google Scholar]
- 14.Prochaska JO, Goldstein MG. Process of smoking cessation. Implications for clinicians. Clin Chest Med. 1991;12(4):727–35. Epub 1991/12/01. [PubMed] [Google Scholar]
- 15.Velicer WF, Prochaska JO, Rossi JS, Snow MG. Assessing outcome in smoking cessation studies. Psychol Bull. 1992;111(1):23–41. Epub 1992/01/01. [DOI] [PubMed] [Google Scholar]
- 16.Campbell S, Bohanna I, Swinbourne A, Cadet-James Y, McKeown D, McDermott R. Stages of change, smoking behaviour and readiness to quit in a large sample of indigenous Australians living in eight remote north Queensland communities. Int J Environ Res Public Health. 2013;10(4):1562–71. Epub 2013/04/18. 10.3390/ijerph10041562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jhun HJ, Seo HG. The stages of change in smoking cessation in a representative sample of Korean adult smokers. J Korean Med Sci. 2006;21(5):843–8. Epub 2006/10/18. 10.3346/jkms.2006.21.5.843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wewers ME, Stillman FA, Hartman AM, Shopland DR. Distribution of daily smokers by stage of change: Current Population Survey results. Preventive medicine. 2003;36(6):710–20. Epub 2003/05/15. [DOI] [PubMed] [Google Scholar]
- 19.Velicer WF, Fava JL, Prochaska JO, Abrams DB, Emmons KM, Pierce JP. Distribution of smokers by stage in three representative samples. Preventive medicine. 1995;24(4):401–11. Epub 1995/07/01. 10.1006/pmed.1995.1065 [DOI] [PubMed] [Google Scholar]
- 20.de Siqueira Galil AG, Cupertino AP, Banhato EF, Campos TS, Colugnati FA, Richter KP, et al. Factors associated with tobacco use among patients with multiple chronic conditions. International journal of cardiology. 2016;221:1004–7. Epub 2016/07/22. 10.1016/j.ijcard.2016.07.041 [DOI] [PubMed] [Google Scholar]
- 21.Ben Taleb Z, Ward KD, Asfar T, Jaber R, Bahelah R, Maziak W. Smoking Cessation and Changes in Body Mass Index: Findings From the First Randomized Cessation Trial in a Low-Income Country Setting. Nicotine & tobacco research: official journal of the Society for Research on Nicotine and Tobacco. 2016. Epub 2016/09/11. [DOI] [PubMed] [Google Scholar]
- 22.Korea Centers for Disease Control and Prevention. Korea National Health and Nutrition Examination Survey Data. Korea National Health and Nutrition Examination Survey website. http://knhanes.cdc.go.kr/. Accessed on March 1, 2015.
- 23.Kim DS, Kim YS, Jung KS, Chang JH, Lim CM, Lee JH, et al. Prevalence of chronic obstructive pulmonary disease in Korea: a population-based spirometry survey. American journal of respiratory and critical care medicine. 2005;172(7):842–7. Epub 2005/06/25. 10.1164/rccm.200502-259OC [DOI] [PubMed] [Google Scholar]
- 24.Ministry of Health and Welfare. Anti-smoking policies in Korea. No Smoke Guide website. https://www.nosmokeguide.or.kr/mbs/nosmokeguide/subview.jsp?id=nosmokeguide_030102010000. Accessed March 2, 2015.
- 25.Cho HJ. The status and future challenges of tobacco control policy in Korea. J Prev Med Public Health. 2014;47(3):129–35. Epub 2014/06/13. 10.3961/jpmph.2014.47.3.129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anda RF, Williamson DF, Escobedo LG, Mast EE, Giovino GA, Remington PL. Depression and the dynamics of smoking. A national perspective. Jama. 1990;264(12):1541–5. Epub 1990/09/26. [PubMed] [Google Scholar]
- 27.Breslau N, Novak SP, Kessler RC. Psychiatric disorders and stages of smoking. Biol Psychiatry. 2004;55(1):69–76. Epub 2004/01/07. [DOI] [PubMed] [Google Scholar]
- 28.Breslau N, Kilbey M, Andreski P. Nicotine dependence, major depression, and anxiety in young adults. Arch Gen Psychiatry. 1991;48(12):1069–74. Epub 1991/12/01. [DOI] [PubMed] [Google Scholar]
- 29.Stanton CA, Keith DR, Gaalema DE, Bunn JY, Doogan NJ, Redner R, et al. Trends in tobacco use among US adults with chronic health conditions: National Survey on Drug Use and Health 2005–2013. Preventive medicine. 2016;92:160–8. Epub 2016/10/30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Teychenne M, Ball K, Salmon J. Physical activity and likelihood of depression in adults: a review. Preventive medicine. 2008;46(5):397–411. Epub 2008/02/22. 10.1016/j.ypmed.2008.01.009 [DOI] [PubMed] [Google Scholar]
- 31.Loprinzi PD, Walker JF. Association of Longitudinal Changes of Physical Activity on Smoking Cessation Among Young Daily Smokers. Journal of physical activity & health. 2016;13(1):1–5. Epub 2015/05/13. [DOI] [PubMed] [Google Scholar]
- 32.Anderson JE, Jorenby DE, Scott WJ, Fiore MC. Treating tobacco use and dependence: an evidence-based clinical practice guideline for tobacco cessation. Chest. 2002;121(3):932–41. Epub 2002/03/13. [DOI] [PubMed] [Google Scholar]
- 33.Zwar N, Richmond R, Borland R, Stillman S, Cunningham M, Litt J. Smoking cessation guidelines for Australian general practice. Aust Fam Physician. 2005;34(6):461–6. Epub 2005/06/03. [PubMed] [Google Scholar]
- 34.Prochaska JO, Velicer WF, DiClemente CC, Fava J. Measuring processes of change: applications to the cessation of smoking. Journal of consulting and clinical psychology. 1988;56(4):520–8. Epub 1988/08/01. [DOI] [PubMed] [Google Scholar]
- 35.Levy DT, Chaloupka F, Gitchell J. The effects of tobacco control policies on smoking rates: a tobacco control scorecard. J Public Health Manag Pract. 2004;10(4):338–53. Epub 2004/07/06. [DOI] [PubMed] [Google Scholar]
- 36.Schumann A, Meyer C, Rumpf HJ, Hannover W, Hapke U, John U. Stage of change transitions and processes of change, decisional balance, and self-efficacy in smokers: a transtheoretical model validation using longitudinal data. Psychology of addictive behaviors: journal of the Society of Psychologists in Addictive Behaviors. 2005;19(1):3–9. Epub 2005/03/24. [DOI] [PubMed] [Google Scholar]
- 37.Boyle RG, Jensen J, Hatsukami DK, Severson HH. Measuring dependence in smokeless tobacco users. Addictive behaviors. 1995;20(4):443–50. Epub 1995/07/01. [DOI] [PubMed] [Google Scholar]
- 38.Etter JF. A comparison of the content-, construct- and predictive validity of the cigarette dependence scale and the Fagerstrom test for nicotine dependence. Drug and alcohol dependence. 2005;77(3):259–68. Epub 2005/03/01. 10.1016/j.drugalcdep.2004.08.015 [DOI] [PubMed] [Google Scholar]
- 39.Fagerstrom K, Russ C, Yu CR, Yunis C, Foulds J. The Fagerstrom Test for Nicotine Dependence as a predictor of smoking abstinence: a pooled analysis of varenicline clinical trial data. Nicotine & tobacco research: official journal of the Society for Research on Nicotine and Tobacco. 2012;14(12):1467–73. Epub 2012/04/03. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.