Supplemental Digital Content is available in the text.
Keywords: diet, hypertension, sodium
Abstract
Background:
Most US adults consume excess sodium. Knowledge about the dietary sources of sodium intake is critical to the development of effective reduction strategies.
Methods:
A total of 450 adults were recruited from 3 geographic locations: Birmingham, AL (n=150); Palo Alto, CA (n=150); and the Minneapolis–St. Paul, MN (n=150), metropolitan areas. Equal numbers of women and men from each of 4 race/ethnic groups (blacks, Asians, Hispanics, and non-Hispanic whites) were targeted for recruitment. Four record-assisted 24-hour dietary recalls were collected from each participant with special procedures, which included the collection of duplicate samples of salt added to food at the table and in home food preparation.
Results:
Sodium added to food outside the home was the leading source of sodium, accounting for more than two thirds (70.9%) of total sodium intake in the sample. Although the proportion of sodium from this source was smaller in some subgroups, it was the leading contributor for all subgroups. Contribution ranged from 66.3% for those with a high school level of education or less to 75.0% for those 18 to 29 years of age. Sodium inherent to food was the next highest contributor (14.2%), followed by salt added in home food preparation (5.6%) and salt added to food at the table (4.9%). Home tap water consumed as a beverage and dietary supplement and nonprescription antacids contributed minimally to sodium intake (<0.5% each).
Conclusions:
Sodium added to food outside the home accounted for ≈70% of dietary sodium intake. This finding is consistent with the 2010 Institute of Medicine recommendation for reduction of sodium in commercially processed foods as the primary strategy to reduce sodium intake in the United States.
Clinical Trial Registration:
URL: http://www.clinicaltrials.gov. Unique identifier: NCT02474693.
Editorial, see p 1784
Sodium reduction has been a component of the Dietary Guidelines for Americans since 1980.1 However, despite long-standing recommendations to limit sodium, most American adults and children consume too much. The prevalence of excess US dietary sodium intake in 2009 to 2012 ranged, by age group, from 85.0% to 93.7%.2 On the basis of the presumption that most sodium consumed came from sodium added to commercially packaged and prepared foods, in 2010, the Institute of Medicine recommended gradual stepwise reductions of the sodium content of these foods as the primary strategy to reduce intake.3
Although numerous studies have examined the contributions to sodium intake of specific foods, food categories, and supplements/antacids,4–7 the amount of discretionary salt added by the consumer (eg, at the table) is difficult to estimate. Thus, most studies are unable to estimate sodium intake from all sources and the relative contribution of each source. In 1991, Mattes and Donnelly8 reported that sodium added to food in commercial processing was the primary source of sodium in the diet (77.0% of total intake), followed by sodium inherent in food (11.6%), sodium from salt added to food at the table (6.2%), sodium from salt added to food in home cooking (5.1%), and water ingested as a beverage (0.1%).
Given the changes in national food production and consumption patterns in the 25 years since the Mattes and Donnelly8 article was published, an update is warranted. Furthermore, the sample size in that study was small (n=62 adults), and participants were homogeneous (predominately female and white from 1 US geographic region). Thus, we conducted a study to provide contemporary data on the major sources contributing to total sodium intake in a larger, more diverse sample of adults, with a primary focus on the proportion of total intake from sodium added to food outside the home (eg, added during commercial processing and preparation).
Methods
Population and Recruitment
Between December 2013 and December 2014, a convenience sample of 450 adults was recruited from 3 geographic locations: Birmingham, AL (n=150); Palo Alto, CA (n=150); and the Minneapolis–St. Paul, MN (n=150), metropolitan areas. We recruited into the study equal numbers of women and men from each of 4 race/ethnic groups (blacks, Asians, Hispanics, and non-Hispanic whites).
Recruitment and data collection activities were conducted by the University of Alabama at Birmingham, Stanford University, and the University of Minnesota–Twin Cities. Recruitment strategies included invitations extended to university employees at each of the universities; study fliers posted around campus and at various community health fairs; university and community newspaper advertisements; and e-mail messages sent to study participants in past studies who had consented to being notified of future studies.
During a screening telephone interview, potential participants were determined eligible if they were between 18 (Palo Alto and Minneapolis–St. Paul) or 19 (Birmingham) and 75 years old, were generally healthy, and had a telephone. Exclusion criteria included being pregnant or breastfeeding or having chronic kidney disease or diabetes insipidus. Participants at all sites were offered a $10 token of appreciation for each completed 24-hour diet recall interview (total of 4 interviews or $40). All participants provided written informed consent. The institutional review board at each participating institution and the Centers for Disease Control and Prevention reviewed and approved the study procedures.
Overview of Data Collection and Measurements
The dietary assessment procedures were designed to allow quantification of the amount and proportion of sodium from the following sources: (1) salt added to food at the table; (2) salt added to food in home food preparation; (3) sodium from home tap water consumed as a beverage; (4) sodium that is inherent to food; (5) sodium that is added to food in processing outside the home; and (6) sodium from dietary supplements and nonprescription antacids.
Participants attended 1 clinic visit and completed 4 record-assisted telephone 24-hour dietary recall interviews over an 11-day period. Duplicate samples of salt added to food at the table and in home food preparation were collected by the participant on each of the 4 days for which dietary recalls were collected.
Before the clinic visit, participants were asked if their home drinking water was from a private well. In addition, they were asked if their tap water was softened or if it was filtered by a home filtration system. If they responded affirmatively to 1 or 2 of these questions, they were instructed to bring a sample of their home tap water to their clinic visit using a study provided collection kit.
At the clinic visit, tap water samples were collected from participants as appropriate, and a questionnaire was administered to obtain information about demographics, smoking, and general health. Height was measured with a wall-mounted stadiometer, and weight was measured with a digital scale. Four telephone 24-hour dietary recall interviews were scheduled with the participants within the next 11 days. Three of the recalls were scheduled to capture eating for a weekday, and 1 recall was scheduled to capture eating on a weekend day. Participants were given a food record form to complete the day before each scheduled recall. Participants were instructed to record on the form the foods eaten and, for foods to which salt was added in home preparation, the total yield (total amount prepared). Participants were given salt collection kits to use in collecting duplicate samples of salt added to their food at the table and in home food preparation. They were instructed to collect the duplicate samples the day before each scheduled telephone recall, thus aligning collection with the 24-hour dietary recall period.
Collection of Duplicate Samples of Salt
For collection of salt added to food at the table, participants were instructed to shake the same amount of salt added to food at the table throughout the day into a plastic resealable collection bag provided by the study for this purpose. The same instructions were provided to collect duplicate amounts of salt added to food in home food preparation, with a separate bag used for each food item prepared with salt. In addition, participants were asked to record the name of the food item and to share the instructions and collection bags with anyone else in their household who may have prepared food at home the day of collection.
Preaddressed postage-paid envelopes were provided for mailing the duplicate salt samples to the study center. At each study center, the contents of each bag were weighed on a digital scale, and the weight was entered into a spreadsheet.
Dietary Recall Collection
All 24-hour dietary recalls were administered by staff at the University of Minnesota Nutrition Coordinating Center who were trained and certified in the administration of dietary recalls following study procedures. Nutrition Data System for Research software (developed by the Nutrition Coordinating Center, University of Minnesota, Minneapolis) was used for the administration and analysis of the recalls.9 Use of dietary supplements and nonprescription antacids over the 24-hour recall period was assessed with the Nutrition Data System for Research Dietary Supplement Assessment Module.10
A variety of study-specific procedures were used during recall collection and processing to ensure that the sources of sodium of interest in this study could be ascertained. For example, participants were asked whether certain types of foods (baked goods, mixed dishes, salads, cooked vegetables, etc) had been prepared at home. If the food had been prepared at home, they were asked whether salt had been added in preparation. If it had, they were asked additional questions such as the yield of the recipe (how much was made).
Procedures for Calculating Sodium Intake by Source
Postrecall data processing procedures included calculating sodium from home tap water consumed as a beverage using participant-specific sodium content values for water. If the participant’s home tap water was from a public water supply and he or she did not have a water softener or water filtration system in the home, the sodium content of water in his or her community as published in municipal water quality reports was used. For the remaining participants, the water sample turned in at the clinic visit was chemically analyzed (Traut Water Analysis Laboratory, Wiate Park, MN) to determine its sodium content.
Sodium from salt added to food at the table and in home food preparation was calculated from data from the duplicate salt samples. The duplicate sample data were added to the dietary recall records following a detailed set of data calculation and entry rules.
To estimate the amount of sodium in foods that was inherent and added outside the home, we adhered to the definitions developed by Mattes and Donnelly.8 These researchers defined inherent as sodium that is naturally present in food, and they defined sodium added to food outside the home as sodium contributed by the addition of sodium compounds in processing food outside the home. Examples of these compounds include sodium chloride, sodium benzoate, sodium phosphate, and sodium bicarbonate (baking soda). For every food, the proportion of sodium in the food considered to be added to food outside the home was estimated with a set of rules and procedures (online-only Data Supplement).
The validity of sodium intake estimates from the 24-hour dietary recalls was evaluated in a subset of study participants (n=150). Four 24-hour urine collections were obtained from the subset over the same time period that the 24-hour dietary recalls were collected. A full description of methods and findings of the validation component of the study is being reported in another article. To summarize key findings, mean 24-hour urinary sodium level in the subset was 3198 compared with 3325 mg/d from the 24-hour dietary recalls (P=0.30).
Data Analysis
For analyses carried out to describe sodium intake by source, means and mean proportions11 were calculated. For each study participant, mean daily sodium intake overall and from each source was calculated by averaging the sodium intake estimates from the four 24-hour dietary recalls collected from the participant. One participant had only 3 recalls, and the average was calculated from 3 instead of 4 recalls for this person. The mean estimates were used in analyses to characterize sodium intake. Because food intake is known to vary from weekday to weekend days, data were weighted so that results reflect the appropriate balance of weekday and weekend days in a week.
To characterize sources of sodium among population subgroups, analyses were carried out stratified by sex, age, level of education, race, and geographic region. Multivariate regression analyses were conducted to determine whether differences between groups were statistically significant (P<0.05). If the overall F test for a demographic variable was significant, pairwise comparisons were conducted. Analyses were carried out with SAS version 9.3 (SAS Institute Inc, Cary, NC).
Results
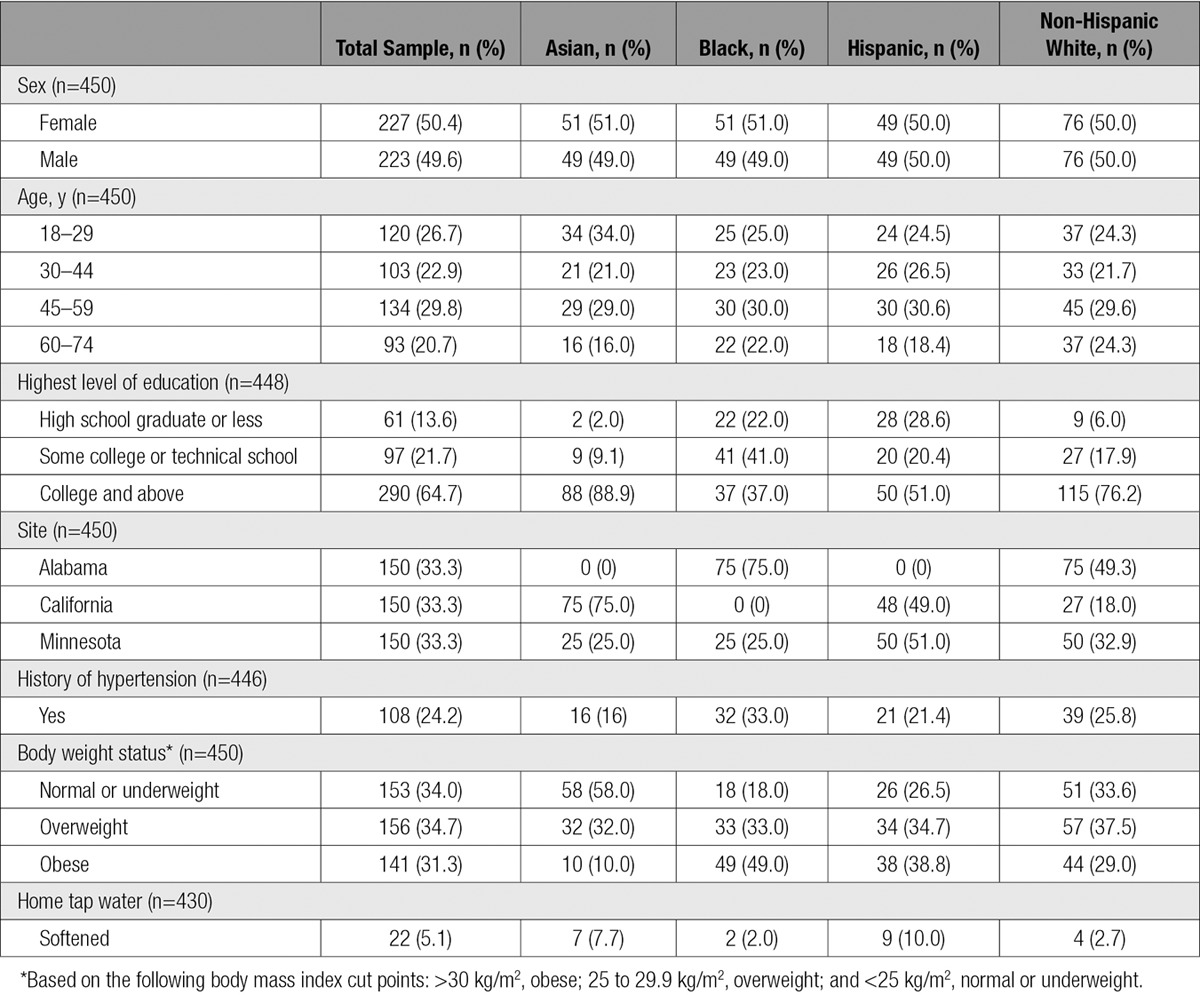
In accord with recruitment targets, 450 participants were recruited; one-half of participants were female, and one-third were from each of the 3 study sites (Table 1). The numbers of participants were approximately equal by age group, and about one-third of participants were non-Hispanic white with approximately equal numbers of Asian, black, and Hispanic participants. Demographics by race are provided in Table 1. Recruitment targets for each ethnic group varied by site; consequently, distribution of race by site is unequal.
Table 1.
Demographic and Health Characteristics of Study Participants Overall and by Race
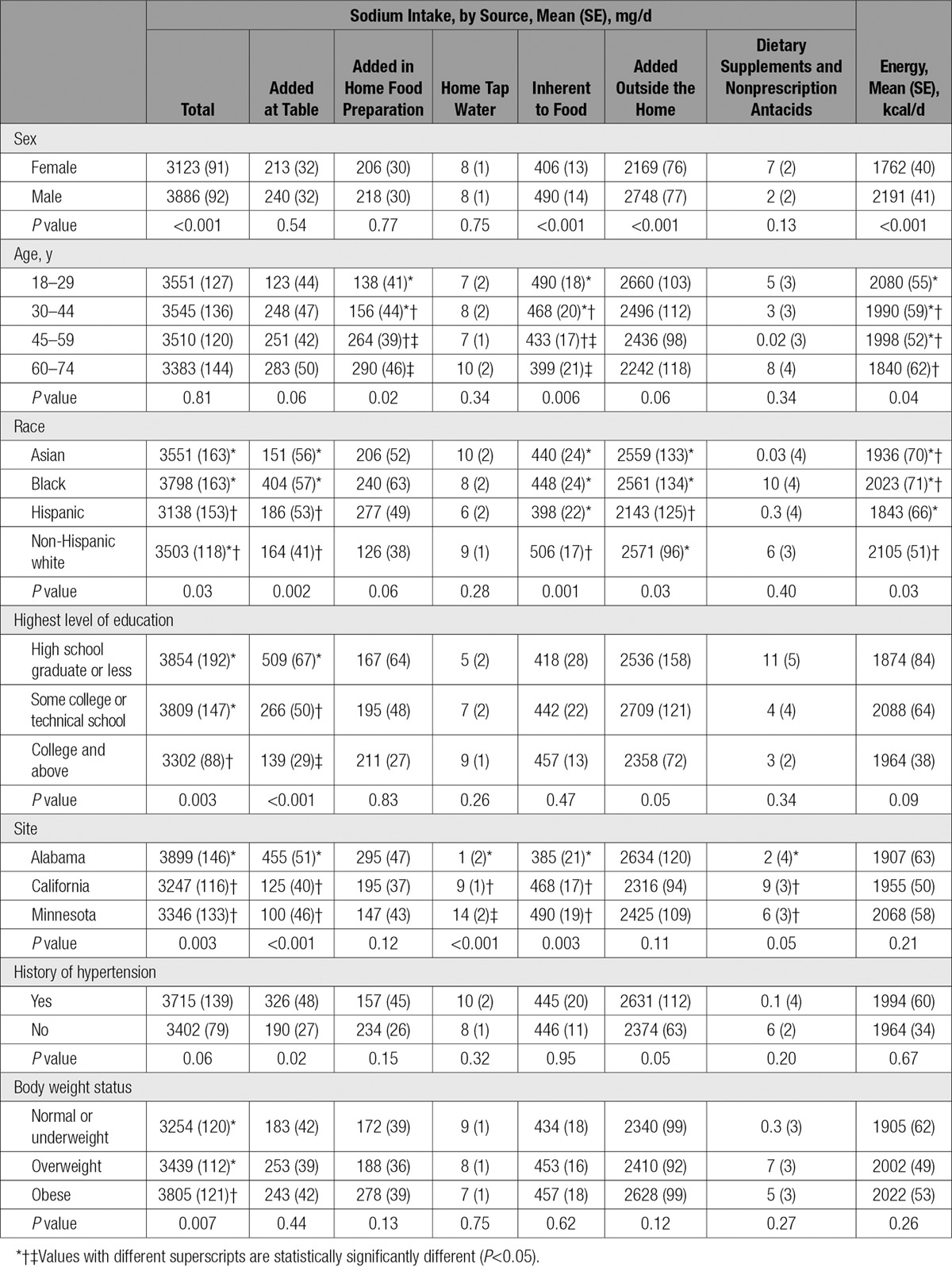
Mean total daily sodium intake in the sample was 3501 mg/d. Total sodium intake was similar across the age groups examined in multivariate-adjusted analyses (Table 2). There were differences in total sodium intake by sex (24% higher in men), race (higher in blacks and Asians compared with Hispanics), education level (17% higher in those with high school or lower level of education compared with college graduates), site (higher in Alabama compared with California and Minnesota), and body weight (17% higher in those who were obese compared with normal-weight participants).
Table 2.
Total Sodium Intake and Intake by Source by Demographic and Health Characteristics Adjusted for Sex, Age, Race, and Site (n=450)
The proportion of total sodium intake by source is presented in the Figure. For the total sample, sodium added to food outside the home (in commercial food processing, restaurant food preparation, etc) was the leading source of sodium, accounting for 70.9% of total sodium intake. Sodium inherent to food was the next highest contributor (14.2%), followed by salt added in home food preparation (5.6%) and salt added to food at the table (4.9%). Home tap water consumed as a beverage and dietary supplements and nonprescription antacids each contributed <0.5% to total sodium intake.
Figure.
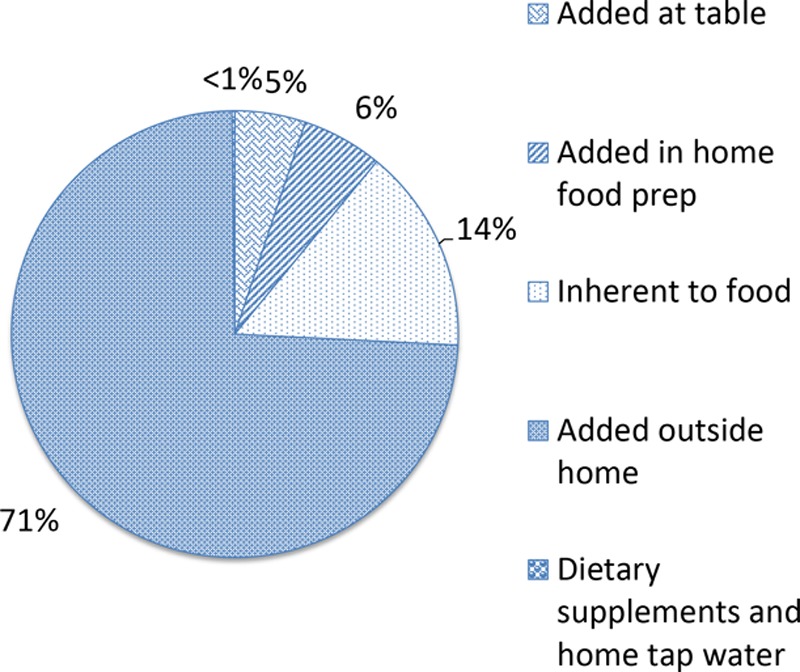
Proportion of total sodium intake from various sources (n=450).
Numerous differences in sources between demographic groups were found in multivariate-adjusted analyses (Table 3). However, for all groups, sodium added to food outside the home was the leading contributor to sodium intake (66.3%–75.0%); and sodium inherent to food, salt added in home food preparation, and salt added to food at the table were the next largest contributors. In all groups, sodium from home tap water and sodium from dietary supplements were minor contributors (<0.5% for most groups).
Table 3.
Proportion of Total Sodium Intake From Various Sources by Demographic and Health Characteristics Adjusted for Sex, Age, Race, and Site (n=450)
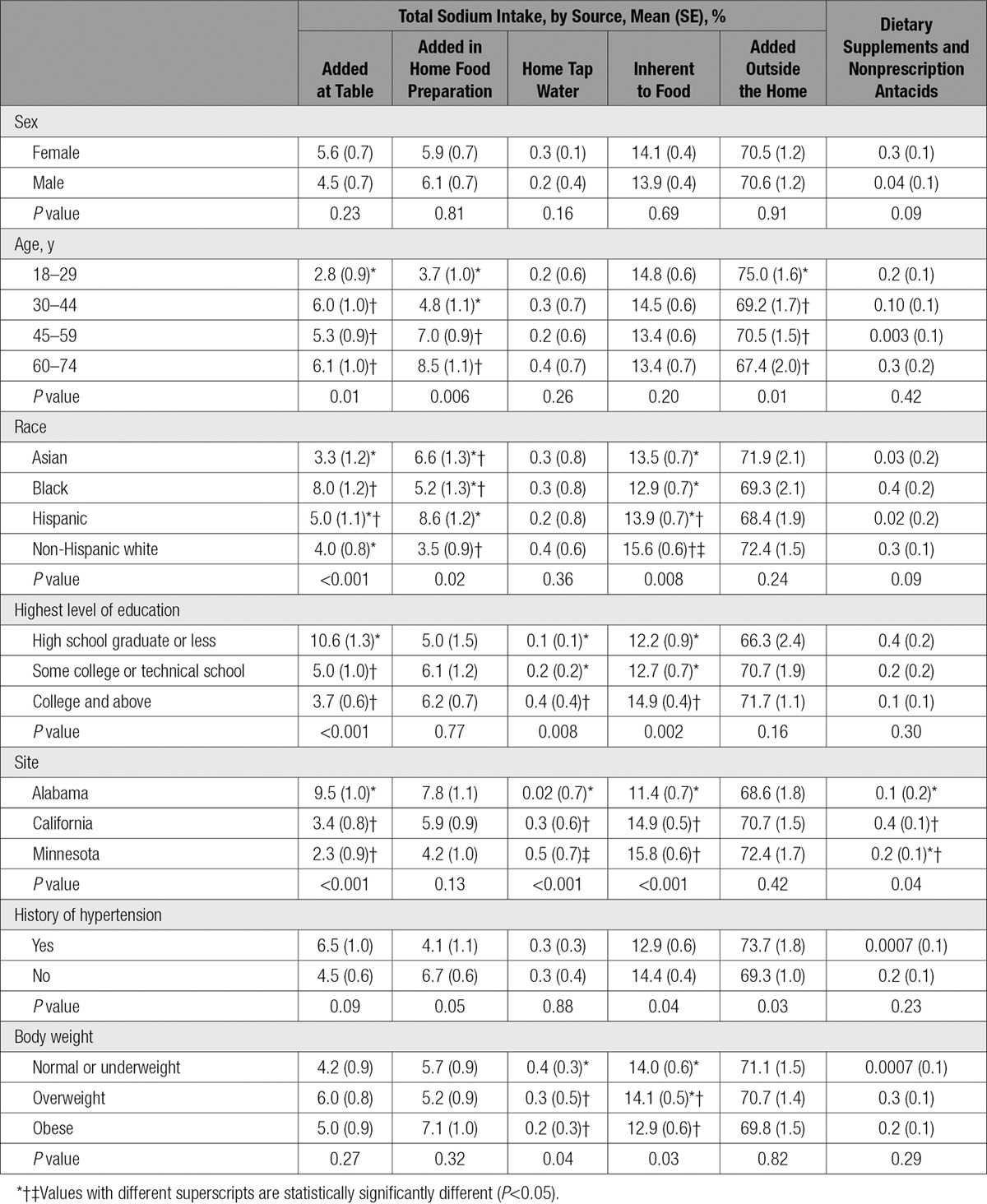
Sodium added to food outside the home was a higher proportion of total sodium intake among those 18 to 24 years of age (75.0%) compared with those in the older age groups (67.4%–70.5%). Conversely, salt added to food in home food preparation and salt added at the table were larger contributors to total sodium intake among older compared with younger participants.
Numerous differences in sodium sources by race were found. Asians and non-Hispanic whites obtained less sodium from salt added to food at the table (3.3% and 4.0%, respectively), whereas blacks obtained a greater share of sodium from this source (8.0%) compared with these groups. Non-Hispanic whites obtained less sodium from salt added to food in home preparation (3.5%) compared with Hispanics (8.6%).
Multiple differences in sources of sodium by education level were evident. Those with the lowest level of education obtained a higher proportion of sodium from salt added to food at the table compared with those with a higher level of education. In contrast, sodium inherent in food and sodium from home tap water made up smaller proportions of total sodium in those with a high school degrees or less education compared with those with a higher level of education.
A number of differences in sources of sodium by site were evident. Most notable is that participants in Alabama obtained a greater proportion of sodium from salt added to food at the table (9.5%) compared with participants in California (3.4%) and Minnesota (2.3%). Analyses were carried out to evaluate whether sources of sodium differed on weekdays and weekend days, and proportions were found to be similar for weekdays and weekend days.
Discussion
Sodium added to food outside the home was the leading source of sodium in this diverse sample, accounting for more than two-thirds (70.9%) of total sodium intake. Although this source of sodium was a smaller proportion of sodium intake in some subgroups, it was the leading contributor for all groups (range, 66.3%–75.0%). These findings are consistent with those of the Mattes and Donnelly8 study. In that study, which consisted of a sample of predominately female and white adults from 1 US geographic region (n=62), 77% of total sodium intake was attributable to sodium added to food outside the home. Like Mattes and Donnelly,8 we found sodium inherent to food, sodium from salt added to food at the table, sodium from salt added in home food preparation, and sodium from water consumed as a beverage to be notably smaller contributors than sodium added to food outside the home.
We found statistically significant differences in sources of sodium intake among demographic subgroups. In some cases, the differences observed were modest and may be of limited public health significance. In other cases, the differences were sizable and potentially worthy of consideration in the design of sodium reduction interventions. Most notable is that although sodium added to food outside the home accounted for the majority of intake, sodium from salt added to food at the table accounted for 9.5% of total sodium intake for those from the Alabama site (455 mg/d). If sodium from salt added to food at the table were reduced by 400 mg/d among study participants residing in Alabama, notable reductions in blood pressure and the incidence of coronary heart disease, myocardial infraction, and stroke might be expected according to projections of dietary sodium reductions reported by Bibbins-Domingo et al.12 Whether salt added at the table is a significant source of sodium intake among adults in Alabama, or potentially in other geographic areas, warrants further investigation.
Consistent with other studies involving samples of US adults,2,13–15 mean sodium intake in our sample (3501 mg/d) was well above the recommended intake level of 2300 mg/d.16 We found sodium intake to be higher among men compared with women, which is consistent with other findings.2,14,15 However, some specific findings of demographic differences in sodium intake were inconsistent with other findings. We found sodium intake to be higher among those with less education, which is inconsistent with other studies in which no difference14 or lower intake15 in those with less education was found. Sodium intake was notably higher among those from the Alabama site (3899 mg/d), whereas previous research has found sodium intake to be lower among those in southeastern compared with nonsoutheastern states.17,18 Blacks had a higher sodium intake in our sample, whereas other studies have found sodium intake of blacks to be lower than that of other groups.2,15,17,18
Study strengths include a larger sample size (n=450) than the previous study that identified sources of sodium in the diet of a sample of adults in the United States.8 In addition, the sample in our study had better representation with respect to race and geographic areas.
Study limitations include the use of a convenience rather than a probability-based sample, potentially limiting the generalizability of the results. The prevalences of hypertension (24%) and overweight/obesity (66%) in the study sample were similar to those in the US adult population (29.1% and 68.5% for hypertension and overweight/obesity, respectively19,20). However, the educational attainment distribution of the sample differed from the general population (the study sample included more college graduates). The process of completing multiple 24-hour dietary recalls and collecting duplicate samples of salt used at the table and in home food preparation could have led to changes in eating behavior and salt use (Hawthorne effect), although we have no way of assessing whether this may have occurred.
Our data suggest that sodium added to food outside the home accounts for the majority of sodium consumed by US adults. These findings support the primary Institute of Medicine–recommended strategy to reduce sodium intake in the United States through setting targets to reduce the sodium content of commercially processed and prepared foods.3 According to a recent report, 36 countries have set voluntary sodium targets for specific foods.21 In the United Kingdom, this approach resulted in an ≈15% (560 mg/d sodium, or 1.4 g/d salt) reduction in the average population sodium intake from 2003 to 2011 and was associated with significant decreases in blood pressure and cardiovascular disease deaths over the same time periods.22 Public education efforts should continue, with foods consumed outside the home (eg, restaurant and commercially processed foods) the primary focus of this education. Limiting salt added to food at the table and in home food preparation should also be recommended but framed as a secondary strategy that may be helpful when paired with efforts to limit sodium from restaurant and commercially processed foods.
Sources of Funding
Funding was provided through a research contract (Broad Agency Announcement) with the Centers for Disease Control and Prevention (contract 200–2012M-52155).
Disclosures
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, the National Institutes of Health, or the US Department of Health and Human Services.
Supplementary Material
Footnotes
The online-only Data Supplement, podcast, and transcript are available with this article at http://circ.ahajournals.org/lookup/suppl/doi:10.1161/CIRCULATIONAHA.116.024446/-/DC1.
Continuing medical education (CME) credit is available for this article. Go to http://cme.ahajournals.org to take the quiz
Circulation is available at http://circ.ahajournals.org.
Clinical Perspective
What Is New?
This study identifies the major sources of sodium in the diets of adults from 3 geographic regions in the United States.
The study shows that sodium added to food outside the home accounts for more than two thirds of total sodium intake, whereas sodium added to food at the table and in home food preparation is a minor contributor to total sodium intake.
Study findings align with a 2010 Institute of Medicine recommendation for reduction of sodium in commercially processed foods as the primary strategy to reduce sodium intake in the United States.
What Are the Clinical Implications?
Commercially processed and restaurant foods should be the primary focus when educating patients on strategies for lowering sodium in the diet.
For packaged food products, the Nutrition Facts panel may be useful in identifying lower-sodium products.
When individuals eat outside the home, sodium content information for menu items should be requested and used as a guide in making food choices.
Limiting salt added to food at the table and in home food preparation should also be encouraged, but patients should be advised that changes in these behaviors alone may not be sufficient for achieving the recommended intake level.
References
- 1.US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Americans, 1980. https://health.gov/dietaryguidelines/history.htm#6. Accessed January 31, 2017.
- 2.Jackson S, Coleman King S, Zhao L, Cogswell M. Prevalence of excess sodium intake in the United States: NHANES, 2009–2012. Morb Mortal Wkly Rep. 2016;64:1393–1397. doi: 10.15585/mmwr.mm6452a1. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine, Committee on Strategies to Reduce Sodium Intake. Strategies to Reduce Sodium Intake in the United States. Washington, DC: National Academies Press; 2010. [Google Scholar]
- 4.Maalouf J, Cogswell ME, Yuan K, Martin C, Gunn JP, Pehrsson P, Merritt P, Bowman B. Top sources of dietary sodium from birth to age 24 mo, United States, 2003–2010. Am J Clin Nutr. 2015;101:1021–1028. doi: 10.3945/ajcn.114.099770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Food categories contributing the most to sodium consumption: United States, 2007–2008. Morb Mortal Wkly Rep. 2012;61:92–98. [PubMed] [Google Scholar]
- 6.Subar AF, Krebs-Smith SM, Cook A, Kahle LL. Dietary sources of nutrients among US adults, 1989 to 1991. J Am Diet Assoc. 1998;98:537–547. doi: 10.1016/S0002-8223(98)00122-9. [DOI] [PubMed] [Google Scholar]
- 7.Block G, Dresser CM, Hartman AM, Carroll MD. Nutrient sources in the American diet: quantitative data from the NHANES II survey, I: vitamins and minerals. Am J Epidemiol. 1985;122:13–26. doi: 10.1093/oxfordjournals.aje.a114072. [DOI] [PubMed] [Google Scholar]
- 8.Mattes RD, Donnelly D. Relative contributions of dietary sodium sources. J Am Coll Nutr. 1991;10:383–393. doi: 10.1080/07315724.1991.10718167. [DOI] [PubMed] [Google Scholar]
- 9.Feskanich D, Sielaff BH, Chong K, Buzzard IM. Computerized collection and analysis of dietary intake information. Comput Methods Programs Biomed. 1989;30:47–57. doi: 10.1016/0169-2607(89)90122-3. [DOI] [PubMed] [Google Scholar]
- 10.Harnack L, Stevens M, Van Heel N, Schakel S, Dwyer JT, Himes J. A computer-based approach for assessing dietary supplement use in conjunction with dietary recalls. J Food Compost Anal. 2008;21(suppl)(1):S78–S82. doi: 10.1016/j.jfca.2007.05.004. doi: 10.1016/j.jfca.2007.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Krebs-Smith SM, Kott PS, Guenther PM. Mean proportion and population proportion: two answers to the same question? J Am Diet Assoc. 1989;89:671–676. [PubMed] [Google Scholar]
- 12.Bibbins-Domingo K, Chertow GM, Coxson PG, Moran A, Lightwood JM, Pletcher MJ, Goldman L. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362:590–599. doi: 10.1056/NEJMoa0907355. doi: 10.1056/NEJMoa0907355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carriquiry A, Moshfegh A, Steinfeldt L, Cogswell M, Loustdot F, Zhang Z, Yang Q, Tian N. Trends in the prevalence of excess dietary sodium intake: United States, 2003–2010. Morb Mortal Wkly Rep. 2013;2:1021–1025. [Google Scholar]
- 14.Meyer KA, Harnack LJ, Luepker RV, Zhou X, Jacobs DR, Steffen LM. Twenty-two-year population trends in sodium and potassium consumption: the Minnesota Heart Survey. J Am Heart Assoc. 2013;2:e000478. doi: 10.1161/JAHA.113.000478. doi: 10.1161/JAHA.113.000478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cogswell ME, Zhang Z, Carriquiry AL, Gunn J, Kuklina E, Saydah S, Yang Q, Moshfegh A. Sodium and potassium intakes among US adults: NHANES 2003–2008. Am J Clin Nutr. 2012;96:647–657. doi: 10.3945/ajcn.112.034413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Americans 2015–2020. https://health.gov/dietaryguidelines/2015/guidelines/. Accessed January 31, 2017.
- 17.Newby PK, Noel SE, Grant R, Judd S, Shikany JM, Ard J. Race and region are associated with nutrient intakes among black and white men in the United States. J Nutr. 2011;141:296–303. doi: 10.3945/jn.110.130583. doi: 10.3945/jn.110.130583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newby PK, Noel SE, Grant R, Judd S, Shikany JM, Ard J. Race and region have independent and synergistic effects on dietary intakes in black and white women. Nutr J. 2012;11:25. doi: 10.1186/1475-2891-11-25. doi: 10.1186/1475-2891-11-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nwankwo T, Yoon S, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011–2012. NCHS Data Brief. 2013;133:1–8. [PubMed] [Google Scholar]
- 20.Ogden C, Carroll M, Kit B, Glegal K. Prevalence of childhood and adult obesity in the United States, 2011–2012. J Am Med Assoc. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trieu K, Neal B, Hawkes C, Dunford E, Campbell N, Rodriguez-Fernandez R, Legetic B, McLaren L, Barberio A, Webster J. Salt reduction initiatives around the world: a systematic review of progress towards the global target. PLoS One. 2015;10:e0130247. doi: 10.1371/journal.pone.0130247. doi: 10.1371/journal.pone.0130247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.He FJ, Pombo-Rodrigues S, Macgregor GA. Salt reduction in England from 2003 to 2011: its relationship to blood pressure, stroke and ischaemic heart disease mortality. BMJ Open. 2014;4:e004549. doi: 10.1136/bmjopen-2013-004549. [DOI] [PMC free article] [PubMed] [Google Scholar]


