Abstract
Purpose
To evaluate adherence to disease-modifying therapies (DMTs) among patients with multiple sclerosis (MS) initiating oral and injectable DMTs, and to estimate the impact of adherence on relapse, health resource utilization, and medical costs.
Patients and methods
Commercially insured MS patients (aged 18–65 years, two or more MS diagnoses, one or more DMT claims) with continuous eligibility 12 months before and after the first DMT claim date (index date) and no DMT claim during the pre-index period were identified from a large commerical claims database for the period from January 1, 2008, to September 30, 2015. Adherence to the index DMT was measured by the 12-month post-index proportion of days covered (PDC) and compared between oral and injectable DMT initiators. After adjustment for sex, age at index DMT, and comorbidities, regression models examined the relationship between adherence and relapse risk, MS-related health resource utilization, and non-drug medical costs (2015 US$).
Results
The study covered 12,431 patients and nine DMTs. Adherence to the index DMT did not differ significantly between oral (n=1,018) and injectable (n=11,413) DMTs when assessed by mean PDC (0.7257±0.2934 vs 0.7259±0.2869, respectively; P=0.0787), or percentages achieving PDC ≥0.8 (61.4% vs 58.6%, respectively; P=0.0806). Compared to non-adherence, adherence to DMT significantly reduced the likelihood of relapse in the post-index 12 months by 42%, hospitalization by 52%, and emergency visits by 38% (all, P<0.0001). Adherent patients would be expected to have on average 0.7 fewer outpatient visits annually versus non-adherent patients (P<0.0001). Based on the differences in predicted mean costs, adherence (vs non-adherence) would decrease the total annual medical care costs by $5,816 per patient, including hospitalization costs by $1,953, emergency visits by $171, and outpatient visits by $2,802.
Conclusion
Adherence remains suboptimal but comparable between oral and injectable DMTs. Potential health and economic benefits underscore the importance of improving adherence in MS.
Keywords: MS, DMT prescribing patterns, implications
Introduction
Multiple sclerosis (MS) is a chronic autoimmune degenerative disorder of the central nervous system afflicting between 400,000 and 570,000 people in the US and 2.5 million individuals worldwide.1,2 Relapsing remitting MS (RRMS), the most common subtype diagnosed in 85%–90% of patients, is characterized by discrete but debilitating bouts of neurologic dysfunction (relapses) followed by periods of remission and recovery.3 Relapse symptoms vary by patient and extent of neurologic involvement, but frequently include fatigue, sensory disturbances, visual impairment, ataxia, and bladder and bowel dysfunction.3,4 On an individual level, the disease course of RRMS is variable and highly unpredictable;5 however, within one to three decades following onset, ~60%–70% of patients advance to a secondary progressive phase MS (SPMS), marked by insidious worsening and accumulation of neurologic and cognitive dysfunction.5–7 Ultimately, patients can suffer increasingly progressive disability and premature death.8 MS is the leading cause of atraumatic disability in young and middle-aged persons in the developed world, as the disease most often manifests between the ages of 20 and 50 years, the prime years for work productivity.8
MS remains incurable; however, clinical studies have demonstrated that disease-modifying therapies (DMTs) currently approved for RRMS can reduce the rates of relapse compared to placebo, decrease the accumulation of lesion burden on magnetic resonance imaging, and slow the progression of disability.5,9–13 DMTs vary by efficacy, route of administration, mechanisms of action, dosing schedule, tolerability, and safety profile.13 While efficacy and safety may vary considerably among products and patients,14 the unifying treatment goal is to reduce the clinical and subclinical disease activity thought to contribute to long-term disability,15–17 thus underscoring the importance of early treatment.14 Attaining therapeutic benefit, however, necessitates strict adherence to both the prescribed DMT dose and the administration schedule. However, studies assessing real-world DMT-usage patterns in MS suggest that adherence is suboptimal. When examined over 1–5 years after commencing treatment, ~25%–40% of injectable DMT initiators and nearly 30% of oral DMT initiators had discontinued treatment or fulfilled the study criteria for non-adherence.4,8,18–21
When first introduced into the market, oral DMTs were perceived to improve adherence, but few studies have compared adherence between oral DMTs and injectable DMTs. Two retrospective analyses of short-term claims data in the US observed that patients initiating an oral DMT (fingolimod) were more adherent and significantly less likely to discontinue treatment than those initiating injectable DMTs.18,19 In Agashivala et al (n=1,891), the proportion of days covered (PDC) for fingolimod initiators (mean ± standard deviation 0.8±0.23) was significantly higher than for initiators of self-injectable DMTs, including IFNβ-1b (0.65±0.31, P<0.0001), IFNβ-1a intramuscularly (0.72±0.3, P=0.0027), IFNβ-1a subcutaneously (0.67±0.31, P<0.0001), and glatiramer acetate (0.72±0.29, P=0.0017).18 Bergvall et al (n=3,750) found that the risk of non-adherence was increased by 2.3-fold in glatiramer acetate initiators (P<0.0001), 2.1-fold in IFN initiators (P<0.0001), and 1.9-fold in natalizumab initiators (P=0.0103) compared to fingolimod initiators.19 These studies, however, were conducted shortly after fingolimod was approved in the US, and warrant further assessment with additional data if available. A third US claims analysis, by Munsell et al, examined prescribing patterns for three oral (total n=444) and five self-injectable DMTs (total n=5,238), and found that the route of administration was not a significant predictor of non-adherence.22 Given the limited, equivocal evidence, the difference in adherence between oral and injectable DMT initiators remains unclear.
While there is a need to re-examine the adherence patterns for different DMTs, it is equally important to investigate the relationship between adherence and outcomes. Many studies have affirmed the association between adherence to DMT and beneficial outcomes, such as a reduced risk for relapse,4,21,23,24 decreased rates of MS-related hospitalizations and emergency room (ER) visits,4,21 improvements in quality of life and cognition,25 and slowing of disability progression, as measured by the Expanded Disability Status Scale (EDSS).26 Despite the evidence, however, most studies have failed to examine both health and economic outcomes in the context of a broad range of DMTs. Tan et al (n=2,446) retrospectively assessed MS-related medical costs and the risks of relapse and hospitalization for 2004–2008, but the analysis is outdated and included only four injectable DMTs.4
To provide a more contemporary, comprehensive perspective, we retrospectively analyzed claims data for MS patients who initiated DMTs in the US during 2008–2015, and investigated the implications of adherence on the risk of MS relapse and both MS-related health resource utilization (HRU) and non-drug medical costs. The aim was to determine whether given the current DMT options, adherence patterns differed between patients initiating oral and injectable DMTs, and to assess both the clinical and economic consequences of real-world adherence in this population.
Patients and methods
Data source
This study utilized commercial claims data from the MarketScan® (Truven Health Analytics) Commercial Claims Database for the period between January 1, 2008 and September, 2015. The MarketScan® database consists of fully adjudicated and paid claims, with integrated enrollment, inpatient, outpatient, and prescription data for a nationally representative sample of ~174 million (since 1995) unique, de-identified individuals insured by employer-sponsored plans. Individuals include active employees, early retirees, Consolidated Omnibus Budget Reconciliation Act continuers, and their dependents. The database is fully compliant with the 1996 Health Insurance Portability and Accountability Act privacy regulations, and provides anonymized patient-level data. No data used in the analyses contained any patient identifiers; therefore, institutional review board approval and patient-informed consent were not required.
Sample selection and DMTs included in analyses
Patients were eligible if they: 1) had two or more distinct claims with a corresponding MS diagnosis (International Classification of Diseases, ninth revision, clinical modification [ICD-9-CM] code 340.xx); 2) were between ages 18 and 65 years at diagnosis; 3) had one or more claims for a DMT following the MS diagnosis; and 4) had no MS DMT claims during the 365 days preceding the date of the first DMT claim. The “index DMT” represented the first DMT claim, and the “index date” signified the date of the index DMT. Eligible patients enrolled continuously for a minimum of 12 months preceding (pre-index) and following the index (post-index) date were included. DMTs included oral and injectable (self-injectable and infusible) products licensed for MS in the US and for which sufficient pharmacy claim data were available. DMTs were identified using pharmacy claims that included the prescription-fill date, National Drug Code, and days of drug supply.
Patient characteristics
Baseline patient characteristics, including age, sex, and comorbidities, were abstracted from the claims data. Comorbidities were reported using the Charlson Comorbidity Index (CCI). The CCI was originally developed to predict the 1-year mortality risk attributable to comorbidity in general hospitalized patients,27 and was subsequently adapted so that ICD-9-CM codes could be used to calculate the CCI with existing administrative data.28 The CCI represents the summary score derived from conditions comprising 19 comorbidity categories. Each condition is weighted 1–6 depending on mortality risk and disease severity, and then summed to calculate the CCI. Higher CCI scores indicate greater comorbidity.29
Key outcomes
Definitions of DMT adherence, discontinuation, and switch
Adherence was measured using the PDC, which represented the proportion of days during the 12-month post-index period that a patient was on the index DMT. The PDC provides a more conservative estimate than the fixed-interval medication possession ratio (MPR), and overlapping fills were counted only once.19,30 Treatment discontinuation was signified by a gap ≥90 days between the end of the index DMT claim and the next DMT claim with no other DMT claim recorded during the 90-day period. A switch was indicated by evidence of another DMT claim within the 90-day gap.
MS relapse rates
MS relapse rates were measured during the 12-month post-index period. A relapse was identified as: 1) an inpatient MS-related claim with MS as the primary diagnosis post-index date or 2) an outpatient MS-related diagnosis code and a prescription claim for a corticosteroid (dexamethasone, methylprednisolone, prednisolone, prednisone, or adrenocorticotropic hormone) ≤7 days following the outpatient visit.31 Relapses recorded within the same 30-day period were classified as a single event.
HRU and costs
MS-related HRU (hospitalizations, ER visits, and outpatient visits) and direct medical costs (total medical, hospitalization, ER, and outpatient costs) were assessed during the 12-month post-index period using medical claims with a corresponding ICD-9-CM diagnosis of MS. Direct medical costs were calculated based on the reimbursed amounts paid to health care providers for ER visits, inpatient or outpatient visits, and hospitalization. As the present study focused primarily on the economic outcomes of DMT adherence in terms of MS-related HRU and the associated medical costs, drug costs, including expenditure on DMTs, were excluded from the total medical cost calculations. This approach is consistent with methods reported in prior studies of DMT adherence in MS.32 All costs are reported in 2015 US$.
Statistical analysis
Categorical data are summarized descriptively as counts and proportions. Continuous data are expressed as the mean ± standard deviation. Baseline demographic and clinical patient characteristics, rates of DMT adherence, discontinuation, and switching were compared between oral and injectable DMT initiators using χ2 or Wilcoxon rank-sum test for categorical and continuous variables, respectively.
In the regression analyses, adherence was modeled as a binary variable, with PDC ≥0.8 representing adherence and PDC <0.8 indicating non-adherence. Explanatory variables (covariates) were selected a priori based on clinical relevance, and depending on the analysis, included sex, age at index date (continuous variable), route of administration (oral or injectable), CCI score (0, 1, 2, or ≥3), and adherence (PDC ≥0.8, PDC <0.8). Separate logistic regression models were used to analyze each of the following: 1) the impact of route of administration (oral or injectable) on adherence to the index DMT; 2) the impact of adherence on likelihood of MS relapse; and 3) the impact of adherence on MS-related HRU (hospitalizations and ER visits). Ordinary least-squares (OLS) regression was performed to evaluate the association between adherence and the number of MS-related outpatient visits. Generalized linear models (GLMs) were applied to examine the relationship between adherence and health care costs (hospitalization, ER, outpatient, and total medical costs). Predicted mean costs for adherent and non-adherent patients were generated based on the regression coefficients. Measures of association were expressed as adjusted odds ratio (OR) and 95% confidence interval (CI) in logistic regression analyses, estimated β-coefficient and standard error in the OLS regression, and maximum-likelihood estimate and standard error in the GLM regression. A two-tailed P-value <0.05 was statistically significant. All statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC, USA).
Results
Baseline characteristics
A total of 12,431 patients met the study criteria (Figure 1), and nine DMTs (three oral, five self-injectable, and one infusible) (Table 1) were included. Of the 12,431 patients, 11,413 (91.8%) had initiated an injectable DMT (Table 2). For the purpose of the analysis, patients initiating self-injectable DMTs (n=11,315) and those prescribed the infusible DMT natalizumab (n=98) were combined and comprised the cohort of injectable DMT initiators. Women comprised over three-quarters (76.2%) of the total sample. Comorbidity was significantly greater among oral DMT initiators, as indicated by mean CCI scores (1.42±1.58 for oral DMT initiators vs 1.14±1.53 for injectable DMT initiators, P<0.0001) and higher proportion of oral DMT initiators with CCI scores >0 (74.9% vs 61.4% of injectable DMT initiators, P<0.0001). Among the injectable DMT initiators (n=11,413), 45.8% were prescribed glatiramer acetate, 22.4% IFNβ-1a intramuscularly, 20.1% IFNβ-1a subcutaneously, 10.5% IFNβ-1b, and 0.9% natalizumab. Among the oral DMT initiators (n=1,018), dimethyl fumarate was prescribed in 58.4%, fingolimod in 31.7%, and teriflunomide in 9.8%.
Figure 1.
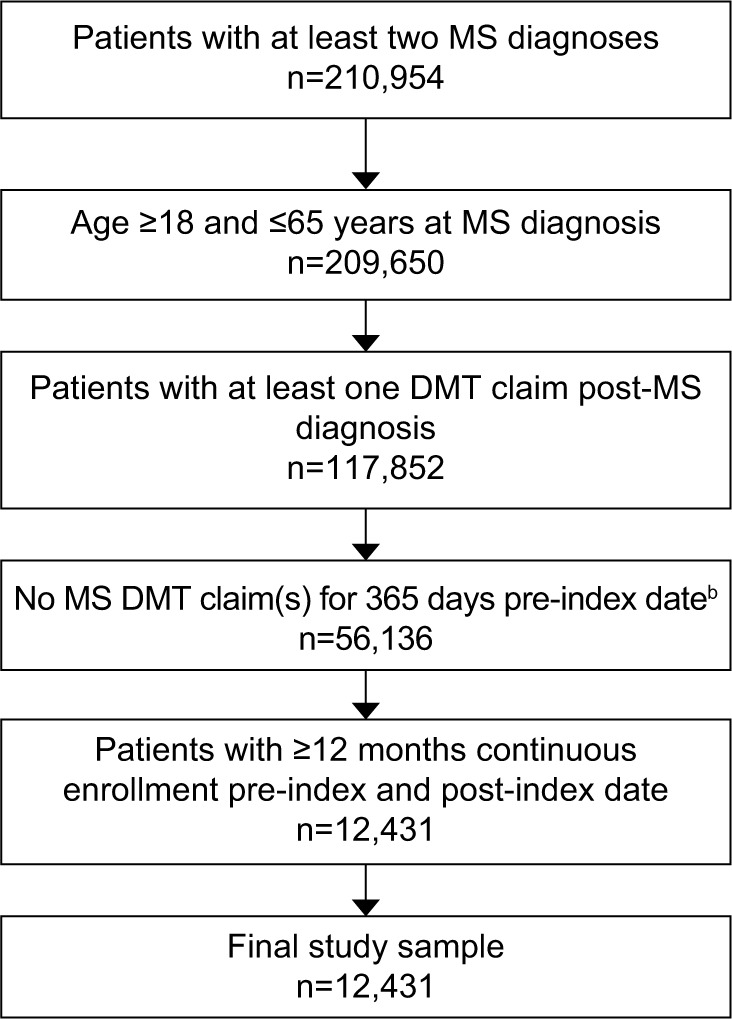
Attrition and inclusion of the study sample.a
Notes: aStudy period January 1, 2008, to September 30, 2015; bindex date defined as date of first DMT claim.
Abbreviations: DMT, disease-modifying therapy; MS, multiple sclerosis.
Table 1.
DMTs for MS included in the retrospective claims database analysisa
| Route | DMT | Manufacturer | Dosing frequency | Approval year (US) |
|---|---|---|---|---|
| Injectable | Avonex® (IFNβ-1a) | Biogen | Once weekly | 1996 |
| Betaseron® (IFNβ-1b) | Bayer Healthcare Pharmaceuticals | Every other day | 1993 | |
| Copaxone® (glatiramer acetate 20/40 mg) | Teva Pharmaceuticals | Daily/3 times weekly | 1996/2014 | |
| Extavia® (IFNβ-1b) | Novartis Pharmaceuticals | Every other day | 2009 | |
| Rebif® (IFNβ-1a) | EMD Serono | 3 times weekly | 2002 | |
| Tysabri® (natalizumab) | Biogen | Once every 4 weeks | 2004 | |
| Oral | Aubagio® (teriflunomide) | Genzyme | Once daily | 2012 |
| Gilenya® (fingolimod) | Novartis Pharmaceuticals | Once daily | 2010 | |
| Tecfidera® (dimethyl fumarate) | Biogen | Twice daily | 2013 |
Note:
More recently approved DMTs – including Zinbryta® (daclizumab), once-weekly injectable; Glatopa® (glatiramer acetate 20 mg), once-daily injectable; Lemtrada® (alemtuzumab) daily infusion on five consecutive days the first year and on three consecutive days one year apart from first year and PLEGRIDY® (PEG-IFNβ-1a), injectable every 14 days – were not included, due to insufficient claims data at the end of the study period (September 30, 2015).
Abbreviations: DMTs, disease-modifying therapies; MS, multiple sclerosis.
Table 2.
Baseline demographic and clinical characteristics of study sample (n=12,431)
| Variables | Total sample (n=12,431) | Injectable (n=11,413) | Oral (n=1,018) | P-value* |
|---|---|---|---|---|
| Age at index date, years, mean (SD) | 44.55 (10.36) | 44.56 (10.35) | 44.41 (10.52) | 0.3877 |
| Age group, years, n (%) | ||||
| 18–24 | 414 (3.33) | 370 (3.24) | 44 (4.32) | 0.3791 |
| 25–34 | 1,864 (14.99) | 1,720 (15.07) | 144 (14.15) | |
| 35–44 | 3,704 (29.8) | 3,393 (29.73) | 311 (30.55) | |
| 45–54 | 4,036 (32.47) | 3,710 (32.51) | 326 (32.02) | |
| 55–64 | 2,413 (19.41) | 2,220 (19.45) | 193 (18.96) | |
| Sex, n (%) | ||||
| Female | 9,478 (76.24) | 8,744 (76.61) | 734 (72.1) | 0.0012 |
| Male | 2,953 (23.76) | 2,669 (23.39) | 284 (27.9) | |
| CCI score, mean (SD) | 1.17 (1.53) | 1.14 (1.53) | 1.42 (1.58) | <0.0001 |
| CCI score, n (%) | ||||
| 0 | 4,667 (37.54) | 4,411 (38.65) | 256 (25.15) | <0.0001 |
| 1 | 4,848 (39) | 4,392 (38.48) | 456 (44.79) | |
| 2 | 1,244 (10.01) | 1,110 (9.73) | 134 (13.16) | |
| ≥3 | 1,672 (13.45) | 1,500 (13.14) | 172 (16.9) |
Note:
Statistically significant (P<0.05) differences between injectable and oral DMT cohorts determined by χ2 test for categorical variables and Wilcoxon rank-sum test for continuous variables.
Abbreviations: CCI, Charlson Comorbidity Index; SD, standard deviation; DMT, disease-modifying therapy.
Comparison of adherence to index DMT between oral and injectable initiators
The mean PDC was nearly identical between oral DMT initiators (0.7257±0.2934) and injectable DMT initiators (0.7259±0.2869) (Table 3). The proportions of patients with PDC ≥0.8 were also similar, although distribution among the PDC categories differed significantly (P<0.001) (Table 3). During the 12-month post-index period, 68.1% (7,768 of 11,413) of injectable DMT initiators and 71.2% (725 of 1,018) of oral DMT initiators had not switched or discontinued the index DMT. Injectable DMT initiators spent significantly more days on therapy than oral DMT initiators before discontinuing therapy (mean 123.7±75.6 days vs 110.3±78.8 days, respectively; P=0.0039) or switching (mean 166±101.8 days vs 122.8±96.8 days, respectively; P<0.0001).
Table 3.
Differences in adherence, discontinuation, and switches between patients with MS initiating oral and injectable DMTs in the US
| Variables | Injectable (n=11,413) | Oral (n=1,018) | P-value* |
|---|---|---|---|
| PDC, mean (SD) | 0.7259 (0.2869) | 0.7257 (0.2934) | 0.0787 |
| PDC group, n (%) | |||
| <0.2 | 864 (7.57) | 112 (11) | <0.0001 |
| 0.2–<0.4 | 1,227 (10.75) | 80 (7.86) | |
| 0.4–<0.6 | 1,147 (10.05) | 69 (6.78) | |
| 0.6–<0.8 | 1,489 (13.05) | 132 (12.97) | |
| ≥0.8 | 6,686 (58.58) | 625 (61.39) | |
| PDC category, n (%) | |||
| <0.8 (non-adherent) | 4,727 (41.42) | 393 (38.61) | 0.0806 |
| ≥0.8 (adherent) | 6,686 (58.58) | 625 (61.39) | |
| DMT discontinuation | |||
| n (%) | 2,089 (18.3) | 172 (16.9) | 0.2645 |
| Days on therapy, mean (SD) | 123.69 (75.61) | 110.30 (78.85) | 0.0039 |
| DMT switch | |||
| n (%) | 1,156 (13.63) | 121 (11.89) | 0.1178 |
| Days on therapy, mean (SD) | 166.00 (101.77) | 122.80 (96.77) | <0.0001 |
Note:
Statistically significant (P<0.05) difference determined by χ2 test for categorical variables and Wilcoxon rank-sum test for continuous variables.
Abbreviations: MS, multiple sclerosis; DMTs, disease-modifying therapies; PDC, proportion of days covered; SD, standard deviation.
After controlling for age, sex, and CCI score, the logistic regression showed no significant difference between oral and injectable DMT initiators with respect to the odds of adherence to the index DMT (Table 4). In contrast, males and patients with a CCI score of 1 (vs CCI=0) were significantly more likely to adhere to the index DMT (both P<0.0001). The odds of adherence were also significantly elevated with each advancing year of age at the index date (OR =1.015, 95% CI: 1.001–1.018; P<0.0001).
Table 4.
Logistic regression analysis: predictors of adherence to index DMT (PDC ≥0.8)
| Covariates | OR (95% CI) | P-value* |
|---|---|---|
| Injectable DMT | Reference | |
| Oral DMT | 0.901 (0.789–1.029) | 0.1254 |
| Sex | ||
| Male | Reference | |
| Female | 0.755 (0.693–0.822) | <0.0001 |
| Age at index DMT | 1.015 (1.011–1.018) | <0.0001 |
| CCI score | ||
| 0 | Reference | |
| 1 | 1.095 (1.009–1.189) | 0.0305 |
| 2 | 0.908 (0.8–1.031) | 0.1369 |
| ≥3 | 1.059 (0.944–1.189) | 0.3252 |
Note:
Statistically significant difference defined as P<0.05.
Abbreviations: DMT, disease-modifying therapy; PDC, proportion of days covered; OR, odds ratio; CI, confidence interval; CCI, Charlson Comorbidity Index.
Predictors of MS relapse
During the 12-month post-index period, 19.3% (2,395 of 12,431) of the study sample had relapsed. After controlling for sex, age at index DMT, and CCI, patients who were adherent to the index DMT were ~42% less likely to relapse than patients who were non-adherent (OR=0.576, 95% CI: 0.526–0.63; P<0.0001) (Table 5). Individuals of younger age were more likely to relapse, with the odds decreased by 0.6% with each incremental year (OR=0.994, 95% CI: 0.99–0.999; P=0.0129). Compared to patients with no comorbidity (CCI=0), the risk of relapse was also significantly increased in those with concomitant conditions (CCI=1, OR=1.351, 95% CI: 1.215–1.501; CCI=2, OR=1.524; 95% CI: 1.305–1.78; and CCI=3, OR=1.585; 95% CI: 1.378–1.824; all P<0.0001).
Table 5.
Logistic regression analysis: predictors of MS relapse
| Covariates | OR (95% CI) | P-value* |
|---|---|---|
| Sex | ||
| Male | Reference | |
| Female | 1.06 (0.952–1.18) | 0.2884 |
| Age at index DMT | 0.994 (0.99–0.999) | 0.0129 |
| CCI score 0 | ||
| 0 | Reference | |
| 1 | 1.351 (1.215–1.51) | <0.0001 |
| 2 | 1.524 (1.305–1.78) | <0.0001 |
| ≥3 | 1.585 (1.378–1.824) | <0.0001 |
| PDC group | ||
| <0.8 | Reference | |
| ≥0.8 | 0.576 (0.526–0.63) | <0.0001 |
Note:
Statistically significant difference defined as P<0.05
Abbreviations: MS, multiple sclerosis; OR, odds ratio; CI, confidence interval; DMT, disease-modifying therapy; CCI, Charlson Comorbidity Index; PDC, proportion of days covered.
Adherence (PDC ≥0.8) as a predictor of MS-related HRU and non-drug medical costs
During the 12-month post-index period, 7.6% (947 of 12,431) of patients had been hospitalized, and 17.9% (2,228 of 12,431) had sought emergent treatment. Patients had on average 5.6 outpatient visits. After controlling for sex, age at index DMT, and CCI score, patients adherent to the index DMT were ~52% less likely to have been hospitalized and 38% less likely to have visited an ER than non-adherent patients (both P<0.0001). In the OLS regression, adherence to the index DMT would be expected to result in an average of 0.7 fewer outpatient visits per patient (P<0.0001) over the 12-month post-index period (Table 6).
Table 6.
Predictors of MS-related hospital visits, ER visits, and outpatient visits in patients with MS treated with DMTs (n=12,431)
| Variables | Hospital visitsa | P-value | ER visitsa | P-value | Outpatient visitsb | P-value |
|---|---|---|---|---|---|---|
| Sex | ||||||
| Female | Reference | Reference | Reference | |||
| Male | 0.939 (0.799–1.104) | 0.4478 | 0.826 (0.737–0.925) | 0.0009 | –0.019 (0.152) | 0.901 |
| Age at index DMT | 1.029 (1.022–1.036) | <0.0001 | 0.992 (0.988–0.997) | 0.0009 | 0.01 (0.006) | 0.110 |
| CCI score | ||||||
| 0 | Reference | Reference | Reference | |||
| 1 | 1.239 (1.053–1.457) | 0.0097 | 1.457 (1.304–1.628) | <0.0001 | 1.035 (0.148) | <0.0001 |
| 2 | 1.767 (1.421–2.198) | <0.0001 | 1.81 (1.545–2.12) | <0.0001 | 0.94 (0.229) | <0.0001 |
| ≥3 | 1.678 (1.374–2.048) | <0.0001 | 2.052 (1.782–2.364) | <0.0001 | 1.724 (0.206) | <0.0001 |
| PDC group | ||||||
| <0.8 | Reference | Reference | Reference | |||
| ≥0.8 | 0.478 (0.417–0.547) | <0.0001 | 0.62 (0.565–0.681) | <0.0001 | –0.712 (0.132) | <0.0001 |
Notes:
Values represent point estimates for the OR (95% CI) generated by logistic regression;
values represent coefficient estimates (SE) generated by ordinal least-squares regression.
Abbreviations: MS, multiple sclerosis; ER, emergency room; DMTs, disease-modifying therapies; CCI, Charlson Comorbidity Index; PDC, proportion of days covered; OR, odds ratio; CI, confidence interval; SE, standard error.
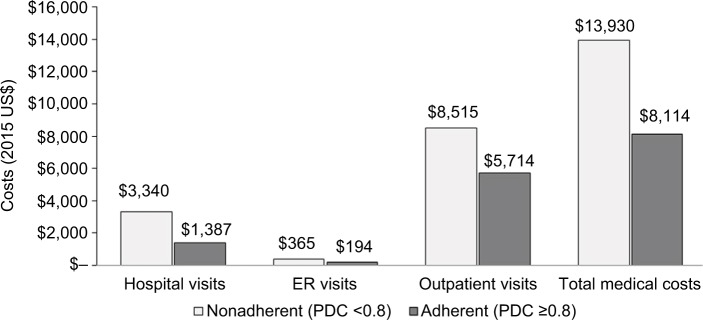
In the GLMs adjusted for sex, age at index DMT, and CCI score, adherence to the index DMT was significantly associated with reductions in total medical costs, including costs for hospitalizations, ER visits, and outpatient visits (all P<0.0001) (Table 7). Comparing the predicted mean costs for the 12 months following initiation of DMT, adherence would be expected to reduce the total medical (non-drug) costs per patient by $5,815.47 (−41.7%), hospitalization cost by $1,953.01 (−58.5%), ER cost by $171.40 (−46.9%), and outpatient admission cost by $2,801.63 (−32.9%) (Figure 2).
Table 7.
Generalized linear regression analysis: predictors of non-drug medical costs in patients with MS on DMT (total n=12,431)a
| Variables | Hospitalization costs
|
ER costs
|
Outpatient visit costs
|
Total medical costs
|
||||
|---|---|---|---|---|---|---|---|---|
| Parameter | P-value | Parameter | P-value | Parameter | P-value | Parameter | P-value | |
| Sex (male) | −0.081 (0.062) | NS | −0.222 (0.051) | <0.0001 | −0.074 (0.036) | 0.038 | −0.083 (0.037) | 0.025 |
| Age at index DMT | 0.043 (0.002) | <0.0001 | −0.008 (0.002) | <0.0001 | 0.009 (0.002) | <0.0001 | 0.015 (0.002) | <0.0001 |
| CCI score | ||||||||
| 1 | 0.496 (0.06) | <0.0001 | 0.423 (0.049) | <0.0001 | 0.350 (0.035) | <0.0001 | 0.373 (0.036) | <0.0001 |
| 2 | 0.573 (0.095) | <0.0001 | 0.651 (0.077) | <0.0001 | 0.396 (0.054) | <0.0001 | 0.442 (0.056) | <0.0001 |
| ≥3 | 1.012 (0.083) | <0.0001 | 0.69 (0.069) | <0.0001 | 0.59 (0.048) | <0.0001 | 0.663 (0.05) | <0.0001 |
| PDC group (≥0.8) | −0.942 (0.054) | <0.0001 | −0.616 (0.044) | <0.0001 | −0.415 (0.031) | <0.0001 | −0.564 (0.032) | <0.0001 |
Note:
Parameter values for generalized linear regression analyses represent maximum-likelihood estimates (SE).
Abbreviations: MS, multiple sclerosis; DMT, disease-modifying therapy; ER, emergency room; NS, not significant; CCI, Charlson Comorbidity Index; PDC, proportion of days covered; SE, standard error.
Figure 2.
Predicted mean non-drug medical costs for MS patients adherent (PDC ≥0.8) and non-adherent (PDC <0.8) to index DMT (total n=12,431).
Notes: Predicted mean costs were generated by generalized linear regression and based on the study sample of 5,120 non-adherent patients (PDC <0.8) and 7,311 adherent patients (PDC ≥0.8).
Abbreviations: MS, multiple sclerosis; PDC, proportion of days covered; DMT, disease-modifying therapy; ER, emergency room.
Discussion
This retrospective cohort claims analysis represents one of the largest, most comprehensive study of real-world adherence to DMTs in MS, with respect to the number of patients and DMTs selected from a representative sample of commercially insured individuals in the US, as well as the inclusion of both clinical and economic outcomes. The predominance of women (76.2%) in the study sample simulated the epidemiology of MS, as women are generally affected two to three times more frequently than men.33 Contrary to that observed in Munsell et al,22 oral DMT initiators in this study tended to have greater comorbidity than injectable DMT initiators (as indicated by the mean CCI scores). This may have reflected differences in patient preferences or prescribing patterns between the study populations. A recent retrospective analysis of population-based data in Canada found that the likelihood of initiating a DMT in MS decreased as the total number of comorbidities increased;34 however, the influence of comorbidities on the choice of oral or injectable DMTs has not yet been determined and may merit further investigation.
In this study, overall adherence to the index DMT was suboptimal, with ~40% of patients failing to meet the adherence criteria (PDC ≥0.8). The rate of adherence (60%) at 12 months was lower than that (77%) reported by Yermakov et al, who applied the PDC criteria in a smaller sample (n=1,510) of commercially insured patients.8 In addition to other contributory factors, the disparate findings may have been due to differences between study populations (eg, Yermakov et al included patients with disability claims) or the DMTs analyzed. Defining adherence as an MPR ≥0.8 over a 12-month period, Tan et al (n=2,446) reported an adherence rate of 59.6%,4 while Munsell et al found that 58.2% of oral DMT initiators (n=444) and 54.8% of self-injectable DMT initiators (n=5,238) had been adherent.22 While adherence rates appear to vary among studies according to study sample and methods, it is apparent that adherence remains suboptimal in patients with MS initiating DMTs, and measures to improve adherence are warranted.
Compared to men, women in this study were 24% less likely to be adherent, a trend also observed recently by Higuera et al, who found that women with MS had a 5.5 percentage-point lower probability of being adherent (as measured by the MPR) than men.35 Although the reasons for poorer adherence among women remain speculative, one explanation is that more intense medication use may compromise adherence.36 A pharmacy claims analysis for 16 million women and 13.5 million men in the US found that women were less likely to be adherent to chronic diabetes and cardiovascular medications, but more likely to take additional medications (such as hormonal contraceptives) than men.36 Since MS affects women predominantly, further research may be warranted to identify patient-centric strategies that can promote better adherence to DMTs in women.35
In this analysis, prescriptions for both oral and injectable DMTs covered on average ~265 of 365 days (72.6%) in the post-index period, indicating that patients had no DMT prescription coverage for ~100 days. As previously reported by Munsell et al (who used the MPR to assess adherence),22 we found no significant difference in the likelihood of adherence between oral DMT initiators and injectable DMT initiators after controlling for sex, age at index DMT, and CCI score. Despite having similar mean PDC and comparable rates of discontinuation and switching, injectable DMT initiators remained on the index DMT significantly longer than oral DMT initiators before discontinuing (P=0.0039) or switching (P<0.0001). In a patient preference study using conjoint analysis, Utz et al found that 93% (145 of 156) of patients with MS preferred oral DMTs over injectable forms when dosing frequency and frequency of side effects were held constant.37 However, patients preferred once-weekly injections over oral DMTs given three times per week and injectable over oral DMTs when the latter produced frequent side effects.37 Other studies in MS have also found dosing frequency to be an important preference attribute.32 A prospective, cross-sectional study in Germany concluded that in addition to efficacy, improving convenience and tolerability, two facets of treatment satisfaction, may be beneficial for increasing adherence levels.38 Although this study assessed self-injectable DMTs only, the findings imply that DMTs perceived to enhance convenience (such as requiring less frequent dosing) may improve adherence. However, this remains to be confirmed by future studies assessing the relationship between adherence, treatment preference, and satisfaction with specific DMT attributes.
The observed association between adherence and a lower likelihood of severe relapse (P<0.0001) aligns with the evidence demonstrating that non-adherence is a significant predictor of relapse.4,21,23,24 The clinical importance of adherence in patients initiating DMTs is highlighted by population-based studies showing that the frequency of early relapses in RRMS is predictive of long-term progression to either disability (as per the EDSS) or SPMS.39–42 Likewise, a retrospective analysis of 2,447 patients with RRMS over 20.6 years determined that an early relapse within 5 years after MS onset increased the hazard for disease progression over the short term by 48% (95% CI: 37%–60%) for reaching EDSS 6 and by 29% (95% CI: 20%–38%) for SPMS.43 Therefore, measures that promote adherence may improve overall outcomes for patients newly initiating DMTs by reducing the frequency of early relapse.
Consistent with other literature,4,8,32 adherence was a significant predictor of MS-related HRU and non-drug medical costs in the adjusted analyses. The predicted mean costs indicated that adherence to the index DMT would most favorably impact the costs for hospitalization, reducing expenditures for this known cost driver44 by 58.5%. While the present analysis did not include drug costs, Hartung et al noted that the annual costs for each of nine approved DMTs in the US exceeded $51,000 (2013 US$) per year.14 As better adherence increases DMT drug costs, determining the net economic advantage of improved adherence must also consider health and societal benefits gained, such as lower relapse rates, improvement in quality of life, and increased productivity.
Several study limitations are noted. While administrative claims data can render a reasonable overview of real-world prescribing patterns, whether patients had utilized the DMTs as prescribed could not be determined. Identification of MS cases and the index DMTs was subject to misdiagnosis or coding error. We also included individuals initiating an infusible DMT (natalizumab) in the injectable DMT cohort; however, these patients (n=98) constituted only 0.9% of this cohort. Additionally, the study criteria for identifying MS cases required documentation of two MS diagnosis codes; however, the identified codes may not have signified the initial MS diagnosis, which is a limitation of utilizing claims data.
Factors related to attributes of the study sample may also compromise the generalizability of the study results. First, despite inclusion of 12,431 MS patients, the sample was restricted to commercially insured individuals. Second, given that pregnant or nursing women and those contemplating pregnancy are advised to discontinue DMT,45 and these cases were not identified by the ICD-9-CM codes, the influence of the predominance of women (76.2%) in the sample on adherence was unknown. The lack of data on other clinical characteristics, such as MS subtype, severity, duration, disability, socioeconomic status, frequency of prior hospitalizations, and presence of comorbid depression,46 all of which may affect DMT adherence or clinical outcomes, precluded analyses of these covariates. Notably, fingolimod and natalizumab, second-line DMTs, may be used as initial induction therapies in patients with more aggressive MS,47 the severity of which may affect adherence. Further, no causal inference between non-adherence and relapse could be established in the present study, although the association has been reported in the literature.4,21,23,24 Finally, because the administrative claims database served as the primary data source, the study did not consider the impact of adherence on societal costs and quality of life. Future research applying economic modeling and incorporating real-world indirect costs in MS might determine the impact of adherence on these endpoints.
Conclusion
Adherence is critical for optimizing the efficacy of DMTs in patients with MS, and can reduce the risk of relapse and non-drug medical costs. Despite the wide availability of oral and injectable DMT options for MS, the present findings indicate that adherence remains suboptimal but comparable between patients initiating oral and injectable DMTs. Adherence to DMT was significantly associated with decreased likelihood of relapse, hospitalization, and emergency visits, as well as fewer outpatient visits. In addition, adherence was associated with savings in direct costs for HRU, including medical care, hospitalization, emergency visits, and outpatient visits. As the number of DMT options continues to rise, future studies evaluating the collective and relative impact of DMT attributes, such as dosing frequency, routes of administration, and safety, may provide more insight into product features affecting adherence and aid in the selection of treatments for individuals with MS.
Acknowledgments
Erin Williams of Marinus Consulting LLC provided medical writing and editing services in the development of this manuscript. AbbVie provided funding to Marinus Consulting LLC for writing assistance.
Footnotes
Disclosure
This study was supported by AbbVie. AbbVie participated in study design, research, data collection, analysis and interpretation of data, writing, reviewing and approving the publication. JB is a professor and director of an MS program at Nova Southeastern University. He has provided consulting services for AbbVie, Bayer, Biogen, Genzyme, and Novartis. TSM and XY are employees of AbbVie, and may own stocks/stock options in the company. The authors report no other conflicts of interest in this work.
References
- 1.Milo R, Kahana E. Multiple sclerosis: geoepidemiology, genetics and the environment. Autoimmun Rev. 2010;9(5):A387–A394. doi: 10.1016/j.autrev.2009.11.010. [DOI] [PubMed] [Google Scholar]
- 2.Campbell JD, Ghushchyan V, McQueen RB, et al. Burden of multiple sclerosis on direct, indirect costs and quality of life: national US estimates. Mult Scler Relat Disord. 2014;3(2):227–236. doi: 10.1016/j.msard.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 3.Gelfand JM. Multiple sclerosis: diagnosis, differential diagnosis, and clinical presentation. Handb Clin Neurol. 2014;122:269–290. doi: 10.1016/B978-0-444-52001-2.00011-X. [DOI] [PubMed] [Google Scholar]
- 4.Tan H, Cai Q, Agarwal S, Stephenson JJ, Kamat S. Impact of adherence to disease-modifying therapies on clinical and economic outcomes among patients with multiple sclerosis. Adv Ther. 2011;28(1):51–61. doi: 10.1007/s12325-010-0093-7. [DOI] [PubMed] [Google Scholar]
- 5.Wingerchuk DM, Weinshenker BG. Disease modifying therapies for relapsing multiple sclerosis. BMJ. 2014;354:i3518. doi: 10.1136/bmj.i3518. [DOI] [PubMed] [Google Scholar]
- 6.Scalfari A, Neuhaus A, Daumer M, Muraro PA, Ebers GC. Onset of secondary progressive phase and long-term evolution of multiple sclerosis. J Neurol Neurosurg Psychiatry. 2013;85(1):67–75. doi: 10.1136/jnnp-2012-304333. [DOI] [PubMed] [Google Scholar]
- 7.Tremlett H, Zhao Y, Devonshire V. Natural history comparisons of primary and secondary progressive multiple sclerosis reveals differences and similarities. J Neurol. 2009;256(3):374–381. doi: 10.1007/s00415-009-0039-7. [DOI] [PubMed] [Google Scholar]
- 8.Yermakov S, Davis M, Calnan M, et al. Impact of increasing adherence to disease-modifying therapies on healthcare resource utilization and direct medical and indirect work loss costs for patients with multiple sclerosis. J Med Econ. 2015;18(9):711–720. doi: 10.3111/13696998.2015.1044276. [DOI] [PubMed] [Google Scholar]
- 9.Rubin SM. Management of multiple sclerosis: an overview. Dis Mon. 2013;59(7):253–260. doi: 10.1016/j.disamonth.2013.03.012. [DOI] [PubMed] [Google Scholar]
- 10.Polman CH, O’Connor PW, Havrdova E, et al. A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. N Engl J Med. 2006;354(9):899–910. doi: 10.1056/NEJMoa044397. [DOI] [PubMed] [Google Scholar]
- 11.Pelletier D, Hafler DA. Fingolimod for multiple sclerosis. N Engl J Med. 2012;366(4):339–347. doi: 10.1056/NEJMct1101691. [DOI] [PubMed] [Google Scholar]
- 12.O’Connor P, Wolinsky JS, Confavreux C, et al. Randomized trial of oral teriflunomide for relapsing multiple sclerosis. N Engl J Med. 2011;365(14):1293–1303. doi: 10.1056/NEJMoa1014656. [DOI] [PubMed] [Google Scholar]
- 13.Torkildsen O, Myhr KM, Bo L. Disease-modifying treatments for multiple sclerosis: a review of approved medications. Eur J Neurol. 2016;23(Suppl 1):18–27. doi: 10.1111/ene.12883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hartung DM, Bourdette DN, Ahmed SM, Whitham RH. The cost of multiple sclerosis drugs in the US and the pharmaceutical industry: too big to fail? Neurology. 2015;84(21):2185–2192. doi: 10.1212/WNL.0000000000001608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scalfari A, Neuhaus A, Degenhardt A, et al. The natural history of multiple sclerosis: a geographically based study 10: relapses and long-term disability. Brain. 2010;133(Pt 7):1914–1929. doi: 10.1093/brain/awq118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brex PA, Ciccarelli O, O’Riordan JL, Sailer M, Thompson AJ, Miller DH. A longitudinal study of abnormalities on MRI and disability from multiple sclerosis. N Engl J Med. 2002;346(3):158–164. doi: 10.1056/NEJMoa011341. [DOI] [PubMed] [Google Scholar]
- 17.Goodin DS, Traboulsee A, Knappertz V, et al. Relationship between early clinical characteristics and long term disability outcomes: 16 year cohort study (follow-up) of the pivotal interferon β-1b trial in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2012;83(3):282–287. doi: 10.1136/jnnp-2011-301178. [DOI] [PubMed] [Google Scholar]
- 18.Agashivala N, Wu N, Abouzaid S, et al. Compliance to fingolimod and other disease modifying treatments in multiple sclerosis patients, a retrospective cohort study. BMC Neurol. 2013;13:138. doi: 10.1186/1471-2377-13-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bergvall N, Petrilla AA, Karkare SU, et al. Persistence with and adherence to fingolimod compared with other disease-modifying therapies for the treatment of multiple sclerosis: a retrospective US claims database analysis. J Med Econ. 2014;17(10):696–707. doi: 10.3111/13696998.2014.940422. [DOI] [PubMed] [Google Scholar]
- 20.Evans C, Marrie RA, Zhu F, et al. Adherence and persistence to drug therapies for multiple sclerosis: a population-based study. Mult Scler Relat Disord. 2016;8:78–85. doi: 10.1016/j.msard.2016.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Steinberg SC, Faris RJ, Chang CF, Chan A, Tankersley MA. Impact of adherence to interferons in the treatment of multiple sclerosis: a non-experimental, retrospective, cohort study. Clin Drug Investig. 2010;30(2):89–100. doi: 10.2165/11533330-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 22.Munsell M, Locklear JC, Phillips AL, Frean M, Menzin J. An assessment of adherence among multiple sclerosis patients newly initiating treatment with a self-injectable versus oral disease-modifying drug. Neurology. 2015;84(14):3, 281. [Google Scholar]
- 23.Cohen BA, Coyle PK, Leist T, Oleen-Burkey MA, Schwartz M, Zwibel H. Therapy optimization in multiple sclerosis: a cohort study of therapy adherence and risk of relapse. Mult Scler Relat Disord. 2015;4(1):75–82. doi: 10.1016/j.msard.2014.09.214. [DOI] [PubMed] [Google Scholar]
- 24.Oleen-Burkey M, Dor A, Castelli-Haley J, Lage MJ. The relationship between alternative medication possession ratio thresholds and outcomes: evidence from the use of glatiramer acetate. J Med Econ. 2011;14(6):739–747. doi: 10.3111/13696998.2011.618517. [DOI] [PubMed] [Google Scholar]
- 25.Devonshire V, Lapierre Y, Macdonell R, et al. The Global Adherence Project (GAP): a multicenter observational study on adherence to disease-modifying therapies in patients with relapsing-remitting multiple sclerosis. Eur J Neurol. 2011;18(1):69–77. doi: 10.1111/j.1468-1331.2010.03110.x. [DOI] [PubMed] [Google Scholar]
- 26.Saiz A, Mora S, Blanco J. Therapeutic compliance of first line disease-modifying therapies in patients with multiple sclerosis: COMPLIANCE study. Neurologia. 2015;30(4):214–222. doi: 10.1016/j.nrl.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 27.McGregor JC, Kim PW, Perencevich EN, et al. Utility of the Chronic Disease Score and Charlson Comorbidity Index as comorbidity measures for use in epidemiologic studies of antibiotic-resistant organisms. Am J Epidemiol. 2005;161(5):483–493. doi: 10.1093/aje/kwi068. [DOI] [PubMed] [Google Scholar]
- 28.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 29.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 30.Nau DP. Proportion of days covered (PDC) as a preferred method of measuring medication adherence. [Accessed February 6, 2017]. Available from: http://www.pqaal-liance.org/images/uploads/files/PQA%20PDC%20vs%20%20MPR.pdf.
- 31.Chastek BJ, Oleen-Burkey M, Lopez-Bresnahan MV. Medical chart validation of an algorithm for identifying multiple sclerosis relapse in healthcare claims. J Med Econ. 2010;13(4):618–625. doi: 10.3111/13696998.2010.523670. [DOI] [PubMed] [Google Scholar]
- 32.Lizan L, Comellas M, Paz S, Poveda JL, Meletiche DM, Polanco C. Treatment adherence and other patient-reported outcomes as cost determinants in multiple sclerosis: a review of the literature. Patient Prefer Adherence. 2014;8:1653–1664. doi: 10.2147/PPA.S67253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Howard J, Trevick S, Younger D. Epidemiology of multiple sclerosis. Neurol Clin. 2016;34(4):919–939. doi: 10.1016/j.ncl.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 34.Zhang T, Tremlett H, Leung S, et al. Examining the effects of comorbidities on disease-modifying therapy use in multiple sclerosis. Neurology. 2016;86(14):1287–1295. doi: 10.1212/WNL.0000000000002543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Higuera L, Carlin CS, Anderson S. Adherence to disease-modifying therapies for multiple sclerosis. J Manag Care Spec Pharm. 2016;22(12):1394–1401. doi: 10.18553/jmcp.2016.22.12.1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Manteuffel M, Williams S, Chen W, Verbrugge RR, Pittman DG, Steinkellner A. Influence of patient sex and gender on medication use, adherence, and prescribing alignment with guidelines. J Womens Health (Larchmt) 2014;23(2):112–119. doi: 10.1089/jwh.2012.3972. [DOI] [PubMed] [Google Scholar]
- 37.Utz KS, Hoog J, Wentrup A, et al. Patient preferences for disease-modifying drugs in multiple sclerosis therapy: a choice-based conjoint analysis. Ther Adv Neurol Disord. 2014;7(6):263–275. doi: 10.1177/1756285614555335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Haase R, Kullmann JS, Ziemssen T. Therapy satisfaction and adherence in patients with relapsing-remitting multiple sclerosis: the THEPA-MS survey. Ther Adv Neurol Disord. 2016;9(4):250–263. doi: 10.1177/1756285616634247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Confavreux C, Vukusic S, Adeleine P. Early clinical predictors and progression of irreversible disability in multiple sclerosis: an amnesic process. Brain. 2003;126(Pt 4):770–782. doi: 10.1093/brain/awg081. [DOI] [PubMed] [Google Scholar]
- 40.Weinshenker BG, Bass B, Rice GP, et al. The natural history of multiple sclerosis: a geographically based study – 2: predictive value of the early clinical course. Brain. 1989;112(Pt 6):1419–1428. doi: 10.1093/brain/112.6.1419. [DOI] [PubMed] [Google Scholar]
- 41.Weinshenker BG, Rice GP, Noseworthy JH, Carriere W, Baskerville J, Ebers GC. The natural history of multiple sclerosis: a geographically based study – 3: multivariate analysis of predictive factors and models of outcome. Brain. 1991;114(Pt 2):1045–1056. doi: 10.1093/brain/114.2.1045. [DOI] [PubMed] [Google Scholar]
- 42.Eriksson M, Andersen O, Runmarker B. Long-term follow up of patients with clinically isolated syndromes, relapsing-remitting and secondary progressive multiple sclerosis. Mult Scler. 2003;9(3):260–274. doi: 10.1191/1352458503ms914oa. [DOI] [PubMed] [Google Scholar]
- 43.Tremlett H, Yousefi M, Devonshire V, Rieckmann P, Zhao Y. Impact of multiple sclerosis relapses on progression diminishes with time. Neurology. 2009;73(20):1616–1623. doi: 10.1212/WNL.0b013e3181c1e44f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ke X, Navaratnam P, Sasane R, et al. Determinants of high cost in multiple sclerosis patients: a claims and chart review study. Curr Med Res Opin. 2016;32(9):1589–1597. doi: 10.1080/03007995.2016.1192529. [DOI] [PubMed] [Google Scholar]
- 45.Lu E, Wang BW, Guimond C, et al. Safety of disease-modifying drugs for multiple sclerosis in pregnancy: current challenges and future considerations for effective pharmacovigilance. Expert Rev Neurother. 2013;13(3):251–261. doi: 10.1586/ern.13.12. [DOI] [PubMed] [Google Scholar]
- 46.Tarrants M, Oleen-Burkey M, Castelli-Haley J, Lage MJ. The impact of comorbid depression on adherence to therapy for multiple sclerosis. Mult Scler Int. 2011;2011 doi: 10.1155/2011/271321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gajofatto A, Benedetti MD. Treatment strategies for multiple sclerosis: when to start, when to change, when to stop? World J Clin Cases. 2015;3(7):545–555. doi: 10.12998/wjcc.v3.i7.545. [DOI] [PMC free article] [PubMed] [Google Scholar]