Abstract
Total anomalous pulmonary venous return (TAPVR), also known as total anomalous pulmonary venous connection, is a congenital cardiovascular malformation that presents itself in the neonatal period, with cyanosis and tachypnea. There are 4 types of TAPVR with the mixed type being the least common. Any type of TAPVR may be associated with obstruction as result of flow redirection through the liver parenchyma before it may return to the heart, but infracardiac is the most common one.
We report a case of a 10-hour-old female, with a mixed (cardiac and infracardiac) TAVPR with obstruction, that showed drainage to the coronary sinus and the portal vein, as the other classic findings in TAVPR, made with computed tomography angiography and echocardiogram. The patient was taken to surgical repair, but unfortunately died during the procedure because of multiple complications.
Keywords: Congenital, Total anomalous pulmonary venous return, Pulmonary venous anomalies, Computed tomography
Case report
A female newborn, 10 hours old, product of second pregnancy of a 31-year-old mother, with an antenatal diagnosis of hypoplastic left heart syndrome by obstetric ultrasound was admitted at our hospital referred by another center who attended the delivery.
Born at term by cesarean section, weighing at 2605 grams, with negative STORCH and no other previous history. At admission, the patient was slightly hypotense, cyanotic, tachypneic, and had a generalized constant heart murmur and slight pulmonary rales as the only positive finding.
A chest x-ray was performed, which showed extensive mixed type opacities in both lungs, with prominent pulmonary vasculature and apparent normal cardiac silhouette. An echocardiogram was performed, which showed total anomalous venous drainage probably intracardiac to coronary sinus, severe pulmonary hypertension, severe dilatation of right heart cavities, slight hypoplasia of left heart cavities, patent ductus arteriosus, and permeable foramen ovale.
A computed tomography angiography was ordered and it showed an infracardiac total anomalous venous return with drainage to the left branch of the porta (Fig. 1, Fig. 2, Fig. 3) and a filiform but varicose vein that drained to the coronary sinus, ostium secundum (Fig. 4), hypoplastic ascending aorta and aortic arch (Fig. 5), common origin of the brachiocephalic trunk and the left common carotid. Also, a patent ductus arteriosus was confirmed, and 3-dimensional reconstructions were performed.
Fig. 1.
Coronal maximum intensity-projection computed tomography (CT) image shows pulmonary veins drain through a common trunk into the left branch of the porta, which is dilated, configuring findings of infracardiac TAVPR.
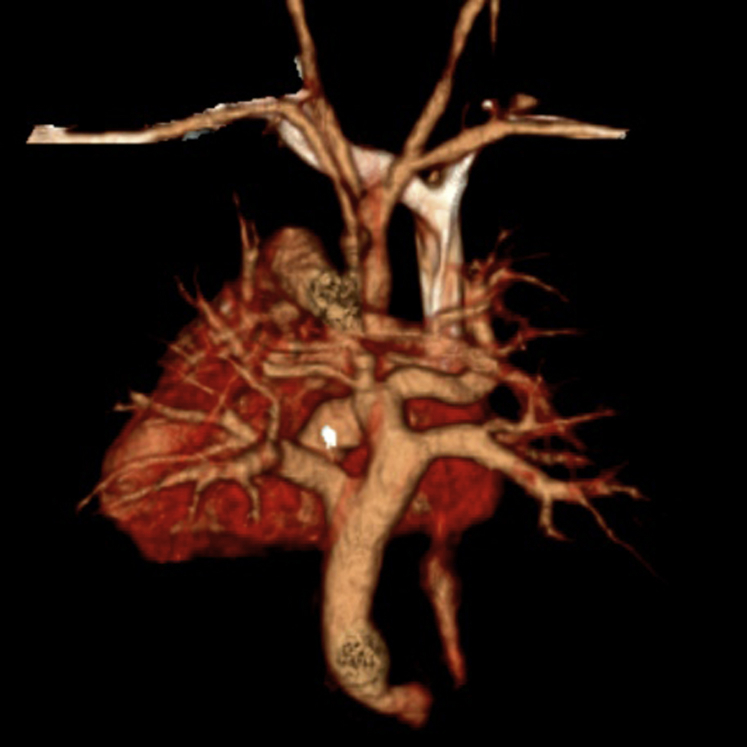
Fig. 2.
Tridimensional reconstruction (3D) CT image in posteroanterior view shows pulmonary veins drain through a common trunk.
Fig. 3.
Tridimensional reconstruction (3D) CT image in posteroanterior view shows pulmonary veins drain through a common trunk below the diaphragm.
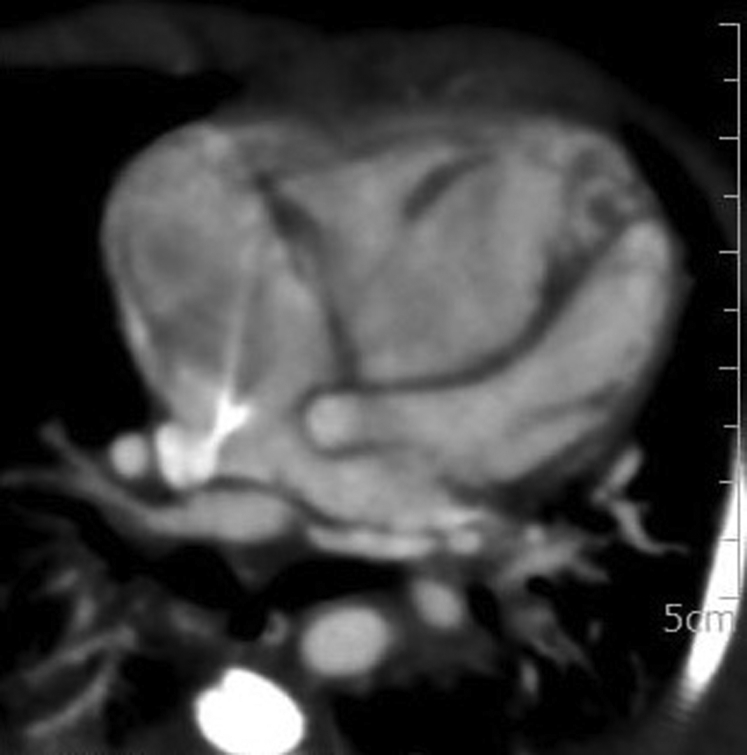
Fig. 4.
Axial 4 chambers projection CT image shows ostium secundum atrial septal defect and hypoplastic left atrium.
Fig. 5.
Tridimensional reconstruction (3D) CT image in posteroanterior view shows a patent ductus arteriosus, hypoplastic ascending aorta and aortic arch and also a common origin of the brachiocephalic trunk and the left common carotid.
The patient was taken to surgical repair. Unfortunately, the patient died during the procedure because of multiple complications.
Discussion
Total anomalous pulmonary venous return (TAPVR), also known as total anomalous pulmonary venous connection, represents 1%-5% of cardiovascular congenital anomalies [1], [2], [3], [4], [5]. It consists of an anomalous connection between the pulmonary veins with the right atrium, or with one or more systemic veins [6], [7]. This type of congenital cardiovascular malformation is more frequently seen in patients with heterotaxy syndromes, especially asplenia or polysplenia [3], [4], [8]. The malformation usually presents itself accompanied by neonatal cyanosis and tachypnea [9] and if a systemic-pulmonary shut (right to left heart shunt) is not performed, it may be a cause of considerably mortality [1], [4]; typical shunts occur by an atrial septal defect (patent foramen ovale) or patent ductus arteriosus (less common), with these communications being almost obligatory for survival [1], [2], [4], [8]. TAPVR is a consequence of the persistence of the primitive connections of the pulmonary veins with the cardinal systemic veins, which results in a failure of common pulmonary veins to connect to the left atrium [10], [11].
The classification of TAPVR is based on the location of the pulmonary venous drainage [1]. There are 4 types: (1) supracardiac, (2) cardiac, (3) infracardiac, and (4) mixed [1], [4], [5], [6], [8], [10]. The supracardiac type is the most common, and it accounts for 44% of cases, followed by the infracardiac (26%), cardiac (21%), and mixed type (9%) [1], [3], [6]. In the supracardial type, the pulmonary veins drain through a vertical vein into the left brachiocephalic vein [1], but rarely drain to the superior vena cava, left superior vena cava, or to the azygous system [1], [12]. In the cardiac type, the pulmonary veins drain to the coronary sinus or directly to the right atrium [1], [3], [5], [6]. In the infracardiac type, the second most common, the drainage is located below the diaphragm, and may be either to a systemic vein such as inferior vena cava, hepatic veins or azygos system, or to the portal venous system [1], [3], [6], [10]. Finally, when the pulmonary veins drain to at least 2 different locations, above or below the diaphragm, it is considered a mixed type [1], [3].
Any type of TAPVR may be associated with obstruction. However, the infracardiac type is the most frequent (78%) [1], [3], [13], [14]. This type of TAPVR is characterized by obstruction located at the level of the diaphragm, caused by an extrinsic narrowing, resulting in a pulmonary edema appearance with normal cardiac silhouette in conventional imaging [1], [3], [6], [12]. This obstruction could be a result of the need for flow redirection through the liver parenchyma before it may return to the heart [6]. Also, the infracardiac type, when draining to the portal vein, may be associated with formation of an aneurism of the portal venous system, described in the literature as being fusiform or saccular, secondary to the increased venous pressures in the portal system [10]. There are few reports in the literature where they describe obliteration of the descending vertical vein with development of multiple collateral pathways [15].
In our case, an infracardiac type of TAVPR was found with drainage to the left branch of the porta (Fig. 1) and a filiform but varicose vein that drains to the coronary sinus. There are signs of obstruction as the drainage is not only through the liver parenchyma, but also because there is dilatation of the portal vein (Fig. 1). Three-dimensional reconstructions allowed for an adequate visualization of the vascular drainage pathway and made easier the understanding of the abnormal anatomy (Figs. 2 and 3). Classic findings in TAVPR like presence of ostium secundum or patent ductus arteriosus were also present (Figs. 4 and 5). Associated findings related to other cardiovascular anomalies were: hypoplastic ascending aorta; and aortic arch and a common origin of the brachiocephalic trunk and the left common carotid (Fig. 5).
Knowledge of the anatomy and the drainage location is essential in the preoperative planning [1], [3]. Chest radiography and echocardiography are the first examinations to be obtained [1], [3], [14]. Echocardiography may be limited in this case specially because of the small field of view and sonic window [7]. Therefore, contrast-enhanced computed tomography and magnetic resonance angiography (MRA) are markedly valuable as they provide accurate anatomic information used for presurgical planning and for postsurgical follow-up [1], [4], [6], [8]. Also, computed tomography allows for the performance of 3-dimensional reconstructions for advanced spatial and anatomic orientation [4], [6]. Reported sensitivities and specificities for MDCT for depicting the drainage site, areas of stenosis of the vertical vein, and the course and caliber of the anomalous vessel is 100% [4], [13]. As a disadvantage, MDCT uses ionizing radiation, which is why, in these patients, dose modulation must be adjusted to the neonatal body-weight parameters [4]. An advantage of magnetic resonance imaging—MRA over MDCT is that it does not use ionizing radiation. However, the need of sedation, prolonged scan times, and the need for trained technicians may become a disadvantage favoring the use of MDCT [4].
The imaging findings vary depending on the subtype of TAVPR. Chest radiography findings include increased pulmonary vascularization and pulmonary edema with or without cardiomegaly [4], [14]. In the supracardiac type, if the drainage is to the left brachiocephalic vein, a characteristic “snowman” or “8-figure” signs may be found being formed by the dilated vertical vein on the left side and the superior vena cava forming the head and the heart as the body [4], [8].
The most important complication in the postoperative period for these patients is the development of pulmonary vein stenosis (5%-19%) [16]. Also, pulmonary hypertension and pulmonary venous obstruction may appear as complications [4]. Five-year survival rates have been reported for 97% of patients [3], but in case of pulmonary stenosis, 3-year survival may be decreased in up to 58.7% [16].
Survival beyond infancy without treatment is uncommon [16], [17]. Those patients who may survive until adulthood present a large atrial defect, but later they may develop pulmonary vascular disease leading to increased cyanosis secondary to a decrease in pulmonary blood flow [16], [17]. Furthermore, adequate postsurgical outcomes may be achieved in adult patients [16].
Conclusion
TAVPR is an uncommon congenital cardiac anomaly. Among the 4 types described in the literature, the mixed type is the least common. All types may be associated with obstruction, with infracardiac being the most common. Chest radiography and echocardiography are the first examinations to be obtained; however, they may be limited in the diagnosis. Contrast-enhanced MDCT and MRA are especially useful in the diagnosis as they provide accurate anatomic information used for presurgical planning—information which may also may be critical in the postsurgical follow-up. Knowledge of the anatomy and the drainage location is essential for guiding the clinician and surgical team to an appropriate execution of the procedure.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Dillman J.R., Yarram S.G., Hernandez R.J. Imaging of pulmonary venous developmental anomalies. AJR. 2009;192:1272–1285. doi: 10.2214/AJR.08.1526. [DOI] [PubMed] [Google Scholar]
- 2.Herlong J.R., Jaggers J.J., Ungerleider R.M. Congenital Heart Surgery Nomenclature and Database Project: pulmonary venous anomalies. Ann Thorac Surg. 2000;69:S56–S69. doi: 10.1016/s0003-4975(99)01237-0. [DOI] [PubMed] [Google Scholar]
- 3.Karamlou T., Gurofsky R., Al Sukhni E., Coles J.G., Williams W.G., Caldarone C.A. Factors associated with mortality and reoperation in 377 children with total anomalous pulmonary venous connection. Circulation. 2007;115:1591–1598. doi: 10.1161/CIRCULATIONAHA.106.635441. [DOI] [PubMed] [Google Scholar]
- 4.Katre R., Burns S.K., Murillo H., Lane M.J., Restrepo C.S. Anomalous pulmonary venous connections. Semin Ultrasound CT MRI. 2012;33:485–499. doi: 10.1053/j.sult.2012.07.001. [DOI] [PubMed] [Google Scholar]
- 5.Shamsuddin A.M., Wong A.R., Anderson R.H., Corno A.F. An unusual type of totally anomalous pulmonary venous connection to the superior cavoatrial junction. World J Pediatr Congenit Heart Surg. 2016;7(4):490–493. doi: 10.1177/2150135115603330. [DOI] [PubMed] [Google Scholar]
- 6.Dyer K.T., Hlavacek A.M., Meinel F.G., De Cecco C.N., McQuiston A.D., Schoepf U.J. Imaging in congenital pulmonary vein anomalies: the role of computed tomography. Pediatr Radiol. 2014;44:1158–1168. doi: 10.1007/s00247-014-3044-7. [DOI] [PubMed] [Google Scholar]
- 7.Kim T.H., Kim Y.M., Suh C.H., Cho D.J., Park I.S., Kim W.H. Helical CT angiography and three-dimensional reconstruction of total anomalous pulmonary venous connections in neonates and infants. AJR. 2000;175:1381–1386. doi: 10.2214/ajr.175.5.1751381. [DOI] [PubMed] [Google Scholar]
- 8.Demos T.C., Posniak H.V., Pierce K.L., Olson M.C., Muscato M. Venous anomalies of the thorax. AJR. 2004;182:1139–1150. doi: 10.2214/ajr.182.5.1821139. [DOI] [PubMed] [Google Scholar]
- 9.Munsi A.S., Hussain M., Rima R., Biswas R., Sayeed A. Clinical profile of patients with total anomalous pulmonary venous return and their shot term outcome in pediatric cardiac centre at Dhaka Shishu Hospital. Bangladesh J Med Sci. 2015;14(3):270–274. [Google Scholar]
- 10.Bhatia A., Sodhi K.S., Saxena A.K., Singhal M., Khandelwal N. Infracardiac total anomalous pulmonary venous return: an unusual cause of neonatal portal vein enlargement. World J Pediatr Congenit Heart Surg. 2014;5(1):131–132. doi: 10.1177/2150135113504307. [DOI] [PubMed] [Google Scholar]
- 11.Vyas H.V., Greenberg S.B., Krishnamurthy R. MR imaging and CT evaluation of congenital pulmonary vein abnormalities in neonates and infants. Radiographics. 2012;32(1):87–98. doi: 10.1148/rg.321105764. [DOI] [PubMed] [Google Scholar]
- 12.White C.S., Baffa J.M., Haney P.J., Pace M.E., Campbell A.B. MR imaging of congenital anomalies of the thoracic veins. RadioGraphics. 1997;17:595–608. doi: 10.1148/radiographics.17.3.9153699. [DOI] [PubMed] [Google Scholar]
- 13.Oh K.H., Choo K.S., Lim S.J., Lee H.D., Park J.A., Jo M.J. Multidetector CT evaluation of total anomalous pulmonary venous connections: comparison with echocardiography. Pediatr Radiol. 2009;39:950–954. doi: 10.1007/s00247-009-1309-3. [DOI] [PubMed] [Google Scholar]
- 14.Shen Q., Pa M., Hu X., Wang J. Role on plain radiography and CT angiography in the evaluation of obstructed pulmonary venous connection. Pediatr Radiol. 2014;47(3):827–835. doi: 10.1007/s00247-012-2609-6. [DOI] [PubMed] [Google Scholar]
- 15.Mishra A., Pujara J., Jain I., Baria K., Patel H. Totally anomalous pulmonary venous connection with obliterated vertical vein. World J Pediatr Congenit Heart Surg. 2016;7(4):513–515. doi: 10.1177/2150135115607188. [DOI] [PubMed] [Google Scholar]
- 16.Wu F.M., Emani S.M., Landzberg M.J., Valente A.M. Rare case of undiagnosed supracardiac total anomalous pulmonary venous return in an adult. Circulation. 2014;130:1205–1207. doi: 10.1161/CIRCULATIONAHA.114.008013. [DOI] [PubMed] [Google Scholar]
- 17.Sharma A., Fulwani M., Kulkarni V. Total anomalous pulmonary venous drainage into coronary sinus along with atrial septal defect and pulmonary stenosis—a rare congenital anomaly in an adult. Indian J Thorac Cardiovasc Surg. 2013;29(1):14–15. [Google Scholar]