Abstract
Ossifying fibroma is a benign fibro-osseous lesion that occurs most commonly in the mandible of female patients. In rare cases, it affects the nasal cavity. The magnetic resonance imaging features may vary depending on the amount of fibrous and bony tissue in its composition. In these tumors, T2-hypointensity is a feature described in the peripheral ossified areas of the lesion, but it may present diffusely, especially when the degree of ossification is extensive. In this scenario, this particular characteristic on T2-weighted imaging is superimposable to the commonly described appearance of other lesions, such as non-Hodgkin's lymphoma, melanoma, and other sinonasal neoplasms with high cellularity and high nucleocytoplasmic ratio. In the present study, we report a case of ossifying fibroma of the nasal cavity that presented as a diffusely and homogeneously T2-hypointense mass, a finding that may cause difficulty in the differential diagnosis with other expansive sinonasal lesions.
Keywords: Ossifying fibroma, Magnetic resonance imaging, T2-hypointensity
Introduction
Ossifying fibroma (OF) is considered a rare benign fibro-osseous lesion that occurs most commonly in female patients during the third and fourth decades of life [1]. It mainly involves the mandibular and maxillary bones, although in rare cases it may develop within the nasal cavity or in long bones [2].
It is often discovered incidentally; nevertheless, it can be locally aggressive. It is best imaged by computed tomography (CT), with magnetic resonance imaging (MRI) serving for surgical planning or evaluation of complications [3].
Imaging features vary with the amount of fibrous and bony tissue within the tumor. Although early-stage lesions may have a thick peripheral rim of bone surrounding a fibrous soft-tissue center, late-stage lesions may be completely filled by bone [3]. On MRI, OF usually has low to intermediate signal on T1-weighted imaging (T1WI) and variable signal on T2-weighted imaging (T2WI). It is widely accepted that low signal on T2WI typically occurs in the ossified peripheral areas of the lesion, whereas higher signal tends to be observed in the nonossified central areas [4]. Despite this classical appearance, there have been some case reports that describe a distinct pattern of imaging presentation on which a largely calcified mass representing OF demonstrates an overall low signal on T2WI [4].
In this more calcified form of appearance, sinonasal OF may have T2WI signal features superimposable with other clinically important lesions that potentially affect the same anatomical region. These differential diagnoses include non-Hodgkin's lymphoma (NHL), whose signal hypointensity on T2WI sequences is explained by a variety of reasons: high cellularity and high nucleocytoplasmic ratio, which both shorten the relaxation time. In addition, sinonasal melanoma may present with similar T2WI hypointensity. However, in this particular case, the low signal is primarily due to the paramagnetic effect of melanin [3].
In the present study, we report a case of a patient who presented with a diffuse and homogeneously T2-hypointense nasal cavity mass—which ultimately turned out to be an OF—making it hard to exclude from the preoperative differential diagnoses more concerning lesions classically associated with this particular imaging pattern, such as NHL and melanoma.
Case presentation
A 23-year-old male patient was referred to the Otorhinolaryngology outpatient clinic with symptoms of a 6-month right progressive nasal congestion and 1 year bulging on the homolateral face when deep breathing. He denied nasal pruritus, sternal attacks, rhinorrhea, epistaxis, hyposmia, as well as weight loss and adynamia. He reported a car accident 2 years ago. He also confessed to being a former cocaine user and reported some episodes of left epistaxis during drug abuse. He has being abstinent for 3 months at the moment of the interview. Other aspects of the previous personal and family history are unremarkable.
Rhinoscopy showed an irregular expansive lesion obstructing the nasal cavity on the right. Other aspects of the physical examination were unremarkable. Nasofibroscopy and nasopharyngolaryngoscopy revealed a mass occupying the posterior two-thirds of the right nasal cavity, with a fleshy appearance, consistent with nasal tumor. Then, the more likely clinical hypothesis of olfactory esthesioneuroblastoma was suggested.
After that, the patient was referred for a CT scan, which was inconclusive, evidencing a bulky heterogeneous expansive mass with mild contrast uptake located in the right nasal cavity and ipsilateral ethmoidal and frontal sinuses (Fig. 1). Then, MRI was performed to clarify the diagnosis and to plan the surgery. In the images obtained by MRI, a solid expansive mass centered on the right nasal cavity was observed, with intermediate signal on T1WI and diffuse and homogeneous hyposignal on T2WI (Fig. 2). The lesion provoked destruction of the sinonasal skeleton and invasion of the right ethmoid and both frontal sinuses, as well as showed signs of possible intracranial extension (Fig. 3). The possibility of a tumor with high cellularity and high nucleocytoplasmic ratio, such as a lymphoproliferative lesion, a nasal melanoma, or an undifferentiated sinonasal carcinoma, was considered in face of the T2WI hyposignal of the lesion and its invasive pattern.
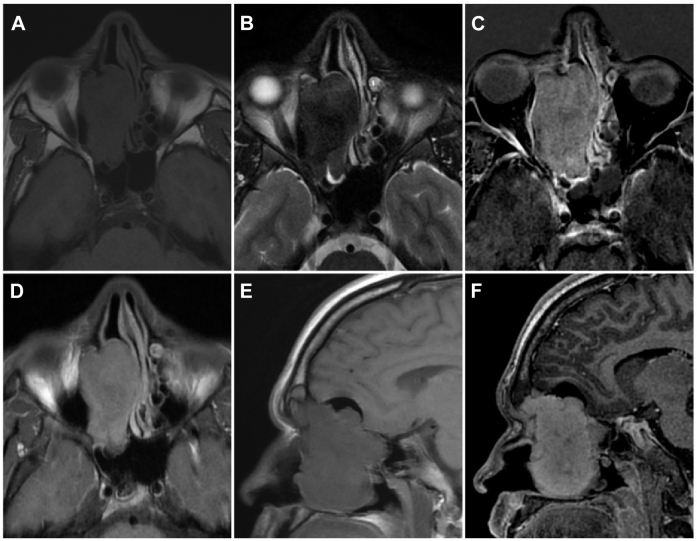
Fig. 1.
Twenty-three-year-old male CT images. (A) Noncontrast axial soft-tissue window. (B) Noncontrast axial bone window and (C) post-contrast coronal. There is a mass filling the right nasal cavity, with bony involvement and mild contrast uptake. CT, computed tomography.
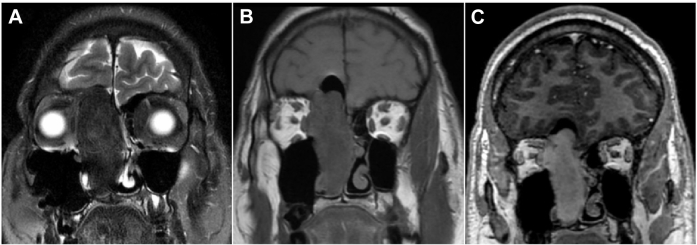
Fig. 2.
Twenty-three-year-old male MRI. (A) Axial T1WI. (B) Axial T2WI. (C) Postgadolinium axial T1WI subtraction image. (D) Postgadolinium axial T1WI. (E) Sagittal T1WI. (F) Postgadolinium sagittal T1WI. There is an invasive mass filling the right nasal cavity, showing enhancement postgadolinium (C, D, and F) and marked hyposignal on T2WI (B). MRI, magnetic resonance imaging; T1WI, T1-weighted imaging; T2WI, T2-weighted imaging.
Fig. 3.
Twenty-three-year-old male MRI imaging on coronals. (A) T2WI. (B) T1WI. (C) postgadolinium T1WI. The marked T2WI hyposignal is again observed diffusely and homogeneously within the mass (A). In addition, it is evident the enhancement postgadolinium (C). It is noticed intracranial extradural extension on the superior aspect of the lesion as well (B and C). MRI, magnetic resonance imaging; T1WI, T1-weighted imaging; T2WI, T2-weighted imaging.
Because of the moderate growth of the lesion between CT and MRI examinations, it was decided to operate. Resection of the nasal tumor was performed by “the debulking technique” with dissection up to the skull base, evidencing a large area of meningeal exposure with a small extravasation of cerebrospinal fluid (Fig. 4).
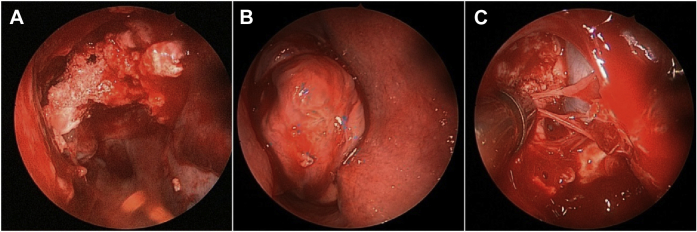
Fig. 4.
Imaging of the tumor during surgical procedure. (A) At the beginning of the surgery, filling the right nasal cavity. (B) After the removal of its inferior portion. (C) The most superior portion of the tumor appears to be in close contact with dura mater.
In face of the malignancy suspicion, an anatomopathological freezing study was acquired during the surgical procedure, which resulted in no malignancy. After the fixation and the inclusion in paraffin of surgical specimens, histological sections revealed a well-delimited lesion composed of spindle cells with elongated nuclei in bone matrix associated with osteoblast rhyme and osteocytes without atypia. Mitotic activity was low and there was no necrosis; therefore, the findings were compatible with ossifying fibroma (Fig. 5).
Fig. 5.
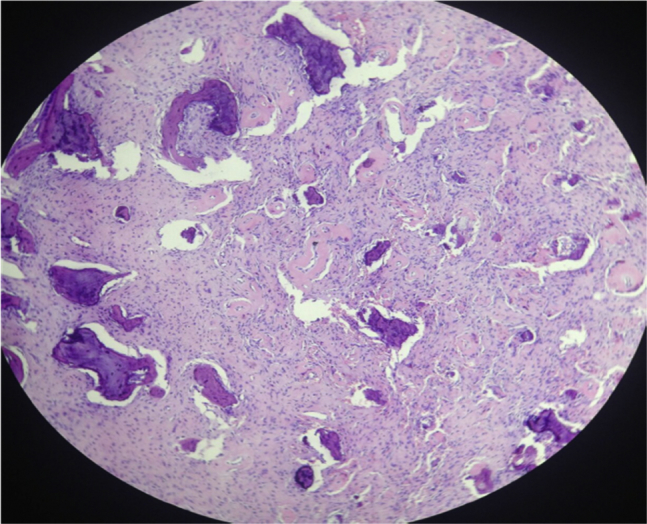
Histopathologic findings of the case. Basophilic areas representing malformed trabeculae osseous, and eosinophilic areas representing the fibrous stroma, which is formed by fibroblasts without atypia. This finding is consistent with ossifying fibroma. H&E coloration increased by 40×.
In follow-up consults, which happened 3 and 9 months after the surgery, the patient was asymptomatic, with no evidence of residual lesion neither on physical examination nor on rhinoscopy.
Discussion
Ossifying fibroma is a rare benign fibro-osseous lesion first described by Menzel in 1872, and the term was first introduced in literature by Montgomery in 1927 [4]. It occurs most commonly in the mandible of female patients during the third and fourth decades of life [1].
As regards classification, it is part of the group of benign fibro-osseous lesions, which includes a spectrum of lesions ranging from fibrous dysplasia to ossifying fibroma, including cementum-osseous dysplasia and juvenile active ossifying fibroma [4]. The OF supposed origin is from mesenchymal blastic cells [2], being formed by high-cellularity fibrous tissue with varying amounts of calcified tissue similar to bone, cement, or both [5].
On the subject of localization and distribution, this lesion predominantly involves the mandibular bone in approximately 75% of cases and the maxilla in 10% to 20%, although in rare cases it may involve the nasal cavity and long bones [2]. Occurrence in paranasal sinuses is considered rare, as only 48 cases were reported by 2011 [4].
It is usually discovered incidentally but it can be locally aggressive. The lesion is best imaged by CT, with MRI serving for surgical planning or evaluation of complications. Imaging features vary with the amount of fibrous and bony tissue within the lesion, being typical in early stages the presence of a thick peripheral rim of bone surrounding a fibrous soft-tissue center, occurring progressive filling of this center with mature bone in later stages [3].
In addition, in the images acquired by MRI, OF usually has low to intermediate signal on T1WI and variable signal on T2WI, being accepted that low T2WI signal occurs in the ossified peripheral areas of the lesion, whereas its nonossified central areas, cystic areas, and associated mucoceles generally have T2WI hypersignal [4]. Thus, regarding the signal intensity on T2WI, OF is usually reported as presenting a hyperintense central region [6], or as a predominantly hyperintense lesion [2]. In addition, there are reports of presentation as a largely calcified mass, and calcified areas tend to appear hypointense on T2WI [4]. Therefore, depending on the degree of calcification, the hypointense signal on T2WI may be predominant, as in the case of this present study.
The main differential diagnoses cited in literature include fibrous dysplasia, sinonasal psammomatous meningioma and well-differentiated osteosarcoma. The first one tends to be more monotonous and polyostotic than OF, the second one usually presents as a polypoid mass, and the third one generally is more aggressive in comparison to OF [4].
However, the T2WI hypointensity of the reported case opens the range of differential diagnoses toward the tumor lesions classically associated with this feature, which are those with high nucleocytoplasmic ratio, such as sinonasal melanoma and sinonasal lymphoma. The T2-hypointense signal of these tumors is explained by its high cellularity and high nucleocytoplasmic ratio because both shorten the relaxation time. In addition, the signal features of sinonasal melanoma are influenced by the paramagnetic effect of melanin [3].
The importance of reminding these options of diagnosis is the great prognostic implications. Although OF is a benign lesion, sinonasal melanoma and NHL, otherwise, are aggressive and may have poor surgical outcomes. However, in the case reported, it was almost indistinguishable those possibilities from OF on imaging assessment, in face of the invasive pattern associated with the marked hyposignal on T2WI.
Furthermore, invasive aspergilloma, Wegener's granulomatosis, and IgG4-related disease with sinonasal involvement must be considered as differential diagnosis of T2WI hypointense sinonasal lesions, which can be distinguished on the basis of clinical setting and IgG4 seric measurement [7]. Because of the absence of specific clinical history and the invasive pattern of the tumor on images, such diagnostic possibilities were considered less probable for the case under study.
The solitary fibrous tumor of the sinonasal cavity must also be included in the differential diagnosis because it usually presents as slow-growth painless mass with heterogeneous hyposignal on T2WI. This signal characteristic is justified by the high collagen content fibrous tissue [8]. As this condition tends to be more heterogeneous on T2WI than our case, it was also considered less probable.
In summary, OF is a fibro-osseous lesion that occurs mainly on the mandibular and maxillary bones and rarely on paranasal sinuses. To prevent misdiagnosis, the radiologists must be aware that this condition may present as an invasive and predominantly T2-hypointense lesion on imaging assessment. Therefore, it must be reminded as a differential diagnosis of sinonasal lesions typically associated with this features, which are those with high nucleocytoplasmic ratio, such as sinonasal melanoma and sinonasal lymphoma.
Footnotes
Acknowledgments: Authors wish to acknowledge Dr. André Alencar Araripe Nunes, otorhinolaryngologist at Walter Cantidio University Hospital, Fortaleza.
References
- 1.de Andrade M., Silva-Sousa Y.T.C., Marques M.F.T., Pontual M.L., Ramos-Perez F.M., Perez D.E. Ossifying fibroma of the jaws: a clinicopathological case series study. Braz Dent J. 2013;24(6):662–666. doi: 10.1590/0103-6440201302364. [DOI] [PubMed] [Google Scholar]
- 2.Kendi A.T.K., Kara S., Altinok D., Keskil S. Sinonasal ossifying fibroma with fluid-fluid levels on MR images. Am J Neuroradiol. 2003;24:1639–1641. [PMC free article] [PubMed] [Google Scholar]
- 3.McCollister K.B., Hopper B.D., Michel M.A. Sinonasal neoplasms: update on classification, imaging features, and management. Appl Radiol. 2015;44(12):7–15. [Google Scholar]
- 4.Mohsenifar Z., Nouhi S., Abbas F.M., Farhadi S., Abedin B. Ossifying fibroma of the ethmoid sinus: report of a rare case and review of literature. J Res Med Sci. 2011;16(6):841–847. [PMC free article] [PubMed] [Google Scholar]
- 5.Liu Y., Wang H., You M., Yang Z., Miao J., Shimizutani K. Ossifying fibromas of the jaw bone: 20 cases. Dentomaxillofac Radiol. 2010;39(1):57–63. doi: 10.1259/dmfr/96330046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jung S.L., Choi K.H., Park Y.H., Song H.C., Kwon M.S. Cemento-ossifying fibroma presenting as a mass of the parapharyngeal and masticator space. Am J Neuroradiol. 1999;20:1744–1746. [PMC free article] [PubMed] [Google Scholar]
- 7.Prabhu S.M., Yadav V., Irodi A., Mani S., Varghese A.M. IgG4-related disease with sinonasal involvement: a case series. Indian J Radiol Imaging. 2014;24(2):117–120. doi: 10.4103/0971-3026.134384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang B.T., Song Z.L., Wang Y.Z. Solitary fibrous tumor of the sinonasal cavity: CT and MR imaging findings. Am J Neuroradiol. 2013;34:1248–1251. doi: 10.3174/ajnr.A3485. [DOI] [PMC free article] [PubMed] [Google Scholar]