Abstract
The purpose of this study was to examine differences in levator veli palatini (levator) morphology between adults with repaired cleft palate and adults with non-cleft anatomy. Fifteen adult participants (10 with non-cleft anatomy, 5 with repaired cleft palate) completed a 3D static MRI. Image analyses included measures of total muscle volume and the circumference and diameter at 6 points along the length of the muscle. Differences between groups were analyzed using independent sample Mann-Whitney U-Tests (α < 0.05). Significant differences between groups were noted for measures of muscle volume, circumference at the origin and insertion, anterior-posterior diameter at the origin and midline, and superior-inferior diameter at the point of insertion into the velum and midline. Differences in measures at other points along the levator muscle belly were not statistically significant. Limited sample size and gender differences may have impacted statistical findings. Overall, the levator muscle in adults with repaired cleft palate is significantly different than that of adults with non-cleft anatomy. This study demonstrates the successful implementation of a method for 3D analysis of velopharyngeal (VP) musculature with potential clinical utility given continued technological advancements in MRI. Continued evaluation of pre- and post-surgical anatomy and short- and long-term outcomes may contribute to a better understanding of the effects of various types of palatoplasties on levator structure, which is important to VP function for speech.
INTRODUCTION
The levator veli palatini (levator) muscle is widely accepted to be the predominant muscle for velar elevation.1–2 In individuals with typical anatomy, the levator muscle originates from the skull base near the apex of the petrous portion of the temporal bone.3 The levator muscle courses across the middle one-third of the velum with interdigitating muscle fibers at the velar midline and no septum separating the two muscle bundles.4 Past studies have demonstrated a relatively consistent size, shape, and location of the levator muscle in individuals with non-cleft anatomy.4–6
Differences in musculature within the velopharyngeal (VP) mechanism have been studied between individuals with cleft palate and those with non-cleft anatomy. Ha et al7 observed variable levator muscle length and thickness among a group of four adult males with repaired cleft palate. Measures of distance between points of levator origin, levator muscle length, and levator muscle thickness were smaller than those observed in adults with non-cleft anatomy, as described by Ettema et al.5 Tian et al8 noticed that the levator muscle was thinner in children with repaired cleft palate as compared to those with non-cleft anatomy.
Nyswonger JC, Perry JL, Kuehn DP, et al (unpublished data, 2016) found no statistically significant differences in the levator muscle between adults with cleft palate and adults with non-cleft anatomy using linear measure analysis methods. However, qualitative differences of midline separation and muscle shape irregularities were reported, such as separation and/or thinning of the levator muscle at the velar midline. Nyswonger JC, Perry JL, Kuehn DP, et al (unpublished data, 2016) proposed that a more complex methodology employing measures of circumference and diameter along the course of the muscle, as described by Perry et al,9 and volumetric analyses may enable more sensitive examination of muscular differences between cleft and non-cleft anatomy.
The purpose of this study was to examine differences in the levator muscle volume, circumference, and diameter between adults with repaired cleft palate and adults with non-cleft anatomy. Perry et al9 indicated that understanding levator muscle morphology could provide important information into muscle function for abnormal VP control for speech and swallowing. It was hypothesized that adult participants with repaired cleft palate would present with significant differences in levator muscle morphology.
METHODS
Participants
In accordance with the local Institutional Review Boards, 15 English-speaking adults were recruited to participate in this study. Five of the participants had a history of repaired cleft palate and were consecutively enrolled. Ten participants were then selected from a normative database6 that were within the same age range as those with repaired cleft palate. The cleft palate group included 2 males and 3 females with a mean age of 25.7 years, while the group with non-cleft anatomy contained 10 males with a mean age of 23.8 years. Of the participants with repaired cleft palate, 3 had bilateral complete cleft lip and palate (subjects 1–3), and the remaining 2 had cleft palate only (subjects 4–5). All reported primary palate repair between the ages of 8–18 months. All participants underwent a Wardill-Kilner (straight line) primary palate repair surgery by different surgeons. Reported surgical information indicated no radical dissection around the hamulus and details of the levator muscle bundle overlap were not provided in any surgical reports. All but one of the participants with repaired cleft palate were judged to have resonance within normal limits. The participant with abnormal resonance was rated as having moderate-to-severe hypernasality. None of the participants had a pharyngoplasty at the time of the magnetic resonance imaging (MRI). Comparisons between groups were performed since the VP muscles are contained within the cranium. Using methods previously described by Tian and Redett10 and Tian et al,8,11 cranial index measures were obtained, and no significant differences were noted between the cleft and noncleft groups.
Magnetic Resonance Imaging
A Siemens 3 Tesla Trio (Erlangen, Germany) MRI scanner and a 12-channel Siemens Trio head coil were used to scan participants while lying in the supine position. The imaging protocol is also consistent with that used in previous MRI investigations of the VP muscles.9 An elastic strap attached to the head coil was used to stabilize the head during the scan to reduce motion artifact that negatively influence image quality. Participants were instructed to breathe through their nose, and images were collected at rest with the velum in a fully lowered position, resting on the tongue base.
Image Analysis
Image-processing methods were consistent with previous studies9,12–14 (also Nyswonger JC, Perry JL, Kuehn DP, et al, unpublished data, 2016). Specifically, raw magnetic resonance images were transferred into Amira 6.0.1 Visualization and Volume Modeling Software (Mercury Company Systems, Inc, Chelmsford, MA), which includes a native Digital Imaging and Communications in Medicine support program to ensure that anatomical geometry is maintained. The entire data set was resampled from the three-dimensional (3D) anatomical scan to obtain the oblique coronal image. This view allows the full sling of the levator muscle to be visualized. The levator muscle fibers were defined by segmentation of successive oblique coronal images using a paintbrush tool, and a voxel set was created to obtain volumetric analyses of the total muscle.
The voxel set was imported into Maya 8.5 (Autodesk, Ontario, Canada) for analysis of circumference and diameter through methods described by previous literature.9 Each participant’s right muscle bundle was measured, as there was little difference between levator muscle length for the right and left muscle bundles. A curve-vector arc tool was utilized to create 6 outlines perpendicular to the long axis of the muscle bundle. Due to the imperfect cylindrical shape of the levator, 8–10 vectors were placed around the model outline so they could be manually positioned against the model’s surface. The 6 landmarks were selected based on successful analysis of levator circumference and diameter of non-cleft participants completed by Perry et al.9 After measuring total muscle circumference, the outlines were then moved to a flat surface plane within the Maya software. Two diameter measures were taken to reflect the cylindrical shape for analysis of the total muscle. The anterior-posterior (A-P) diameter was generally the larger diameter. The smaller diameter has two directional names dependent on the location of the measurement due to the levator’s curvilinear form, medial-lateral (M-L) in the extravelar segment (points 1–3) and superior-inferior (S-I) in the intravelar segment (points 4–6). See Figure 1 for measures of interest and diameter illustrations.
FIGURE 1.
Image of the levator muscle displayed in Maya. The 6 points along the length of the muscle are shown as lines perpendicular to the muscle. As previously described by Perry et al,9 the 6 points include: (1) origin of the muscle, (2) halfway between origin and velum, (3) halfway between measure 2 and 4, (4) point where levator inserts into the velum, (5) halfway between measure 4 and midline of muscle at velum, and (6) midline insertion within the velum.
Statistical Analysis
Mann-Whitney U-Tests (α < .05) for independent samples were conducted to analyze differences in total levator muscle volume, circumference, and diameter across each of the 6 points using SPSS 20.0 (IBM Corp, Armonk, NY). An un-corrected p value was employed for between-group comparisons. Nonparametric statistical analyses allowed for quantitative analyses of measures between the cleft and non-cleft anatomy groups at rest given outliers and a small sample size. Descriptive statistics, including the median, were also given due to presence of outliers.
RESULTS
Total Volume of the Levator Muscle
Total levator muscle volume for participants with repaired cleft palate (Median = 1264.27 mm3, Mean = 1247.50 mm3, SD = 197.19 mm3) was significantly (U = 8, p = .040) smaller than that observed for participants with non-cleft anatomy (Median = 1646.23 mm3, Mean = 1855.90 mm3, SD = 653.68 mm3). The non-cleft group had more variability, as noted by the larger standard deviation, but there were no outliers.
Circumference of the Levator Muscle
Table 1 shows group medians, means, and standard deviations for levator circumference for both study groups along 6 points of the muscle bundle. Figure 2 depicts the mean circumference of the levator muscle along the 6 specific data points. At point 1 (muscle origin at the base of the skull), levator circumference for participants with repaired cleft palate was significantly (U = 4, p = .027) less than that observed for non-cleft anatomy. At point 6 (the midline), levator circumference for participants with repaired cleft palate was significantly (U = 7, p = .028) less than that observed for non-cleft anatomy. All other points were not significant. The greatest difference in mean circumference for consecutive points (7.44 mm) was noted between point 5 (Mean = 20.84 mm) and point 6 (Mean = 13.40 mm), which is evidence of midline dehiscence.
TABLE 1.
Circumference shown (in mm) at 6 points along the length of the levator muscle for cleft participants. Mean, standard deviation (in parentheses), and median shown for cleft and non-cleft groups.
| Cleft | ||||||
|---|---|---|---|---|---|---|
| Subject | 1 | 2 | 3 | 4 | 5 | 6 |
| 1 | 10.69 | 22.82 | 15.49 | 17.07 | 19.05 | 12.31 |
| 2 | 16.19 | 19.46 | 20.49 | 21.16 | 21.73 | 14.85 |
| 3 | 15.35 | 20.71 | 19.83 | 19.47 | 20.92 | 2.62 |
| 4 | 16.67 | 20.57 | 20.07 | 16.49 | 18.70 | 15.35 |
| 5 | 16.74 | 24.19 | 23.05 | 26.09 | 23.77 | 21.88 |
| Mean/SD | 15.13(2.5) | 21.55(1.9) | 19.79(2.7) | 20.06(3.9) | 20.84(2.1) | 13.40(7.0) |
| Median | 16.19 | 20.71 | 20.07 | 19.47 | 20.92 | 14.85 |
| Non-Cleft | ||||||
| Mean/SD | 18.90(2.6) | 22.40(4.9) | 22.76(4.0) | 22.02(3.6) | 21.96(5.3) | 23.71(6.5) |
| Median | 18.39 | 21.23 | 21.315 | 20.87 | 22.345 | 22.57 |
FIGURE 2.
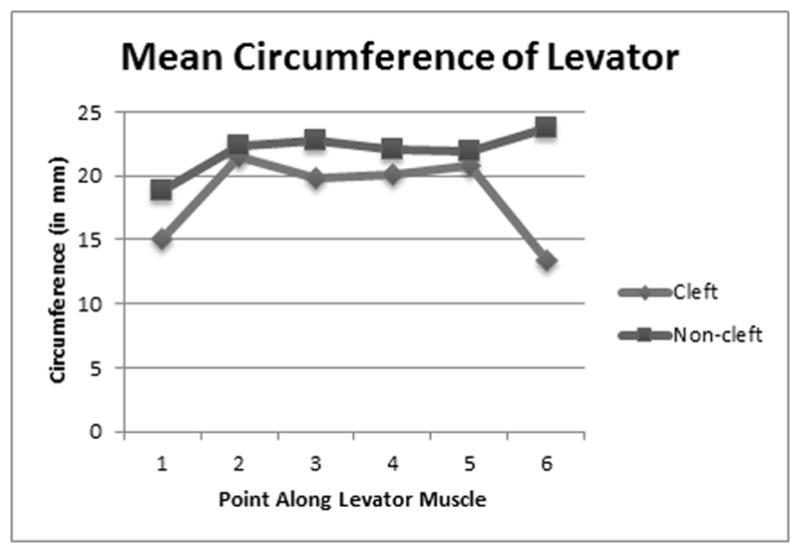
Mean circumference shown (in mm) at 6 points along the length of the levator muscle for cleft and non-cleft participants.
Diameter of the Levator Muscle
Difference in A-P diameter at point 1 was significant (U = 4, p = .008) between the repaired cleft palate and non-cleft groups (Table 2). At point 6 (the midline), A-P diameter for participants with repaired cleft palate was significantly (U = 5, p = .013) smaller than that observed for non-cleft anatomy. All other points were not significant. Similar to the circumference measures, the greatest difference in mean A-P diameter measures for consecutive points was noted between points 5 and 6 for the cleft group (3.3 mm). Figure 3 depicts the A-P diameter of the levator broken down into the 6 specific data points.
TABLE 2.
The larger diameter, anterior-to-posterior (A-P), and the smaller diameter, medial-to-lateral (M-L) and superior-to-inferior (S-I), shown (in mm) at 6 points along the length of the levator muscle for cleft participants. Mean, standard deviation, and median shown for cleft and non-cleft groups.
| Cleft | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |||||||
| Subject | A-P | M-L | A-P | M-L | A-P | M-L | A-P | S-I | A-P | S-I | A-P | S-I |
| 1 | 3.4 | 2.6 | 8.8 | 5.0 | 5.7 | 3.7 | 7.3 | 2.6 | 7.2 | 3.9 | 5.0 | 2.3 |
| 2 | 6.3 | 3.8 | 6.8 | 4.9 | 7.7 | 4.9 | 8.6 | 2.9 | 9.6 | 3.3 | 5.7 | 2.8 |
| 3 | 6.1 | 3.3 | 8.1 | 4.3 | 8.0 | 3.9 | 8.4 | 3.8 | 8.4 | 3.6 | 0.9 | 0.9 |
| 4 | 7.2 | 2.3 | 7.4 | 5.2 | 7.5 | 4.7 | 6.2 | 3.9 | 7.2 | 3.1 | 5.2 | 2.7 |
| 5 | 4.8 | 3.6 | 9.8 | 5.7 | 9.9 | 4.2 | 9.3 | 3.4 | 8.7 | 3.8 | 7.5 | 1.8 |
| Mean/SD | 5.6(1.5) | 3.1(0.6) | 8.2(1.2) | 5.0(0.5) | 7.8(1.5) | 4.3(0.5) | 8.0(1.2) | 3.3(0.6) | 8.2(1.0) | 3.6(0.6) | 4.9(2.4) | 2.1(0.8) |
| Median | 6.1 | 3.3 | 8.1 | 5.0 | 7.7 | 4.3 | 8.4 | 3.4 | 8.4 | 3.6 | 5.2 | 2.3 |
| Non-Cleft | ||||||||||||
| Mean/SD | 7.9(1.2) | 3.1(0.7) | 8.3(2.2) | 4.4(1.2) | 9.2(1.7) | 4.1(1.0) | 8.7(1.8) | 4.2(0.8) | 8.8(2.6) | 3.8(1.1) | 9.6(3.5) | 3.6(1.1) |
| Median | 7.6 | 3.15 | 8.9 | 4.4 | 8.9 | 3.8 | 8.8 | 4.15 | 8.8 | 3.6 | 9.3 | 3.5 |
FIGURE 3.

Mean A-P diameter shown (in mm) at 6 points along the length of the levator muscle for cleft and non-cleft participants.
Difference in S-I diameter was significant (U = 8, p = .040) at point 4 (levator insertion into the velum) between the repaired cleft palate and non-cleft groups. Difference in S-I diameter was also significant (U = 5, p = .013) at point 6 (midline). All other points were not significant. The greatest difference in mean side-side diameter measures for consecutive points was noted between points 1 and 2 for the cleft individuals (1.9 mm). Figure 4 depicts the side-side diameter of the levator broken down into the 6 specific data points.
FIGURE 4.

Mean M-L and S-I diameter shown (in mm) at 6 points along the length of the levator muscle for cleft and non-cleft participants.
Reliability
Pearson product correlation was used to obtain inter- and intra-rater reliability measures. A random sample of 40% of the data were considered for reliability. Intra-rater reliability was r = .80, which was calculated using separate measurements completed by 2 investigators with experience in 3D MRI data analyses using volumetric measurements. Inter-rater reliability was r = 1.00 for volumetric measures.
DISCUSSION
Using linear analysis measures, Nyswonger JC, Perry JL, Kuehn DP, et al (unpublished data, 2016) found no statistically significant difference in the levator muscle between adults with repaired cleft palate and adults without cleft palate but described qualitative differences in the muscle form. This study aimed to use a morphologic approach to quantify these observations using 3D measures of volume, circumference, and diameter. In the present study, total volume of the levator muscle in adults with repaired cleft palate was found to be significantly reduced compared to noncleft anatomy. These results support our hypothesis that adult participants with repaired cleft palate present with significant differences in levator muscle morphology.
Based on the present study, it was evident that the largest discrepancy between repaired cleft and non-cleft levator anatomy existed at the velar midline (point 6). Two participants in the repaired cleft group, both with bilateral cleft lip and palate, exhibited a midline levator muscle dehiscence to some extent, which is also consistent with previous literature.7 (also Nyswonger JC, Perry JL, Kuehn DP, et al, unpublished data, 2016). The participants in the present study all underwent a Wardill-Kilner palatoplasty15 without radical dissection around the hamulus. Surgical reports did not provide detail about the use of levator muscle overlapping techniques. It is possible that without adequate repositioning of the levator and overlap of the levator muscle fibers in the velar midline, as performed in the double opposing Z-plasy,16 contraction of the levator muscle may cause the two bundles to pull apart and separate at the midline. Over time, this repeated action may impact the positioning of the two muscle bundles, displacing them more laterally, as seen by the dehiscence among 2 of the participants in the present study. It is also possible that dissection around the hamulus provides greater release of the anterior velar muscles and creates a more normalized placement of the levator muscular sling. Additionally, most all subjects had very thin midline bundles, which likely contributed to our findings. Future studies should investigate the levator morphology as a function of surgery type to determine if overlapping techniques16–18 produce a more uniform cohesive midline levator sling. Furthermore, it is not known whether overlapping the muscle produces a greater midline bulk more similar to that of the non-cleft anatomy.
Research has shown that the Furlow double opposing Z-plasty is a successful secondary surgical option to improve speech in individuals who have already undergone a primary palate repair, indicating that replacement and overlapping of the levator muscle improves speech outcomes.18 Due to the small sample size and within group variability in this study, we were not able to assess the degree of contribution point 6 had to the overall measurements of volume, circumference, and diameter. However, it is indisputable that the varying degree of midline deficiency observed in all of the 5 participants played a significant role in the observed morphological differences found in the present study. Longitudinal studies and computational modeling may help us understand the effects of surgical techniques and corresponding outcomes on anatomy.
Previous literature has described the levator muscle as a flattened cylinder that fans out upon entering the intravelar segment.19–21 Perry et al9 quantified this shape in adults with normal anatomy using 3D analysis of magnetic resonance images. In the present study, the muscle in the cleft group exhibited a similar shape with the exception of the midline, regardless of whether muscular dehiscence was present. Throughout the extravelar segment (points 1–3), similar measurements were noted between the cleft group in this study and non-cleft anatomy in the literature9,19–21 with the exception of smaller mean circumference and A-P diameter at the muscle origin (point 1).
Previous studies of noncleft anatomy observed a broadening of muscle fibers at the insertion of the levator muscle into the velum22–26 and greater variation in thickness across the intravelar segment (points 4–6).9 In the present study, consistency in circumference and A-P diameter was observed for cleft anatomy across points 3–5. There was less consistency in S-I diameter for these points, specifically at point 4. The largest difference between cleft and non-cleft anatomy was observed at measurement point 6 (midline of the levator). Perry et al9 reported the largest mean circumference (23.71 mm) and A-P diameter (9.6 mm) measures to be at midline non-cleft anatomy, whereas the cleft group showed the smallest mean circumference (13.40 mm), A-P diameter (4.86 mm), and S-I diameter (2.08 mm) in this study. Midline difference in the cleft group was not only impacted by the 2 participants with muscular dehiscence, but also the thinness of the muscle across all participants with repaired cleft palate. Overall, variation in thickness and overlap of muscle bundles was observed in the repaired cleft palate group; however, this did not correspond with variations in resonance as expected.
It is important to note that the speech of the 2 individuals with midline dehiscence was within normal limits. Although velopharyngeal dysfunction (VPD) occurs secondary to various changes within the complex VP mechanism, muscle dehiscence has been associated with increased incidence of VPD. Surprisingly, the participant with moderate-severe hypernasality did not display any degree of midline separation but did have a very thin muscle at the velar midline, with circumference and A-P diameter measures greater than one SD below the mean for non-cleft individuals. This finding highlights the importance of investigating other VP variables in addition to the levator variables of the present study. It is well known that VP function is related to the coordination of multiple muscular actions. Additionally, the VP portal dimensions contribute to VP function. Future studies should investigate a potential relationship between 3D levator muscle measures and presence of hypernasality with a larger sample of participants with VPD. Inoyue et al27 effectively demonstrated through computational modeling that when the levator was not connected at midline, the least amount of velar force was generated, suggesting overlap is a critical feature of levator physiology. In the future, more complex computational modeling including additional VP musculature may be an effective tool to investigate questions related to VP function given variations in the morphology of additional muscles. Since the VP muscles work together as a cohesive mechanism, it is possible that a deficit in the levator muscle could be compensated for by the function of other muscles, resulting in little to no speech difference.
The present study emphasizes the need for long-term surgical follow up after palatoplasty. Kuehn et al28 proposed questions regarding the fate of the levator muscle following surgery and emphasized the need for pre- and post-surgical MRI evaluation. Given the adult population utilized in this study, these participants were decades past their initial palate repair, and it is impossible to know where the levator was placed during surgery and whether it migrated to a less favorable position. Future studies should employ a longitudinal design to determine levator morphology within the cleft palate population over time to better understand the effects the healing and aging processes have on the muscle.
Limitations
Findings from the present study are most limited by the small sample size (N=15). Future studies should employ a larger sample size in order to make these comparisons of location along the levator between cleft and non-cleft participants. Other limitations of this study include unmatched treatment groups. Perry et al29 found significant differences between Caucasian men and women across several two-dimensional levator muscle measures. This may explain some of the variability seen within the 3D muscle measures of this study.
Conclusions
Results of this study indicate that adults with repaired cleft palate exhibit decreased levator muscle volume, circumference, and diameter as compared to adults with normal anatomy. This study contributes to the research base to further our understanding into muscle function for abnormal VP control for speech and swallowing, as emphasized by Perry et al.9 Further MRI studies are needed to assess these differences in levator muscle morphology in a more clinically relevant population, such as children with cleft palate. Detailed analyses should be performed using the 6 landmarks designated by Perry et al.9 Pre- and post-operative analyses of levator morphology will be crucial to understanding how surgery can optimize levator muscle form and function.
Acknowledgments
This study was made possible by grant number 1R03DC009676–01A1 from the National Institute on Deafness and Other Communicative Disorders. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
“The authors wish to thank Dr. David Kuehn and Dr. Bradley Sutton at the University of Illinois at Urbana-Champaign for their contribution to data collection”
References
- 1.Kuehn DP, Moller KT. Speech and language issues in the cleft palate population: the state of the art. Cleft Palate Craniofac J. 2000;37:348–1348. [Google Scholar]
- 2.Ha S. The levator veli palatini muscle in cleft palate anatomy and its implications for assessing velopharyngeal function: a literature review. Korean J Commun Disord. 2007;12:77–89. [Google Scholar]
- 3.Kuehn DP, Perry JL. Anatomy and physiology of the velopharynx. In: Losee JE, Kirschner RE, editors. Comprehensive Cleft Care. New York: McGraw-Hill; 2009. pp. 557–567. [Google Scholar]
- 4.Kuehn DP, Moon JB. Histologic study of intravelar structures in normal human adult specimens. Cleft Palate Cranio J. 2005;42:481–489. doi: 10.1597/04-125r.1. [DOI] [PubMed] [Google Scholar]
- 5.Ettema SL, Kuehn DP, Perlman AL, et al. Magnetic resonance imaging of the levator veli palatini muscle during speech. Cleft Palate Cranio J. 2002;39:130–144. doi: 10.1597/1545-1569_2002_039_0130_mriotl_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 6.Perry JL, Kuehn DP, Sutton BP, et al. Anthropometric analysis of the velopharynx and related craniometric dimensions in three adult populations using MRI. Cleft Palate Cranio J. 2016;53:e1–e13. doi: 10.1597/14-015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ha S, Kuehn DP, Cohen M, et al. Magnetic resonance imaging of the levator veli palatini muscle in speakers with repaired cleft palate. Cleft Palate Cranio J. 2007;44:494–501. doi: 10.1597/06-220.1. [DOI] [PubMed] [Google Scholar]
- 8.Tian W, Yin H, Redett RJ, et al. Magnetic resonance imaging assessment of the velopharyngeal mechanism at rest and during speech in Chinese adults and children. J Speech Hear Res. 2010;53:1595–1615. doi: 10.1044/1092-4388(2010/09-0105). [DOI] [PubMed] [Google Scholar]
- 9.Perry JL, Kuehn DP, Sutton BP. Morphology of the levator veli palatini muscle using magnetic resonance imaging. Cleft Palate Cranio J. 2013;50:64–75. doi: 10.1597/11-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tian W, Redett RJ. New velopharyngeal measurements at rest and during speech: implications and applications. J Cranio Surg. 2009;20:532–539. doi: 10.1097/SCS.0b013e31819b9fbe. [DOI] [PubMed] [Google Scholar]
- 11.Tian W, Li Y, Yin H, et al. Magnetic resonance imaging assessment of velopharyngeal motion in Chinese children after primary palatal repair. J Cranio Surg. 2010;21:578–587. doi: 10.1097/SCS.0b013e3181d08bee. [DOI] [PubMed] [Google Scholar]
- 12.Perry J, Kuehn D. Three-dimensional computer reconstruction of the levator veli palatini muscle in situ using magnetic resonance imaging. Cleft Palate Craniofac J. 2007;69:214–216. doi: 10.1597/06-137.1. [DOI] [PubMed] [Google Scholar]
- 13.Perry JL, Kuehn DP. Magnetic resonance imaging and computer reconstruction of the velopharyngeal mechanism. J Craniofac Surg. 2009;20:1739–1746. doi: 10.1097/SCS.0b013e3181b5cf46. [DOI] [PubMed] [Google Scholar]
- 14.Perry JL, Kuehn DP, Sutton BP, et al. Craniometric and velopharyngeal assessment of infants with and without cleft palate. J Craniofac Surg. 2011;22:499–503. doi: 10.1097/SCS.0b013e3182087378. [DOI] [PubMed] [Google Scholar]
- 15.Wardill WEM. The technique of operation for cleft palate. Br J Surg. 1937;25:117–130. [Google Scholar]
- 16.Furlow LT., Jr Cleft palate repair by double opposing Z-plasty. Plast Reconstr Surg. 1986;78:724–738. doi: 10.1097/00006534-198678060-00002. [DOI] [PubMed] [Google Scholar]
- 17.Nyguyen DC, Patel KB, Woo AS. A new technique to improve velopharyngeal dysfunction by combining the radical intravelar veloplasty and overlapping intravelar veloplasty for primary palatoplasty. Plast Reconstr Surg. 2016 Feb 15; doi: 10.1097/PRS.0000000000002205. [DOI] [PubMed] [Google Scholar]
- 18.Chen PK, Wu JTH, Chen Y, et al. Correction of secondary velopharyngeal insufficiency in cleft palate patients with the Furlow palatoplasty. Plast Reconstr Surg. 1994;94:933–941. [PubMed] [Google Scholar]
- 19.Azzam NA, Kuehn DP. The morphology of musculus uvulae. Cleft Palate J. 1977;14:78–87. [PubMed] [Google Scholar]
- 20.Kuehn DP, Azzam NA. Anatomical characteristics of palatoglossus and the anterior faucial pillar. Cleft Palate J. 1978;15:349–359. [PubMed] [Google Scholar]
- 21.Huang MH, Lee ST, Rajendran KA. A fresh cadaveric study of the paratubal muscles: implications for eustachian tube function in cleft palate. Plast Reconstr Surg. 1997;100:833–842. doi: 10.1097/00006534-199709001-00003. [DOI] [PubMed] [Google Scholar]
- 22.Dickson DR, Grant JC, Sicher H, et al. Status of research in cleft palate anatomy and physiology. Cleft Palate J. 1974;11:471–492. [PubMed] [Google Scholar]
- 23.Boorman JG, Sommerlad BC. Levator palate and palatal dimples: their anatomy, relationship and clinical significance. Br J Plast Surg. 1985;38:326–332. doi: 10.1016/0007-1226(85)90236-x. [DOI] [PubMed] [Google Scholar]
- 24.Kuehn DP, Kahane JC. Histologic study of the normal human adult soft palate. Cleft Palate J. 1990;27:26–34. doi: 10.1597/1545-1569(1990)027<0026:hsotnh>2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 25.Carrasco VN. Management of middle ear disease and malformations. In: Turvey TA, Vi KWL, Fonesca RJ, editors. Facial Clefts and Craniosynostosis. Philadelphia: WB Saunders; 1996. pp. 213–221. [Google Scholar]
- 26.Huang MH, Lee ST, Rajendran KA. Anatomic basis of cleft palate and velopharyngeal surgery: implication from a fresh cadaveric study. Plast Reconstr Surg. 1998;101:613–627. doi: 10.1097/00006534-199803000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Inouye JM, Pelland CM, Lin KY, et al. A computational model of velopharyngeal closure for simulation cleft palate repair. J Craniofac Surg. 2015;26:658–662. doi: 10.1097/SCS.0000000000001441. [DOI] [PubMed] [Google Scholar]
- 28.Kuehn DP, Ettema SL, Goldwasser MS, et al. Magnetic resonance imaging of the levator veli palatini muscle before and after primary palatoplasty. Cleft Palate Craniofac J. 2004;41:584–592. doi: 10.1597/03-060.1. [DOI] [PubMed] [Google Scholar]
- 29.Perry JL, Kuehn DP, Sutton BP, et al. Sexual dimorphism of the levator veli palatini muscle: an imaging study. Cleft Palate Cranio J. 2014;51:544–552. doi: 10.1597/12-128. [DOI] [PMC free article] [PubMed] [Google Scholar]



