Abstract
Background
Assisted living is a popular option for housing and long-term care.
Objective
To develop and test a methodology to identify Medicare beneficiaries residing in assisted living facilities.
Research Design
We compiled a finder file of 9-digit ZIP codes representing large assisted living facilities (ALFs) (25+ beds) by matching Outcome and Assessment Information Set (OASIS) assessments and Medicare Part B Claims to the Medicare enrollment records and addresses of 11,751 ALFs. Using this finder file, we identified 738,567 beneficiaries residing in validated ALF ZIP codes in 2007–2009. We compared characteristics of this cohort to those of ALF residents in the National Survey of Residential Care Facilities (NSRCF; n=3009), a sample of community-dwelling Medicare beneficiaries (n=33,025,690), and long-stay nursing home residents (n= 1,287,572).
Data Sources
A national list of licensed ALFs, Medicare enrollment records, and administrative healthcare databases.
Results
The ALF cohort we identified had good construct validity based on their demographic characteristics, health, and healthcare utilization when compared to ALF residents in the National Survey of Residential Care Facilities (NSRCF), community-dwelling Medicare beneficiaries, and long-stay nursing home residents.
Conclusions
Our finder file of 9-digit ZIP codes enables identification of ALF residents using administrative data. This approach will allow researchers to examine questions related to the quality of care, healthcare utilization, and outcomes of residents in this growing sector of long-term care.
Keywords: Assisted Living Facilities, Medicare, National Survey of Residential Care Facilities, ZIP codes
INTRODUCTION
Over the past two decades, assisted living has rapidly emerged as a housing and long-term care (LTC) option for older adults. In 2012, assisted living facilities (ALFs) provided a home to over 710,000 older Americans each day(1). Assisted living has been defined by the Joint Commission on Accreditation of Healthcare Facilities as “a congregate residential setting that provides or coordinates personal services, 24-hour supervision and assistance (scheduled and unscheduled), activities, and health related services”(2). Despite the large numbers of Americans residing in ALFs, the development and growth of the industry has occurred without the influence of federal financing or federal regulation resulting in less monitoring and fewer reporting requirements than other healthcare settings such as nursing homes(3). Although ALFs are regulated by states, the stringency of these regulations varies markedly by state, likely resulting in variations in quality of care(4).
Given that ALFs do not routinely submit Medicare claims for services or resident assessments as are required for nursing home residents, rehabilitation patients, and home health recipients, researchers and policy-makers have no reliable methodology for studying the health and healthcare utilization of ALF residents. Although there have been a few studies of ALFs and the care provided to residents, they have been limited to small samples and have primarily been cross-sectional(4–12). We currently do not have systematic knowledge, on a national level, of who enters ALFs, what type of care they receive, what their health outcomes are, and how this varies among facilities. Therefore, a first critical step for better understanding this growing demographic is to identify Medicare beneficiaries who reside in ALFs.
The purpose of this study was to develop and test a novel methodology to identify residents in large ALFs using secondary data sources, specifically the 9-digit ZIP code reported in Medicare enrollment records. In this paper, we report on the utility of the 9-digit ZIP code in identifying ALF residents using the ZIP codes of subsamples of ALF residents (i.e., identified in routinely collected Home Health assessment data and Medicare Part B claims). We then compare characteristics of the identified ALF residents to those of residents from the National Survey of Residential Care Facilities and the national population of community-dwelling older adults and long-stay nursing home residents.
METHODS
Identifying a Cohort of ALF Residents
Creating a National List of Licensed Assisted Living Facilities
Data on ALFs come from a national list of licensed residential care facilities (i.e., facilities that are licensed, registered, listed, certified, or otherwise regulated by the states) operating in 2007 and/or 2008. The list of residential care facilities, their addresses, and their size (i.e., number of beds) were compiled separately from individual state licensing agencies by the authors and checked for duplicates before being concatenated to form a list of residential care facilities for each state. States include a wide range of licensure categories for congregate residential facilities (e.g., residential care facilities, assisted living facilities, community living arrangements, adult family care homes, and personal care homes). Therefore, following the work of others(13, 14), we defined “assisted living facility” as a facility that was licensed to serve mainly an elderly population and that had 25 or more licensed beds. Using this definition for ALFs, we identified 11,751 unique ALFs operating in 2007 and/or 2008 and obtained their 9-digit ZIP codes by matching their addresses to the Archived United States (US) Postal Service ZIP+4 Product File.
Identifying ZIP Codes of Patients Receiving Home Health or Medicare Part B-Covered Services in ALFs
We linked the Medicare Denominator File to the Outcome and Assessment Information Set (OASIS) and the Medicare Carrier File to obtain Medicare beneficiaries’ 9-digit ZIP codes. The Denominator File combines all Medicare beneficiaries’ entitlement status information, demographic information, Medicare coverage information, dual-eligibility status, and also provides their 9-digit ZIP code. This 9-digit ZIP code is based upon the mailing address used for sending cash benefits to the beneficiary or for other reporting purposes (e.g., premium billing) and represents where the person lived in December of the reference year.
The Outcome and Assessment Information Set (OASIS) is the instrument/data collection tool used to collect and report performance data by home health agencies. Centers for Medicare & Medicaid Services (CMS) requires Medicare-certified home health agencies to collect OASIS data for all patients. Important to our study in the OASIS documentation, providers indicate the recipient’s Place of Residence with an option being “Board and Care or Assisted Living.” Using the start of care assessments and the Place of Residence code, we identified 465,722 unique individuals receiving home health in Board and Care or Assisted Living in 2007 through 2009.
The Carrier file (also known as the Physician/Supplier Part B claims file) contains claims submitted on a CMS-1500 claim form. Most of the claims are from non-institutional providers, such as physicians, physician assistants, nurses, clinical social workers, and nurse practitioners. This file includes diagnosis and procedure codes, dates of service, reimbursement amounts, provider numbers, beneficiary demographic information and important to this study, a Place of Service (POS) Code to identify where services were provided(15, 16). We selected claims with POS code #13 in item 24b to identify Medicare beneficiaries receiving care provided in an ALF. Using a 20% random sample for 2007–2009, we identified 122,038 unique individuals with a Part B claim for services received in an ALF.
Approach to Creating a List of Validated 9-Digit ZIP Codes Representing an ALF
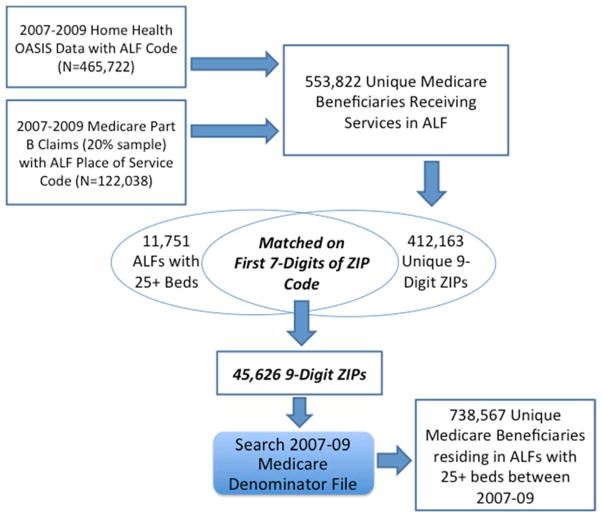
A 9-digit ZIP code uses the basic five-digit code plus four additional digits to identify a geographic segment within the five-digit delivery area, such as a city block, a group of apartments, an individual high-volume receiver of mail or any other unit that could use an extra identifier to aid in efficient mail sorting and delivery. The sixth and seventh digits of a 9-digit ZIP code indicate a “delivery sector,” such as a group of streets, post office (P.O.) boxes, a group of buildings, or even a single high-rise building. The eighth and ninth digits designate a “delivery segment,” such as a specific side of a street, a floor in an office or apartment building, or a specific department within a large office. Therefore, it is plausible that one large ALF will contain multiple 9-digit ZIP codes for its residents. However, each ALF address in the national list of licensed residential care facilities can only be matched to one 9-digit ZIP code in the Archived US Postal Service ZIP+4 Product File. Because it is possible that many 9-digit ZIP codes represent one large ALF and we were interested in identifying a collection of 9-digit ZIP codes that represents ALF residents, we matched the first seven digits, the sector of Medicare beneficiaries ZIP codes (number of Medicare beneficiaries receiving home health or Part B services in ALFs = 553,822; number of unique ZIP codes among these 553,822 beneficiaries = 412,163), to the first seven digits of an ALF’s ZIP code (See Figure 1). We compiled the 9-digit ZIP codes of beneficiaries who matched to the first 7-digits of the ALF ZIP codes and included the 9-digit ZIP codes of ALFs to create a finder file of “validated 9-digit ZIP codes” (n=45,626). Using this finder file, we searched the Medicare Denominator File to identify all Medicare beneficiaries residing in the validated ALF 9-digit ZIP codes (See Figure 1).
Figure 1.
Method of Compiling an Assisted Living Facility Resident Finder File and Identifying Medicare Beneficiaries Residing in Large (25+ Beds) Assisted Living Facilities
Examining the Construct Validity of Our Cohort of ALF Residents
To test that the individuals we identified were representative of the population of ALF residents, we compared their characteristics (i.e., demographics, chronic conditions, and healthcare utilization) to a nationally representative sample of ALF residents from the 2010 public use file of the National Survey of Residential Care Facilities (NSRCF). Residential care facilities (RCFs) are another name for ALFs. The NSRCF used a stratified two-stage probability sample design. The first stage was the selection of RCFs from the sampling frame representing the universe of RCFs. For the 2010 NSRCF, 3,605 RCFs were sampled with probability proportional to facility size. Interviews were completed with 2,302 RCFs, for a first-stage, facility-level weighted response rate of 81%, which was weighted for differential probabilities of selection. In the second stage of sampling, 3–6 current residents were selected depending on RCF bed size. All data collected on sampled residents came from interviews with RCF staff who answered questions by referring to the residents’ records or their own knowledge of the residents. The second-stage, resident-level weighted response rate was 99%. A detailed description of NSRCF sampling design, data collection, and procedures is provided both in a previous report(8) and on the NSRCF website(17). For these analyses, we only included characteristics of residents age 65+ years in facilities with 25+ beds (n=3009). We calculated the demographic characteristics and chronic conditions of ALF residents age 65+ years in the NSRCF and compared them to our cohort of identified ALF residents. Weights were applied to the NSRCF data to provide national estimates.
We also compared the demographic characteristics, health, and healthcare utilization of our identified cohort of Medicare fee-for-service (FFS) ALF residents to that of community-dwelling Medicare beneficiaries and long-stay nursing home residents. Specifically, we selected from our identified cohort of ALF residents in 2008, those who were Medicare FFS and had not been enrolled in any Medicare Advantage plan in the year (N=434,239). Using the Residential History File methodology(18), we identified a sample of community-dwelling Medicare FFS beneficiaries in 2008 who had not been in a nursing home, hospital, or emergency room in the previous year (2007) and who did not have any Medicare Advantage coverage in 2008 (n=33,025,690). We also identified a cohort of long-stay nursing home residents defined as FFS Medicare beneficiaries who had been in a nursing home for greater than 90 days at any point during 2008 and did not have any Medicare Advantage coverage during the year (n=1,287,572).
We calculated the descriptive characteristics of the Medicare FFS cohort of ALF residents, age 65+ years, including their age, race, gender, and enrollment status and compared that to the community-dwelling and long-stay nursing home resident populations. Using the chronic conditions listed in the Chronic Conditions Warehouse data, we calculated the number and type of chronic conditions and present those for each of the three cohorts of Medicare FFS beneficiaries.
RESULTS
With the finder file of validated 9-digit ZIP codes corresponding to an ALF, we identified in the denominator files a total of 548,009 Medicare beneficiaries with an ALF ZIP code in 2007, 539,182 in 2008, and 524,469 in 2009. This represented 738,567 unique Medicare FFS beneficiaries over the three-year period. By state, the number of Medicare beneficiaries we identified in 2008 relative to the number of ALF beds in 2007/2008 varied from over 90% in some (i.e., Connecticut, Illinois, Missouri, and Massachusetts) to less than 40% in others (i.e., Utah, North Carolina, Minnesota, Hawaii and Alaska).
The demographic characteristics of ALF residents identified in 2008 using the finder file are shown in Table 1. As compared to the characteristics of individuals in large ALFs in the NSRCF, we found that our cohort of residents age 65+ identified using the finder file were similar to residents age 65+ in the NSRCF in terms of age, race and gender. We also compared the prevalence of chronic conditions reported among Medicare FFS beneficiaries age 65+ identified in our cohort to those of residents age 65+ in the NSRCF (see Table 2). For many of the conditions (i.e., Alzheimer’s/dementia, asthma, depression, and stroke) the samples’ prevalence rates did not differ by more than <1 to 4.3 percentage points. However, the groups did markedly differ in reported congestive heart failure and hypertension.
Table 1.
Comparison of Identified Assisted Living Residents’ Demographic Characteristics to Residents’ Characteristics in the National Survey of Residential Care Facilities
| Beneficiaries Residing in Validated ALF ZIP Codes in 2008 (n=501,058) | ALF Residents in the 2010 NSRCF (n=3009) | |
|---|---|---|
| % | Weighted % (95%CL) | |
| Age Group 65–74 | 12.6 | 9.9 (8.7 – 11.0) |
| Age Group 75–84 | 31.3 | 30.6 (28.6 – 32.6) |
| Age Group 85+ | 56.1 | 59.5 (57.4 – 61.6) |
| Female | 71.6 | 71.9 (70.0 – 73.9) |
| White | 94.1 | 95.0 (94.2 – 95.8) |
| Black | 3.9 | 3.4 (2.7 – 4.1) |
Note. All residents are age 65 years or older. ALF = Assisted Living Facility with 25 or more beds; NSRCF = National Survey of Residential Care Facilities; CL = Confidence Limit for Weighted Percent
Table 2.
Comparison of Identified Medicare Fee-For-Service Assisted Living Facility Residents’ Chronic Conditions to Residents’ Conditions in the National Survey of Residential Care Facilities
| Medicare FFS Beneficiaries Residing in Validated ALF ZIP Codes in 2008 (N=370,693) | ALF Residents from the 2010 NSRCF (N = 3009) | |
|---|---|---|
| % | Weighted % (95%CL) | |
| Alzheimer’s Disease or Related Dementia | 41.4 | 45.6 (43.6 – 47.5) |
| Heart Attack/Acute Myocardial Infarction | 1.9 | 3.7 (2.9 – 4.5) |
| Asthma | 4.9 | 4.3 (3.4 – 5.1) |
| Heart Failure | 36.7 | 14.0 (12.6 – 15.5) |
| Chronic Obstructive Pulmonary Disease | 18.5 | 14.2 (12.8 – 15.6) |
| Depression | 26.1 | 25.6 (23.9 – 27.4) |
| Hypertension | 71.7 | 58.9 (56.9 – 60.8) |
| Stroke//Transient Ischemic Attack | 9.7 | 10.9 (9.6 – 12.3) |
Note. All residents are age 65 years or older. ALF = Assisted Living Facility with 25 or more beds; FFS = Medicare Fee-For-Service; NSRCF = National Survey of Residential Care Facilities; CL = Confidence Limits for Percent
Table 3 describes the health and healthcare utilization of the sample of Medicare beneficiaries residing in ALFs compared to those of community-dwelling older adults and long-stay nursing home residents in 2008. The cohort of FFS Medicare beneficiaries residing in ALFs that we identified have higher rates of hospitalization, nursing home utilization, and chronic conditions than community-dwelling beneficiaries and lower rates than the long-stay nursing home population. For example, the hospitalization rate for ALF residents at any time in 2008 was 36.3% compared to 9.4% of community-dwelling older adults and 48.6% of Medicare beneficiaries who were or became long-stay nursing home residents in 2008. This rate of hospitalization was similar to that observed in the NSRCF data (Weighted % = 37.6; 95% Confidence Limits = 35.6 – 39.7). Similarly, 46.6% of Medicare FFS ALF residents in our cohort had 6 or more chronic conditions compared to 9.6% of community-dwelling older adults and 64.1% of long-stay nursing home residents. The proportion of Medicare FFS ALF residents with a documented diagnosis of Alzheimer’s disease or dementia also tracks as expected: 38.9% of ALF residents compared to 3.5% of community-dwelling Medicare beneficiaries and 73% of long-stay nursing home residents.
Table 3.
Health and Healthcare Utilization of Medicare Fee-For-Service Beneficiaries in Assisted Living Facilities Compared to Community-Dwelling and Long-Stay Nursing Home Residents in 2008
| Community-Dwelling Medicare FFS Beneficiaries | Medicare FFS Beneficiaries Residing in Validated ALF ZIP Codes | Medicare FFS Long-Stay NH Residents | |
|---|---|---|---|
| N | 33,025,690 | 434,239 | 1,287,572 |
| Demographic Characteristics | |||
| Age 0–64 | 31.64 | 7.65 | 9.32 |
| Age 65–74 | 39.51 | 11.42 | 12.98 |
| Age 75–84 | 20.76 | 28.56 | 29.73 |
| Age 85+ | 8.09 | 52.37 | 47.98 |
| Female | 52.73 | 69.25 | 69.14 |
| White | 82.79 | 93.00 | 83.52 |
| Black | 9.69 | 4.75 | 12.06 |
| Dually-Eligible for Medicaid | 11.85 | 30.94 | 73.17 |
| Healthcare Utilization | |||
| Any Hospitalization | 9.35 | 36.29 | 48.56 |
| Any NH Stay | 0.01 | 34.37 | 100.00 |
| Chronic Conditions | |||
| At Least 3 Chronic Conditions* | 35.47 | 81.99 | 92.61 |
| At Least 6 Chronic Conditions* | 9.59 | 46.62 | 64.12 |
| Alzheimer’s/Related or Senile Dementia | 3.53 | 38.92 | 73.00 |
| Heart Attack/Acute Myocardial Infarction | 0.44 | 1.77 | 2.26 |
| Heart Failure | 6.61 | 34.46 | 47.64 |
| Chronic Obstructive Pulmonary Disease | 5.47 | 18.40 | 23.95 |
| Depression | 6.11 | 26.89 | 40.83 |
| Diabetes | 15.59 | 28.41 | 40.55 |
| Glaucoma | 6.84 | 13.04 | 7.98 |
| Stroke/Transient Ischemic Attack | 1.72 | 9.37 | 18.03 |
Note.
Number of conditions present out of the 26 reported in the Chronic Conditions Data Warehouse.
Samples include Medicare Fee-For-Service (FFS) Beneficiaries without any Medicare Advantage coverage in 2008.
Community-Dwelling Population identified as having no nursing home, hospital, or emergency room utilization in prior year (2007).
Assisted Living Facility Residents defined as having a validated ALF 9-digit ZIP code.
Long-Stay Nursing Home Residents are defined as having a length of stay in a nursing home for more than 90 days at any point during 2008.
DISCUSSION
Although the importance of characterizing the population of ALF residents has been appreciated for over 25 years(19), we know of no previously published approach that has been effective in identifying and describing a national population of ALF residents using secondary data. Our paper identifies a reliable and reproducible methodology, specifically the use of 9-digit ZIP codes, to identify ALF residents using secondary data. We validated our approach by comparing the demographic characteristics and chronic conditions of Medicare beneficiaries we identified as living in ALF ZIP codes to those of a nationally representative sample of ALF residents, finding that they were very similar. Furthermore, among the FFS sample of ALF residents, our results suggest that their health and healthcare utilization patterns fall in between those of community-dwelling and long-stay nursing home populations, as expected.
Moving forward, the approach we have created can be used by researchers to study a range of outcomes among a national population of ALF residents such as hospitalizations, inappropriate medication use, access to primary care, nursing home entry, and mortality. Indeed, we would assert that ALFs have been understudied relative to other long-term care settings, partly due to the gaps in data. By using the 9-digit ZIP codes to link Medicare data to these ALF residents, our data provides an important complement to smaller survey data such as the NSRCF. In addition, this approach would allow us to examine ALF provider quality of care with Medicare claims data because we would be able to ascribe Medicare beneficiaries to specific ALFs.
It is important to note that our methodological approach does not capture the entire universe of ALF residents: given that the total number of beds in large ALFs (>25 beds) in 2008 were 878,223, we potentially accounted for 57% of all licensed beds with our methodology. However, few large ALFs operate at 100% occupancy (only 13% are at 95% occupancy or greater, 36% operate between 80 and 95% occupancy, 27% between 65 and 80% occupancy, and 23% are operating at less than 65% occupancy(8)) and the NSRCF reports that 12% of residents in ALFs with 25+ beds are under the age of 65. Therefore, our estimate of identifying 57% of all licensed beds in large ALFs is a conservative estimate of the proportion of ALF residents that we were able to identify with our methodology.
Although we found that the ALF residents we identified were very similar to the nationally representative sample of ALF residents in the NSRCF in terms of age, gender, and race, they did vary quite markedly on some of their reported health conditions (e.g., congestive heart failure and hypertension). We believe this to be attributable to the way that chronic conditions are reported for both cohorts. In the Chronic Conditions Warehouse Data, Congestive Heart Failure is identified by having at least one inpatient, hospital outpatient, or carrier claim code with a heart failure diagnosis code in the last two years. Medicare FFS beneficiaries are identified as having hypertension if they have at least one inpatient, skilled nursing facility, home health agency or two hospital outpatient or carrier claims in the last year with a hypertension diagnosis code. In the NSRCF, residents’ health comes from staff report. Specifically, staff are handed a list of diagnoses and are asked “As far as you know, has a doctor or other health professional ever diagnosed [RESIDENT] with any of the following conditions?” Therefore, should a resident have controlled hypertension or congestive heart failure, it is possible that the staff member completing the survey is unaware of their history, thereby leading to potential underreporting.
Limitations
We were unable to identify a number of ALF residents with our methodology. Obviously, individuals in ALFs and not enrolled in the Medicare program will not be included as we rely on the Medicare Denominator File to identify our cohort. In addition, Medicare beneficiaries who are in an ALF for a short amount of time or who chose not to provide the Medicare program with their new address following a move to an ALF will not be identified by our finder file. Nevertheless, we believe that this is a relatively small percentage of all ALF residents as data suggests that the median length of stay in a residential care facility is 22 months(20) and mail is the primary means of contact between the Medicare program and beneficiaries. In addition, some individuals residing in ALFs may have their mail routed to a family member, their former residence, or in some cases that we found, a legal guardianship agency and therefore would not appear in our sample. Furthermore, we only had 20% of the Part B file so it is likely that some of the ZIP codes of the remaining 80% of Medicare beneficiaries receiving services in ALFs are not included in our ZIP code finder file. Regardless, we were able to confidently identify over 738,657 unique individuals residing in a 9-digit ZIP code that corresponded to a large ALF between 2007 and 2009.
Another potential limitation is that there may be some issues surrounding the accuracy of the OASIS and Part B place of service codes; however, it is important to point out that we are not testing the accuracy of the place of service codes, but compiling a list of “validated” 9-digit ZIP codes representing ALFs using a population of Medicare beneficiaries with an ALF place of service code. We recognize the need to conduct future research to assess the validity of our ZIP code methodology against gold standards that conclusively ascertain place of residence.
A limitation in testing the construct validity of our methodology was that we were unable to make direct comparisons to the patient population in the NSRCF. For example, we were unable to ascertain Medicare eligibility and enrollment in the sample from the NSRCF. Therefore, the comparison group of ALF residents in the NSRCF included beneficiaries enrolled in a Medicare Advantage plan and might account for some of the differences observed in the rates of chronic conditions. In addition, our cohort of identified ALF residents’ data come from 2008 and therefore might represent a somewhat different population than residents in the 2010 NSRCF. However, we have no reason to believe that the resident composition and characteristics of ALF residents changed dramatically between 2008 and 2010. Future work is needed to confirm this. In addition, to make comparisons among the cohort of ALF residents we identified, community-dwelling Medicare beneficiaries, and long-stay nursing home resident populations, we defined the groups as mutually exclusive with ALF residence taking priority. Although it is possible that a number of the 34.4% of Medicare beneficiaries residing in an ALF ZIP code and utilizing nursing home care in 2008 transitioned to become long-stay nursing home residents during the year, we did not include these individuals in our long-stay nursing home cohort. Therefore, the population of long-stay nursing home residents did not include these individuals who lived in an ALF ZIP code and became long-stay nursing home residents during the year. Examining this rate of transition to becoming a long-stay nursing home resident is an area ripe for future investigation.
Because the estimated 1900 Continuing Care Retirement Communities (CCRCs)(21) in the U.S. contain a combination of living arrangements (from independent living in apartments and cottages, to assisted living, to nursing beds in a dedicated unit) our methodology may have misclassified independent living or nursing home residents as residing in ALFs. Future work similar to this is needed to identify and classify residents of CCRCs. In addition, nursing home residents who are receiving services on a campus co-located with an ALF may have potentially been misclassified as ALF residents. However, with the Minimum Data Set and claims data, it would be possible to exclude the nursing home residents from our sample of assisted living residents.
To overcome many of these limitations in this methodology as well as the growth in Medicare Advantage beneficiaries, it would be worthwhile for the Centers for Medicare and Medicaid Services to include a place of residence code for all Medicare beneficiaries so that more direct approaches can be used to track quality of care across settings in the future. In addition, this could provide an approach to testing the sensitivity and specificity of our methodology.
CONCLUSIONS
This paper provides a first of its kind methodology to capture data on a growing long-term care industry. Using 9-digit ZIP codes and providing comparisons with a reliable, nationally representative data and other cohorts of Medicare beneficiaries, we have developed a research methodology for providing pertinent information on the ALF market. As more federal and state dollars are spent on providing care in this sector of long-term care, it is important that we have sound research to understand the quality of these facilities and the health and health outcomes of Medicare beneficiaries residing in ALFs. The development of this methodology sets the stage for important additional work in this area.
Acknowledgments
Funding:
This work was supported by the National Institute on Aging (#R21AG047303).
Footnotes
Conflicts of Interest:
Authors Kali Thomas, David Dosa, Jennifer Nazareno, David Grabowski, Rajesh Makenini and Pedro Gozalo have no potential conflicts of interest to declare. Vincent Mor, Ph.D. is a founder and on the board of directors of PointRight, Inc. an information services company serving nursing homes on quality measurement and improvement. Dr. Mor is also a stock holder for PointRight, Inc. and Navi Health. Dr. Mor receives no research funding, data or consultation on his research from PointRight or NaviHealth. Dr. Mor also received honoraria from the Alliance for Health Care Quality. Dr. Nazareno is a co-owner of an assisted living facility in California.
Contributor Information
Kali S. Thomas, Assistant Professor of Health Services, Policy and Practice, Phone: 401-863-9036, Fax: 401-863-34891.
David Dosa, Associate Professor of Medicine, Associate Professor of Health Services, Policy and Practice, Phone: 401-863-3758, Fax: 401-863-34891.
Pedro L. Gozalo, Associate Professor of Health Services, Policy and Practice, Phone: 401-863-7795, Fax: 401-863-34891.
David C. Grabowski, Professor of Health Care Policy in the Department of Health Care Policy, Phone: 617-432-3369, Fax: 617-432-34352.
Jennifer Nazareno, Post Doctoral Fellow, Phone: 401-863-1822, Fax: 401-863-34891.
Rajesh Makineni, Senior Programmer/Statistical Analyst, Phone: 401-863-1277, Fax: 401-863-34891.
Vincent Mor, Florence Pirce Grant University Professor, Professor of Health Services, Policy and Practice, Phone: 401-863-2959, Fax: 401-863-34891.
References
- 1.Harris-Kojetin L, Sengupta M, Park-Lee E, et al. Long-Term Care Services in the United States: 2013 Overview. Vital Health Stat. 2013;3:1–107. [PubMed] [Google Scholar]
- 2.Hawes C, Rose M, Phillips CD. A National Study of Assisted Living for the Frail Elderly: Results of a National Survey of Facilities. Washington, DC: 1999. [Google Scholar]
- 3.Polzer K. Assisted Living State Regulatory Review. Washington, DC: 2012. [Google Scholar]
- 4.Hawes C, Phillips CD, Rose M. High service or high privacy assisted living facilities, their residents and staff: Results from a national survey. Research Triangle Park ND: Research Triangle Institute; 2000. [Google Scholar]
- 5.Phillips CD, Holan S, Sherman M, et al. Medicare expenditures for residents in assisted living: data from a national study. Health Serv Res. 2005;40:373–388. doi: 10.1111/j.1475-6773.2005.00362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Phillips CD, Munoz Y, Sherman M, et al. Effects of facility characteristics on departures from assisted living: results from a national study. Gerontologist. 2003;43:690–696. doi: 10.1093/geront/43.5.690. [DOI] [PubMed] [Google Scholar]
- 7.Zimmerman S, Gruber-Baldini AL, Sloane PD, et al. Assisted living and nursing homes: apples and oranges? Gerontologist. 2003;43(Spec No 2):107–117. doi: 10.1093/geront/43.suppl_2.107. [DOI] [PubMed] [Google Scholar]
- 8.Park-Lee E, Caffrey C, Sengupta M, et al. Residential care facilities: a key sector in the spectrum of long-term care providers in the United States. NCHS Data Brief. 2011:1–8. [PubMed] [Google Scholar]
- 9.Mollica R, Sims-Kastelein K, O’Keefe J. Residential Care and Assisted Living Compendium. Washington, DC: 2007. [Google Scholar]
- 10.Mollica R, Houser AN, Ujvari K. Assisted Living and Residential Care in the States. Washington, DC: 2010. [Google Scholar]
- 11.Kozar-Westman M, Troutman-Jordan M, Nies MA. Successful aging among assisted living community older adults. J Nurs Scholarsh. 2013;45:238–246. doi: 10.1111/jnu.12027. [DOI] [PubMed] [Google Scholar]
- 12.Resnick B, Galik E, Gruber-Baldini AL, et al. Perceptions and performance of function and physical activity in assisted living communities. J Am Med Dir Assoc. 2010;11:406–414. doi: 10.1016/j.jamda.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Stevenson DG, Grabowski DC. Sizing up the market for assisted living. Health Aff (Millwood) 2010;29:35–43. doi: 10.1377/hlthaff.2009.0527. [DOI] [PubMed] [Google Scholar]
- 14.Grabowski DC, Stevenson DG, Cornell PY. Assisted living expansion and the market for nursing home care. Health Serv Res. 2012;47:2296–2315. doi: 10.1111/j.1475-6773.2012.01425.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Iwashyna TJ. On the Detection of Nursing Home Use in Medicare Claims. Health Serv Outcomes Res Methodol. 2003;4:187–196. [Google Scholar]
- 16.Yun H, Kilgore ML, Curtis JR, et al. Identifying types of nursing facility stays using medicare claims data: an algorithm and validation. Health Serv Outcomes Res Methodol. 2010;10:100–110. [Google Scholar]
- 17.Moss AJ, Harris-Kojetin LD, Sengupta M, et al. Design and operation of the 2010 National Survey of Residential Care Facilities. Vital Health Stat. 2011;1:1–131. [PubMed] [Google Scholar]
- 18.Intrator O, Hiris J, Berg K, et al. The residential history file: studying nursing home residents’ long-term care histories(*) Health Serv Res. 2011;46:120–137. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seip DE. Tallying the first national Assisted Living Survey. Contemp Longterm Care. 1989;12:28, 30, 32–23. [PubMed] [Google Scholar]
- 20.Caffrey C, Sengupta M, Park-Lee E, et al. Residents living in residential care facilities: United States, 2010. NCHS Data Brief. 2012:1–8. [PubMed] [Google Scholar]
- 21.Ziegler Capital Markets. Ziegler National Continuing Care Retirement Community (CCRC) Listing and Profile, a report. Nov, 2009. [Google Scholar]