Abstract
Cardiovascular disease (CVD) is the leading cause of death and disability in Russia as is case with the most other countries of the world, although Russia has unique features and demographic trends. In the late 90’s and early 2000’s Russia has sustained a profound demographical crisis with a period of overmortality but since 2003 the mortality rates are declining. By 2013, the birth rates exceeded mortality. The reversal of the demographic crisis took place on the background of a number of comprehensive governmental efforts with focus on non-communicable diseases prevention. The National Priority Project “Health” implied enhancement of primary care along with improving availability of state-of-art care for CVD patients. The most notable activities in the field of preventive medicine were the launch of Health Centers for universal free-of-charge screening for risk factors and for preventive counseling and the Dispanserization program (a large scale health screening aiming on detection of both people with chronic conditions and of high-risk persons).
Keywords: Risk factors, prevention, screening, counseling
Cardiovascular disease (CVD) is the leading cause of death and disability in most countries of the world, including Russia (1-4). At the same time Russia has a number of unique features and demographic trends. First of all, in the late 90’s and early 2000’s Russia has sustained a profound demographical crisis with a period of overmortality primarily due to CVD which has led to the so called “Russian cross” phenomenon when the number of deaths exceeded the number of births in 1992 and the corresponding curves criss-crossed (4). It was time of turbulent political and economic changes and subsequent decline in population well-being. In recent years the prosperity has increased due to economic growth, but CVD mortality is still much higher in the Russian Federation compared to the average in Europe (55.7% vs. 46% according to the World Health Organization Mortality Database 2013) (5,6), but still we have come up with a marked improvement (7). Surely, these positive trends could also be influenced by migration but in fact the migration rates were higher in the 90’s than nowadays. For instance, the positive migration balance amounted to 877,532 in 1994 and 20 years later in 2014 it was only 299,990 people.
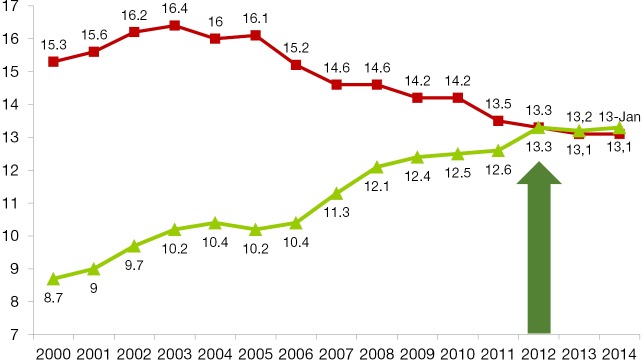
The mortality rates have been declining in Russia since 2003 with an average rate of mortality lowering of 3.2% per year, and in 2013 fertility finally exceeded mortality again (see Figure 1). This recent favorable trend coincided with economic growth but improvement of CVD health was also based on huge governmental efforts.
Figure 1.
Fertility and mortality in Russia (2000–2014, per 1,000).
The chronological order of state activities in the field of CVD prevention is provided in Table 1. In January 2006, the National Priority Project called “Health” (8) was launched in Russia which implied following activities. First of all, enhancement of primary care took place through GPs training, financial support of primary care practitioners and through equipment upgrade in outpatient clinics and ambulance services. The next step was the so called “vascular programme” (implemented from 2008 to 2011) which aimed at establishing of state-of-art care for patients with CVD foremost with acute myocardial infarction and strokes.
Table 1. State support of CVD prevention.
| Year | Action |
|---|---|
| 2006 | Start of the “Health” State National Project |
| 2008 | Russia has signed the WHO Frame Convention against Smoking |
| 2009 | 695 Health Centers were opened throughout Russia |
| 2010 | Vladimir Putin has signed the National Antismoking Concept: Ban on advertising of cigarettes in shops; 21% increase of taxes on cigarettes; Ban on smoking in public places from 2013 |
| 2011 | First Global Ministerial Conference on Healthy Lifestyles and NCDs control, 28–29 April, 2011 (Moscow Declaration) |
| 2011 | Federal law #323 “Healthcare of citizens of the Russian Federation”: Priority of preventive strategy in healthcare |
| 2014 | State programme of the Russian Federation “Development of Healthcare till 2020 year”: Subprogramme 1. Prevention of NCDs and healthy lifestyle |
CVD, cardiovascular disease.
Since 2008, promoting of healthy lifestyle and prevention of non-communicable diseases and in particular CVD have been in the highlight. That year Russia had joined the WHO Frame Convention on Tobacco Control and after all the necessary arrangements (9) our country signed the National Antismoking Concept in 2010. Subsequently, the Federal law on health protection from environmental tobacco smoke and consequences of tobacco use (10) came into effect in 2013 that implied a ban on cigarettes advertising in shops; a 21% increase of tobacco taxes and a ban on smoking in public places.
The 2009 was year of birth for unique preventive care facilities, so called Health Centers for adult population and Health Centers for children (11,12). A total of 695 such institutions have been opened throughout Russia that year. In some regions the Health Centers became the very first institutions dealing with medical prevention. This conceptually new structures in the Russian healthcare system were launched as a part of the National priority project “Health” and their services were free of charge for the citizens of the Russian Federation. The core areas of Health Centers activities are detection and monitoring of risk factors for CVDs and other non-communicable diseases, as well as group and personal counselling on healthy lifestyle and risk factors. The Health Centers are equipped to assess following risk factors and health indicators: the smoking status (by self-report and based on carbon monoxide in the exhaled air and urinary cotinine measurements); the level of physical activity; eating habits; the body mass index (BMI): waist circumference; blood pressure; heart rate; grip strength, stress level; ankle-brachial index; heart rate variability; total cholesterol, blood glucose; adiposity using bioimpedance analysis; oral health and hygiene, vision acuity and intraocular pressure.
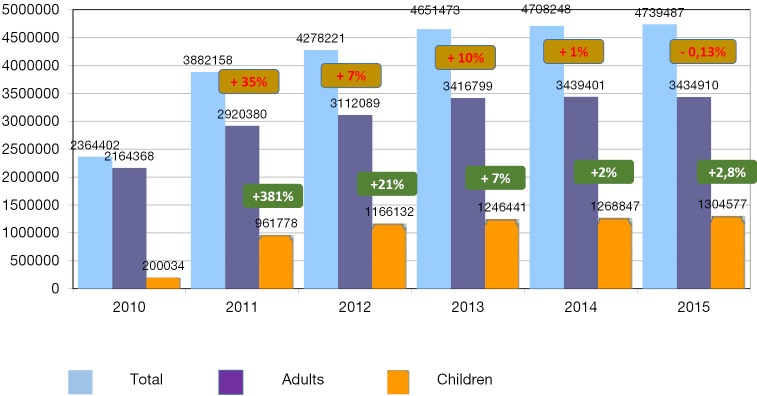
As shown in the Figure 2, the Health Centers have rapidly gained popularity: in 2015 there were a total of 4,739,487 visits versus only 2,364,402 in 2010. To address the growing need for their services additional Health Centers were launched later, so by 2015 we had 806 Health Centers, including 501 Health Centers for adults, 219 Health Centers for children, 23 mixed Health Centers for the whole family and 63 mobile Health Centers for use in rural areas. The latter enhance preventive care in remote and hard to access rural regions. According to the Health Center data up to 81.1% of adults and 66.5% of children visiting these facilities had some risk factors in 2015. Subsequently 86.2% of adult visitors and 82.3% of kids have received individual health counselling.
Figure 2.
Health Center visits (absolute numbers and changes relative to the preceding year) of adult and pediatric patients in 2010–2015.
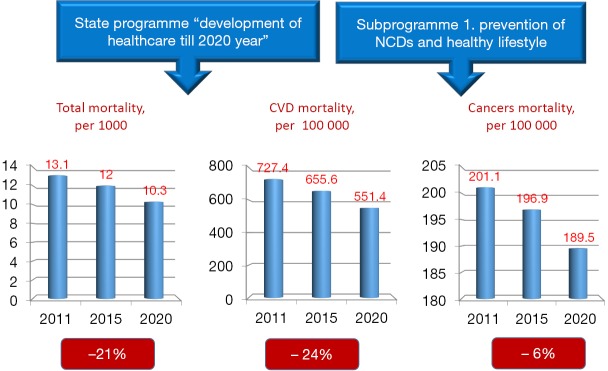
These policies focusing on preventive care were in line with global trends. An important landmark to honor these efforts was the decision to hold the First Global Ministerial Conference on Healthy Lifestyles and NCDs Control in Moscow. The Ministerial Conference took place on 28–29 April, 2011 and resulted in a political declaration (13), committing world governments to develop a global policy on NCDs prevention as well as a global monitoring framework. The commitment to develop such policy was reflected in the Federal Law #323 “Healthcare of citizens of the Russian Federation” (14) which was passed later that year and set specific goals for reducing total and disease-specific mortality (see Figure 3).
Figure 3.
FEDERAL LAW #323 “Healthcare of citizens of the Russian Federation”: main goals.
One of the most striking measures embodied in the new legislation is the dispanserization program, which is a comprehensive health screening program launched in 2013. The word “dispanserization” is another term for screening commonly used in Russia and many other post-Soviet countries. It stems from the French word “dispensaire”, which means a kind of a clinic. All citizens aged 18 and older irrespective of the working status are eligible for this screening program every 3 years. The program is carried out by public outpatient clinics and outpatient departments of hospitals, and people can be referred to such facilities at domiciliary and job or learning locations.
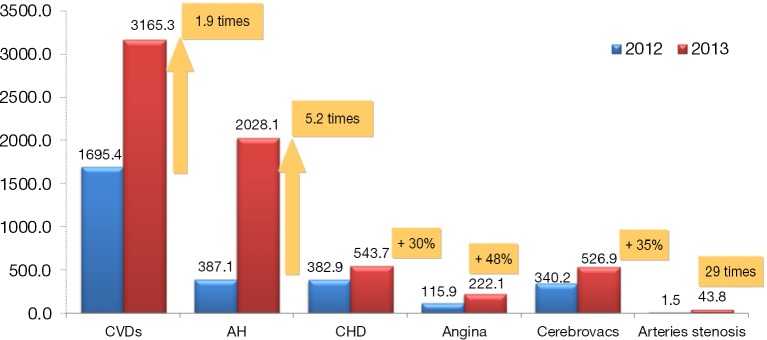
The extent of the work-up in the scope of the dispanserization program depends on age and sex but anyway it consists of two stages. The basic evaluations of the first stage include measurements of height and weight with the calculation of BMI, blood pressure, total cholesterol, blood glucose, ECG, SCORE risk estimates, blood count and urinalysis, chest fluorography, mammography for women aged 39–75 years, pap-smear, PSA for men aged 45 years and older, abdominal ultrasound (every 6 years after 39), intraocular pressure and others. After examination and review of the results primary care physicians can refer patients for additional tests if needed (the second stage of dispanserization). Based on the first stage results patients are categorized into three groups: the 1st health group consists of healthy people with SCORE risk estimates <5%, the 2nd health group implies estimated 10-year fatal CVD risk of ≥5% and the 3rd health group consists of patients with confirmed chronic diseases including CVDs. The identification of the second health group enables follow-up and timely management of high risk patients (approximately 21% of all screened people according to the 2014 dispanserization results). As shown in Figure 4, the start of the dispanserization program enabled identification of many new CVD patients who could receive appropriate care including high tech procedures and interventions (15). From the regulatory point of view dispanserization programs are equal in rural and urban areas, but in some scenarios it’s more complicated for rural population to participate in it because of traffic issues. Nevertheless many regions solve this problem with the use of mobile multidisciplinary teams which carry out the screening program at rural primary care facilities. Along with the abovementioned availability issues the dispanserization program is widely criticized for its being not fully evidence based. In fact, many included tests (e.g., complete blood count, urinalysis, abdominal ultrasound and the ECG) really don’t have any proven benefit as screening methods. Their inclusion was primarily based on their wide availability and relatively low cost. Another reason for their utilization was the intent to meet peoples’ conservative expectations because these tests have been long established as a part of dispanserization programs during the Soviet period. It is planned to gradually eliminate them as soon as the population gets used to the program.
Figure 4.
Dispanserization results, Moscow 2013. New diagnoses of cardiovascular diseases per 100,000.
Obviously all these efforts would not be possible without most active support from the professional community. From 2009 to 2011 the biggest professional associations in the field, the Russian National Society of Cardiology and Russian National Society of Preventive Cardiology, have carried out the so called Healthy Hearts Project which consisted of public actions, educational and social activities. It involved 27 big Russian cities from Kaliningrad to Vladivostok. Within the Healthy Hearts Project 11,000 GPs and cardiologists were involved in training on contemporary strategies of CVD prevention and more than 57,000 citizens participated in basic health-checks and got a professional advice on CVD prevention. 2011 was also the year of the development of the first Russian National Guidelines on CVD prevention (16). Since 2013 we also have National Guidelines on non-communicable diseases prevention. By now, after the release of the 2016 European guidelines on CVD prevention the development of a revised Russian National guideline is underway.
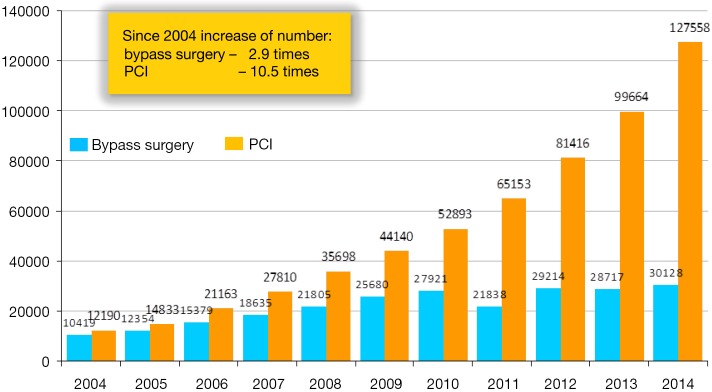
Despite prevention being the primary focus of Russian healthcare policy in recent years as noted above the Priority State National Project “Health” included also the so called “Vascular Program”. Since 2008 more than 16,800 million rubles (approx. 525 million USD) were spent in order to increase the availability of the modern technologies of CVD treatment. As part of the Vascular Program 55 regional vascular centers and 146 vascular departments were opened throughout Russia in 2008–2011 providing all essential cardiovascular surgeries and interventions (percutaneous coronary interventions, bypass grafting, valve surgeries, catheter ablation for arrhythmias, carotid artery surgeries, etc.) in particular in emergency settings. The vascular centers network is designed to improve the uptake of emergency interventions throughout the country including but not limited to rural areas. Figure 5 depicts the marked increase of the coronary revascularization rates in Russia from 2004 to 2014 (17). Current PCI rates have reached 531 PCI per 1,000,000 with placement of 1.37 stents per PCI (18). Nevertheless, we still need improvement of emergency patient logistics in very many rural areas.
Figure 5.
Coronary revascularization procedures in Russian Federation, 2004–2013.
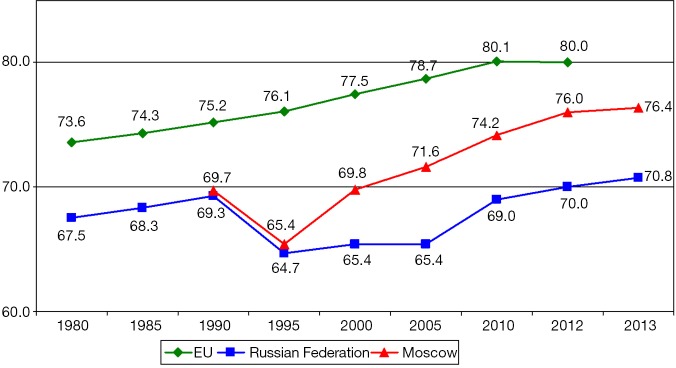
It’s clear that Russian healthcare reform is still at its very beginning and we have a long way to go. But despite the fact that too little time has passed since it started the statistics really began to improve, and it’s very reassuring. In fact, in 2013 the life expectancy of Moscow city inhabitants reached 76.4 years, with only 4 years separating Moscow residents from the European Union population (Figure 6). The life expectancy for the whole country is still much lower than in the capital (70.8 years) but we hope it will improve further.
Figure 6.
Life expectancy at birth, years.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.European Mortality Database. Mortality indicators by 67 causes of death, age, sex. HFA-MDB. Updated July 2016.
- 2.Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315-81. 10.1093/eurheartj/ehw106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Townsend N, Wilson L, Bhatnagar P, et al. Cardiovascular disease in Europe: epidemiological update 2016. Eur Heart J 2016;37:3232-45. 10.1093/eurheartj/ehw334 [DOI] [PubMed] [Google Scholar]
- 4.The demographic yearbook of Russia. 2015: Statistical Handbook/ Rosstat. Moscow, 2015:263.
- 5.World Health Organization Regional Office for Europe. European Health for All Database (HFA-DB). Available online: http://data.euro.who.int/hfadb/ (30 August 2013): WHO Regional Office for Europe, Copenhagen, Denmark, 2013.
- 6.World Health Organization. WHO Mortality Database: 1st May 2013 update. Available online: http://www.who.int/healthinfo/statistics/mortality_rawdata/en/index.html (30 August 2013): World Health Organization, Department of Health Statistics and Information Systems, Geneva, Switzerland, 2013.
- 7.Critical 10 Years. Demographic Policies of the Russian Federation: Successes and Challenges. Moscow: “Delo” Publishing House (RANEPA), 2015:125.
- 8.Popovich L, Potapchik E, Shishkin S, et al. Russian Federation. Health system review. Health Syst Transit 2011;13:1-190, xiii-xiv. [PubMed] [Google Scholar]
- 9.WHO. Guidelines for implementation of the WHO FCTC. 2011. Available online: http://www.who.int/fctc/protocol/guidelines/adopted/guidel_2011/en/index.html, accessed 11 December 2012.
- 10.On protection of population health from exposure of environmental tobacco and consequences of tobacco smoking: the Federal Law of 2013, February 23. Nº15-FZ. Available online: http://www.consultant.ru/cons/cgi/online.cgi?req=doc&base=LAW&n=197273&rnd=235642.2453931421&from=142515-0#0
- 11.Pogosova NV, Vergazova EK, Ausheva AK, et al. Tsentry zdorov'ya: dostignutye rezul'taty i perspektivy. [Health centers: achieved results and prospects]. Profilakticheskaya meditsina 2014;17:16-24.
- 12.Pogosova NV, Vergazova EK, Ausheva AK, et al. Health Centers: achieved results and perspectives (continued). Profilakticheskaya meditsina 2015;18: 34-42.
- 13.First Global Ministerial Conference on Healthy Lifestyles and Noncommunicable Disease Control. Moscow, 28-29 April 2011 MOSCOW DECLARATION. Available online: http://www.who.int/entity/nmh/events/moscow_ncds_2011/conference_documents/conference_report.pdf?ua=1
- 14.Federal Law No. 323-FZ of 21 November 2011 on Basics of Health Protection of the Citizens in the Russian Federation as amended to 29 December 2015. Available online: http://www.consultant.ru/document/cons_doc_LAW_121895/
- 15.Kalinina AM, Ipatov PV, Kushunina DV, et al. Results of circulatory disease detection during prophylactic medical examination of the adult population: the first two years' experience. Ter Arkh 2016;88:46-52. 10.17116/terarkh201688146-52 [DOI] [PubMed] [Google Scholar]
- 16.Russian National Society of Cardiology. Cardiovascular prevention. National guidelines. Moscow, 2011:64. [Google Scholar]
- 17.Bokeriya LA, Gudkova RG. Annual collection of the Cardiovascular Surgery, 2004-2013.
- 18.Kharlamov AN. Cardiovascular burden and percutaneous interventions in Russian Federation: systematic epidemiological update. Cardiovasc Diagn Ther 2017;7:60-84. 10.21037/cdt.2016.08.10 [DOI] [PMC free article] [PubMed] [Google Scholar]