Abstract
Authors conducted a systematic literature review on early identification steps leading at-risk young children to connect with Part C services. Authors classified data collection settings as primary (settings for general population) or specialized (settings for children at risk of developmental delay) and according to the phases of early identification in the study: (a) original population of children aged 0 to 6 years who had received Part C services, (b) screening and/or referral and/or developmental assessment from 0 through age 2 years, and (c) were deemed eligible and/or received Part C services. Authors identified 43 articles including at least two phases of the early identification process. The literature about connecting children to Part C early intervention (EI) is sparse and fragmented; few studies document the full process from community monitoring to service receipt. Results indicate opportunities for development of systems to better track and improve the identification of young children in need of EI.
Keywords: Child Find, Individuals With Disabilities Education Act, Part C, developmental surveillance, community monitoring
The first few years of life are a time of rapid development, with most children following a predictable sequence of learning to move, speak, act, learn, and play (Cole, Cole, & Lightfoot, 2005; Shelov & Hanneman, 1993); however, across childhood, an estimated 15% of children are identified with developmental delays or disabilities (Boyle et al., 2011). Federal law, under the Individuals With Disabilities Education Improvement Act (IDEA; 2004), contributes federal funding for early intervention (EI) services to children with significant developmental challenges: Part C (originally Part H) provides EI for children from birth to age 3 (Part B for children aged 3–5) with diagnosed physical or mental conditions likely to result in developmental delays (e.g., Down syndrome, very low birth weight [VLBW]), or who meet a state-defined level of significant developmental delay (IDEA, 2004), or, in some states, have a high probability of negative developmental impacts (e.g., due to environmental risk factors; Danaher, Armijo, & Lazara, 2006). Current single point in time counts indicate that approximately 2.8% of infants and toddlers receive Part C EI services (U.S. Department of Education, 2012) and, on average, children are referred to EI at around 13 months of age and receive services around 16 months (Bailey, Hebbeler, Scarborough, Spiker, & Mallik, 2004). However, parents of children who receive EI often express concerns many months before ultimately being referred to EI due to physicians conducting independent diagnostics (Bailey et al., 2004) or simply taking a “wait and see” approach (Sices, Egbert, & Mercer, 2009). This can lead to several months of lost EI services and speaks to the vital importance of how integrated and visible Part C early identification efforts are in the community.
Before an infant or toddler can participate in EI services, developmental concerns or delays must be identified. To identify children, states have developed mandated Child Find, assessment, and Individualized Family Service Plan (IFSP) systems (Blackman, Healy, & Ruppert, 1992; Bricker, Macy, Squires, & Marks, 2013). Child Find refers to state systems designed to locate children who are eligible for EI services and may optionally include formal developmental surveillance efforts (American Academy of Pediatrics [AAP] et al., 2006). Upon referral, EI programs have 45 days to evaluate a child’s development and determine whether the child is eligible for Part C EI services. A positive eligibility determination can lead to the creation of an IFSP and official entrance to Part C EI services.
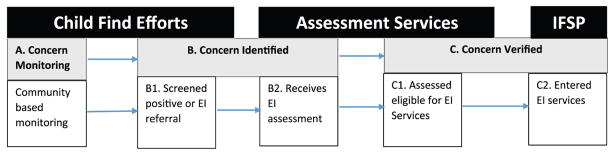
Figure 1 provides a conceptual model of this early identification process from community monitoring to IFSP receipt. Briefly, the identification process begins when community partners (e.g., health care providers) conduct developmental surveillance activities (e.g., developmental screening). Once a developmental concern is identified, children are referred to EI for an assessment that results in an eligibility determination to verify the developmental concern and, for eligible children, facilitates entrance into EI.
Figure 1.
Model of steps in the process leading to early identification for Part C systems.
Note. Black boxes up top indicate broader Part C processes associated with aspects of early identification efforts. Mid-level gray boxes indicate steps in the identification of concerns affecting Part C decisions as children move from monitoring into the Part C referral, assessment, and services systems. White boxes indicate tangible activities addressing concerns occurring at each step of the Part C early identification process.
Child Find–Specific Data Needs
The U.S. Department of Education and Congress require data on most of the steps leading to an IFSP receipt (Bricker et al., 2013). This includes data on referrals, timeliness of developmental evaluations, eligibility determinations, timeliness of an IFSP receipt, demographic data, and location of rendered services (Derrington, Spiker, Hebbeler, & Diefendorf, 2013). Thus, federally reported data begin once a concern is identified (B1 in Figure 1); however, there is currently no systematically collected information allowing us to assess the effectiveness of Child Find efforts at identifying children in need of EI.
The lack of data on Child Find systems may stem from the fact that federal regulations are minimal and simply require that states “ensure that all children with disabilities … are identified, located, and evaluated; and a practical method is developed and implemented to determine which children are currently receiving needed special education and related services” (IDEA, 2004, 34 C.F.R. § 300.125). “Practical methods” used by states currently range from public awareness campaigns to the coordinated merging of state and/or local data systems track community cohorts across multiple systems (Bricker et al., 2013; Clements, Barfield, Ayadi, & Wilber, 2007; Clements, Barfield, Kotelchuck, Lee, & Wilber, 2006; Clements, Barfield, Kotelchuck, & Wilber, 2008; Montgomery & Miller, 2001). The federal government requires that states monitor the number of children referred and those who receive Part C EI services; however, states are not required to track or report the number of children from the community who are monitored or screened (Bricker et al., 2013). The lack of systematic data collection efforts limits current understanding of Child Find activities, including the use and effectiveness of developmental monitoring and screening as a factor in the process of early identification (Bricker et al., 2013; Derrington et al., 2013).
It seems likely that the implementation of Child Find identification efforts vary widely. For example, primary care physicians in one state may directly report concerns about a child to Part C (Bricker et al., 2013), but physicians in another state may rely on interconnected data systems where children’s medical records are linked to Part C (Clements et al., 2007; Clements et al., 2006). Furthermore, some community partners use formal screening tools or interviews to elicit caretaker concerns to inform referral decisions, whereas others may not (Bricker et al., 2013; Dworkin, 1989; King & Glascoe, 2003; Pulsifer, Hoon, Palmer, Gopalan, & Capute, 1994; Shannon & Anderson, 2008). Other groups working with niche early childhood groups may have professional policies or mandates requiring referrals due to serving high-risk children (e.g., Bricker et al., 2013), whereas other groups may not. For example, under the Child Abuse Prevention and Treatment Act (CAPTA; 2003), children suspected of abuse or neglect are supposed to receive developmental screening, as are newborns suspected of hearing problems (Centers for Disease Control and Prevention, 2012; White & Blaiser, 2011). Finally, although technically an education law, Part C is often administered via non-education entities (typically public health agencies; Bricker et al., 2013), potentially affecting specific Child Find practices. Thus, the capacity to understand, assess, and improve Child Find efforts is hindered by a lack of data on practices that likely vary greatly across communities.
Early Identification Process Data Needs
Research Questions
The purpose of this article is to answer the following research questions:
Research Question 1: How many published studies capture data on at least two steps in the process of identifying concerns (Figure 1) routing children to Part C services?
Research Question 2: Do recent studies report data on all three steps in the process of identifying concerns for Part C intervention as modeled in Figure 1, including EI entrance (C2)?
Research Question 1 aims to establish and quantify the scarce research base reporting data on multiple aspects of Part C early identification systems. Research Question 2 aims to establish recent data systems that may serve as models researchers may reference when designing studies concerned with tracking data from children in community setting through referrals and ultimately receipt of EI services.
Method
Literature Search
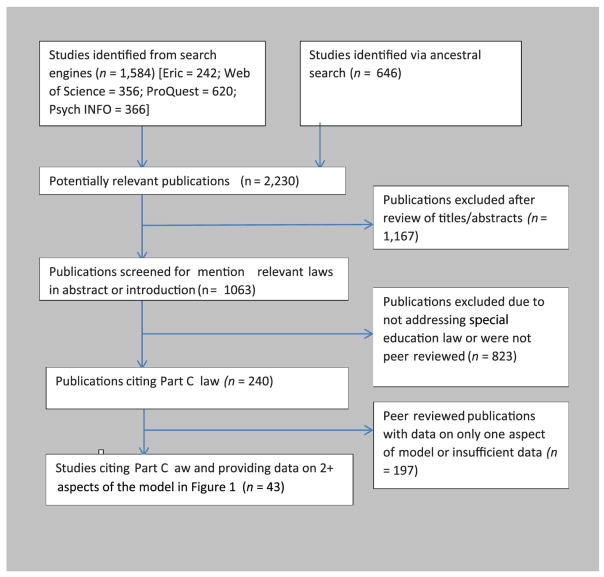
Authors used ERIC, PsycINFO, Proquest, and Web of Science to locate articles across education, psychology, public health, and medical literatures pertaining to both Part C and steps in the identification process. Search terms included Individuals With Disabilities Education Act, part c, part h, child find, Title V, 108-446, 105-17, 99-457, 101-476, 102-119, and 105-17 paired with monitor*, surv*, eligib*, screen*, ancil*, assess*, interven*, established risk, category one, presumed eligibility, established condition, or presumptive eligibility. Authors also performed ancestral searches from studies considered for the final analysis. Authors limited literature searches to studies published from January 1986 to December 2015. Authors chose January 1986 as a cutoff because IDEA was re-authorized with the addition of Part C that year. All studies came from peer-reviewed journals.
Inclusion and exclusion criteria
Authors included only databased studies citing Part C of IDEA in abstracts or in the text of literature reviews. Authors included studies with data on at least two of the following three key steps in identifying children for Part C services (see Figure 1): (a) the number of children in the study population, (b) the subset of children in A who screened positive and/or were referred for (B1) and/or received a developmental assessment (B2), (c) the subset of children in A and/or B assessed eligible for (C1) and/or entered Part C EI services (C2). Authors omitted psychometric studies and studies soliciting professional opinions or training on Part C systems. See Figure 2 for details of the search process.
Figure 2.
Flow diagram displaying decision-making criteria across the literature search and selection.
Coding
Steps to early identification
The author’s primary variables of interest were the early identification steps leading to Part C services. First, authors coded whether data were collected on community cohorts of children (A1 from the model in Figure 1) for whom a subset was reported to have developmental concerns, positive screens, assessment or evaluation, referral to EI, EI eligibility, or entrance into EI. Second, authors coded studies with data indicating whether a subset of children was eligible for a Part C assessment. Eligibility for an assessment was determined by whether children were screened or referred or actually assessed. Screened and/or referred indicates studies reporting on subsets of children who screened positive or subsets of children who were referred for an EI assessment (B1 from the model). Assessed indicates studies reporting subsets of children who received developmental assessments (B2 from the model). Finally, authors coded studies that collected data indicating that a subset of children was eligible for, or was entered in, Part C EI services. Eligible for indicates studies reporting subsets of children who received a Part C qualifying eligibility or scored below a certain threshold on a developmental assessment (C1 from the model). Entered indicates subsets of children who actually received EI services (C2 from the model).
Model systems
Because a critical goal of Child Find is to use developmental monitoring, screening, and referral to identify children in the population who may qualify for Part C EI services, studies identifying a process for following total populations of children from screening or referral to actually entering EI are considered model systems. Authors chose model systems according to the following criteria: (a) recent publication (i.e., since 2006), (b) presence of all three steps in the process to early identification seen in Figure 1, (c) data available on the number of children who entered EI (i.e., section C2 of the model), and (d) not national survey data. Inclusion of EI entrance, and not simply EI eligibility, that was selected for model systems as EI eligibility, although important, does not translate to actual service receipt, the ultimate end point of Child Find. Furthermore, national surveys, although critical to developing population estimates (Rosenberg, Zhang, & Robinson, 2008), are omitted due to a lack of critical information about Child Find processes in communities.
Population setting
Some states focus their Child Find efforts in specialized settings where children at higher risk of developmental delay may be found, whereas others use a broader, community-based approach. Understanding these differences sheds light on the variety of Child Find efforts and could provide insight on the effectiveness of approaches. Primary, or general, population settings refer to sites collecting data from children in the general population, regardless of socioeconomic status or developmental risk (e.g., in pediatricians’ offices, day care/preschools). Specialized population settings refer to sites collecting data on specific groups of children who have a higher risk of developmental delays compared with the general population (e.g., in neonatal intensive care units, developmental clinics).
Descriptive characteristics
In addition to data answering the research questions, authors also coded studies according to several descriptive characteristics that may be interesting to some readers: (a) year of publication, (b) sample age range, (c) state/region where data were collected, (d) journal/academic field, (e) sample type, and (f) analysis focus. Year of publication included actual publication year and unreported. Sample age range included age ranges of the subjects and unreported. State/region included options for each of the 50 states, multiple states weighted or unweighted for national representation, and unreported. Journal/academic field included developmental/disability, education/intervention, or medical journal classifications. Sample type included cohort/epidemiological population, convenience/community samples, or other/unreported. Analysis focus included systems level, measurement/individual level, or both.
Data Management and Analysis
Two authors independently coded a random sample of studies (N = 18). Using the Landis and Koch (1977) reliability values for coding entries, population setting, analysis focus, IDEA Law Centrality, eligible/entered, and total model ratings achieved “substantial” agreement; state/region, journal, sample type, data type, and screened/referred codes were “almost perfect.” The senior author reviewed studies categorized differently by the two reviewers, as well as reviewed all data on steps leading to Part C services. Disagreements between authors were settled via further review of the article and discussion. The primary data for this study are found in Tables 1 and 2. Table 1 documents the overall steps in the identification process found across studies broken down by primary and specialized settings. Table 2 contains abstracted data on the studies identified in this review including authors, setting type, steps in the identification process, details of the community systems, age ranges of the children, and a synopsis of the study in terms of steps in the EI early identification process. This table is organized chronologically by primary and secondary settings.
Table 1.
Central Characteristics of Studies by Setting (N = 43).
| Variablea | Primary n | Specialized n | Total n (%) |
|---|---|---|---|
| Whole (A, B, C in Figure 1) | 9 | 12 | 21 (46.2) |
| Total and screened/referred (A, B) | 2 | 1 | 3 (7.7) |
| Total and eligible/diagnosed (A, C) | 6 | 11 | 17 (41.0) |
| Screened/referred and eligible/diagnosed (B, C) | 0 | 2 | 2 (5.1) |
Note. Primary settings refer to sites collecting data from children in the general population. Specialized settings refer to sites collecting data on specific groups of children with a higher risk of developmental delays compared with the general population.
Stages of identification.
Table 2.
Synopses of Peer-Reviewed Research on Part C Monitoring Model, by Setting and Date.
| Author | Setting | Step | System | Ages (in months) | Synopsis |
|---|---|---|---|---|---|
| Lynch, Mercury, DiCola, and Widley (1988)a | Primary | A, B1, C2 | MN elementary school system | 0–48 | Of 277 children, 68 were in SPED and 56 children were referred to EI before 48 months; 15 received EI; 101 of the 277 were screened prior to 48 months. |
| Study 1 | |||||
| Rojahn et al. (1993) | Primary | A, C1 | OH birth certificate | NA | Of 1,520 children 106 to 579 were EI eligible depending on assessment cutoff used. |
| Simpson, Colpe, and Greenspan (2003)a | Primary | A, B2, C2 | NHISD | 4–59 | Of 15,291 infants, ~505 to 520 were EI eligible depending on assessment used. Of these, ~86 to 161 were enrolled in EI. |
| Mott and Dunst (2006) | Primary | A, B2 | western NC, 4 counties | 0–36 | Of a 0–3 population of ~8,500, 180 were enrolled in EI. |
| Clements, Barfield, Kotelchuck, Lee, and Wilber (2006) | Primary | A, B1, B2, C1 | MA PELL | 0–12 | Of 219,037 live births, 215,313 had linkable records. Of these, 14,852 were referred to EI; ~13,081 were assessed and 11,170 were EI eligible. |
| Clements, Barfield, Ayadi, and Wilber (2007) | Primary | A, B1, B2 | MA PELL | 0–36 | Of 76,901 live births surviving 28 days, 14,033 were referred to EI, ~13,051 were assessed, and ~9,683 were EI eligible. |
| Shannon and Anderson (2008) | Primary | A, B1, B2, C1 | NH Easter Seals: Baby Steps | 0–60 | Of 3,063 children, 924 screened positive and 191were referred to EI. Of 185 children who went to their referrals, 146 were EI eligible. |
| Clements, Barfield, Kotelchuck, and Wilber (2008) | Primary | A, B1, B2, C2 | MA PELL | 0–36 | Of 219,001 live births, 40,711 were referred to EI, ~35,707 were assessed, and 29,950 enrolled in EI. |
| Barfield et al. (2008) | Primary | A, B1, B2 | MA PELL | 0–36 | Of 247,959 total live births, 1,233 were VLBW (weight <1,200 g), of who 1,108 were referred to EI for an assessment. |
| Rosenberg, Zhang, and Robinson (2008) | Primary | A, C1 | ECLBS: National survey | 9–24 | Longitudinal study of 10,700 children. At 9 months old, of 10,200 children with data, 1,224 were either EI eligible or VLBW (<1,500 g). At 24 months old, of 8,950 children with data, ~1,235 were EI eligible or were VLBW (<1,500 g). |
| Meade, Sweeney, Chandler, and Woodward (2009) | Primary | A, B1, B2, C1 | Houston Co., MN; 5 clinics | 4–8 | Of 55 children, 33 screened positive and 43 were evaluated; 15 of the 43 were referred to EI. |
| Manning et al. (2011) | Primary | A, C2 | MA PELL | 0–36 | Of 388,644 children, 3,013 were in EI with an autism spectrum disorder. |
| Feinberg, Silverstein, Donahue, and Bliss (2011) | Primary | A, C1, C2 | ECLBS: National survey | 9–24 | Of 10,700 infants at 9 month olds, 1,000 were EI eligible and ~90 were in EI. Of 9,850 of the same children at 24 months old, 1,000 were EI eligible and ~120 were in EI. |
| McManus and Rosenberg (2012) | Primary | A, C1, C2 | ECLBS: National survey | 9–24 | Longitudinal study of 10,700 children. Of ~8,800 children at 9 or 24 months, ~2,800 to ~2,900 were EI eligible depending on assessment type and cutoff score. Up to ~2,279 were in EI at 9 months and up to 2,702 were in EI at 24 months. |
| Derrington (2012)a | Primary | A, B1, B2, C2 | MA PELL | 0–36 | Of 624,269 live births, 7,348 were drug exposed and 7,290 of these infants survived; 4,436 drug-exposed children were referred to EI, 3,868 were assessed, and 3,459 entered EI. |
| Rosenberg, Robinson, Shaw, and Ellison (2013) | Primary | A, C1 | ECLBS: National survey | 9–24 | Longitudinal study of 10,700 children. Of ~7,300 9-month-olds and ~6,400 24-month-olds who had been full-term infants, ~128 to ~5,694 were EI eligible depending on age and state EI requirements. |
| Blackman, Lindgren, Hein, and Harper (1987)a | Specialized | A, B1, B2, C2 | IHRFUP | 0–60 | Of 1,014 infants, 155 screened positive at 30 months and 396 were assessed at 60 months. Of the screened children, ~141 could be reached at 60 months and ~94 were enrolled in EI. |
| Lynch et al. (1988) | Specialized | B1, C1 | MN school system | 0–48 | Of 223 EI referrals, 183 children were EI eligible. |
| Study 1 | |||||
| Brinker, Frazier, Lancelot, and Norman (1989) | Specialized | A, B1, B2, C1 | Chicago, IL NICU & Health clinics | 0–36 | Of 4,750 NICU infants, 1,790 returned for a follow-up visit. Of 579 children, 115 screened positive, 105 were referred for assessments, 22 were assessed, and 15 were EI eligible. |
| Feldman, Ploof, Hofkosh, and Goehring (1993) | Specialized | A, B2, C1 | Pittsburgh, PA Children’s Hospital | 0–36 | Of 135 children spending >30 consecutive days in hospital, 83 were assessed, 48 were eligible for tracking, but not EI; 73 were EI eligible. |
| Kirby, Swanson, Kelleher, Bradley, and Casey (1993) | Specialized | A, C1 | IHDP | 7–83 | Of 562 LBW infants (birth weight (≤2,500 grams or (≤37 weeks), ~148 were EI eligible at 36 months. |
| Sinclair (1993) | Specialized | A, B2, C1 | UCLA Head Start | Of 900 children, 159 were assessed and 151 were EI eligible. | |
| Kang, Barnard, and Oshio (1994) | Specialized | A1, B1 | WA EIPD | Infants | Of 75 infants, 25 were referred to EI. |
| Solomon, Clougherty, Shaffer, Hofkosh, and Edwards (1994) | Specialized | A, B1, C1 | Allegheny, PA Welfare Dept. | Of 313 children screened, 95 were referred for an assessment and 90 were EI eligible | |
| Dunbar and Reed (1999) | Specialized | A, B1, C1 | Women’s & Children’s | NA | Of 77 children observed, ~39 were screened and 38 assessed. Of screened children, one was referred to EI; of assessed children, 28 needed further assessments and three were referred to EI. |
| Montgomery and Miller (2001) | Specialized | A, B1, C1 | CO CNRP birth defects | 0–36 | Of 10,990 children, 4,146 were contacted, 1,812 children were referred to EI, and 1,365 of those referred were EI eligible. |
| Shapiro and Derrington (2004) | Specialized | B1, C2 | HI Child Find | 0–60 | Of 161 EI referrals, 96 children were enrolled in EI. |
| Peterson et al. (2004) | Specialized | A, C1, C2 | Head Start | 0–36 | Of 3,001 children, 286 had diagnosed conditions, 1,173 were EI eligible, 1,421 had biological risks, and 99 were in EI. |
| Robinson and Rosenberg (2004) | Specialized | A, C1, C2 | CO CWEST | 0–36 | Of 5,473 children receiving welfare, 668 had EI eligible conditions; however, only 113 were enrolled in EI. |
| Stahmer et al. (2005) | Specialized | A, C1, C2 | NSCAW National Survey | 0–60 | Of ~1,350 0- to 2-year-olds in the child welfare system, ~84 to 413 were EI eligible depending on assessment type, ~174 received any services, and ~95 were in EI. Of ~1,463 3- to 5-year-olds, ~120 to 467 were EI eligible depending on the assessment used, ~462 received any services, and ~238 were in EI. |
| Jackson and Needelman (2007)a | Specialized | A, B1, C2 | NE TIPS | 0–36 | Of 2,631 NICU children, ~1,496 children screened positive depending on screener type, 458 were referred and 303 enrolled in EI. |
| Casanueva, Cross, and Ringeisen (2008) | Specialized | A, C1, C2 Assessed | NSCAW: National | 0–36 | Of 1,845 children under investigation for maltreatment, ~649 were EI eligible at baseline and ~723, 1.5 years later; ~216 were enrolled in EI at baseline and ~114, 1.5 years later. |
| Derrington and Lippitt (2008)a | Specialized | A, B1, C2 | National, state, published, MECLI, and 0 to 3 Maltreatment counts | 0–36 | Of 178,384 children in zero to three maltreatment counts, 107,030 were referred to EI, and 57,343 enrolled in EI. |
| Rosenberg and Smith (2008) | Specialized | A, C1 | NSCAW National Survey | 0–36 | Of 1,997 children investigated for abuse, 938 were EI eligible |
| Scarborough and McCrae (2008) | Specialized | A, C1 | NSCAW National Survey | 0–12 | Of 1,196 children investigated for abuse, 630 had IFSP data available; 241 children had an IFSP and 389 had none. Of the 1,196, ~84 to ~634 were EI eligible depending on assessment used. |
| McManus, McCormick, Acevedo-Garcia, Ganz, and Hauser-Cram (2009) | Specialized | A, C1, C2 | NSCHCN: National survey | 0–36 | Of 2,350 children with special health care needs, 900 were EI eligible and ~411 were enrolled in EI. |
| Scarborough, Lloyd, and Barth (2009) | Specialized | A1, C1 | NSCAW National Survey | 0–36 | Of 997 children investigated for maltreatment, 756 to 786 had assessment data available at 18 months post-baseline and 675 to 786 had assessment data available at 36 months post-baseline; ~279 to 330 were EI eligible at 18 months post-baseline and ~196 to 353 at 36 months post-baseline depending on the assessment type. |
| Wang et al. (2009) | Specialized | A, C2 | Unreported state, death, Medicaid, Vital, and EI records | 0–36 | Of 884 ELBW (<1,000 g) infants, ~477 were enrolled in EI. |
| Tang, Feldman, Huffman, Kagawa, and Gould (2012) | Specialized | A, B1, C1 | CA NICU | 0–36 | Of 5,129 infants at an initial visit, 1,609 were screened and 3,270 assessed; 185 screened positive and 588 were EI eligible. Of 1,737 of the same infants at a second visit, 486 were screened and 1,169 assessed; 78 screened positive and 191 were EI eligible. |
| Marshall and Mendez (2014) | Primary | A, B1, C1 | FL screening program | 24–60 | Of 138 screened children, 57 had follow-up data. Of those 57, 25 were referred for an EI assessment and 17 were EI eligible. |
| McManus, Magnusson, and Rosenberg (2014) | Specialized | A, C1 | NSCSHCN | 0–36 | Of 923 children with developmental disabilities or delays, 484 were enrolled in EI. |
| Roberts, Needelman, Jackson, McMorris, and Munyon (2014) | Specialized | A, B1, C1 | NE TIPS | 0–24 | Of 356 children with a gestational age of <31 weeks, all were referred to EI and 283 were EI eligible. |
| Talmi et al. (2014) | Specialized | A, B1, B2, C1 | Urban hospital | 6–60 | Of 382 high-risk children, 128 were referred to EI, 38 were assessed, and 25 were EI eligible. |
Note. ~indicates approximate values calculated from data available in the publication; A = data on number of children from primary or specialized settings of whom a subset screened positive, were assessed, deemed eligible, or entered EI; B1 = number of children who were screened positive or referred for a developmental assessment, B2 = number of children who were assessed; C1 = number of children who were EI eligible; C2 = number of children who entered EI; SPED = special education; EI = early intervention; NHISD = National Health Interview Survey on Disability; PELL = Pregnancy and Early Life Longitudinal Study; VLBW = very low birth weight; ECLBS = Early Childhood Longitudinal Birth Study; IHRFUP = Iowa High Risk Follow Up Program; NICU = neonatal intensive care unit; IHDP = Infant Health and Development Program; LBW = low birth weight; UCLA = University of California at Los Angeles; EIPD = Early Intervention Program Division; CNRP = Community Notification and Referral Program; CWEST = Colorado Child Welfare Data Set; NSCAW = National Survey of Child and Adolescent Wellbeing; ELBW = Extremely Low Birth Weight; TIPS = tracking infant progress statewide; MECLI = Massachusetts Early Childhood Linkage Initiative; IFSP = Individualized Family Service Plan; NSCHCN = National Survey of Children’s Health Care Needs.
Indicates study with data from all three identification steps, including IFSP receipt.
Results
Steps in Identification Process
Forty-three studies (16 primary, 26 secondary) reported data on cohorts of children following the early identification steps that lead to Part C services described in Figure 1. Of those 43, 21 (nine primary, 12 secondary) reported data on all three steps of the early identification process and 22 reported data on only two (see Table 1). Of the 21 reporting on all three steps, only seven reported data on actual IFSP receipt.
Model Systems
Only two systems were identified that met criteria for a “model system.” The Pregnancy to Early Life Longitudinal (PELL) Data System from Massachusetts was identified from published reports that included all the key data points in the model for children from general population (primary) settings (Barfield et al., 2008; Clements et al., 2007; Clements et al., 2006; Clements et al., 2008; Derrington, 2012; Manning et al., 2011). The PELL Data System was a project by Boston University School of Public Health and the Massachusetts Department of Public Health in collaboration with the Centers for Disease Control and Prevention. PELL linked data systems from birth records, death records, and hospital records, and provides both cross-sectional and longitudinal data on the population of children screened, referred, and assessed/eligible for Part C EI services, as well as other social service systems (e.g., women, infants, and children). Furthermore, the PELL is unique in that can track subsets of children from high-risk groups such as children with autism (Manning et al., 2011) and VLBW children (Barfield et al., 2008).
Nebraska uses a data system for specialized settings: the Developmental Tracking Infant Progress Statewide (NE TIPS) program (Jackson & Needelman, 2007; Roberts, Needelman, Jackson, McMorris, & Munyon, 2014). The NE TIPS program was jointly developed by the Nebraska Departments of Education and Health and Human Services for tracking neonatal intensive care unit (NICU) infants. Authors report information on the project funding sources, NICU enrollment, screening, and referral and follow-up processes. The NE TIPS system involves three levels of follow-up for NICU infants at specified times from 6 months to 3 years. Level 1 is for low-risk infants whose parents receive developmental screening with validated screeners. Level 2 is for moderate-risk infants (e.g., low birth weight) who receive more detailed, but brief developmental assessments (e.g., the Bayley Infant Neurological Screener, the Communication Symbolic Behavior System, and the Brigance Preschool Screen). Level 3 is for high-risk infants (e.g., VLBW) and involves a comprehensive developmental assessment with the Bayley Scales of Infant Development–II. Authors report the number of children from each level who screen positive and enter EI. Furthermore, recent data reported from TIPS illustrate its utility for assessing important community-based factors, such as differences among urban and rural VLBW children in terms of EI eligibility (Roberts et al., 2014).
Descriptive Characteristics
Table 2 displays descriptive characteristics that may be interesting to some readers (sorted chronologically by primary or specialized settings). One interesting trend identified in these data is that since 2006, the number of publications on EI early identification systems has dramatically increased, predominately from the medical literature. Otherwise, the characteristics of studies conducted in primary and specialized settings were largely similar. However, historically, there is little research on early identification leading to EI eligibility in primary settings, but a steady stream of research from specialized settings. Finally, studies using primary settings mostly came from the medical literature, with a few studies from development/disability or education journals; studies using specialized settings mostly came from medical and education journals, with a few from development/disability journals.
Discussion
Despite a sizable literature on psychometric screener development, evaluation assessment development, and interventions, this review only identified 43 empirical reports reporting data on two or more aspects of community systems following a population of children from initial developmental concern through screening, assessment, eligibility, and receipt of services. Results of this review point out significant gaps in the current understanding of how integrated Part C early identification systems are within local communities or Part C’s effectiveness at tracking children from community settings from initial concerns through referrals, assessments, and ultimately EI receipt. However, the authors identified two model systems that may serve as references for policy makers and researchers seeking to improve and develop more effective early identification systems for Part C services.
Data From Population to EI Services
Ideally, data on the process of early identification to Part C EI services would be available through state Child Find programs. In sharp contrast to the minimal required reporting on Child Find efforts, Congress requires much more detailed post-referral data (e.g., demographics, EI outcomes). Similarly, the peer-reviewed literature tends to focus on data collected post-referral, with few studies reporting pre-screening/referral data on a community cohort of children (e.g., Lynch, Mercury, DiCola, & Widley, 1988; Mott & Dunst, 2006; Scarborough, Lloyd, & Barth, 2009; Shapiro & Derrington, 2004). Ultimately, the dearth of available data prevents a rigorous assessment of the effectiveness of Part C early identification systems.
In addition to data collection issues, federal regulations for Child Find activities are minimal, and this review indicates that implementation of activities varies across states. For example, some states conduct systematic developmental monitoring of all children, regardless of a child’s risk of developmental delays or disabilities (e.g., Barfield et al., 2008), and other states only monitor children who are at high risk (e.g., Shannon & Anderson, 2008). Thus, two states may be similar in the number and type of conditions that qualify children for EI, but differ in the proportion of children receiving services due to whether states target primary or secondary populations. These differences may be exacerbated by whether states adopt proactive Child Find strategies, such as electronic tracking systems linking medical and education databases (e.g., Clements et al., 2008), or more passive strategies, such as public announcements or making flyers available (Bricker et al., 2013; Fulton, 2006). The capacity to evaluate the collective impact of these policies on the number of children enrolled in EI is not possible on a national level due to the authorization limitations related to Child Find activities.
Model Systems
This review identified primary and specialized model state early identification systems that track community cohorts from monitoring to receipt of EI services. The PELL system serves as the primary population model for successfully linking existing systems for developmental monitoring and Child Find purposes (Barfield et al., 2008; Clements et al., 2007; Clements et al., 2006; Clements et al., 2008; Derrington, 2012; Manning et al., 2011). Because Massachusetts’s Part C lead agency is housed in the Department of Public Health (Bricker et al., 2013), this may have facilitated the PELL system’s ability to link state birth, death, and hospital records to data on Part C referral and EI entrance. Emulating the success of this program is a promising route for other states to consider. The NE TIPS program (Jackson & Needelman, 2007) serves as a model for tracking NICU survivors (i.e., specialized setting) from monitoring to EI service receipt. Unlike the PELL, which highlights the importance of linking data systems, the NE TIPS program highlights the importance of using developmental screeners to monitor development. The use of reliable and valid screeners is crucial to the Child Find process (AAP et al., 2006; Bricker et al., 2013). Furthermore, recent data from TIPS indicate how this system may be used to assess and address within-state discrepancies. Specifically, Roberts et al. (2014) used TIPS data to determine that NE children living in rural areas were 3 times more likely than urban children to be assessed eligible for EI. Such analyses will be useful for NE Part C administrators and policy makers to address discrepancies and identify and remedy the potential causes of these differences.
Whereas the identified model systems underscore the importance of partnerships for Child Find (e.g., PELL with federal, state, and local organizations), other systems also provide important considerations for Part C Child Find. For example, a report from Shannon and Anderson (2008) details a community engagement plan emphasizing (a) relationship building between Part C specialists and potential community monitoring sites, (b) the development of a collaborative agreement plan, (c) buy-in from and training of front-line workers, (d) screening implementation, and (e) debriefing and referral processes for families. In addition, data from Head Start programs (Peterson et al., 2004; Sinclair, 1993) indicate how Part C Child Find coordinators may collaborate with other early childhood programs that also track children’s developmental progress. The data from the Head Start program from the University of California–Los Angeles underscore the point that non-Part C systems can track outcomes for specialized populations (Peterson et al., 2004; Sinclair, 1993).
Collectively, these systems illustrate the complex and collaborative nature of community-based developmental monitoring. Foremost, developmental monitoring systems require collaborations between multiple federal, state, and local institutions. In addition, data systems should allow Child Find to track data on community monitoring efforts for entire birth-to-three populations from monitoring, screening, referral, developmental assessment, identification, and EI receipt. As this conversation progresses, researchers and policy makers may build on the successes of these recent groundbreaking examples.
Limitations and Future Directions
Like any quantitative review, this study has several limitations. In particular, narrowing the scope to studies citing Part C laws in introduction sections undoubtedly screened out studies investigating issues relevant to Child Find systems (e.g., Hix-Small, Marks, Squires, & Nickel, 2007); however, this step allowed the authors to ascertain the impact of IDEA Part C via citations in studies addressing developmental monitoring systems. Another limitation is the decision not to include data from studies using national surveys (e.g., Feinberg, Silverstein, Donahue, & Bliss, 2011), which are not systems per se. The reasoning for this was that these surveys might be adapted for the purposes of monitoring; however, some might maintain that this is an overly liberal generalization of the concept of “system.” As with any developed coding protocol, the one used in this study is limited in its scope, and future researchers may want to investigate this literature with items not included in the coding scheme used here. Finally, it should be noted that this article’s operational definitions for ease of data identification do not indicate judgments of study quality. Authors chose not to assess study quality as the purpose of the studies included here varied widely and represented different fields across 30 years. Ease of data identification definitions is simply meant to indicate the degree of difficulty authors had in identifying and abstracting numerical data.
Conclusion
This systematic review identified 43 studies reporting on data following cohorts of children from indication of developmental concern to delay or disability identified, and summarized the data based on setting, either primary or specialized. Currently, there is a dearth of available data on Child Find, thereby limiting a thorough evaluation of the effectiveness of current systems to both monitor those at risk and identify those with developmental delays and disabilities. Thus, to understand the early identification process, more systematic data are needed following population cohorts from developmental monitoring, screening, assessment, all the way through entrance into EI services. Without such data, it is impossible for policy makers to make databased decisions to improve Child Find systems or judge the effectiveness of early identification systems. The good news is that transparent and detailed data on Child Find systems are beginning to be disseminated; hopefully, this will result in more active research on this topic. Interested readers should direct their attention to the two recent model systems identified in this review: MA PELL and NE TIPS. These model systems include data tracking population (PELL) and specialized (TIPS) cohorts all the way from community monitoring to EI receipt.
Supplementary Material
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: From July 2013 to June 2015, Barger was supported by a Policy Research Fellowship sponsored by the University of South Carolina Disability Research and Dissemination Center in collaboration with the Centers for Disease Control and Prevention’s National Center on Birth Defects and Developmental Disabilities, “Learn the Signs. Act Early.” program. Since August 2015, research support came from the Administration on Intellectual and Developmental Disabilities grant #90DD0662.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Asterisk indicates manuscript identified in systematic review.
- American Academy of Pediatrics, Council on Children With Disabilities, Section on Developmental Behavioral Pediatrics Bright Futures Steering Committee Medical Home Initiatives for Children With Special Needs Project Advisory Committee. Identifying infants and young children with developmental disorders in the medical home: An algorithm for developmental surveillance and screening. Pediatrics. 2006;118:405–420. doi: 10.1542/peds.2006-1231. [DOI] [PubMed] [Google Scholar]
- Bailey DB, Hebbeler K, Scarborough A, Spiker D, Mallik S. First experiences with early intervention: A national perspective. Pediatrics. 2004;113:887–896. doi: 10.1542/peds.113.4.887. [DOI] [PubMed] [Google Scholar]
- *.Barfield WD, Clements KM, Lee KG, Kotelchuck M, Wilber N, Wise PH. Using linked data to assess patterns of early intervention (EI) referral among very low birth weight infants. Maternal and Child Health Journal. 2008;12:24–33. doi: 10.1007/s10995-007-0227-y. [DOI] [PubMed] [Google Scholar]
- Blackman JA, Healy A, Ruppert ES. Participation by pediatricians in early intervention: Impetus from public law 99-457. Pediatrics. 1992;89:98–102. [PubMed] [Google Scholar]
- *.Blackman JA, Lindgren SD, Hein HA, Harper DC. Long-term surveillance of high-risk children. Archives of Pediatrics & Adolescent Medicine. 1987;141:1293–1299. doi: 10.1001/archpedi.1987.04460120055034. [DOI] [PubMed] [Google Scholar]
- Boyle CA, Boulet S, Schieve LA, Cohen RA, Blumberg SJ, Yeargin-Allsopp M, Kogan MD. Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics. 2011;127:1034–1042. doi: 10.1542/peds.2010-2989. [DOI] [PubMed] [Google Scholar]
- Bricker D, Macy M, Squires J, Marks K. Developmental screening in your community: An integrated approach for connecting children with services. Baltimore, MD: Brookes; 2013. [Google Scholar]
- *.Brinker RP, Frazier W, Lancelot B, Norman J. Identifying infants from the inner city for early intervention. Infants & Young Children. 1989;2(1):49–58. [Google Scholar]
- *.Casanueva CE, Cross TP, Ringeisen H. Developmental needs and individualized family service plans among infants and toddlers in the child welfare system. Child Maltreatment. 2008;13:245–258. doi: 10.1177/1077559508318397. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Summary of 2012 National CDC EHDI data. 2012 Retrieved from http://www.cdc.gov/ncbddd/hearingloss/2012-data/2012_ehdi_hsfs_summary_b.pdf.
- Child Abuse Prevention and Treatment Act of 2003, Pub. L. No. 108-36, 42 U.S.C. § 5106 (2003).
- *.Clements KM, Barfield WD, Ayadi MF, Wilber N. Preterm birth–associated cost of early intervention services: An analysis by gestational age. Pediatrics. 2007;119:e866–e874. doi: 10.1542/peds.2006-1729. [DOI] [PubMed] [Google Scholar]
- *.Clements KM, Barfield WD, Kotelchuck M, Lee KG, Wilber N. Birth characteristics associated with early intervention referral, evaluation for eligibility, and program eligibility in the first year of life. Maternal and Child Health Journal. 2006;10:433–441. doi: 10.1007/s10995-006-0080-4. [DOI] [PubMed] [Google Scholar]
- *.Clements KM, Barfield WD, Kotelchuck M, Wilber N. Maternal socio-economic and race/ethnic characteristics associated with early intervention participation. Maternal and Child Health Journal. 2008;12:708–717. doi: 10.1007/s10995-007-0291-3. [DOI] [PubMed] [Google Scholar]
- Cole M, Cole SR, Lightfoot C. The development of children. New York, NY: Macmillan; 2005. [Google Scholar]
- Danaher J, Armijo C, Lazara A. Part C Updates: Eighth in a series of updates on selected aspects of the Early Intervention Program for Infants and Toddlers With Disabilities, Part C of the Individuals With Disabilities Education Act (IDEA) National Early Childhood Technical Assistance Center; 2006. Retrieved from http://files.eric.ed.gov/fulltext/ED493101.pdf. [Google Scholar]
- *.Derrington TM. Development of the Drug-Exposed Infant Identification Algorithm (DEIIA) and its application to measuring Part C Early Intervention referral and eligibility in Massachusetts, 1998–2005. Maternal and Child Health Journal. 2012;17:1567–1575. doi: 10.1007/s10995-012-1157-x. [DOI] [PubMed] [Google Scholar]
- *.Derrington TM, Lippitt JA. State-level impact of mandated referrals from child welfare to Part C early intervention. Topics in Early Childhood Special Education. 2008;28:90–98. [Google Scholar]
- Derrington T, Spiker D, Hebbeler K, Diefendorf M. IDEA Part C and B 619 state data systems: Current status and future priorities. 2013 (Technical report for DASY: The Center for IDEA Early Childhood Systems). Retrieved from http://dasycenter.sri.com/downloads/DaSy_papers/DaSyNeedsAssessmentReport.pdf.
- *.Dunbar SB, Reed CN. A developmental screening program in primary health care: Meeting the challenges of children in low-income families. Infant-Toddler Intervention: The Transdisciplinary Journal. 1999;9:195–202. [Google Scholar]
- Dworkin PH. British and American recommendations for developmental monitoring: The role of surveillance. Pediatrics. 1989;84:1000–1010. [PubMed] [Google Scholar]
- *.Feinberg E, Silverstein M, Donahue S, Bliss R. The impact of race on participation in Part C Early intervention services. Journal of Developmental & Behavioral Pediatrics. 2011;32:284–291. doi: 10.1097/DBP.0b013e3182142fbd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Feldman HM, Ploof DL, Hofkosh D, Goehring EL. Developmental needs of infants and toddlers who require lengthy hospitalization. American Journal of Diseases of Children. 1993;147:211–215. doi: 10.1001/archpedi.1993.02160260101034. [DOI] [PubMed] [Google Scholar]
- Fulton JL. An investigation of state-level child find and public awareness campaigns to promote early intervention to the medical community. Doctoral dissertation. 2006 Retrieved from http://drum.lib.umd.edu/bitstream/handle/1903/3757/umi-umd-3595.pdf;jsessionid=87977F4588611D095610FE5644CF2593?sequence=1.
- Hix-Small H, Marks K, Squires J, Nickel R. Impact of implementing developmental screening at 12 and 24 months in a pediatric practice. Pediatrics. 2007;120:381–389. doi: 10.1542/peds.2006-3583. [DOI] [PubMed] [Google Scholar]
- Individuals With Disabilities Education Improvement Act of 2004, 20 U.S.C. § 1400 et seq. (2004)
- *.Jackson BJ, Needelman H. Building a system of child find through a 3-tiered model of follow-up. Infants & Young Children. 2007;20:255–265. [Google Scholar]
- *.Kang R, Barnard K, Oshio S. Description of the clinical practice of advanced practice nurses in family-centered early intervention in two rural settings. Public Health Nursing. 1994;11:376–384. doi: 10.1111/j.1525-1446.1994.tb00202.x. [DOI] [PubMed] [Google Scholar]
- King TM, Glascoe FP. Developmental surveillance of infants and young children in pediatric primary care. Current Opinion in Pediatrics. 2003;15:624–629. doi: 10.1097/00008480-200312000-00014. [DOI] [PubMed] [Google Scholar]
- *.Kirby RS, Swanson ME, Kelleher KJ, Bradley RH, Casey PH. Identifying at-risk children for early intervention services: Lessons from the Infant Health and Development Program. The Journal of Pediatrics. 1993;122:680–686. doi: 10.1016/s0022-3476(06)80004-1. [DOI] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- *.Lynch EC, Mercury MG, DiCola JM, Widley R. The function of a central referral system in inter-agency identification, eligibility, and service delivery: A case study. Topics in Early Childhood Special Education. 1988;8(3):86–97. [Google Scholar]
- *.Manning SE, Davin CA, Barfield WD, Kotelchuck M, Clements K, Diop H, Smith LA. Early diagnoses of autism spectrum disorders in Massachusetts birth cohorts, 2001–2005. Pediatrics. 2011;127:1043–1051. doi: 10.1542/peds.2010-2943. [DOI] [PubMed] [Google Scholar]
- *.Marshall J, Mendez LMR. Following up on community-based developmental screening: Do young children get the services they need? Infants & Young Children. 2014;27:276–291. [Google Scholar]
- *.McManus B, McCormick MC, Acevedo-Garcia D, Ganz M, Hauser-Cram P. The effect of state early intervention eligibility policy on participation among a cohort of young CSHCN. Pediatrics. 2009;124(Suppl 4):S368–S374. doi: 10.1542/peds.2009-1255G. [DOI] [PubMed] [Google Scholar]
- *.McManus BM, Magnusson D, Rosenberg S. Restricting State Part C eligibility policy is associated with lower early intervention utilization. Maternal and Child Health Journal. 2014;18:1031–1037. doi: 10.1007/s10995-013-1332-8. [DOI] [PubMed] [Google Scholar]
- *.McManus BM, Rosenberg SA. Does the persistence of development delay predict receipt of early intervention services? Academic Pediatrics. 2012;12:546–550. doi: 10.1016/j.acap.2012.07.003. [DOI] [PubMed] [Google Scholar]
- *.Meade VA, Sweeney JK, Chandler LS, Woodward BJ. Identifying 4-month-old infants at risk in community screening. Pediatric Physical Therapy. 2009;21:150–157. doi: 10.1097/PEP.0b013e3181a3a01c. [DOI] [PubMed] [Google Scholar]
- *.Montgomery A, Miller L. Using the Colorado birth defects monitoring program to connect families with services for children with special needs. Teratology. 2001;64(Suppl 1):S42–S46. doi: 10.1002/tera.1098. [DOI] [PubMed] [Google Scholar]
- *.Mott DW, Dunst CJ. Use of presumptive eligibility for enrolling children in Part C early intervention. Journal of Early Intervention. 2006;29:22–31. [Google Scholar]
- *.Peterson CA, Wall S, Raikes HA, Kisker EE, Swanson ME, Jerald J, Qiao W. Early head start identifying and serving children with disabilities. Topics in Early Childhood Special Education. 2004;24:76–88. [Google Scholar]
- Pulsifer MB, Hoon AH, Palmer FB, Gopalan R, Capute AJ. Maternal estimates of developmental age in preschool children. The Journal of Pediatrics. 1994;125(1):S18–S24. doi: 10.1016/s0022-3476(94)70171-7. [DOI] [PubMed] [Google Scholar]
- *.Roberts H, Needelman H, Jackson B, McMorris C, Munyon A. Effect of community size on eligibility for early intervention for infants with a neonatal intensive care experience. The Journal of Rural Health. 2014;30:259–264. doi: 10.1111/jrh.12055. [DOI] [PubMed] [Google Scholar]
- *.Robinson CC, Rosenberg SA. Child welfare referrals to Part C. Journal of Early Intervention. 2004;26:284–291. [Google Scholar]
- *.Rojahn J, Aman MG, Marshburn E, Moeschberger ML, King EH, Logsdon DA, Schroeder SR. Biological and environmental risk for poor developmental outcome of young children. American Journal on Mental Retardation. 1993;97:702–708. [PubMed] [Google Scholar]
- *.Rosenberg SA, Robinson CC, Shaw EF, Ellison MC. Part C early intervention for infants and toddlers: Percentage eligible versus served. Pediatrics. 2013;131:38–46. doi: 10.1542/peds.2012-1662. [DOI] [PubMed] [Google Scholar]
- *.Rosenberg SA, Smith EG. Rates of Part C eligibility for young children investigated by child welfare. Topics in Early Childhood Special Education. 2008;28:68–74. [Google Scholar]
- *.Rosenberg SA, Zhang D, Robinson CC. Prevalence of developmental delays and participation in early intervention services for young children. Pediatrics. 2008;121:e1503–e1509. doi: 10.1542/peds.2007-1680. [DOI] [PubMed] [Google Scholar]
- *.Scarborough AA, Lloyd EC, Barth RP. Maltreated infants and toddlers: Predictors of developmental delay. Journal of Developmental & Behavioral Pediatrics. 2009;30:489–498. doi: 10.1097/DBP.0b013e3181c35df6. [DOI] [PubMed] [Google Scholar]
- *.Scarborough AA, McCrae JS. Maltreated infants reported eligibility for Part C and later school-age special education services. Topics in Early Childhood Special Education. 2008;28:75–89. [Google Scholar]
- *.Shannon P, Anderson PR. Developmental screening in community health care centers and pediatric practices: An evaluation of the Baby Steps Program. Intellectual and Developmental Disabilities. 2008;46:281–289. doi: 10.1352/1934-9556(2008)46[281:DSICHC]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- *.Shapiro BJ, Derrington TM. Equity and disparity in access to services: An outcomes-based evaluation of early intervention child find in Hawaii. Topics in Early Childhood Special Education. 2004;24:199–212. [Google Scholar]
- Shelov SP, Hanneman RE. Caring for your baby and young child: Birth to age 5. The complete and authoritative guide. New York, NY: Broadway; 1993. [Google Scholar]
- Sices L, Egbert L, Mercer MB. Sugar-coaters and straight talkers: Communicating about developmental delays in primary care. Pediatrics. 2009;124:e705–e713. doi: 10.1542/peds.2009-0286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Simpson GA, Colpe L, Greenspan S. Measuring functional developmental delay in infants and young children: Prevalence rates from the NHIS-D. Paediatric and Perinatal Epidemiology. 2003;17:68–80. doi: 10.1046/j.1365-3016.2003.00459.x. [DOI] [PubMed] [Google Scholar]
- *.Sinclair E. Early identification of preschoolers with special needs in Head Start. Topics in Early Childhood Special Education. 1993;13:184–201. [Google Scholar]
- *.Solomon R, Clougherty SL, Shaffer D, Hofkosh D, Edwards M. Community-based developmental assessment sites: A new model for pediatric “child-find” activities. Infants & Young Children. 1994;7(2):67–71. [Google Scholar]
- *.Stahmer AC, Leslie LK, Hurlburt M, Barth RP, Webb MB, Landsverk J, Zhang J. Developmental and behavioral needs and service use for young children in child welfare. Pediatrics. 2005;116:891–900. doi: 10.1542/peds.2004-2135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Talmi A, Bunik M, Asherin R, Rannie M, Watlington T, Beaty B, Berman S. Improving developmental screening documentation and referral completion. Pediatrics. 2014;134:e1181–e1188. doi: 10.1542/peds.2012-1151. [DOI] [PubMed] [Google Scholar]
- *.Tang BG, Feldman HM, Huffman LC, Kagawa KJ, Gould JB. Missed opportunities in the referral of high-risk infants to early intervention. Pediatrics. 2012;129:1027–1034. doi: 10.1542/peds.2011-2720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Education. 33rd annual report to Congress on the implementation of the Individuals With Disabilities Act, 2009. 2012 Retrieved from http://www2.ed.gov/about/reports/annual/osep/2011/parts-b-c/33rd-idea-arc.pdf.
- *.Wang CJ, Elliott MN, Rogowski J, Lim N, Ratner JA, Schuster MA. Factors influencing the enrollment of eligible extremely-low-birth-weight children in the Part C early intervention program. Academic Pediatrics. 2009;9:283–287. doi: 10.1016/j.acap.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White KR, Blaiser KM. Strategic planning to improve EHDI programs. Volta Review. 2011;111(2):83–108. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.