Case report
KEY TEACHING POINTS
|
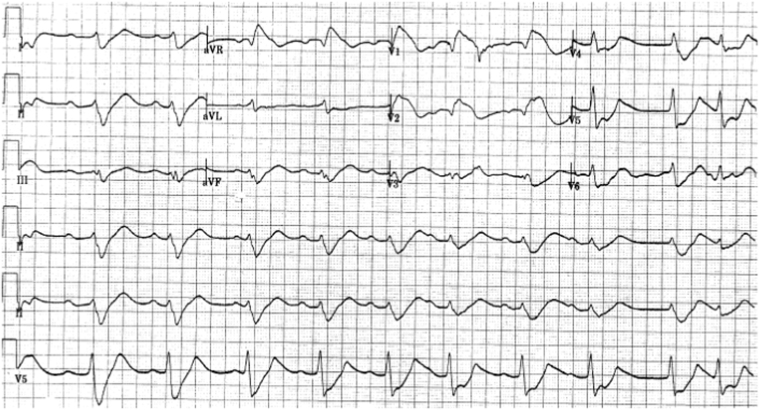
Ms. A is a 33-year-old woman with a history of depression and polysubstance use disorder who presented to our hospital after transfer from another facility’s emergency department after an intentional flecainide overdose. Her spouse heard a “thud” at approximately 5 AM on the day of admission. He found her unconscious after she had ingested 12 tablets of 150-mg flecainide originally prescribed to him. She was taken to another facility, where she was found to be in a wide complex rhythm with a heart rate of 63 (Figure 1) and blood pressure of 69/29. She was given 1 L normal saline, started on 2 μg/kg/min of dobutamine, and electively intubated for airway protection in the setting of altered mental status. Promptly after intubation, she developed pulseless ventricular tachycardia (VT), which necessitated initiation of advanced cardiac life support. During this process, she received 11 ampules of sodium bicarbonate, was started on intravenous (IV) isotonic sodium bicarbonate at 150 cc/h, and given a 500-cc bolus of IV fat emulsion. At this point, return of spontaneous circulation was obtained, and the dobutamine infusion was stopped.
Figure 1.
ECG on presentation.
On arrival to our hospital, the patient was noted to be in an irregular, wide complex tachycardia; otherwise her physical examination was unremarkable. Result of laboratory studies were notable for Na 160, K 3.0, HCO3 50, Cr 0.78, and iCal 0.77. Her blood gas values were pH 7.71, Paco2 48, and Pao2 166 on 100% Fio2. During the early part of her course, she received another 11 ampules of bicarbonate, and her bicarbonate gtt was uptitrated to 300 cc/h. With this treatment, her ECG stabilized to a junctional rhythm at 82 bpm with intermittent runs of hemodynamically stable, slow VT. Given her high pH, additional bicarbonate was not administered. She was given another 1000 cc of IV fat emulsion.
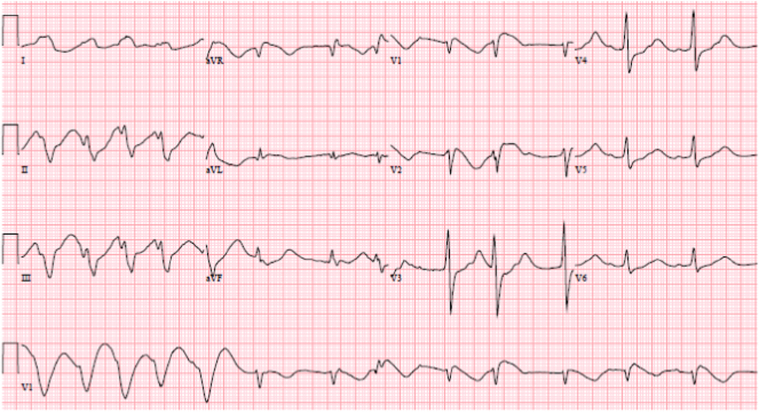
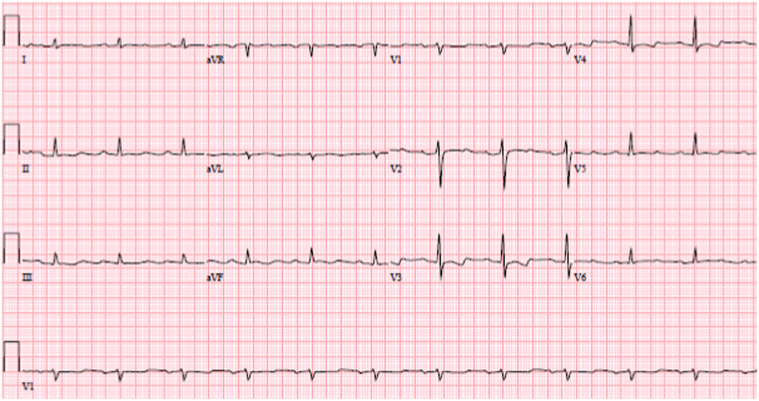
During the day she became bradycardic, with heart rates into the 40s, and was refractory to atropine. Despite the development of atrial fibrillation with frequent premature ventricular complexes and an extremely prolonged QTc of approximately 700 ms (Figure 2), her hemodynamic status remained stable on vasopressin 0.04 units and phenylephrine 100 μg/min. Approximately 14 hours after arrival to our hospital, she became more hemodynamically unstable and was refractory to multiple defibrillations. Her rhythm twice devolved into pulseless electrical activity but recovered each time after advanced cardiac life support to a monomorphic VT. At this time, the decision was made to cannulate for venoarterial extracorporeal membrane oxygen (VA-ECMO) support for refractory VT and shock. During cannulation, her hemodynamics were supported with a norepinephrine gtt and IV pushes of epinephrine. Initial rates of VA-ECMO were approximately 4 L/min. During her time on VA-ECMO, the patient received a total of 8 units of packed red blood cells and 8 units of fresh frozen plaza, believed secondary to blood loss. Approximately 72 hours after cannulation, her ECG normalized to normal sinus rhythm with first-degree AV block and nonspecific ST/TW changes (Figure 3). She was weaned and decannulated from VA-ECMO. Upon decannulation, she was weaned off sedation and extubated uneventfully before transfer to a psychiatric facility for further treatment of her depression. Approximately 2 months after discharge, her neurologic function is intact.
Figure 2.
ECG before venoarterial extracorporeal membrane oxygen (VA-ECMO) cannulation.
Figure 3.
ECG before venoarterial extracorporeal membrane oxygen (VA-ECMO) decannulation.
Discussion
We report the longest successful use of VA-ECMO for treatment of flecainide overdose and the first successful use of VA-ECMO for flecainide overdose in the United States. Flecainide is a class IC antiarrhythmic drug, a class of medications whose overdose is associated with approximately 20% mortality.1 Flecainide causes rate-dependent slowing of the fast sodium current INa during phase 0 of the cardiac action potential as well as inhibition of the rectifier potassium current IKr during phase 3.2, 3, 4 Flecainide overdose is difficult to treat because of the drug’s high oral bioavailability (90%), high volume of distribution (8–9 L/kg), long half- life (up to 23 hours), poor ability to be dialyzed, lack of an antidote, and rapid onset of shock and arrhythmias (as early as 30 minutes after ingestion).1, 5, 6
Flecainide overdose is relatively rare, and the literature on its treatment is limited to animal studies and case reports. Initial management consists of careful monitoring of vital signs, telemetry, aggressive IV fluids, repletion of electrolytes, and admission to the intensive care unit. Because of flecainide’s high oral bioavailability, treatment may include gastric lavage if the patient presents within 1 hour of ingestion and activated charcoal regardless of the time to presentation.1, 6 Our patient did not receive gastric lavage because she presented to our hospital more than 1 hour after ingestion. Multiple studies support the early and ample use of hypertonic sodium bicarbonate,2, 3, 5, 7 which has been reported in doses up to 350 mEq5 for a goal pH of 7.5–7.55 or a goal QRS width <160 ms.1 A high sodium concentration is theorized to antagonize flecainide at sodium channels on cardiac myocytes.5 Flecainide is a weak base, and alkalization of the blood may decrease the ionized form of flecainide, which binds sodium channels.2, 7 Recent literature supports the use of IV fat emulsion (100 mL or 1.5 mL/kg of 20% IV fat emulsion) to decrease the volume of distribution of fat-soluble medications such as flecainide.8
Flecainide can induce rapid arrhythmias, particular bradyarrhythmias, heart block, VT, ventricular fibrillation, and pulseless electrical activity.5, 9 These rhythms may be refractory to electrical cardioversion.8, 10, 11 Treatment options include atropine or a pacemaker for bradyarrhythmias, although capture may be difficult.10, 12, 13 For tachyarrhythmias, there have been reports of success with lidocaine for sustained VT, although the theoretical risk of interaction between class IB and IC agents remains high.14 Another report from Germany reported success with amiodarone for treatment of refractory ventricular fibrillation,11 and a separate review suggested antitachycardia treatment with a pacemaker or isoproterenol if needed.1 Because of flecainide’s ability to cause both bradyarrhythmias and tachyarrhythmias, clinicians should be cautious when monitoring for therapeutic interventions causing overcompensation (ie, bradyarrhythmia becoming a tachyarrhythmia and vice versa).
Shock can develop rapidly in flecainide overdose due to chronotropic and inotropic incompetence.2, 4 Use of vasopressors such as phenylephrine is difficult because of reflex bradycardia. Use of inotropic agents may be limited by the rate-dependent effect of flecainide as well as the risk of precipitating ventricular arrhythmias. There have been reports of use of assist devices to support individuals through flecainide-induced cardiogenic shock. Timperley et al4 published the first and only successful use of an intra-aortic balloon pump for a patient treated as having cardiogenic shock from a myocardial infarction, which was diagnosed after discharge as a flecainide overdose. In the first description of VA-ECMO for flecainide overdose, Yasui et al15 showed that 10 hours of VA-ECMO lowered flecainide levels (peak 5.45 μg/mL) after ingestion of an unknown quantity of medication. However, care was withdrawn after the patient was found to have poor neurologic function. The report argued for the use of VA-ECMO in shock to maintain perfusion to the liver, which sustains flecainide clearance. The first successful report using VA-ECMO was in 1999 from Australia, where VA-ECMO was used for 30 hours for a 4-g ingestion.13 The patient survived to discharge with normal neurologic function. In the second successful report, also from Australia, VA-ECMO was used for 26 hours for a 6-g ingestion, and the authors argue that VA-ECMO time >36 hours is unlikely to be required.12 The use of VA-ECMO in these reports was complicated by bleeding and hematoma formation requiring blood products,12, 13, 15 similar to our experience.
To our knowledge, this is the first case report of VA-ECMO time >36 hours for treatment of flecainide overdose and the first successful use of VA-ECMO for flecainide overdose in the United States. This reports shows that a longer duration of VA-ECMO (up to 72 hours) may be required for flecainide overdose. A longer duration of VA-ECMO can lead to survival with resulting normal neurologic function.
In treatment of flecainide overdose, our review of the literature suggests that initial care should include careful monitoring of vital signs with admission to the intensive care unit, administration of activated charcoal, repletion of electrolytes, aggressive use of IV fluids and hypertonic sodium bicarbonate, and the potential use of IV fat emulsion. Flecainide overdose can rapidly cause arrhythmias and shock, which if refractory to medications (antiarrhythmics, vasopressors) and electricity (pacing, cardioversion) will require mechanical circulatory support, most commonly VA-ECMO. We recommend early evaluation of the patient by the ECMO team because VA-ECMO, even of sustained duration, appears to be a lifesaving intervention for refractory cardiogenic shock due to flecainide overdose.
References
- 1.Cheung I., Man C. Review on flecainide poisoning. Hong Kong J Emerg Med. 2002;9:150–153. [Google Scholar]
- 2.Rognoni A., Bertolazzi M., Peron M. Electrocardiographic changes in a rare case of flecainide poisoning: a case report. Cases J. 2009;2:9137. doi: 10.1186/1757-1626-2-9137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lovecchio F., Berlin R., Brubacher J.R., Sholar J.B. Hypertonic sodium bicarbonate in an acute flecainide overdose. Am J Emerg Med. 1998;16:534–537. doi: 10.1016/s0735-6757(98)90013-4. [DOI] [PubMed] [Google Scholar]
- 4.Timperley J., Mitchell A.R., Brown P.D., West N.E. Flecainide overdose—support using an intra-aortic balloon pump. BMC Emerg Med. 2005;5:10. doi: 10.1186/1471-227X-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Devin R., Garrett P., Anstey C. Managing cardiovascular collapse in severe flecainide overdose without recourse to extracorporeal therapy. Emerg Medicine Austr. 2007;19:155159. doi: 10.1111/j.1742-6723.2006.00909.x. [DOI] [PubMed] [Google Scholar]
- 6.Gotz D., Pohle S., Barckow D. Primary and secondary detoxification in severe flecainide intoxication. Intensive Care Med. 1991;17:181184. doi: 10.1007/BF01704725. [DOI] [PubMed] [Google Scholar]
- 7.Goldman M.J., Mowry J.B., Kirk M.A. Sodium bicarbonate to correct widened QRS in a case of flecainide overdose. J Emerg Med. 1997;15:183–186. doi: 10.1016/s0736-4679(96)00345-9. [DOI] [PubMed] [Google Scholar]
- 8.Ellsworth H., Stellpflug S.J., Cole J.B., Dolan J.A., Harris C.R. A life-threatening flecainide overdose treated with intravenous fat emulsion. Pacing Clin Electrophysiol. 2013;36:e87–e89. doi: 10.1111/j.1540-8159.2012.03485.x. [DOI] [PubMed] [Google Scholar]
- 9.Kolecki P.F., Curry S.C. Poisoning by sodium channel blocking agents. Crit Care Clin. 1997;13:829–848. doi: 10.1016/s0749-0704(05)70371-7. [DOI] [PubMed] [Google Scholar]
- 10.Bauman J.L., Gallastegui J., Tanenbaum S.R., Hariman R.J. Flecainide-induced sustained ventricular tachycardia successfully treated with lidocaine. Chest. 1987;92:573–575. doi: 10.1378/chest.92.3.573. [DOI] [PubMed] [Google Scholar]
- 11.Siegers A., Board P.N. Amiodarone used in successful resuscitation after near-fatal flecainide overdose. Resuscitation. 2002;53:105–108. doi: 10.1016/s0300-9572(01)00503-2. [DOI] [PubMed] [Google Scholar]
- 12.Auzinger G.M., Scheinkestel C.D. Successful extracorporeal life support in a case of severe flecainide intoxication. Crit Care Med. 2001;29:887–890. doi: 10.1097/00003246-200104000-00041. [DOI] [PubMed] [Google Scholar]
- 13.Corkeron M.A., van Heerden P.V., Newman S.M., Dusci L. Extracorporeal circulatory support in near-fatal flecainide overdose. Anaesth Intens Cre. 1999;27:405–408. doi: 10.1177/0310057X9902700413. [DOI] [PubMed] [Google Scholar]
- 14.Hanley N.A., Bourke J.P., Gascoigne A.D. Survival in a case of life-threatening flecainide overdose. Intensive Care Med. 1998;24:740–742. doi: 10.1007/s001340050655. [DOI] [PubMed] [Google Scholar]
- 15.Yasui R.K., Culclasure T.F., Kaufman D., Freed C.R. Flecainide overdose: is cardiopulmonary support the treatment? Ann Emerg Med. 1997;29:680–682. doi: 10.1016/s0196-0644(97)70257-9. [DOI] [PubMed] [Google Scholar]