Introduction
The subcutaneous ICD (S-ICD) uses a different approach to sensing in comparison to conventional transvenous devices. A subcutaneous signal is used instead of an intracardiac signal. This may introduce new sensing issues as demonstrated by our case.
Case report
KEY TEACHING POINTS
|
A 37-year-old man was admitted after experiencing an out-of-hospital cardiac arrest due to ventricular fibrillation. He was successfully resuscitated and had good neurologic recovery. During admission, he was diagnosed with Brugada syndrome and received a subcutaneous implantable cardioverter-defibrillator (S-ICD; Boston Scientific, Marlborough, MA) using a standard technique.1 For the S-ICD implantation, a left lateral pocket was created for the generator. Two small incisions were made in the left parasternal area to secure the distal and proximal sensing electrodes of the lead system (Q-TRAK 3010EU, Boston Scientific), which had been tunneled subcutaneously. After the subcutaneous pockets were closed, automatic vector optimization was performed and the device chose the alternate vector for detection, which involves the proximal and distal sensing electrodes. Sustained ventricular fibrillation was induced with the patient under general anesthesia, and sinus rhythm was effectively restored with a submaximal 65-J polarity shock. The evening of the implantation, the patient experienced 2 inappropriate shocks due to oversensing of low-amplitude signals and artifact (Figure 1). The artifact could be reproduced by manipulation over the proximal electrode. Provocative maneuvers did not produce an artifact in the secondary vector (sensing between distal electrode and can); however, this vector was not suitable because of a low R/T ratio. Lateral chest radiography revealed entrapped subcutaneous air surrounding the proximal electrode (Figure 2). Four days after implantation, partial subcutaneous air resolution with no air surrounding the proximal electrode occurred. No artifact could be produced with provocative maneuvers. Complete air resolution occurred 10 days after implantation. The patient did not experience any inappropriate shocks during mid-term follow-up.
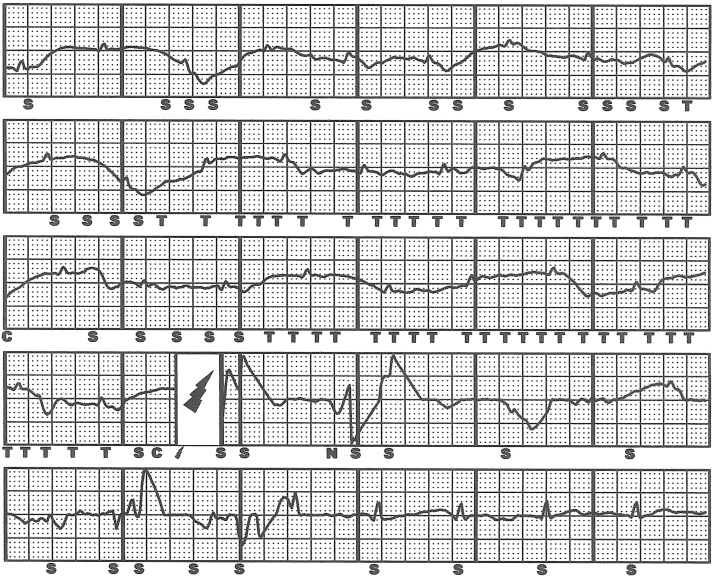
Figure 1.
Device electrogram at the time of an inappropriate shock showing oversensing of low-amplitude signals with subsequent shock. The alternate vector was used for sensing. Note baseline wandering of the electrogram.
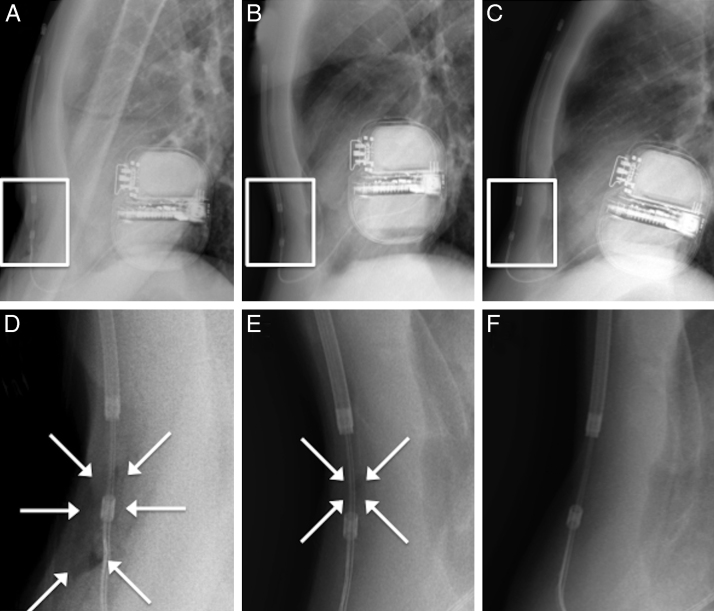
Figure 2.
Lateral chest radiography at day 0 (A, D), day 4 (B, E), and day 10 (C, F) after implantation. Note complete resolution of subcutaneous air (arrows) at the proximal sensing electrode during short-term follow-up.
Discussion
The S-ICD is a suitable alternative to a conventional transvenous ICD system. It avoids intravascular lead failures and minimizes operative complications. These benefits are especially important for young patients. Recent real-world data from the EFFORTLESS S-ICD registry demonstrated appropriate system performance with clinical event rates and inappropriate shock rates comparable to those reported for conventional ICDs.2 The 1-year inappropriate shock rate was 7%. The majority of inappropriate shocks were the result of oversensing (85%), especially from T-wave oversensing or oversensing due to low-amplitude signals.
The present case report shows that inappropriate shocks can occur early after implantation and highlights the importance of good tissue contact of the electrodes to prevent inappropriate shocks. The presence of air in the pocket insulates the sensing contact ring, causing inadequate sensing and low-amplitude signals, and thus oversensing from autogain.3 Care must be taken during implantation not to introduce air into the subcutaneous tissue. Boston Scientific has updated the user’s manual to prevent air entrapment (Personal Communication, November, 2014): “Good tissue contact with the electrode and pulse generator is important to optimize sensing and therapy delivery. Use standard surgical techniques to obtain good tissue contact. For example, keep the tissue moist and flushed with sterile saline, express any residual air out through the incisions prior to closing and, when closing the skin, take care not to introduce air into the subcutaneous tissue.”
Timely recognition of air entrapment is important to prevent early inappropriate shocks. Device interrogation during pocket manipulation immediately after implantation can identify air entrapment by the presence of noise. However, it is important to note that, in our case, sensing was normal immediately after implantation, raising the possibility that air entrapment occurred shortly after the procedure. Therefore, it is important to check the lateral chest radiograph the next day for air entrapment at the superior and inferior parasternal pockets. When air entrapment is diagnosed as the cause of oversensing, the device can be (temporarily) reprogrammed o use another vector, thus avoiding use of the affected sensing electrode. As demonstrated in our case, subcutaneous air usually resorbs within a few days.
References
- 1.Olde Nordkamp L.R., Dabiri Abkenari L., Boersma L.V., Maass A.H., de Groot J.R., van Oostrom A.J., Theuns D.A., Jordaens L.J., Wilde A.A., Knops R.E. The entirely subcutaneous implantable cardioverter-defibrillator: initial clinical experience in a large Dutch cohort. J Am Coll Cardiol. 2012;60:1933–1939. doi: 10.1016/j.jacc.2012.06.053. [DOI] [PubMed] [Google Scholar]
- 2.Lambiase P.D., Barr C., Theuns D.A. Worldwide experience with a totally subcutaneous implantable defibrillator: early results from the EFFORTLESS S-ICD Registry. Eur Heart J. 2014;35:1657–1665. doi: 10.1093/eurheartj/ehu112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zipse M.M., Sauer W.H., Varosy P.D., Aleong R.G., Nguyen D.T. Inappropriate shocks due to subcutaneous air in a patient with a subcutaneous cardiac defibrillator. Circ Arrhythm Electrophysiol. 2014;7:768–770. doi: 10.1161/CIRCEP.114.001614. [DOI] [PubMed] [Google Scholar]