Abstract
Universal health coverage generates significant health and economic benefits and enables governments to reduce inequity. Where universal health coverage has been implemented well, it can contribute to nation-building. This analysis reviews evidence from Asia and Pacific drawing out determinants of successful systems and barriers to progress with a focus on women and children. Access to healthcare is important for women and children and contributes to early childhood development. Universal health coverage is a political process from the start, and public financing is critical and directly related to more equitable health systems. Closing primary healthcare gaps should be the foundation of universal health coverage reforms. Recommendations for policy for national governments to improve universal health coverage are identified, including countries spending < 3% of gross domestic product in public expenditure on health committing to increasing funding by at least 0.3%/year to reach a minimum expenditure threshold of 3%.
Key questions.
What is already known about this topic?
Universal health coverage can generate significant health and economic benefits.
Despite costing more to national governments in the short term universal health coverage pays back its initial debt to national economic growth in multiples.
Access to healthcare contributes to early childhood development.
What are the new findings?
This analysis draws out determinants of successful universal health coverage systems and barriers to progress with a focus on women and children.
Next steps for governments are suggested in 10 policy recommendations to improve universal health coverage.
Key recommendations for policy
Invest in good quality accessible primary healthcare as the foundation of universal health coverage.
Countries spending <3% of GDP in public expenditure on health should commit to increase funding by at least 0.3%/year.
Introduction
Universal health coverage (UHC) can generate significant health and economic benefits to populations1 and enable governments to reduce inequity.2 Despite costing more to national governments in the short term, UHC pays back its initial debt to national economic growth in multiples. Access to healthcare is important for women and children, including establishing breastfeeding and immunisation, and contributes to early childhood development.
The Lancet Commission on Investing in Health in 2013 found that the economic benefits of achieving a grand convergence of global health outcomes for infectious diseases and for maternal and child health would outweigh the costs by a factor of between 9 and 20 over 20 years from 2015 to 2035.3 When implemented well UHC can contribute to nation-building.4–6 UHC has an important role to play in global health security efforts through building a strong frontline health system, strengthening access to vital services and funding robust surveillance systems.7–9
There is a huge wealth of technical and policy materials on UHC from Asia, and the rate of production has increased since UHC was formalised as a sustainable development goal target. This analysis synthesises the best available evidence to inform political decision-makers in Asia and Pacific by identifying critical lessons emerging from the region and suggesting policy recommendations. A summary of the methods used is shown in box 1.
Box 1. Methodological approach.
Structured literature search including grey literature. Keywords used for searching PubMed, Google Scholar, and United Nations publication banks. Documents were selected based on relevance to UHC, Asia and Pacific, and maternal and child health.
Interviews with more than 35 stakeholders across the region to identify policy priorities and lessons from experience.
Data review including health financing data and progress made in delivering health outcomes for women and children for the countries of Asia and Pacific.
What is UHC?
UHC is defined by the WHO as a means to ensuring that “all people obtain the health services they need without suffering financial hardship when paying for them”.10 UHC combines two benefits: first, everyone is covered by a package of good quality health services; and, second, UHC provides financial protection from healthcare costs.
Several critical elements underpin UHC, including an efficient, equitable and resilient health system; a financing system that does not impoverish users; access to essential medicines and technologies; sufficient numbers of motivated and skilled health workers; efficient administrative and governance arrangements; and transparency in tracking progress. Achieving UHC requires countries to advance health services. The proportion of the population covered should extend to encompass all people in a country (universal population coverage). The range of services covered should expand as resources permit, including sufficient investment in essential public health functions. Services must be accessible and be of adequate quality to be effective. And, the proportion of the financing required to deliver services should be increasingly drawn from pooled funds raised through compulsory prepayment mechanisms, including general or specific taxation or public social insurance.
UHC has increasingly become the focus of the global health agenda.11 In 2012, Margaret Chan called UHC, “the single most powerful concept that public health has to offer”.12 Adopting and sustaining a UHC system is as much a political process as a technical one. UHC begins with and is sustained by genuine political commitment by national leaders. Choosing how to advance UHC is different in each country's context, but countries that have made progress with UHC have experienced a range of benefits (table 1).
Table 1.
| Health benefits | Broad health coverage leads ‘to better access to necessary care and improved population health, with the largest gains accruing to poorer people’.15 A study by Imperial College, London found that a 10% increase in pooled government health spending led to a reduction of almost 8 deaths per 1000 children under 5. Universal health coverage improves outcomes fastest among the poorest and most marginalised districts, supporting equity and reducing or eliminating disparities within populations.16 |
| Health system benefits | UHC can act as a driver of sustaining investments aimed at strengthening health systems, overcoming bottlenecks and, in particular, improving the availability and performance of healthcare workers and essential medicines and supplies.17 |
| Economic benefits | Healthier populations support economic growth while unhealthy populations, particularly those afflicted with preventable diseases, can slow down and even stall economic growth.18 With the use of ‘value life years’ to estimate the economic benefits, over the period 2015–2035 these benefits would exceed costs by a factor of about 9–20 for infectious diseases and for maternal and child health.3 It is estimated that every year 100 million households fall into poverty because of medical and health expenses.19 |
| Political benefits | As a political process, UHC requires strong redistributive policies and actions by the state and transparent processes for allocation of resources across different interest groups. Many politicians have found that extending health coverage to underserved populations is a popular policy and attracts support.20 It builds universalism and solidarity across social groups in society, acting as a force to unite rather than divide groups.21 |
| Helping to deliver the right to health | Article 24 of the Convention on the Rights of the Child22 (a convention signed by all countries in the Asia and Pacific regions) can be advanced through UHC in several ways. By covering the whole population, governments can guarantee the right to health of citizens.23 The package of services covered by UHC can advance many of the Convention's requirements, including care at birth, interventions to prevent diseases, nutrition counselling to parents and protection from harmful practices. |
UHC, universal health coverage.
Where are Asia and Pacific countries on the UHC journey?
There are never enough resources to fund all the health services that the population can consume. UHC needs to operate within reasonable financial constraints. The Lancet Commission on Investing in Health (2013) shows that as economies grow, countries that increase their public health expenditure (PHE) to more than 3% of gross domestic product (GDP) can make faster progress reducing health outcome disparities and provide a basic package of care (and 4% of GDP is even better).3
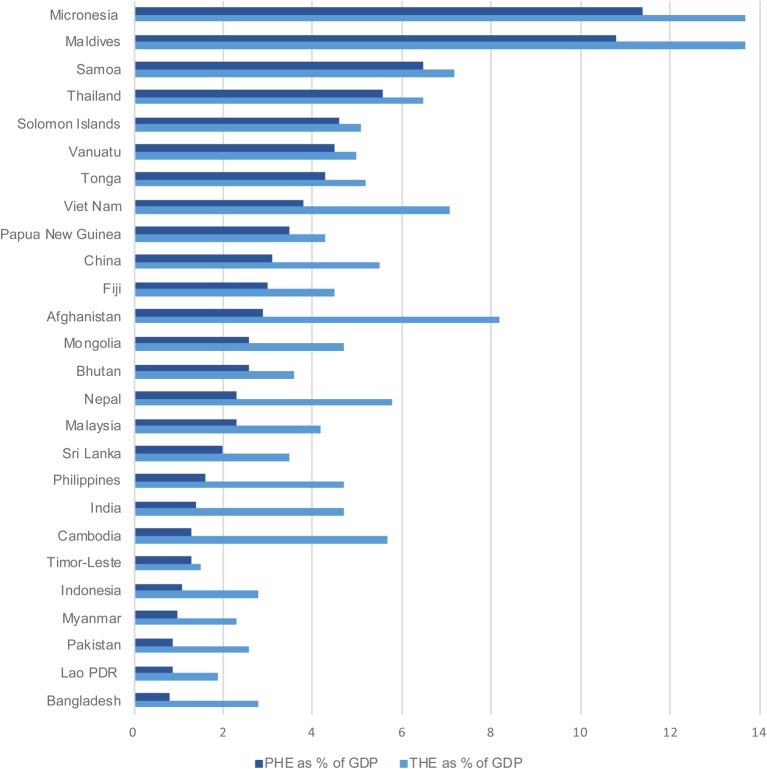
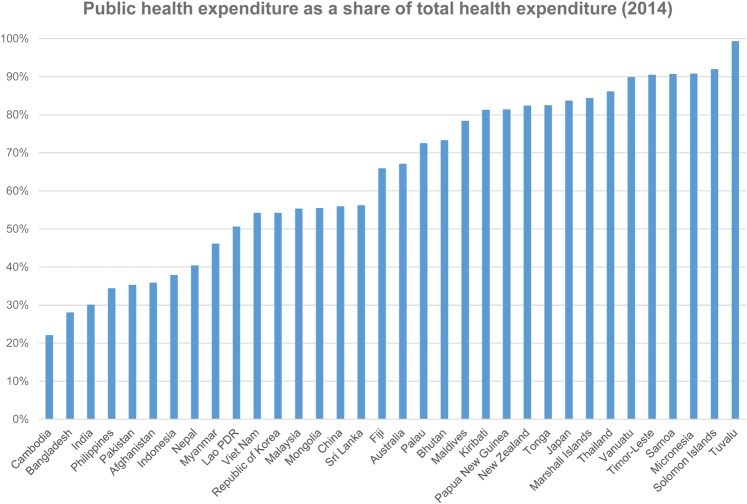
Resources available for health come either from public mechanisms (tax funding, social insurance and external aid) or through private mechanisms such as private insurance schemes, direct out-of-pocket (OOP) payments and some limited use of personal health savings accounts. Total health expenditure (THE) calculates spending on health from all sources of financing, including public and private sources. Figure 1 shows the total and public health spending in Asia and Pacific, expressed as a percentage of GDP, and figure 2 shows PHE as a share of THE (2014).
Figure 1.
THE and PHE in Asia and Pacific countries World Bank 2014. THE, total health expenditure; PHE, public health expenditure.
Figure 2.
Public health expenditure as a share of total health expenditure World Bank 2014.
Most countries spend <4% for public expenditure on health. The higher the PHE as a share of THE, the more control a country has over how it can allocate resources equitably to respond to its burden of disease.
What should countries do to accelerate progress towards UHC?
Using evidence and experience from the Asia and Pacific region, this analysis identifies a series of insights to support countries as they seek to improve UHC within their own context.
UHC is a political process from the start
Across Asia and Pacific, political leaders have recognised that successful UHC reforms are extremely popular and can be a potent political tool to help win and sustain power. UHC can generate huge benefits for some groups in society but can have significant costs for other groups. This, in turn, can result in considerable political costs and benefits (in terms of popularity) for governments and political leaders overseeing reform processes. Given the high political stakes involved, it is not surprising that UHC reforms in the region have often been led by the head of state (eg, Prime Minister Hayato Ikeda in Japan (1963), President Park Chung Hee in the Republic of Korea (1977) and most recently President Joko Widodo in Indonesia (from 2014)). In particular, fulfilling the equity principle underlying UHC (that healthy and wealthy people subsidise services for the poor, vulnerable and sick) requires a strong role for the state in establishing and governing a progressive health financing system. Many analyses of large-scale UHC programmes in Asia have cited political reasons as the main motivation behind these reforms.20 24 25
Closing primary healthcare gaps is the foundation
Closing primary healthcare gaps should be the foundation of UHC reforms.26 Countries that want to make rapid progress towards UHC should prioritise primary healthcare, including prevention and health promotion as a first step. Well-structured, efficient primary health services can meet most of the health needs of the population. Engaging communities and removing barriers to access is a core dimension of strengthening primary care. These measures include removing non-financial access barriers, including perceptions about poor quality; language and cultural barriers; lack of appropriate services (eg, for adolescents); indirect costs; and poor community engagement in health. Some of these barriers can be addressed through strengthening health services while others, such as the indirect costs of accessing care, may involve other social protection measures such as cash transfers.
Improve the quality of care through sustained health systems strengthening
For many countries, the risk is that UHC is launched, entitlements are announced, but the services promised are not available.27 Promises concerning service coverage have to translate into usage in practice. Although hard to measure, quality is generally thought to encompass several defining features, including patient safety, effectiveness, people-centredness and delivering integrated services. Perceived quality is what patients think about the quality of care they receive and it is judged by the experience of attending health services. The main determinants of quality include availability of drugs; qualified, available and respectful health staff; and integrated, appropriate services that meet community needs.1
Make progress with social and economic determinants of health
Health services alone do not engender health and there are a number of important contributors to health that lie outside the health sector's direct authority. Nutrition underpins health to such an extent that it is linked to 45% of child deaths.28 Water, sanitation and hygiene; gender empowerment; household income (poverty); quality of housing; infrastructure; and education (especially for girls and women) all drive health outcomes.29 Countries and states that have made the most progress in improving the social and economic determinants of health can also demonstrate the best health outcomes. Other policies can have a significant impact on the promotion of healthy behaviour, including, for example, excise taxes on tobacco products, taxes on sugar and sweeteners, legislation to enforce the use of bicycle helmets, seatbelts and other measures.
Public financing is critical
Public financing is critical and directly related to more equitable health systems.30 As countries in Asia and Pacific have become wealthier, their health financing systems have developed in similar ways. First, as their economies have grown they have spent more on health as a share of their GDP, indicating a growing societal demand for health services. In common with the rest of the world, high-income countries in the region now spend around 9% to 12% of their GDP on health, middle-income countries spend between 5% and 9%, and low-income countries spend < 5%. Second, the composition of the health financing systems has changed, with the share of public financing (from general taxation and social health insurance) growing over time and replacing private voluntary financing (mostly in the form of OOP health financing). This is demonstrated across the region where private financing dominates in low-income and lower-middle-income countries, whereas public financing is dominant in higher-income countries.
These health financing trends show that economic growth is the main driver of increasing overall health spending, and it is political pressure from populations that lead governments to enact legislation to give public financing a dominant role.31 Populations and politicians have realised that only publicly governed health financing systems can enforce the cross-subsidies required from the rich to the poor and the healthy to the sick, which are necessary to achieve UHC. Politically driven financing transitions have been evident across Asia and Pacific over the last few decades, with many countries socialising their health financing systems, for example, Japan (1963), Republic of Korea (1977), Thailand (2001), Nepal (2008), China (2009) and Indonesia (2014).
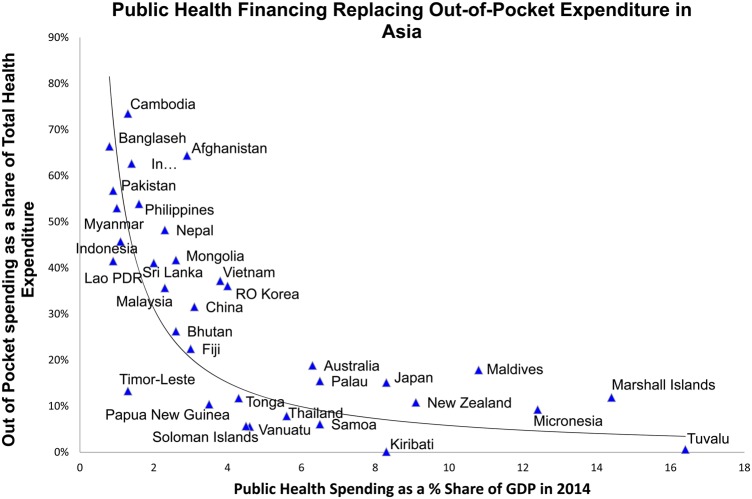
Large increases in public funding gives countries the financial resources to increase the availability and quality of health services while reducing the burden on households financing health services out of their own pockets. Figure 3 shows that in countries spending more than 3% of GDP of public finances on health, OOP spending was <20% of THE. This is important because below this level OOP spending tends to be less catastrophic and impoverishing in nature.32
Figure 3.
Public health financing replacing out-of-pocket expenditure in Asia and the Pacific World Bank 2014.
Pool funds to increase efficiency and equity
Moving away from financing a health system through direct OOP payments requires introducing or strengthening forms of prepayment and the pooling of health funds to protect the population against the financial risk of paying for services. Pooling funds can drive equity.19 21 In creating these pools, it is important to emphasise that only publicly governed risk pools, where contributions are compulsory and progressive (related to people's ability to pay), can meet the equity requirements for UHC. Private voluntary insurance schemes do not achieve this outcome because there is an incentive to exclude high-need people in society and for richer or healthier members to refuse to pay higher contributions. Those less likely to use health services tend not to join, which limits cross-subsidisation. All countries can take steps towards increasing cross-subsidisation even if fully combining all public pools of funds is not immediately feasible.
Priority setting for equity is a political process
Priority setting is the process of deciding what health services should be covered under UHC, and who should benefit and when. Priority setting is an inherently political process and is often controversial since it leads to choices about who in society will benefit from public resources and who will not. If countries used cost-effectiveness analysis, including explicit and transparent methods such as health technology assessment, to re-allocate available health funding to equity-enhancing health interventions, many more lives could be saved. Few countries can afford to immediately fund a full package of services to all citizens and the vast majority take incremental steps over time.5 One key decision to be taken in working towards UHC is whether to prioritise coverage of people with a basic package of care or to extend the quality and range of services to be offered to a more limited group, such as the formally employed. Coverage of the whole population with a defined range of services leads to improved population outcomes and lower inequalities than covering a narrow group of citizens with higher quality services.33 This approach also promotes equity and embeds the principles of cross-subsidy from the start.34 35
Engage the private sector to support UHC
Across Asia and Pacific, the majority of outpatient health services are delivered by private health providers, although in most countries inpatient care is still mainly delivered in public-sector hospitals.36 The challenge for countries is to find ways to engage private providers, maximising their potential to increase the coverage of basic services to all people while minimising their incentives to oversupply and overcharge for services. Whereas public financing is essential for UHC, when it comes to the provision of services there is much more scope to deliver services through a mixture of public and private providers.
Make UHC a long-term proposition
Although one political party may seize an opportunity to launch UHC, ultimately, a UHC system has to be seen as a national goal, belonging to all and one that needs sustained, enduring, cross-party and intergenerational commitment.5 In Japan, Republic of Korea, Sri Lanka, Thailand and other countries with well-developed UHC systems, populations have come to expect UHC as their right and politicians stand on platforms that include how—not whether—they will protect and advance that right.24 Reaching this ‘tipping point’ on the UHC journey is a vital milestone if the system is to become resilient in the face of inevitable challenges. As a dynamic process, UHC needs to contend with: the ebb and flow of national economic growth that can stall UHC; population health needs that change constantly due to ageing, migration, old and new diseases; the health impacts of climate change; and, natural disasters.
Build accountability through transparent progress tracking and monitoring
The UHC journey is unique to each country. Maintaining momentum towards the achievement of UHC goals requires timely and reliable data, the willingness to undertake course corrections at periodic intervals and a strong sense of accountability to citizens. Open and transparent accountability helps policymakers maintain commitment and focus. It helps to ensure resources are used as intended. And, it supports citizen empowerment to track progress and provide feedback, deepening citizen engagement. Most countries that have made progress with UHC also have good data collection and analysis at the heart of their systems founded on a health management information system.
Policy recommendations
Each country's UHC journey will be different: there is no blueprint. Yet, there are some important determinants of success. Every country can make progress from their current position. All countries, regardless of their economic status, can increase domestic revenue for health by improving tax collection, adjusting tax rates and introducing new progressive taxes, including taxes on alcohol, tobacco and other commodities. Box 2 makes 10 policy recommendations for countries aiming to advance UHC.
Box 2. Ten policy recommendations for countries aiming to advance UHC.
Ten policy recommendations:
Make UHC a ‘whole of government’ decision linked to nation-building and achieving citizen development;
Engage political actors, including the head of state, parliamentarians, administrators and powerful interest groups across the political and social spectrum;
Engage beyond health to strengthen the critical drivers of UHC systems such as tax collection and budget management;
Invest in good quality accessible primary healthcare as the foundation of UHC and a precondition for success;
Be willing to develop differentiated strategies and to pay more to address equity and remove barriers to access for the poorest;
Countries spending <3% of GDP in public expenditure should commit to increase funding by at least 0.3%/year;
Take steps towards combining funds from all sources to create the largest pool of resources possible to maximise cross-subsidisation;
Establish a transparent priority-setting process to determine what should be included in the UHC package;
Engage the private sector through strengthened regulation, negotiated payment systems, and partnership;
Strengthen accountability through developing and monitoring clear, explicit and measureable targets.
Success is possible through policy change and maintenance of a UHC system. An independent review of the first 10 years of Thailand's Universal Coverage Scheme (UCS) showed a dramatic reduction in the proportion of OOP health expenditure and falls in catastrophic health expenditure and impoverishment due to healthcare costs.17 Between 1996 and 2008 the incidence of catastrophic healthcare expenditure among the poorest quintile of UCS members fell from 6.8% to 2.8%. Furthermore, the incidence of non-poor households falling below the poverty line because of healthcare costs fell from 2.71% in 2000 to 0.49% in 2009. The review calculated that the comprehensive benefit package provided by the UCS and the reduced level of OOP expenditure protected a cumulative total of 292 000 households from health-related impoverishment between 2004 and 2009.
UHC is a whole of government decision linked to nation-building. It needs to engage stakeholders beyond the health system and critically the head of state to achieve success. Strengthening primary care is critical coupled with ongoing increases in public investment. Massive change at scale with the potential to change lives is possible through a combination of learning the successful lessons from countries further on in the UHC journey, and taking the policy steps necessary to secure change.
Footnotes
Handling editor: Seye Abimbola
Twitter: Follow Rob Yates at @yates_rob and Douglas Noble at @douglasnoblemd
Contributors: AB drafted the first version, and RY and DJN edited the manuscript. This paper is based on a longer thematic report released on 7 November 2016 at the Asia Pacific High Level Meeting on Child Rights.
Funding: This work was funded from the resources of Unicef and Chatham House.
Disclaimer: This paper is based on a longer thematic report presented on November 7th and 8th, 2016 at the UNICEF High Level Meeting on South-South Cooperation for Child Rights in Asia and the Pacific. The opinions expressed in this paper are solely those of the authors and do not necessarily represent the views or policies of UNICEF or any other agency.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.World Bank. 2005. Dying for change: poor people's experience of health and ill-health. Washington DC: World Bank; http://documents.worldbank.org/curated/en/2005/12/6114408/dying-change-poor-peoples-experience-health-ill-health [Google Scholar]
- 2.Nicholson D, Yates R, Warburton W et al. 2015. Delivering universal health coverage: a guide for policymakers. Report of the WISH UHC Forum 2015. https://www.imperial.ac.uk/media/imperial-college/institute-of-global-health-innovation/public/Universal-health-coverage.pdf
- 3.Jamieson DT, Summers LH, Alleyne G et al. Global health 2035: a world converging within a generation. Lancet 2013;382:1898–195. 10.1016/S0140-6736(13)62105-4 [DOI] [PubMed] [Google Scholar]
- 4.Zhu C. China's latest health reforms: a conversation with Chinese health minister Chen Zhu. Interview by Tsung-Mei Cheng. Health Aff (Millwood) 2008;27:1103–10. [DOI] [PubMed] [Google Scholar]
- 5.Stuckler D, Feigl AB, Basu S et al. The political economy of universal health coverage. First Global Symposium on Health Systems Research, Montreux, 2010. [Google Scholar]
- 6.McKee M, Balabanova D, Basu S et al. Universal health coverage: a quest for all countries but under threat in some. Value Health 2013;16(1 Suppl):S39–45. 10.1016/j.jval.2012.10.001 [DOI] [PubMed] [Google Scholar]
- 7.Alsan M, Schoemaker L, Eggleston K et al. Out-of-pocket health expenditures and antimicrobial resistance in low-income and middle-income countries: an economic analysis. Lancet Infect Dis 2016;15:1203–10. 10.1016/S1473-3099(15)00149-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kutzin J, Sparkes SP. Health systems strengthening, universal health coverage, health security and resilience. Bull World Health Organ 2016;94:2 10.2471/BLT.15.165050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO Regional Office for the Western Pacific. Universal health coverage: moving towards better health. Manila: WHO Regional Office for the Western Pacific, draft November 2015. [Google Scholar]
- 10.World Health Organization. What is universal health coverage? http://www.who.int/features/qa/universal_health_coverage/en/ (accessed 26 Mar 2016).
- 11.Bristol N. Global action toward universal health coverage. Washington DC: Center for Strategic and International Studies, 2014. [Google Scholar]
- 12.Chan M. Universal coverage is the ultimate expression of fairness. Acceptance speech at the 65th World Health Assembly, Geneva, Switzerland, 23 May 2012. [Google Scholar]
- 13.WHO. Anchoring universal health coverage in the right to health: what difference would it make? Policy brief Geneva: World Health Organization, 2015. [Google Scholar]
- 14.Yates R. Accelerating progress towards universal health coverage in the commonwealth. London: The Commonwealth, 2015. [Google Scholar]
- 15.Moreno-Serra R, Smith PC. Does progress towards universal health coverage improve population health? Lancet 2012;380:917–23. 10.1016/S0140-6736(12)61039-3 [DOI] [PubMed] [Google Scholar]
- 16.Gruber J, Hendren N, Townsend RM. The great equalizer: health care access and infant mortality in Thailand. Am Econ J Appl Econ 2014;6:91–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Evans TG, Chowdhury AMR, Evans DG, et al. Thailand's universal coverage scheme successes and challenges - an independent assessment of the first 10 years (2001-2011). Nonthaburi, Thai: Health Insurance System Research Office, 2012. [Google Scholar]
- 18.Dreze J, Sen A. An uncertain glory—India and its contradictions. Princeton University Press, 2013. [Google Scholar]
- 19.Evans DB, Elovainio R, Humphreys G. The world health report: health systems financing: the path to universal coverage. Geneva: World Health Organization, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pisani E, Olivier Kok M, Nugroho K. Indonesia's road to universal health coverage: a political journey. Health Policy Plan 2016. doi:10.1093/heapol/czw120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.James C, Savedoff WD. Riskpooling and redistribution in health care: an empirical analysis of attitudes toward solidarity world health report. 2010. Background Paper 5 World Health Organisation; http://www.who.int/healthsystems/topics/financing/healthreport/SolidarityNo5FINAL.pdf [Google Scholar]
- 22. The convention on the rights of the child. http://www.ohchr.org/en/professionalinterest/pages/crc.aspx.
- 23.Sridar D, McKee M, Ooms G et al. Universal health coverage and the right to health: from legal principle to post-2015 indicators. Int J Health Serv 2015;45:495–506. 10.1177/0020731415584554 [DOI] [PubMed] [Google Scholar]
- 24.Ikegami N. ed. Universal health coverage for inclusive and sustainable development—lessons from Japan. The World Bank, 2014. http://www-wds.worldbank.org/external/default/WDSContentServer/WDSP/IB/2014/10/10/000442464_20141010104230/Rendered/PDF/911630PUB0Box30see0also0888620Sep25.pdf [Google Scholar]
- 25.Engel J, Glennie J, Adhikari SR et al. Nepal's story: understanding improvements in maternal health. Oxford: ODI, 2014. https:// http://www.odi.org/sites/odi.org.uk/files/odi-assets/publications-opinion-files/8624.pdf [Google Scholar]
- 26.World Health Report. Primary health care (now more than ever). World Health Organisation, 2008. http://www.who.int/whr/2008/en/ [Google Scholar]
- 27.Meesen B, et al. Removing user fees in the health sector: a review of policy processes in six sub-Saharan African countries. Health Pol Plan, 2011;26(suppl 2):ii16–ii29. http://heapol.oxfordjournals.org/content/26/suppl_2/ii16.full [DOI] [PubMed] [Google Scholar]
- 28.WHO Fact Sheet. http://www.who.int/mediacentre/factsheets/fs178/en/
- 29.Institute for Health Metrics and Evaluation (IHME). Rethinking Development and Health: Findings from the Global Burden of Disease Study. Seattle, WA: IHME, 2016. http://www.healthdata.org/sites/default/files/files/images/news_release/2016/IHME_GBD2015.pdf. [Google Scholar]
- 30.Reeves A, Gourtsoyannis Y, Basu S et al. Financing universal health coverage—effects of alternative tax structures on public health systems: cross-national modelling in 89 low-income and middle-income countries. Lancet 2015;386:274–80. 10.1016/S0140-6736(15)60574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Savedoff WD, Ferranti FD, Smith AL et al. Transitions on health financing and policies for universal health coverage. Washington, DC: Centre for Global Development, 2012. [Google Scholar]
- 32.WHO and the World Bank. Tracking Universal Health Coverage First Global Monitoring Report. 2015. http://apps.who.int/iris/bitstream/10665/174536/1/9789241564977_eng.pdf
- 33.Kutzin J. Anything goes on the path to universal health coverage? No. Bull World Health Organ 2012;90:867–8. 10.2471/BLT.12.113654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oxfam, Universal Health Coverage. Why health insurance schemes are leaving the poor behind. Oxfam Briefing Paper 176, 9 Oct 2013. http://policy-practice.oxfam.org.uk/publications/universal-health-coverage-why-health-insurance-schemes-are-leaving-the-poor-beh-302973
- 35.Kutzin J. Health financing for universal coverage and health system performance: concepts and implications for policy. Bull World Health Organ 2013;91:602–11. http://www.who.int/bulletin/volumes/91/8/12-113985.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wagstaff A. World Bank blog post on data quality and reliability. 2013. http://blogs.worldbank.org/developmenttalk/what-exactly-public-private-mix-health-care