Abstract
Stigma is synonymous with leishmaniasis, an endemic deadly flesh-eating disease in Yemen that affects predominantly poor rural women and children. Women with leishmaniasis often present late and experience not only physical deformities and the risk of death, but also the painful stigma of the disease and its consequences, a similar situation to that of leprosy decades ago. The International Society of Dermatology–sponsored community dermatology project Eradication of Leishmaniasis from Yemen Project has made a difference in the leishmaniasis situation in Yemen and addressed its magnitude. The program eradicated leishmaniasis from some areas, dealt with and improved its alarming prevalence among children and women who are the neglected and highest risk groups, and solved some issues associated with poor access to proper drugs. Medicine donation has enabled women with leishmaniasis to freely receive medicine they otherwise would not have been able to afford, reduced their mortality and morbidity, and minimized the extensive impact the socio-aesthetic stigma has on their lives. Our cause has attracted local and global attention to these problematic issues.
Keywords: ELYP, Impact, Leishmaniasis, RLCC, Women, Yemen
Introduction
Leishmaniasis is a group of protozoan diseases, caused by Leishmania parasites, transmitted by the bite of some species of sand fly. It ranks third in disease burden in disability-adjusted life years caused by neglected tropical diseases and is the second most frequent cause of parasite-related deaths after malaria (Boer et al., 2011, Peter, 2008).
Cutaneous leishmaniasis (CL) is generally mild but may cause cosmetic disfigurement. Mucocutaneous leishmaniasis (MCL) and visceral leishmaniasis (VL) are associated with significant morbidity and mortality. If left untreated, the fatality rate of VL is as high as 100%; in some areas, the case fatality rate is three times higher in women than in men because of gender inequality (Desjeux, 2004).
Leishmaniasis constitutes the greatest threat to the health and socioeconomic status of women as a gender and social group in Yemen. The clinical course and results of infections are generally different in women because exposure to infection may be related to behavior and work patterns of males and females, which are frequently distinct. Immunity to infection and response to treatment may differ between the sexes, and pregnancy alters susceptibility to infection (Brabin and Brabin, 1992).
Leishmaniasis—a hidden disease in Yemen
Leishmaniasis, which has been neglected for decades, is an serious endemic disease, but the true epidemiological data were underestimated. There was a huge disconnect between physicians and patients in the knowledge of leishmaniasis, and it was difficult to find a doctor who could properly diagnose or treat leishmaniasis (Canizares, 1986, World Health Organization, 2006).
Hidden victims
Yemeni leishmaniasis patients had been suffering from neglect, improper diagnosis, maltreatment, lack of affordability, and the shortage of appropriate medicine. Once afflicted, patients suffered from serious complications, including death without a recorded cause. The situation is similar to that of leprosy decades ago.
Yemeni women, particularly rural women, are considered a neglected group that receives less attention and greater restrictions than they deserve. They are more vulnerable to skin disease and suffer greater social stigma than men. The prevalence of leishmaniasis is the highest among rural adult females and male children (Al-Kamel, 2015, Al-Kamel, 2016).
Objectives
This article represents a personal account of the impact of leishmaniasis on women in Yemen based on my 13 years of experience treating affected patients, with an update on my International Society of Dermatology (ISD)-supported initiative to combat leishmaniasis in Yemen.
Impact of leishmaniasis in Yemeni women
Synonyms
Stigma is synonymous with leishmaniasis disease in Yemen. “Bada’h,” “Ofiyah,” “Atharah,” and “Shegnah” are the most common names that I identified that are used to refer to the leishmaniasis disease skin lesion in the endemic regions of Yemen. All of these terms mean apparent lingering residual or life-long stigma (Al-Kamel, 2015).
Impact upon women’s physical health and well-being
Most of the women with leishmaniasis present late with severe symptoms, such as mucosal involvement or huge ulcerative-crusted plaques or nodules, mainly but not exclusively on their faces. Others present with unwanted complications such as disseminations, perforated or deformed nose, disfigured lips, infected ulcers, big ugly scars, or even malignant transformation (Fig. 1, Fig. 2). Children with VL usually present very late with massive hepatosplenomegaly, substantial weight loss, and anemia; some of them die even through the disease is under treatment (Fig. 3) (Al-Kamel, 2015).
Fig. 1.
Yemeni female children with (A) mucocutaneous leishmaniasis (MCL) complicated by stigmatizing nasal perforation, (B) lepromatous diffuse cutaneous leishmaniasis (DCL), (C) giant CL plaque on the right cheek, and (D) destructive MCL ulcer on the lower lip who were treated at the Regional Leishmaniasis Control Center’s clinics in Sana’a, the capital city; and Radaa, a district of the Al Baydaa governorate in central Yemen.
Fig. 2.
Aesthetic stigma associated with mucocutaneous leishmaniasis in adult Yemeni females, at the Regional Leishmaniasis Control Center clinics in Yemen.
Fig. 3.
Two female children with visceral leishmaniasis granted free medicine at the Regional Leishmaniasis Control Center’s Hajjah unit at the north of Yemen.
Families from some endemic districts in Al Baydaa, Hajjah, and Sana’a governorates reported many cases of children and adult women with VL symptoms. Some had been diagnosed as malignancies; others died without diagnoses after undertaking long trips to receive medical, nonmedical, and popular treatments. Yemeni women express more concern about their physical appearance, but leishmaniasis-related aesthetic stigma often depresses their sense of body satisfaction, limits their mobility, and leads to poor physical health.
In brief, deformity, disability, lifelong disfiguring scarring, general health deterioration, and the risk of death are the most common health consequences in Yemeni women with leishmaniasis.
Impact upon women’s sociocultural concepts
Depending on the level of deformities and disfiguring scars, Yemeni women with leishmaniasis receive enacted, perceived, or self-stigma with different levels of discrimination. Stigmatization often affects all aspects of women’s lives, especially interpersonal relationships, social activities, work capacity, and, finally, marriage in a community in which much of their role and identity is based upon marriage and the ability to give birth to children. To my knowledge, cases of divorce on the grounds of the disease have never been reported, but the potential for risk of divorce could be taken in consideration. Some affected wives often experience a stressed marriage, and girls encounter many difficulties in getting married.
Although leishmaniasis may, in fact, be infectious but not contagious in a person-to-person sense (with rare exceptions of congenital transmission of VL from mother to child upon birth, or during blood transfusions), some mothers with leishmaniasis have tried keeping themselves away from their children for fear of infecting them.
Most rural women wear face veils; thus, some of the stigma, especially of facial lesions in uncovered women, is associated with the blame-the-victim idea that if the woman had been modestly covered, she would not have been infected.
From my observations, the deep pain the leishmaniasis-related stigma inflicts upon affected women is the most destructive power in their lives.
Impact upon women’s psychological well-being
Women with leishmaniasis who complain of social stigmatization and discrimination usually experience decreased self-esteem, emotional stress, and anxiety that may predispose them to psychiatric morbidity.
Impact upon women’s economic opportunities
To afford treatment, some affected rural women attempt to avoid potentially stigmatizing situations; others have been forced to sell valuable assets, thereby significantly increasing their level of poverty. Leishmaniasis-related stigma limits their mobility and working capacity both inside and outside the home. Girls and women who became isolated on the grounds of leishmaniasis usually face destitution.
Risk factors for Yemeni women
I identified the following gender-specific factors that may intensify the spread and impact of leishmaniasis in populations of Yemeni women (Al-Kamel, 2015):
-
1.
Children and women represent the sector suffering the greatest deficiencies of medical care. They have poor access to proper drugs for leishmaniasis, which are unaffordable and often unavailable in pharmacies and even in the public health stores. The excess of females over males in rural endemic areas, inherited social habits, and a perceived inability to obtain a proper diagnosis and treatment are also factors. The last of these may encourage women to try more kinds of treatment, such as self-treatment and local healers’ methods.
-
2.
Late presentation that might be a result of lack of healthcare access, a sort of gender inequality in preferential treatment in rural and tribal communities, or the social stigma associated with the disease that keeps females hidden may accentuate leishmaniasis morbidity and mortality.
-
3.
Most women with late presentation depend exclusively on unsafe popular therapies, such as corrosive chemicals and topical steroids.
-
4.
Almost all women displayed a lack of essential knowledge about the disease’s nature and etiology and primary protective measures.
-
5.
Poverty, which is more aggressive among rural females who do not have any source of income except that obtained from their families' sponsor males.
-
6.
Keeping livestock within human habitations maintains a leishmaniasis reservoir and vector that is much closer to the human host, especially women who spend most of their time inside houses.
-
7.
It has been speculated that much of the observed excess of leishmaniasis in adult females and male children may derive from habitual gender- and age-specific occupational roles. Most boys and women work in agriculture and animal care and are responsible for procuring water, especially at dusk and in the early morning, which increase their exposure to sand fly bites.
-
8.
There is a high illiteracy rate among rural Yemeni females. Analysis of the 2005 Yemen Household Budget Survey (HBS) indicated that rural women, irrespective of poverty status, have literacy rates around 25%, whereas even poor urban women have twice the literacy rate (World Bank, 2014).
Myths and beliefs
A lot of myths and false beliefs surrounding leishmaniasis have been reported. Many old women referred to leishmaniasis as a divine punishment, the devil touch, and so on. Some believed that the lesion is highly contagious, and others associated it with water or air pollution.
My initiative to combat leishmaniasis in Yemen
To confront the dire need for action to implement effective leishmaniasis surveillance and control, my ISD-sponsored community dermatology project Eradication of Leishmaniasis from Yemen Project (ELYP) took place in January 2013 as the first and most effective community movement against leishmaniasis in the history of the disease in Yemen.
The first phase of ELYP included the foundation of the Regional Leishmaniasis Control Center (RLCC) in Sana’a in April 2013, with a grant from the American Academy of Dermatology. Subsequently, three more units were established at Al Baydaa, Ibb, and Hajjah governorates (Fig. 1, Fig. 2, Fig. 3, Fig. 4).
Fig. 4.
(A) Dr. Mohamed Al-Kamel treating female child with leishmaniasis. (B) A young girl with leishmaniasis granted free medicine by an Eradication of Leishmaniasis from Yemen Project volunteer at RLCC’s Radaa clinic.
ELYP had strategies to address and eradicate leishmaniasis from Yemen, support needy patients, and improve patients’ lives. The program depended on effective awareness raising and educational, surveillance, treatment, control, and research programs. Bringing global attention to the burden of leishmaniasis in Yemen and the issues of women and children were its main objectives.
Achievements
Within a short period after its announcement, four regional units/clinics were established, 100 volunteers were engaged, remote field campaigns (Fig. 5, Fig. 6) to more than 62 endemic villages and settlements in 6 governorates were organized, and more than 1,050 patients received free diagnosis and treatment services (including parenteral and intralesional antimonial injections, topical and oral antifungal and antibacterial medications, surgery, electrocautery, and cryotherapy). During remote field visits, an average of 10 to 50 hidden leishmaniasis patients in each village, all inhabitants were infected in some villages, and some families with all members’ being infected were recorded. All Yemeni population sectors have benefited from more than 30,000 copies of awareness-raising newsletters; hand brochures and wall posters; meetings and workshops; mobile teledermatology tool; and mass media educational flashes, programs, and television episodes.
Fig. 5.
Eradication of Leishmaniasis from Yemen Project remote field’s educational, surveillance, and treatment campaigns to many endemic regions of Yemen.
Fig. 6.
Some methods ELYP's and RLCC's staff use to raise the awareness for leishmaniasis and combat its related stigma in Yemen: (A) teaching school students (Dr. Al-Kamel and Dr. Mogali, Hajjah unit); (B) teaching public health workers (Dr. Zakaria, Hajjah unit); (C-D) teaching teachers workshops (Dr. Al-Arhabi, Ibb unit); (E) meetings with Ministry of Health officials; and (F) TV and mass media (Al Jazeera Channel).
In August 2014, ELYP organized the first RLCC Conference that was accompanied by a Medicine-For-All Program launching ceremony, under the slogan “insuring medicine for the poor” in Sana’a. The conference attracted the people of interest and media from Yemen and the world (Fig. 7).
Fig. 7.
Dr. Mohamed Al-Kamel, Dr. Luitgard Wiest, and Dr. Ahmed Alanisey speaking at the first Regional Leishmaniasis Control Center Congress in Sana’a, August 13, 2014.
Together with the ISD executive members for 2013, ISD successfully lobbied Stiefel/GlaxoSmithKline (GSK) to provide a compassionate supply of anti-leishmaniasis medication (Pentostam injections) to this project over three years. In 2014, the International League of Dermatological Societies considerately awarded RLCC a grant, supported by the ISD, for laboratory diagnostic equipment.
Many research activities have been conducted at RLCC that have addressed and reported the burden of leishmaniasis in Yemen, its impact on women and children as the populations at the highest risk, and the issues associated with poor access to anti-leishmanial drugs. This research as aimed to find effective solutions.
Burden estimates of leishmaniasis in Yemen upon ELYP
The magnitude of leishmaniasis infection in Yemen is alarming. RLCC estimated the prevalence of leishmaniasis in Yemen as average of 180,000 patients in June 2013 (0.72% of the population, as captured and collected with ELYP initiative through RLCC outpatient clinics’ databases and surveillance campaigns in the endemic governorates during the same period) (Al-Kamel, 2013).
There are no solid data on the incidence of Leishmania infections in Yemen, but the disease is certainly underreported, especially in women and children, and may exceed 10,000 cases per year (Ali, 2011).
The following conclusions have been drawn according to recently published literature based on research conducted at the RLCC:
-
1.
Leishmaniasis is the most common parasitic infestation and the most prevalent infectious disease in central Yemen, with an overall prevalence of 4.11% among all detected skin diseases (Al-Kamel, 2016).
-
2.
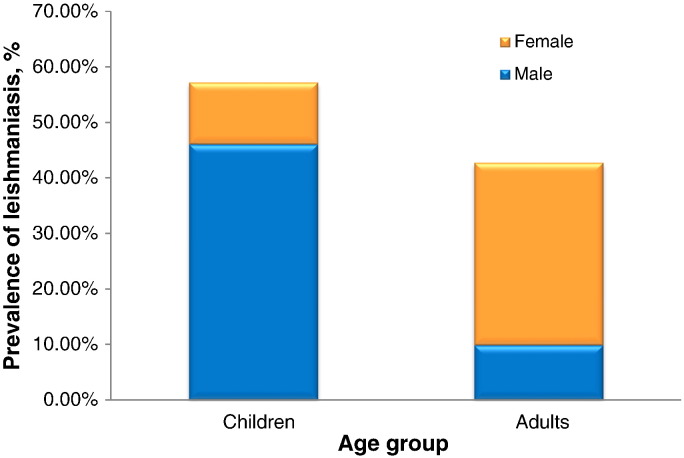
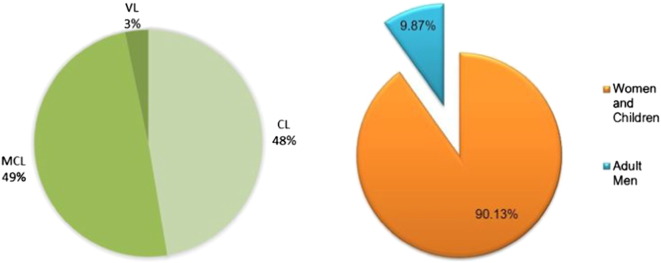
CL, MCL, and VL have significant endemicity in Yemen, and Al Bayda is the most endemic governorate. Incidence of leishmaniasis is highest among rural children and female populations (90.1%) (Fig. 1, Fig. 2, Fig. 3) and is higher among adult females (Fig. 2) than adult males (Fig. 8). MCL seems to be the most prevalent form (49.3%) and occurs more frequently among females than males. It is followed by CL (47.4%), then VL (3.3%) (Fig. 9). The most prevalent Leishmania strains are Leishmania major, Leishmania tropica, Leishmania infantum, and Leishmania donovani. The incidence of leishmaniasis infection peaks in August (autumn), and the majority of patients belong to poor farming families (Al-Kamel, 2015).
Fig. 8.
Overall prevalence of leishmaniasis by age and sex group. Source: Al-Kamel, 2015.
Fig. 9.
Prevalence of different clinical forms of leishmaniasis among study population. Source: Al-Kamel, 2015.
Impact of medicine donation
Although sodium stibogluconate antimony (Pentostam) is the drug of choice, this medicine is usually unavailable, and when available is costly and unaffordable for poorer leishmaniasis patients. The mean relative cost of a treatment regimen for an adult woman is USD 200, USD 100 for a child.
Stiefel/GSK Pentostam donation helped ELYP in offering needy patients, particularly women, a free, relatively safe, and highly effective drug they otherwise would not have been able to afford. Donations are estimated to reach an average of 1,500 patients.
After the first year (October 2014–December 2015) and despite the conditions of war, 348 patients have benefited from the Pentostam donation: 90.43% were rural inhabitants, 48.85% females, 62.64% under the age of 12 years, 54.89% with CL, 39.94% with MCL, and 5.17% with deadly VL (Table 1). Most of the patients (47%) were granted the medicine at the RLCC’s Al Baydaa unit in Radaa district, and the majority of patients came from Al Baydda, Sana’a, Hajjah, Dhamar, Raimah, Ibb, Mahweet, Amran, and Taiz governorates, respectively (Al-Kamel, 2014). Moreover, in response to ELYP’s recommendation and concurrently with its generous medicine donation, Stiefel/GSK reduced the price of Pentostam injections in the local pharmaceutical market to enable competent patients purchasing the medicine.
Table 1.
RLCC: Leishmaniasis Patients Who Benefited from Stiefel/GSK Pentostam Donation for the First Year (October 2014-December 2015).
| Diagnosis | Females | Males | Total | % |
|---|---|---|---|---|
| Cutaneous leishmaniasis | 96 | 95 | 191 | 54.89% |
| Mucocutaneous leishmaniasis | 68 | 71 | 139 | 39.94% |
| Visceral leishmaniasis | 6 | 12 | 18 | 05.17% |
| Total | 170 | 178 | 348 | 100.00% |
Source: Al-Kamel, 2014, Al-Kamel, 2015.
Despite the fact that access to these medicines has significantly improved and high curative rates have been achieved, 6.51% of patients showed resistance, intolerability, or an allergy to this drug’s ingredients; thus, the need for alternative drugs may be imperative (Al-Kamel, 2014).
It was reported that the prevalence of leishmaniasis in some villages in central Yemen, where the disease remained a significant problem up to September 2014, has been remarkably reduced to zero at the end of 2015.
Medicine donation through our Medicine-For-All Program has had a great impact on affected women: It has saved and improved their lives, reduced deformities, minimized the impact of leishmaniasis-related stigma and its psychosocial consequences, and improved the situation of what was considered a hidden disease in Yemen.
Lasting impact of ELYP
Despite the scarcity of resources, war, and instability, ELYP has made a difference in the leishmaniasis situation in Yemen. To my knowledge, for the first time, we have addressed the magnitude of the disorder and eradicated it from some areas in central Yemen. We have dealt with and improved its alarming prevalence among children and women, who are among the neglected and highest risk groups. Issues associated with poor access to proper drugs were solved. Our cause has attracted local and global attention to these problematic issues.
Thanks to RLCC’s volunteers, awareness of the disease that was near to zero has been significantly increased in the community. Now, most physicians in rural and urban health units are aware of and interested in the disease and have at least the essential knowledge in how to diagnose, manage, and refer leishmaniasis patients. As a result, the research capabilities of leishmaniasis in Yemen have improved.
Impact of the war conditions and displacement of populations
The ongoing war in Yemen (started in March 2015) forced us to close the head RLCC unit in Sana’a for 3 months (April-June 2015), restricted our ability to effect more field campaigns, and prevented some leishmaniasis patients from reaching our centers. It has been observed that the war pushed millions of big city inhabitants out to villages, where leishmaniasis is endemic. Currently, increased numbers of leishmaniasis cases who were considered urban inhabitants before the war are seen. I have noticed that wounds in injured fighters represent easy meals for leishmaniasis vectors (female sand flies). Given the substantial growth of populations of dogs, rodents, feral cats, and flies in the cities, I expect a future increase in leishmaniasis among the urban populations who were considered the lowest risk groups (International Society of Dermatology, 2016).
If women are not educated to provide for themselves and take care of their own needs, they are at risk as they lose the protection of the men who are caught up with the war. It also would affect both adults and children in being able to go to school and to get health examinations to detect disease at an earlier stage.
Recommendations
ELYP faces an imperative need to offer alternative medications, such as meglumine antimonite (Glucantime), Amphotericin B, miltefosine, and paromomycin to those who cannot tolerate sodium stibogucanate antimonials. Cost and availability should not be obstacles preventing poor rural women from accessing anti-leishmanial medicines.
The next phase of partnership with project ELYP should include, in addition to further medicine donation, the possibility of medical staff training, molecular diagnosistics, clinical research sponsorships, disfigured women’s rehabilitation program, and improvement of access to our services for populations living in remote areas. ELYP’s surveillance, educational, and management remote field campaigns are in need of vehicles and camping capabilities. Public investment in our research, educational, treatment, and control programs would decrease the leishmaniasis local and global burden.
Yemen is often left out of maps of the worldwide distribution of leishmaniasis. These maps should be redrawn regularly considering the alarming magnitude of leishmaniasis in Yemen, one of its endemic countries.
Conflict of interest disclosure
None declared. Stiefel/GSK had no involvement in the preparation or review of this manuscript.
Acknowledgement
First and foremost, I would like to thank Dr. Dedee Murrell for her contribution to the Eradication of Leishmaniasis from Yemen Project (ELYP). She played a key role in medicine donation and the research program. Furthermore, I must mention my deep sense of appreciation to Dr. Luitgard Wiest for her invaluable assistance in launching the project and setting up the Regional Leishmaniasis Control Center.
I am also deeply grateful to the International Society of Dermatology and its Community Dermatology Task Force, the American Academy of Dermatology, and the International League of Dermatological Societies for their support and contribution to the ELYP.
Footnotes
Supplementary data to this article can be found online at http://dx.doi.org/10.1016/j.ijwd.2016.04.003.
Appendix A. Supplementary data
Supplementary material.1: Leishmaniasis in Yemen: a clinicoepidemiological study of leishmaniasis in central Yemen.
Supplementary material.2: Spectrum of winter dermatoses in rural Yemen.
Supplementary material.3: Eradication of Leishmaniasis from Yemen Project (ELYP) - Regional Leishmaniasis Control Center (RLCC), Yemen - Annual Report – 2015 - Leishmaniasis patients benefited from Stiefel/GSK Pentostam Donation for the 1st Year (Oct. 2014-Dec. 2015).
Supplementary material.4: War in Yemen Not Deterring ISD Member from Aiding Leishmaniasis Patients.
Supplementary material.5: Development of affordable molecular techniques for the diagnosis of leishmaniasis in Yemen.
Supplementary figure.
References
- Ali A. 2011. Development of affordable molecular techniques for the diagnosis of leishmaniasis in Yemen. [cited December 11, 2015]. Available from: http://geb.uni-giessen.de/geb/volltexte/2011/8060/pdf/AliAbdullatif_2011_03_22.pdf. [Google Scholar]
- Al-Kamel M.A. Presented at the 22nd Congress of the European Academy of Dermatology and Venereology, Istanbul, Turkey. October 2–6, 2013. 2013. Leishmaniasis in Yemen. [Accessed April 2, 2016]. [Google Scholar]
- Al-Kamel M.A. Leishmaniasis patients benefited from Stiefel/GSK Pentostam donation for the 1st Year (Oct. 2014-Dec. 2015) Regional Leishmaniasis Control Center (RLCC); Yemen: 2014. Eradication of Leishmaniasis from Yemen Project (ELYP) pp. 2–6. Annual Report–2015 [Accessed April 2, 2016]. [Google Scholar]
- Al-Kamel M.A. Leishmaniasis in Yemen: a clinicoepidemiological study of leishmaniasis in central Yemen. Int J Dermatol. 2016;55(8):849–855. doi: 10.1111/ijd.13041. [DOI] [PubMed] [Google Scholar]
- Al-Kamel M.A. Spectrum of winter dermatoses in rural Yemen. Int J Dermatol. 2016;55:512–517. doi: 10.1111/ijd.12886. [Accessed April 2, 2016] [DOI] [PubMed] [Google Scholar]
- Boer M., Argaw D., Jannin J., Alvar J. Leishmaniasis impact and treatment access. Clin Microbiol Infect. 2011;17(10):1471–1477. doi: 10.1111/j.1469-0691.2011.03635.x. [DOI] [PubMed] [Google Scholar]
- Brabin L., Brabin B.J. Parasitic infections in women and their consequences. Adv Parasitol. 1992;31:01–81. doi: 10.1016/s0065-308x(08)60020-2. [DOI] [PubMed] [Google Scholar]
- Canizares O. Dermatological priorities in developing countries. Trop Doct. 1986;16:50–53. doi: 10.1177/004947558601600203. [DOI] [PubMed] [Google Scholar]
- Desjeux P. Leishmaniasis: current situation and new perspectives. Comp Immunol Microbiol Infect Dis. 2004;27(5):305–318. doi: 10.1016/j.cimid.2004.03.004. [DOI] [PubMed] [Google Scholar]
- International Society of Dermatology . ISD Connection. 10(1) 2016. ISD member fights for leishmaniasis patients amidst war in Yemen; pp. 4–5. (The Official Newsletter of the International Society of Dermatology). [cited Feb. 16, 2016]. Available from: http://www.intsocderm.org/files/2016_February_ISDConnection.pdf. [Google Scholar]
- Peter C.M. Leishmaniasis. In: Kliegman R.M., Jenson H.B., Behrman R.E., Stanton B.F., editors. Nelson textbook of pediatrics. 18th ed. WB Saunders; Philadelphia: 2008. [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2006. Health System Profile – Yemen. [Google Scholar]
- World Bank. "Republic of Yemen." the Status of Yemeni Women: From Aspiraton to Opportunity . Middle east and North Africa Region; June 2014. Report No. 87820_YE. Page 22. Poverty Reduction and Economic Management Department. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.1: Leishmaniasis in Yemen: a clinicoepidemiological study of leishmaniasis in central Yemen.
Supplementary material.2: Spectrum of winter dermatoses in rural Yemen.
Supplementary material.3: Eradication of Leishmaniasis from Yemen Project (ELYP) - Regional Leishmaniasis Control Center (RLCC), Yemen - Annual Report – 2015 - Leishmaniasis patients benefited from Stiefel/GSK Pentostam Donation for the 1st Year (Oct. 2014-Dec. 2015).
Supplementary material.4: War in Yemen Not Deterring ISD Member from Aiding Leishmaniasis Patients.
Supplementary material.5: Development of affordable molecular techniques for the diagnosis of leishmaniasis in Yemen.