Abstract
Background
Mid-dermal elastolysis (MDE) is a rare, yet well-defined clinical and histopathologic entity manifested by fine wrinkling of the skin and mid-dermal loss of elastic fibers. This disease predominantly affects young to middle-aged Caucasian females and although it has no reported systemic features, it is psychologically bothersome and can be of great cosmetic concern.
Methods
We report a case of a healthy 45 year-old female with widespread mid-dermal elastolysis. A literature search using the search terms “mid-dermal elastolysis,” “mid dermal elastolysis,” “middermal elastolysis,” and “elastophagocytosis” was conducted on Pubmed, using articles published from January 2008 until November 2014 to accompany Gambichler’s comprehensive 1977 to 2009 review of mid-dermal elastolysis. The references of relevant papers were reviewed and further cases included as appropriate.
Results
We review the clinical features and histological, ultrastructural, and immunohistochemical findings of MDE, as well as differential diagnoses. There are 13 new publications of MDE since 2008. The novel findings since Gambichler’s review are discussed and pathomechanisms revisited. Interestingly, given the striking female predominance of MDE, there is no known hormonal role in its etiology.
Key words: mid dermal elastolysis, middermal elastolysis, mid-dermal elastolysis, elastophagocytosis
Introduction
Fibrillar collagen and elastin are two of the most abundant extracellular matrix constituents, which maintain the structure of the skin (Scola et al., 2011). The density and spatial alignment of the collagen and elastin architecture define the mechanical tissue properties of the skin, namely laxity, stiffness, and porosity. Elastic fibers, which are made up of an inner core of cross-linked elastin proteins surrounded by fibrillin microfibrils, form an architecturally distinct meshwork that confers elastic recoil properties to the skin (Baldwin et al., 2013). The turnover of elastin in an adult is very low, with its half-life likely exceeding the lifespan of the individual (Sandberg et al., 1982). This has clinical implications: Once these fibers are lost, the skin definitively loses its elasticity.
Mid-dermal elastolysis (MDE) is an acquired elastic tissue disease manifested by fine wrinkling of the skin and mid-dermal loss of elastic fibers. It was first described by Shelley and Wood in 1977 as “wrinkles due to idiopathic loss of mid dermal elastic tissue.” The patient reported by Shelley and Wood had a history of recurrent, unexplained urticaria preceding the development of asymptomatic, finely wrinkled plaques. A subsequent report by Brenner et al. (1978) described two morphological subtypes of MDE: Type I, consisting of fine wrinkles arranged parallel to the skin cleavage lines; and Type II, consisting of miniature, soft papular lesions made up of tiny perifollicular protrusions. Since that time, almost 90 cases of MDE have been reported in the literature and, more recently, a third morphological subtype has been described presenting with reticular erythema (Hillen, 2008, Martin et al., 2008).
The aim of this review is to highlight the prevalence of MDE among middle-aged healthy Caucasian females. In total, 10 new cases (13 publications) have been reported since Gambichler’s, 2010 review. Despite the striking female predominance of MDE, a hormonal role in the etiopathogenesis of this entity remains elusive.
Case
A 45-year-old female was referred to our General Dermatology Clinic for a second opinion regarding what was thought to be a case of generalized atrophoderma by the referring dermatologist. The patient noticed unusual, wrinkled skin on her arms first beginning over 2 years earlier; wrinkling later began spreading to her trunk, back, and proximal legs. Other than occasional pruritus, the skin findings were asymptomatic and there was no preceding erythema.
Her past medical history was unremarkable (of note, she was nulliparous) and she had no recent travel. She was very active outdoors and often exercised without sun protection. She was taking no medications, including no oral contraceptives, and had no known allergies.
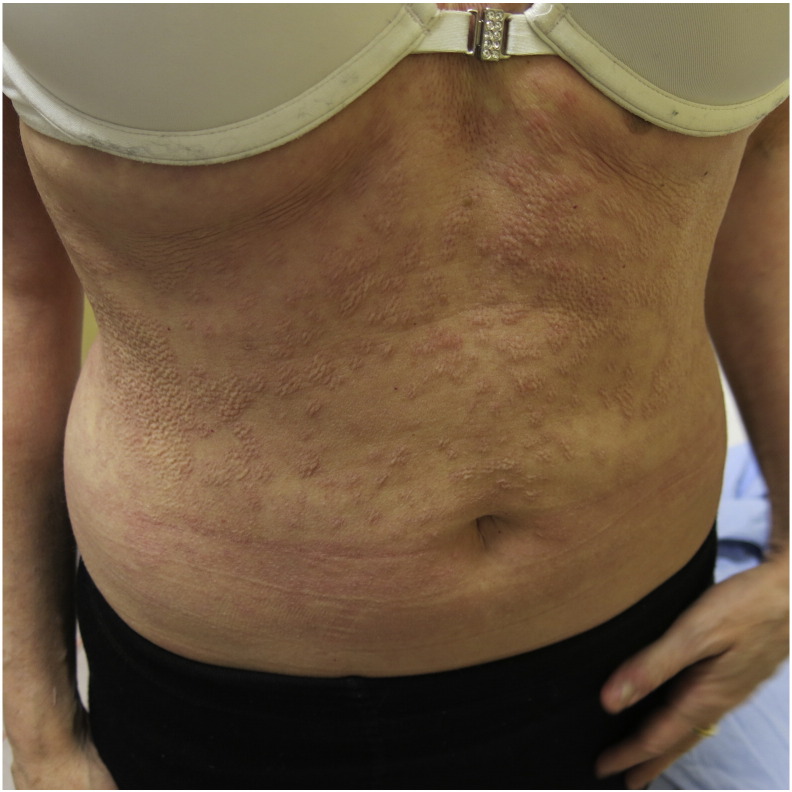
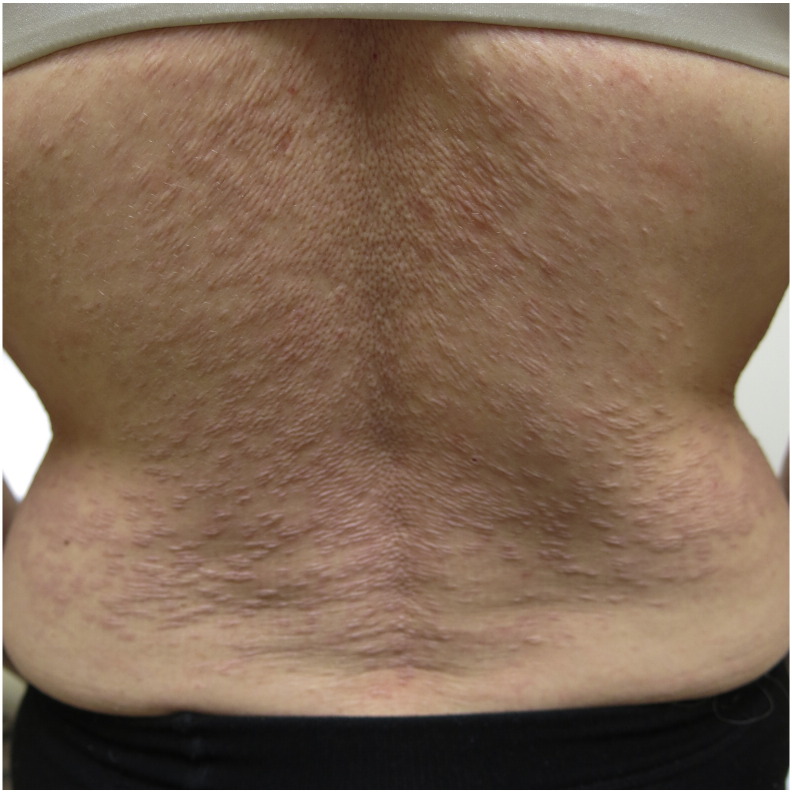
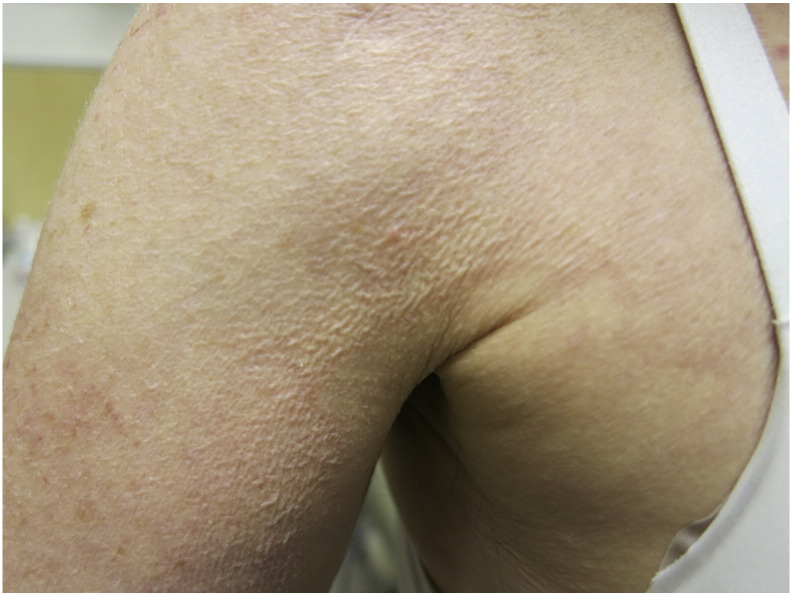
Physical examination revealed widespread papules and plaques with wrinkling and mild protrusion from the surface of the skin (Fig. 1). This morphology was predominantly over her abdomen, trunk, and proximal arms and legs with sparing of her face and hands; it did not appear to be photo-distributed (Fig. 2). She had finer wrinkling of the skin of her anterior shoulder areas (Fig. 3).
Fig. 1.
Flesh-colored, wrinkled papules and plaques with mild protrusion from the surface of the skin.
Fig. 2.
Flesh-colored, wrinkled papules and plaques on the back.
Fig. 3.
Fine wrinkling on right upper-arm skin.
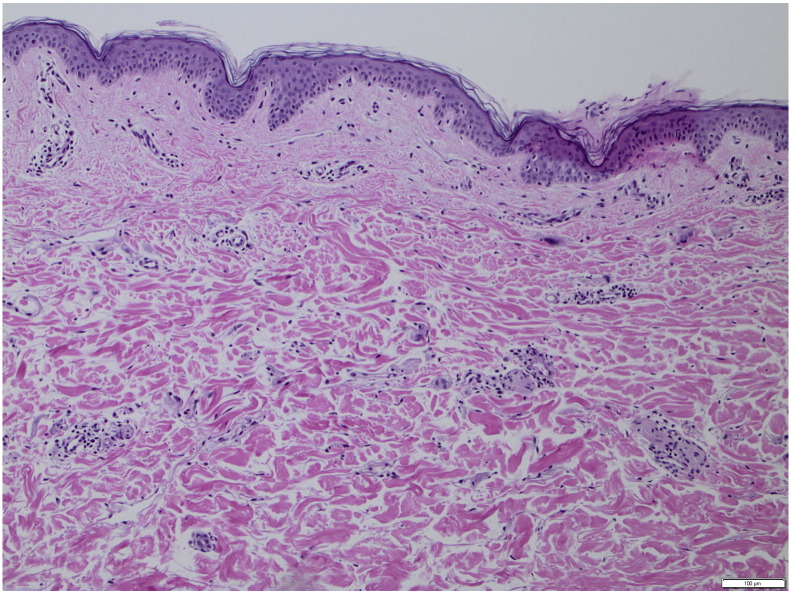
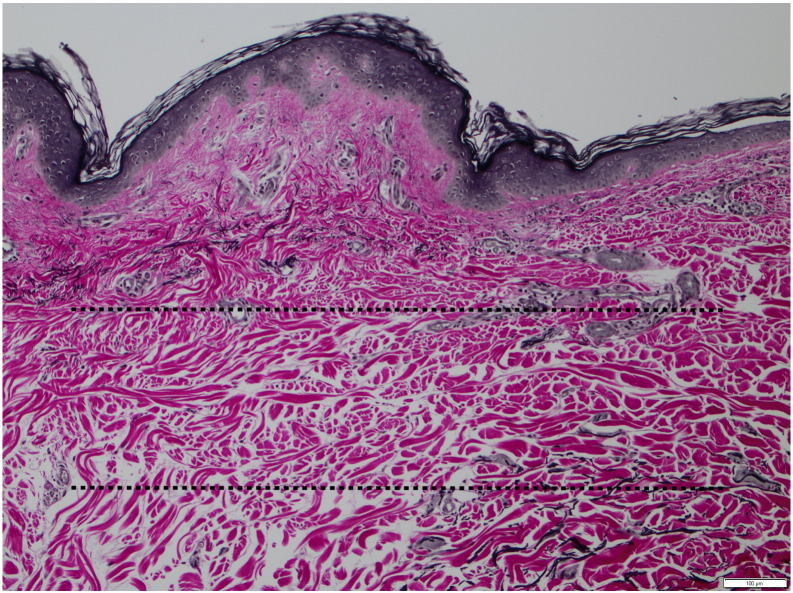
Histologically, Verhoeff–Van Gieson stains revealed mid-dermal loss of elastic tissue (Fig. 4, Fig. 5, Fig. 6).
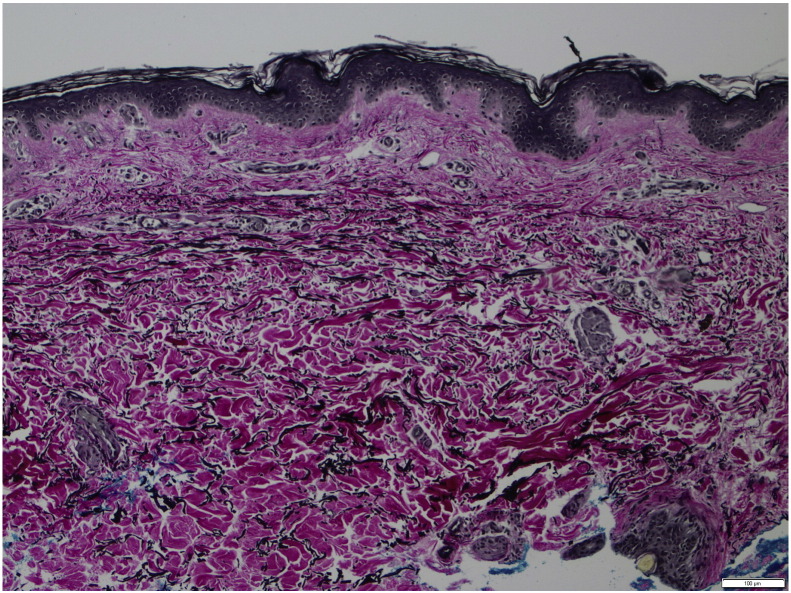
Fig. 4.
Normal histology of hemotoxylin and eosin (H&E)–stained initial biopsy (40 × magnification).
Fig. 5.
Verhoeff–van Gieson stain of normal skin showing normal elastic tissue (40 × magnification).
Fig. 6.
Verhoeff–van Giesson stain of affected skin revealing complete loss of elastic tissue in the mid dermis, annotated with dotted lines (40 × magnification).
Discussion
Epidemiology and clinical presentation
Clinically, MDE predominantly affects the trunk, shoulders, back, and upper extremities and usually spares the palms, soles, and face. In Gambichler’s review, only 12.7% of patients had involvement of the face and distal extremities (Martinez-Escala et al., 2012).
Of the 10 new reported cases, zero reported facial involvement and all cases involved the abdomen and back with variable involvement of neck and proximal extremities. Patients typically present with asymptomatic, well-demarcated, symmetric fine wrinkling of the skin (Type I) and perifollicular papular protrusions (Type II). A third type, an erythematous reticular variant, has more recently been described (Bannister et al., 2001, Cutillas et al., 2010, Gambichler and Lubbe, 2012, Gambichler et al., 2010, Hillen, 2008, Martin et al., 2008, Meyer et al., 2012, Posada et al., 2013).
Since Gambichler’s review in 2010, there have been 13 new publications regarding MDE, but these cover only 10 novel clinical cases, as Gambichler and colleagues wrote three distinct publications all regarding the same clinical patient (Gambichler and Skrygan, 2013, Gambichler et al., 2010, Scola et al., 2011). Furthermore, there were two publications on MDE that did not report new clinical cases (El-Khoury et al., 2014, Tong et al., 2013). Finally, there was one report of two male patients with Type III MDE (Meyer et al., 2012). The remainder of the publications were novel cases of Type I and II MDE (Cohen and Tschen, 2013, Cota et al., 2014, Lai et al., 2014, Martinez-Escala et al., 2012) or Type III MDE (Cutillas et al., 2010, Gambichler and Lubbe, 2012, Posada et al., 2013).
Epidemiologically, MDE affects Caucasian females predominantly of North American and Central European origin (Gambichler, 2010). Aside from two Asian females and one Filipino female, all other reported patients have been Caucasian (Cohen and Tschen, 2013, Suda et al., 2008, Tajima et al., 1999). Gambichler (2010) reported an 83.5% female prevalence in 2010, with a median age of 38 years. Since that time, 6 of the 10 new reported cases have been female. Interestingly, of the publications since 2009, 6 of the 10 were reports of Type III MDE. Unlike Type I and Type II MDE, Type III demonstrates a strong male predominance, with only three reported cases affecting females (Gambichler and Lubbe, 2012, Gambichler et al., 2010, Posada et al., 2013). Therefore, if the six recent reports of Type III MDE are removed (three of which were in males), three of the four cases of Type I and II MDE since 2009 have been female. The only male presentation has been in an human immunodeficiency virus–positive male suffering from immune reconstitution inflammatory syndrome (IRIS; Cota et al., 2014).
Like Shelley and Wood’s (1977) first presentation, lesions are preceded by erythema and/or burning that resolves, leaving well-demarcated patches of fine wrinkling in approximately 50% of cases of MDE (Gambichler, 2010). In our case, the patient had little or no preceding erythema and only occasional, inconsistent pruritus.
MDE has been reported in association with many inflammatory skin conditions including urticaria (Fimiani et al., 1995, Shelley and Wood, 1977) and granuloma annulare (Adams and Mutasim, 2003), supporting theories suggesting destruction of elastic fibers by preceding inflammation that may be clinically obvious or subclinical (Kim and Su, 1992, Maghraoui et al., 1994b, Neri et al., 1996, Rudolph, 1992, Shelley and Wood, 1977, Suda et al., 2008).
Furthermore, in almost half of the cases reported, sun exposure was implicated and/or the lesions were photo-distributed (Agha et al., 1994, Bannister et al., 2001, Fimiani et al., 1995, Gambichler, 2010, Patroi et al., 2003, Snider et al., 1993). It is interesting that for a photo-distributed eruption, the face is rarely affected. However, this is most often the case as well in polymorphous light eruption, a condition that is clearly photo-induced (Isedeh and Lim, 2013). Vatve et al. (2009) reported a case of MDE following narrowband ultraviolet (UV) B therapy for a first episode of guttate psoriasis. However, there is often no histological evidence of chronic sun damage or involvement of chronically sun-exposed sites. As a result, Snider et al. (1993) postulated that the association of MDE to sun exposure is idiosyncratic and not related to long-term sun exposure. Pregnancy or the use of contraceptives prior to the onset of MDE was reported in 25% of patients, which may be lower than expected given the median and mode ages of females affected (Gambichler, 2010, Patroi et al., 2003).
Known associations and differential diagnosis
The association of MDE with rheumatoid arthritis (Rudolph, 1990), false positive serology for Borrelia burgdorferi (Kirsner and Falanga, 1992), Hashimoto’s thyroiditis (Cozzani et al., 2009, Gambichler et al., 1999, Patroi et al., 2003), Grave’s disease (Gambichler, 2010), systemic lupus erythematosus (Boyd and King, 2001), positive antinuclear antibodies (Tajima et al., 1999), protein S deficiency (Cozzani et al., 2009), Type I diabetes, dermatitis herpetiformis, and antiphospholipid antibodies (Martinez-Escala et al., 2012) lends support to an autoimmune process in the pathogenesis of MDE. Martinez-Escala et al. treated their patient with MDE who also had a positive antinuclear antibody and antiphospholipid antibody syndrome with hydroxychloroquine and noted cessation of progression of lesions after 4 months; after 10 months, the patient experienced regression of lesions on the upper extremities. Most recently, a 32 year-old HIV-positive male developed MDE as a manifestation of IRIS, suggesting the inflammatory environment induced by IRIS and the loss of immune self-tolerance to tissue-associated antigens may lead to increased susceptibility to develop local and/or systemic pathological autoimmune conditions against elastic fibers (Cota et al., 2014).
The differential diagnosis for MDE includes anetoderma, annular elastolytic giant cell granuloma, cutis laxa and cutis laxa-like syndromes, and pseudoxanthoma elasticum-like papillary dermal elastosis (Gambichler, 2010).
Histopathology, ultrastructure, and pathogenesis
A band-like focal loss of elastic fibers along the mid-dermis is the characteristic histopathological diagnostic feature of MDE. Biopsies sent for hematoxylin and eosin staining are commonly reported as normal, and the clinician must prompt the pathologist to pursue orcein or van Gieson staining. This was the case in our patient, as initial biopsies by a referring dermatologist were nonspecific; it was only after the diagnosis of MDE was suggested that the dermatopathologist ordered the elastic tissue stains, which demonstrated classic pathology of MDE.
The papillary and deeper reticular dermis are unaffected and elastic tissue remains intact around appendages, even with Type II MDE (Gambichler et al., 1999, Maghraoui et al., 1994a). There is no evidence of dermal actinic damage such as elastosis. Inflammatory infiltrates, most often lymphocytic and perivascular, are more commonly seen in Type III MDE (Bannister et al., 2001, Hillen, 2008, Martin et al., 2008). Interstitial histiocytes, multinucleated giant cells, and occasional figures of elastophagocytosis have been reported (Neri et al., 1996). Interestingly, it has been observed that the degree of histological inflammation parallels the presence of elastophagocytosis (Patroi et al., 2003, Tong et al., 2013).
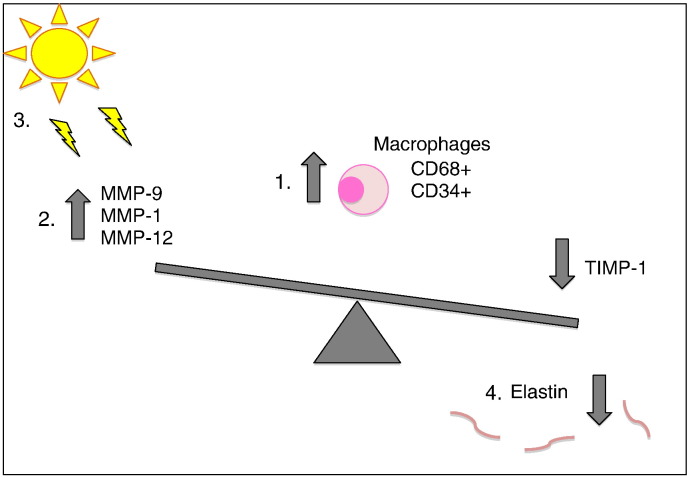
Ultrastructural studies have demonstrated phagocytosis of degenerated abnormal elastic fibers by macrophages, a loose assembly of skeleton fibrils, and irregular aggregations of dense substance (Agha et al., 1994, Fimiani et al., 1995, Gambichler, 2010, Neri et al., 1996, Sterling et al., 1994). Immunohistochemical studies have demonstrated enhanced expression of CD34 + and CD68 + histiocytes and CD3 + and CD4 + lymphocytes in lesional skin (Gambichler et al., 2004, Patroi et al., 2003). Gambichler et al. found elevated cellular expression of MMP-1 (matrix metalloproteinase-1) and MMP-12 in lesional skin with decreased tissue-inhibitor of metalloproteinases 1 (TIMP-1). Patroi et al. reported elastin, but not fibrillin-1, immunoreactivity disappearing from the mid-dermis, as well as MMP-9 in epidermal keratinocytes and in the cytoplasm of large, multinucleated cells located in lesional dermis. Suda et al. (2008) found numerous CD68 + and MMP-9-producing histiocytes and giant cells in erythematous MDE lesions, with few CD68 + in wrinkled skin. As a result, the authors concluded MDE may be initiated by MMP-9 produced by histiocytes and giant cells through its degradation of elastic fibers.
The pathogenesis of MDE is not well understood, but has been postulated to be related to induction of matrix metalloproteinases. Matrix metalloproteinases (MMPs) play a central role in the physiologic and timely breakdown of extracellular matrix essential for embryonic development, morphogenesis, reproduction, and tissue resorption and remodeling (Nagase and Woessner, 1999). The expression of most matrix metalloproteinases is transcriptionally regulated by growth factors, hormones, cytokines, and cellular transformation. The proteolytic activities of MMPs are precisely controlled by endogenous inhibitors, α-macroglobulins, and tissue inhibitors of metalloproteinases (TIMPs). Soluble factor, cell–matrix, and cell–cell interactions are all involved in the complex nature of MMP induction (Nagase and Woessner, 1999). The balance between activated MMPs and TIMPs determines the overall MMP proteolytic activity and, consequently, the extent of extracellular matrix degradation. Further, local disruption of this balance can lead to pathological degradative processes such as increased elastolysis. Several studies have speculated an imbalance in MMP–TIMP activity in MDE (Gambichler et al., 2004, Patroi et al., 2003). More specifically, matrix metalloproteinases gelatinase A (MMP-2) and gelatinase B (MMP-9) are implicated in the physiological and pathological breakdown of several extracellular matrix proteins (Baldwin et al., 2013, Isnard et al., 2002). Cultured fibroblasts from MDE lesional skin have demonstrated increased synthesis of elastases (Fimiani et al., 1995, Prigent et al., 1993, Tajima et al., 1999). As such, Gambichler (2010) hypothesized that decreased elastase inhibition combined with increased MMP activity followed by elastophagocytosis may constitute the background on which MDE can arise. In addition to MMPs, the lysyl oxidase (LOX) family has also been found to be responsible for the formation of collagen and elastin fibrils in the extracellular matrix. In addition to LOX, four LOX-like (LOXL) proteins have also been identified and play a role in biosynthesis and renewal of elastic tissue. Gambichler and Skrygan (2013) found increased MMP-9 expression decreased LOXL2 mRNA levels in lesional MDE skin.
Whether ultraviolet radiation or hormonal triggers are pathogenic factors in MDE remains unknown. Certainly, a hormonal and/or UV-induced alteration in MMPs could potentially explain the unequivocal proportion of female patients reported, as well as the significant history of sun or tanning bed exposure amongst them. Brenneisen et al. (2002) reported UVB-triggered induction of MMP-1 and MMP-3 and, subsequently, Brennan et al. (2003) found increased MMP-1 levels in punch biopsies of human skin obtained 1 day after irradiation with two minimal erythema doses of UVB. Cho et al. (2008) observed that infrared/visible light spectrum of sunlight significantly increased MMP-1 and MMP-9 expression. Interestingly, endogenous estrogen was found to exacerbate UV-induced inflammation and photo-aging in mice (Yoon et al., 2014). However, to our knowledge, the only study currently published linking estrogen to MMPs evaluated the role of estrogen on osteoarthritic chondrocytes and actually found that estrogen was protective and may improve the imbalance between the amounts of MMPs and TIMPs in the chondrocytes of postmenopausal osteoarthritic females (Fig. 7; Lee et al., 2003).
Fig. 7.
An imbalance between metalloproteinases (MMPs) and tissue-inhibitor of metalloproteinases (TIMP) is suspected in the pathogenesis of MDE. (1) In MDE lesional skin there is an increased number of CD68 + and CD34 + histiocytes. (2) There is also increased expression of MMP-1, MMP-9, and MMP-12 with decreased elastase inhibitor TIMP-1. (3) Ultraviolet B, infrared, and visible light are hypothesized to play a role in alteration of MMP expression. (4) Disruption of this balance is thought to lead to degradative processes such as increased elastolysis in MDE.
Imaging and investigations
Noninvasive imaging methods, such as coherence tomography and high frequency ultrasound, are potential new modalities recently reported to be of use in evaluating MDE (Scola et al., 2011). Further, multiphoton microscopy, which uses near-infrared light to visualize deep tissues and exploit autofluorescent extracellular matrix fibers, has been used to calculate and three-dimensionally quantify elastic fibers (Tong et al., 2013).
Treatment
Unfortunately, there are no reports of efficacious treatment for MDE. In fact, most studies do not report on treatment modalities, likely owing to the benign course of MDE. Use of topical and systemic steroids (Boyd and King, 2001, Lewis et al., 2004), colchicine (Sterling et al., 1994), and tretinoin (Harmon et al., 1994, Sterling et al., 1994) have been reported. Topical tretinoin seems to be the most widely used and has been reported to reduce wrinkles, but not to alter the natural history of the disease (Sterling et al., 1994). As previously mentioned, Martinez-Escala et al. (2012) reported a patient with positive ANA and antiphospholipid antibody syndrome who had cessation of progression of lesions after 4 months and regression of lesions on the upper extremities after 10 months with hydroxychloroquine.
Novel natural therapies include soybean extract and eicosapentanoic acid (EPA). Mouse and swine skins topically treated with soybean extracts showed enhanced elastic fiber network and inhibition of elastases. Further, elastin expression was also augmented in human skin transplanted onto immunodeficient mice in response to soy treatment (Zhao et al., 2009). Topical EPA has been found to inhibit UV-induced MMP-1 expression in dermal fibroblasts as well as increase collagen and elastic fibers (tropoelastin and fibrillin-1; Kim et al., 2006). Whereas MDE does not alter fibrillin microfibrils, EPA may be a potential agent for the treatment of MDE.
Lastly, the cosmetic implications of MDE can be life altering and clinicians should not neglect the psychosocial impact of this diagnosis.
Conclusion
Mid-dermal elastolysis is a clinical and histological diagnosis that predominantly affects young, healthy females. Its pathogenesis remains elusive, although potential theories suggest correlation with sun exposure as well as autoimmunity. Clinicians may be tempted to diminish the severity of this diagnosis as there are no systemic manifestations. However, they need to be aware of the dramatic cosmetic implications for affected patients.
Acknowledgements
Dr. Charlene Hunter supplied the pathology images.
References
- Adams B.B., Mutasim D.F. Colocalization of granuloma annulare and mid-dermal elastolysis. J Am Acad Dermatol. 2003;48(Suppl. 2):S25–S27. doi: 10.1067/mjd.2003.118. [DOI] [PubMed] [Google Scholar]
- Agha A., Hashimoto K., Mahon M. Mid dermal elastolysis: case report and review of the literature. J Dermatol. 1994;21(10):760–766. doi: 10.1111/j.1346-8138.1994.tb03284.x. [DOI] [PubMed] [Google Scholar]
- Baldwin A.K., Simpson A., Steer R., Cain S.A., Kielty C.M. Elastic fibres in health and disease. Expert Rev Mol Med. 2013;15:e8. doi: 10.1017/erm.2013.9. [DOI] [PubMed] [Google Scholar]
- Bannister M.J., Rubel D.M., Kossard S. Mid-dermal elastophagocytosis presenting as a persistent reticulate erythema. Australas J Dermatol. 2001;42(1):50–54. doi: 10.1046/j.1440-0960.2001.00474.x. [DOI] [PubMed] [Google Scholar]
- Boyd A.S., King L.E., Jr. Middermal elastolysis in two patients with lupus erythematosus. Am J Dermatopathol. 2001;23(2):136–138. doi: 10.1097/00000372-200104000-00009. [DOI] [PubMed] [Google Scholar]
- Brennan M., Bhatti H., Nerusu K.C., Bhagevathula N., Kang S., Fisher G.J. Matrix metalloproteinase-1 is the major collagenolytic enzyme responsible for collagen damage in UV-irradiated human skin. Photochem Photobiol. 2003;78(1):43–48. doi: 10.1562/0031-8655(2003)078<0043:mmitmc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Brenneisen P., Sies H., Scharffetter-Kochanek K. Ultraviolet-B irradiation and matrix metalloproteinases: from induction via signaling to initial events. Ann N Y Acad Sci. 2002;973:31–43. doi: 10.1111/j.1749-6632.2002.tb04602.x. [DOI] [PubMed] [Google Scholar]
- Brenner W., Gschnait F., Konrad K., Holubar K., Tappeiner J. Non-inflammatory dermal elastolysis. Br J Dermatol. 1978;99(3):335–338. doi: 10.1111/j.1365-2133.1978.tb02006.x. [DOI] [PubMed] [Google Scholar]
- Cho S., Lee M.J., Kim M.S., Lee S., Kim Y.K., Lee D.H. Infrared plus visible light and heat from natural sunlight participate in the expression of MMPs and type I procollagen as well as infiltration of inflammatory cell in human skin in vivo. J Dermatol Sci. 2008;50(2):123–133. doi: 10.1016/j.jdermsci.2007.11.009. [DOI] [PubMed] [Google Scholar]
- Cohen P.R., Tschen J.A. Linear lumbar localized lysis of elastic fibers: a distinctive clinical presentation of mid-dermal elastolysis. J Clin Aesthet Dermatol. 2013;6(7):32–39. [PMC free article] [PubMed] [Google Scholar]
- Cota C., Latini A., Lora V., Cerroni L. Mid-dermal elastolysis as a manifestation of immune reconstitution inflammatory syndrome in an HIV-infected patient. J Am Acad Dermatol. 2014;71(4):e134–e135. doi: 10.1016/j.jaad.2014.04.051. [DOI] [PubMed] [Google Scholar]
- Cozzani E., Santoro F., Parodi A. Mid-dermal elastolysis with prothrombotic abnormalities: two cases. Br J Dermatol. 2009;161(1):203–205. doi: 10.1111/j.1365-2133.2009.09202.x. [DOI] [PubMed] [Google Scholar]
- Cutillas E., Ferrando F.J., Marti M.E., Mateu A., Rausell N. Reticular variant of mid-dermal elastolysis after insertion of a pacemaker. Clin Exp Dermatol. 2010;35(5):498–500. doi: 10.1111/j.1365-2230.2009.03736.x. [DOI] [PubMed] [Google Scholar]
- El-Khoury J., Kurban M., Abbas O. Elastophagocytosis: underlying mechanisms and associated cutaneous entities. J Am Acad Dermatol. 2014;70(5):934–944. doi: 10.1016/j.jaad.2013.12.012. [DOI] [PubMed] [Google Scholar]
- Fimiani M., Mazzatenta C., Alessandrini C., Paola M., Paola C., Andreassi L. Mid-dermal elastolysis: an ultrastructural and biochemical study. Arch Dermatol Res. 1995;287(2):152–157. doi: 10.1007/BF01262324. [DOI] [PubMed] [Google Scholar]
- Gambichler T. Mid-dermal elastolysis revisited. Arch Dermatol Res. 2010;302(2):85–93. doi: 10.1007/s00403-009-1004-0. [DOI] [PubMed] [Google Scholar]
- Gambichler T., Lubbe J. Reticular variant of mid-dermal elastolysis accompanied by persistent urticarial lesions. J Dermatol. 2012;39(11):963–965. doi: 10.1111/j.1346-8138.2012.01596.x. [DOI] [PubMed] [Google Scholar]
- Gambichler T., Skrygan M. Decreased lysyl oxidase-like 2 expression in mid-dermal elastolysis. Arch Dermatol Res. 2013;305(4):359–363. doi: 10.1007/s00403-012-1308-3. [DOI] [PubMed] [Google Scholar]
- Gambichler T., Linhart C., Wolter M. Mid-dermal elastolysis associated with hashimoto's thyroiditis. J Eur Acad Dermatol Venereol. 1999;12(3):245–249. [PubMed] [Google Scholar]
- Gambichler T., Breuckmann F., Kreuter A., Boms S., Altmeyer P., Stucker M. Immunohistochemical investigation of mid-dermal elastolysis. Clin Exp Dermatol. 2004;29(2):192–195. doi: 10.1111/j.1365-2230.2004.01480.x. [DOI] [PubMed] [Google Scholar]
- Gambichler T., Stucker M., Kreuter A., Matip R., Gaifullina R., Scola N. Expression of extracellular matrix proteins in reticular variant of mid-dermal elastolysis. J Eur Acad Dermatol Venereol. 2010;24(12):1481–1484. doi: 10.1111/j.1468-3083.2010.03683.x. [DOI] [PubMed] [Google Scholar]
- Harmon C.B., Su W.P., Gagne E.J., Fransway A.F., Zelickson B.D. Ultrastructural evaluation of mid-dermal elastolysis. J Cutan Pathol. 1994;21(3):233–238. doi: 10.1111/j.1600-0560.1994.tb00266.x. [DOI] [PubMed] [Google Scholar]
- Hillen U. Reticular erythema with focal mid-dermal elastophagocytosis (REMDE) J Dtsch Dermatol Ges. 2008;6(10):857–859. doi: 10.1111/j.1610-0387.2008.06663.x. [857–60] [DOI] [PubMed] [Google Scholar]
- Isedeh P., Lim H.W. Polymorphous light eruption presenting as pinhead papular eruption on the face. J Drugs Dermatol. 2013;12(11):1285–1286. [PubMed] [Google Scholar]
- Isnard N., Peterszegi G., Robert A.M., Robert L. Regulation of elastase-type endopeptidase activity, MMP-2 and MMP-9 expression and activation in human dermal fibroblasts by fucose and a fucose-rich polysaccharide. Biomed Pharmacother. 2002;56(5):258–264. doi: 10.1016/s0753-3322(02)00196-8. [DOI] [PubMed] [Google Scholar]
- Kim J.M., Su W.P. Mid dermal elastolysis with wrinkling: report of two cases and review of the literature. J Am Acad Dermatol. 1992;26(2 Pt 1):169–173. [PubMed] [Google Scholar]
- Kim H.H., Cho S., Lee S., Kim K.H., Cho K.H., Eun H.C. Photoprotective and anti-skin-aging effects of eicosapentaenoic acid in human skin in vivo. J Lipid Res. 2006;47(5):921–930. doi: 10.1194/jlr.M500420-JLR200. [DOI] [PubMed] [Google Scholar]
- Kirsner R.S., Falanga V. Features of an autoimmune process in mid-dermal elastolysis. J Am Acad Dermatol. 1992;27(5 Pt 2):832–834. doi: 10.1016/0190-9622(92)70259-i. [DOI] [PubMed] [Google Scholar]
- Lai J.H., Murray S.J., Walsh N.M. Evolution of granuloma annulare to mid-dermal elastolysis: report of a case and review of the literature. J Cutan Pathol. 2014;41(5):462–468. doi: 10.1111/cup.12292. [DOI] [PubMed] [Google Scholar]
- Lee Y.J., Lee E.B., Kwon Y.E., Lee J.J., Cho S.W., Kim H.A. Effect of estrogen on the expression of matrix metalloproteinase (MMP)-1, MMP-3, and MMP-13 and tissue inhibitor of metalloproternase-1 in osteoarthritis chondrocytes. Rheumatol Int. 2003;23(6):282–288. doi: 10.1007/s00296-003-0312-5. [DOI] [PubMed] [Google Scholar]
- Lewis K.G., Dill S.W., Wilkel C.S., Robinson-Bostom L. Mid-dermal elastolysis preceded by acute neutrophilic dermatosis. J Cutan Pathol. 2004;31(1):72–76. doi: 10.1046/j.0303-6987.2004.0141.x. [DOI] [PubMed] [Google Scholar]
- Maghraoui S., Grossin M., Crickx B., Blanchet P., Belaich S. Acquired mid-dermal elastolysis. Ann Dermatol Venereol. 1994;121(3):259–265. [PubMed] [Google Scholar]
- Maghraoui S., Grossin M., Crickx B., Blanchet P., Belaich S. Acquired mid-dermal elastolysis. 2 new cases. Ann Dermatol Venereol. 1994;121(3):245–246. [PubMed] [Google Scholar]
- Martin L.K., Kossard S., Murrell D.F. Reticular variant of mid-dermal elastolysis. Am J Dermatopathol. 2008;30(3):287–290. doi: 10.1097/DAD.0b013e31816906bc. [DOI] [PubMed] [Google Scholar]
- Martinez-Escala M.E., Rozas E., Pujol R.M., Herrero-Gonzalez J.E. Mid-dermal elastolysis: another dermatological clue to autoimmunity? Acta Derm Venereol. 2012;92(4):434–435. doi: 10.2340/00015555-1292. [DOI] [PubMed] [Google Scholar]
- Meyer A., Aaron D., Perry A., Guill M., III Erythematous reticular patches: a rare presentation of mid-dermal elastolysis. J Am Acad Dermatol. 2012;67(5):e216–e217. doi: 10.1016/j.jaad.2012.03.017. [DOI] [PubMed] [Google Scholar]
- Nagase H., Woessner J.F., Jr. Matrix metalloproteinases. J Biol Chem. 1999;274(31):21491–21494. doi: 10.1074/jbc.274.31.21491. [DOI] [PubMed] [Google Scholar]
- Neri I., Patrizi A., Fanti P.A., Passarini B., Badiali-De Giorgi L., Varotti C. Mid-dermal elastolysis: a pathological and ultrastructural study of five cases. J Cutan Pathol. 1996;23(2):165–169. doi: 10.1111/j.1600-0560.1996.tb01290.x. [DOI] [PubMed] [Google Scholar]
- Patroi I., Annessi G., Girolomoni G. Mid-dermal elastolysis: a clinical, histologic, and immunohistochemical study of 11 patients. J Am Acad Dermatol. 2003;48(6):846–851. doi: 10.1067/mjd.2003.452. [DOI] [PubMed] [Google Scholar]
- Posada C., No N., De La Torre C., Florez A. Reticular variant of mid-dermal elastolysis. Australas J Dermatol. 2013;54(1):69–71. doi: 10.1111/j.1440-0960.2012.00925.x. [DOI] [PubMed] [Google Scholar]
- Prigent F., Baulac C., Duroselle M., Marinho E., Beranger J.Y., Frances C. Mid dermal elastolysis: A case with a study of elastases. Ann Dermatol Venereol. 1993;120(11):853–855. [PubMed] [Google Scholar]
- Rudolph R.I. Mid dermal elastolysis. J Am Acad Dermatol. 1990;22(2 Pt 1):203–206. doi: 10.1016/0190-9622(90)70024-c. [DOI] [PubMed] [Google Scholar]
- Rudolph R.I. Mid-dermal elastolysis. J Am Acad Dermatol. 1992;27(5 Pt 1):789. doi: 10.1016/s0190-9622(08)80245-9. [DOI] [PubMed] [Google Scholar]
- Sandberg L.B., Soskel N.T., Wolt T.B. Structure of the elastic fiber: an overview. J Invest Dermatol. 1982;79(Suppl. 1):128s–132s. doi: 10.1111/1523-1747.ep12546005. [DOI] [PubMed] [Google Scholar]
- Scola N., Goulioumis A., Gambichler T. Non-invasive imaging of mid-dermal elastolysis. Clin Exp Dermatol. 2011;36(2):155–160. doi: 10.1111/j.1365-2230.2010.03864.x. [DOI] [PubMed] [Google Scholar]
- Shelley W.B., Wood M.G. Wrinkles due to idiopathic loss of mid-dermal elastic tissue. Br J Dermatol. 1977;97(4):441–445. doi: 10.1111/j.1365-2133.1977.tb14255.x. [DOI] [PubMed] [Google Scholar]
- Snider R.L., Lang P.G., Miaze J.C. The clinical spectrum of mid-dermal elastolysis and the role of UV light in its pathogenesis. J Am Acad Dermatol. 1993;28(6):938–942. doi: 10.1016/0190-9622(93)70134-f. [DOI] [PubMed] [Google Scholar]
- Sterling J.C., Coleman N., Pye R.J. Mid-dermal elastolysis. Br J Dermatol. 1994;130(4):502–506. doi: 10.1111/j.1365-2133.1994.tb03386.x. [DOI] [PubMed] [Google Scholar]
- Suda T., Hara H., Yoshitake M., Ohbayashi T., Nakamura T., Terui T. Immunohistochemical investigation of mid-dermal elastolysis with a history of erythema. Am J Dermatopathol. 2008;30(5):477–480. doi: 10.1097/DAD.0b013e318176b874. [DOI] [PubMed] [Google Scholar]
- Tajima S., Inazumi T., Kajiya H., Osakabe T., Seyama Y., Sakamoto H. Elastin metabolism in skin fibroblasts explanted from a patient with mid-dermal elastolysis. Br J Dermatol. 1999;140(4):752–754. [PubMed] [Google Scholar]
- Tong P.L., Qin J., Cooper C.L., Lowe P.M., Murrell D.F., Kossard S. A quantitative approach to histopathological dissection of elastin-related disorders using multiphoton microscopy. Br J Dermatol. 2013;169(4):869–879. doi: 10.1111/bjd.12430. [DOI] [PubMed] [Google Scholar]
- Vatve M., Morton R., Bilsland D. A case of mid-dermal elastolysis after narrowband ultraviolet B phototherapy. Clin Exp Dermatol. 2009;34(2):263–264. doi: 10.1111/j.1365-2230.2008.02829.x. [DOI] [PubMed] [Google Scholar]
- Yoon H.S., Shin C.Y., Kim Y.K., Lee S.R., Chung J.H. Endogenous estrogen exacerbates UV-induced inflammation and photoaging in mice. J Invest Dermatol. 2014;134(8):2290–2293. doi: 10.1038/jid.2014.160. [DOI] [PubMed] [Google Scholar]
- Zhao R., Bruning E., Rossetti D., Starcher B., Seiberg M., Iotsova-Stone V. Extracts from glycine max (soybean) induce elastin synthesis and inhibit elastase activity. Exp Dermatol. 2009;18(10):883–886. doi: 10.1111/j.1600-0625.2009.00862.x. [DOI] [PubMed] [Google Scholar]