Abstract
Introduction:
There is evidence that non-sterile clinical gloves (NSCG) are over-used by healthcare workers (HCWs) and are associated with cross-contamination. This study aimed to determine attitudes of student nurses and members of the public to the use of NSCG.
Methods:
Third-year student nurses completed a questionnaire indicating tasks for which they would wear NSCG and influences on their decision. Correlations between tasks were identified using exploratory factor analysis. An online survey of the public was conducted using snowball sampling method.
Results:
Sixty-seven students completed the questionnaire; they indicated use of NSCG for low-risk tasks and reported their own judgement as the main influence on their decision to wear them. Correlated tasks included ‘perceived to be risky’ or ‘definitive indication for gloves/no gloves’ and ‘related to personal hygiene’. A total of 142 respondents completed the public survey. They reported being uncomfortable with HCW wearing gloves for some personal tasks, e.g. assisting to toilet and dressing, but 94% preferred their use for washing ‘private parts’; 29% had observed inappropriate glove use by HCWs during recent contact with healthcare.
Conclusion:
Student nurses reported using NSCG routinely for tasks for which they are neither required nor recommended. The public observe inappropriate glove use and are uncomfortable with their use for some personal tasks.
Keywords: Gloves, infection prevention, hand hygiene, patient experience, student nurses
Introduction
The use of non-sterile clinical gloves (NSCG) in healthcare settings emerged in the mid-1980s as a measure to protect healthcare workers (HCWs) from exposure to blood-borne viruses in blood and body fluids (Centers for Disease Prevention & Control, 1988). The concept of ‘universal precautions’ recommended the use of protective clothing for direct contact with blood and blood-stained body fluids. This guidance was subsequently developed into the concept of Standard Precautions which advises that personal protective equipment (PPE) should be used for procedures where a risk of direct contact with any blood and body fluids (BBF) is anticipated (Loveday et al., 2014a; Royal College of Nursing, 2012; Seigel et al., 2007). These policies were based on the concept that pathogens that cause healthcare-associated infections (HCAIs) are most likely to be present in body fluids and using PPE in these situations reduces the risk of transference. Subsequently, the World Health Organization (WHO) guidelines on hand hygiene recognised the potential for NSCG to be over-used and provided guidance on when gloves are indicated and when they are not required (WHO, 2009). However, recent studies suggest that the use of NSCG has extended to a wide range of care activities that do not involve direct contact with BBF and their use has been associated with a risk of cross-contamination because they are put on too early, removed too late and acquire pathogens during use that can then be transferred to susceptible sites, or other surfaces and patients (Flores and Pevalin, 2006; Fuller et al., 2011; Girou et al., 2004; Loveday et al., 2014a, 2014b; Snyder et al., 2008).
There is therefore a need to address how HCWs use gloves to ensure that they are used appropriately and safely. To be successful, strategies focused on changing this behaviour need to take account of the key drivers of glove-use behaviour. In a previous study involving interviews with HCWs, we identified that both emotion and socialisation were important drivers of glove-use behaviour (Loveday et al., 2014b). While the main emotional drivers were linked to self-protection, perception of patient preference was also cited as a factor that influenced HCWs to use of NSCG. HCWs expressed views that patients preferred to see them wearing gloves as they conferred a sense of hygiene but also provided a form of emotional barrier against ‘intimacy’, for example for washing genital areas. However, HCWs also recognised that glove use interferes with the ‘therapeutic touch’ and could give patients the impression that they were somehow ‘dirty’ or contagious (Loveday et al., 2014b).
There is a paucity of evidence about what the public actually think about HCW use of gloves and whether HCW perceptions of patient preference is borne out by their opinions. The aim of this study was therefore to explore the perceptions of the public about HCWs’ use of gloves and their experience of glove use in healthcare settings. In addition, we have explored the views of student nurses nearing the end of their training about situations when they would wear NSCG to determine the extent to which their attitudes matched those of patients and what influenced their decision-making. The information captured by this study will help inform infection prevention strategies directed at improving the use of NSCG to ensure that care delivered is both safe and acceptable to patients.
Methods
Survey of student nurses’ attitudes to use of NSCG
A cohort of student nurses in their third year of training were asked to complete a questionnaire about their use of NSCG when they attended a university-based practical class. Participants were asked to indicate which of 46 different clinical tasks they would routinely wear NSCG and to select all relevant influences on their decision to wear NSCG from eight options. The students had not received any specific information or training about the use or misuse of NSCG other than that which formed part of their normal clinical training.
Survey of public perceptions of the use of NSCG by HCWs
Members of the public were recruited via social media from contacts of the research team, members of an HCAI service-user research forum (SURF) (Whitfield, 2015), public involvement contacts of the research team and from a notice in the University e-newsletter. Participants were asked to complete an online survey in SurveyMonkey©, which was developed with input from the HCAI SURF group. The survey aimed to explore the views on whether public would like HCWs to wear gloves for a range of clinical activities. In addition, respondents who indicated experience of being in hospital within the last six months were asked for their views on activities they had observed HCWs undertaking while using gloves and whether they felt this was appropriate, their views on specific activities they had observed HCWs using or not wearing gloves, whether they had ever challenged a HCW about their use of gloves and other comments they wished to make about HCW glove use (Table 1). Demographic data on age and gender were recorded. Free text comments were reviewed and content extracted to provide context to responses and represent general views of survey participants.
Table 1.
Survey questions of public on use of gloves by healthcare workers.
| 1. In the last six months, have you had personal experience of being a patient in an NHS hospital (either as an inpatient or as an outpatient)? [If ‘Yes’ answer all Qs; if ‘No’ answer Qs 6 (+/– 7), 8 (+/– 9), 10–13] 2. Thinking back to the time/s when you have been in a hospital, over the last six months, can you recall at least one occasion when a health professional (HP) wore gloves when caring for you? Examples of ‘health professionals’ are doctors, nurses, healthcare assistants and physiotherapists. 3. Please briefly describe what activities the HPs were undertaking while wearing gloves, for example ‘changing my dressing, taking a blood sample, etc’. 4. For each of the examples you have given above, please indicate if you feel it was/wasn’t appropriate for gloves to be worn. 5. Finally, for each of the examples you have given, please state why you felt it was or wasn’t appropriate for gloves to be worn 6. Can you think of any occasion where you have seen a HP undertaking an activity where they WERE NOT wearing gloves and you think they should have been? (This could have been during your care, the care of someone else or while the HP was undertaking some other activity.) 7. You said you have seen a HP undertaking an activity where they were not wearing gloves and you think they should have been. Please tell us what they were doing. 8. Can you think of any occasion where you have seen a HP wearing gloves when you think they SHOULD NOT have been? (This could have been during your care, the care of someone else or while the HP was undertaking some other activity.) 9. You said you have seen a HP wearing gloves when you think they should not have been. Please tell us what they were doing. 10. HPs carry out a number of activities; in the examples given below please indicate how you would feel about them wearing gloves while doing so (select from: I would like the HPs to wear gloves for this/I would feel uncomfortable with the HPs wearing gloves for this/I wouldn’t mind either way) ○ Taking my blood pressure ○ Giving me an injection ○ Making my bed ○ Giving me medication (tablets) ○ Helping me to eat ○ Taking a sample of my blood ○ Helping me off the toilet ○ Giving me a wash ○ Helping me walk to the toilet ○ Washing my private areas (genitals) ○ Changing my wound dressing ○ A doctor listening to my chest with a stethoscope ○ Helping me to get undressed for theatre ○ Cleaning my bedside table ○ Serving me tea and coffee 11. Do you want to make any other comments about HPs’ use of gloves? 12. Have you ever challenged a HP about their use of gloves while caring for you or a friend /relative? 13. You said that you have challenged a HP about their use of gloves. Please tell us about this. |
Both surveys included an assurance about maintaining confidentiality of the responses and consent was implied if participants chose to complete the survey. Ethical approval to conduct the survey of the public and interviews with student nurses was obtained from the College of Nursing, Midwifery and Healthcare Research Committee (CRSEC15).
Exploratory factor analysis
Exploratory factor analysis is a technique that attempts to uncover the underlying reasons (so-called ‘latent variables’) that cause people to act (or respond) in a certain way. In this research, respondents were asked about their behaviour (wear/do not wear gloves) when performing each of 46 tasks. But many of these tasks were similar and if the responses were consistent, similar responses should be given for similar tasks. By grouping together responses that are related (correlated) it may be possible to make inferences about the reasons behind these responses. Factor loadings were calculated for four factors. These factor loadings, which vary between −1 and +1, can be interpreted as the correlation between a variable and a factor. If a variable is highly correlated (near to +1 or −1) with Factor A, but not correlated with Factor B then that variable is said to ‘load’ onto Factor A. Loadings of more than 0.5 and less than −0.5 are considered high.
Results
Survey of nursing students
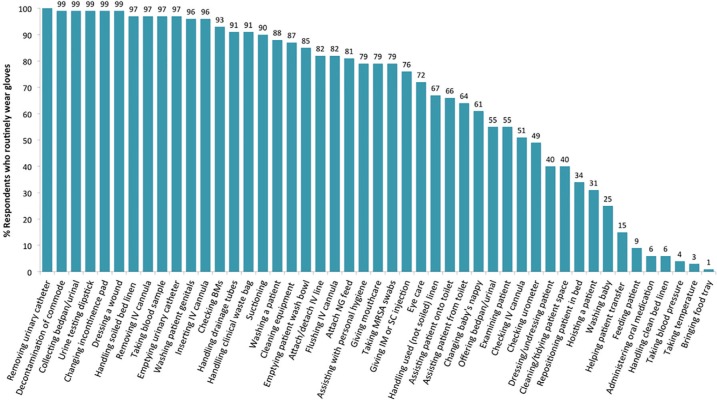
All of the 67 students in the class completed the questionnaire. The mean age of respondents was 29.5 years (SD ± 8.2), of whom 36 (63%) were aged 21–30 years, 15 (26%) were aged 31–40 years and six (10.5%) were aged over 40 years. The mean number of years working in healthcare settings was 4.6 years (SD ± 3.2). Responses about the routine use of clinical gloves for the 46 tasks are shown in Figure 1. While these responses indicated that almost all students would routinely wear NSCG for tasks involving contact with BBF such as removing an IV cannula and handling a bedpan, fewer reported using them for suctioning. The responses demonstrated inconsistencies in reported behaviour. For example, more students would wear gloves for washing an adult (59; 88.1%) than a baby (17; 25.4%) and changing a nappy (41; 61.2%) than an incontinence pad (66; 98.5%). In addition, there were many examples of tasks for which at least 40% of respondents indicated they would routinely wear NSCG but where their use would not be necessary, e.g. giving IM/SC injection (51; 76%), dressing a patient (27; 40%), taking MRSA swabs (53; 79%), handling used but not soiled linen (45; 67%), attaching/detaching an IV line (55; 82%), assisting a patient onto a commode/toilet (44; 65.7%). A smaller proportion of student nurses would wear gloves for very low-risk tasks such as feeding patients (6; 8.9%), administering oral medication (4; 6%) or taking blood pressures (3; 4.5%). Table 2 provides examples of where gloves are reported to be used routinely for procedures where their use is not indicated.
Figure 1.
Percentage of student nurses who would routinely wear NSCG for different clinical tasks.
Table 2.
Comparison of student nurse and public perception of appropriate use of NSCG (separated into those where gloves are and are not indicated).
| Task | Student nurses would routinely wear gloves (n = 67) |
Public would prefer HCW to wear gloves (n = 142) |
||
|---|---|---|---|---|
| n | % | n | % | |
| Procedures where gloves ARE indicated | ||||
| Removing urine catheter | 67 | 100.0 | – | – |
| Collecting a bedpan/urinal | 66 | 98.5 | – | – |
| Changing an incontinence pad | 66 | 98.5 | – | – |
| Dressing a wound | 66 | 98.5 | 135 | 95.1 |
| Decontaminating a commode | 66 | 98.5 | – | – |
| Removing an IV cannula | 65 | 97.0 | – | – |
| Emptying urinary catheter | 65 | 97.0 | – | – |
| Checking blood glucose | 62 | 92.5 | – | – |
| Suctioning | 60 | 89.5 | – | – |
| Changing a baby’s nappy | 41 | 61.2 | – | – |
| Procedures where gloves ARE NOT indicated | ||||
| Washing a patients’ genital areas | 64 | 95.5 | 133 | 93.7 |
| Washing/ bathing/showering patient | 59 | 88.1 | 83 | 58.5 |
| Attaching/detaching IV line | 55 | 82.1 | – | – |
| Taking MRSA swabs | 53 | 79.1 | – | – |
| Giving IM/SC injection | 51 | 76.1 | 93 | 65.5 |
| Handling used (not soiled) bed linen | 45 | 67.0 | 7 | 4.9 |
| Assisting patient onto toilet/commode | 44 | 65.7 | 9 | 6.3 |
| Assisting patient transfer from commode to bed/chair | 43 | 64.2 | 101 | 71.1 |
| Cleaning/tidying patient bed space | 27 | 40.1 | 37 | 26.1 |
| Dressing/undressing a patient | 27 | 40.0 | 12 | 8.5 |
| Washing a baby | 17 | 25.4 | – | – |
| Helping patient transfer from bed to chair | 10 | 14.9 | – | – |
| Feeding a patient | 6 | 8.9 | 12 | 8.5 |
| Handling clean bed linen | 4 | 6.0 | – | – |
| Administering oral medication | 4 | 6.0 | 15 | 10.6 |
| Taking blood pressure | 3 | 4.5 | 4 | 2.8 |
The four factors identified in the exploratory factor analysis provide some possible insights into decision-making by student nurses about the use of NSCG (Table 3). The tasks listed under each factor are highly correlated, i.e. the responses given for the set of tasks within a factor are consistent. This suggests that a respondent who chooses to wear gloves for ‘handling drainage tubes’ is also going to choose to wear them for ‘suctioning’ or ‘attaching an NG tube’. In the case of Factor 1, these are procedures perceived to be ‘risky’, although some do not involve a risk of exposure to BBF such as taking MRSA swabs, attaching an NG feed or IM/SC injections. Factor 2 reflects tasks for which there is likely to be a strong tendency to either wear gloves (e.g. changing an incontinence pad) or not wear gloves (e.g. feeding a patient). Factor 3 reflects procedures where there is not a risk of exposure to BBF but for which some student nurses would consistently wear gloves and Factor 4 comprises tasks linked to personal hygiene for which it is routinely perceived that gloves are required regardless of potential exposure to BBF.
Table 3.
Exploratory factor analysis of student nurses’ reported routine use of NSCG.
| Factor 1 |
Factor 2 |
Factor 3 |
Factor 4 |
|---|---|---|---|
| Perceived to be ‘risky’ | Definitive indication for ‘gloves’ or ‘no gloves’ | Low-risk task but wear gloves | Personal hygiene |
| Handling drainage tubes | Taking temperature | Repositioning patient in bed | Wash a patient |
| Handling clinical waste bags | Taking blood pressure | Cleaning/tidying patient space | Assisting patient with personal hygiene |
| Giving IM/SC injections | Changing continence pad* | Dressing/undressing patient | Emptying patient wash bowl |
| Suctioning | Inserting IV cannula* | Hoisting a patient | Assisting patient onto commode/toilet |
| Attach NG feed | Helping patient transfer from bed to chair | Assisting patient from commode to chair/bed | |
| Giving mouth care | Feeding patient | ||
| Emptying urine drainage bag |
All coefficients greater than 0.5 and positive except * which are negative.
Interestingly, ‘washing a baby’ is not correlated with the personal hygiene (Factor 4) and changing a nappy is not correlated with Factors 1 or 2 (procedures perceived to be risky or a strong tendency to wear/not wear gloves). This suggests that student nurses do not categorise the risk of exposure to BBF or ‘dirt’ for these tasks in the same way that they would for adult patients.
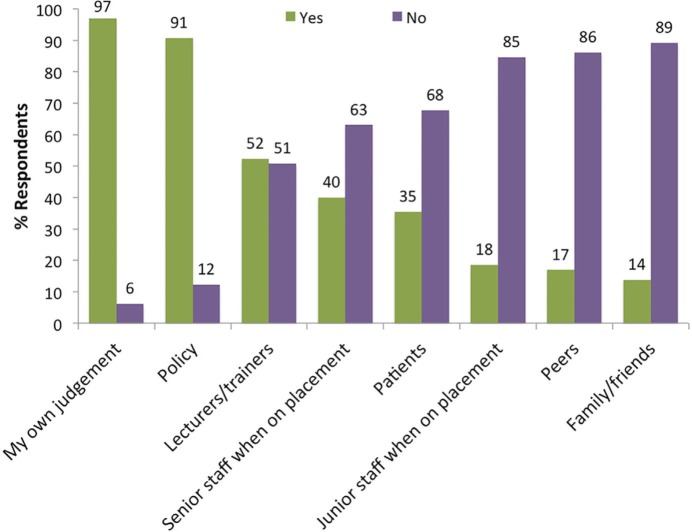
The students indicated that the most common influence on their decision to use NSCG was their own judgement (63; 94%), followed by policy (59; 88.1%), lecturers/trainers (34; 50.7%) and senior staff in their placements (26; 38.8%) (Figure 2).
Figure 2.
Influences on the decision of student nurses to wear NSCG.
Public survey
A total of 142 responses to the survey were received from members of the public. The mean age of the respondents was 49.2 years (SD ± 11.7) and the majority (87; 61%) were women. Eighty respondents (56%) indicated that they had experienced a visit to hospital within the last six months and reported 107 activities where HCWs had worn gloves to care for them. The most common reported activities were minor invasive procedures (28; 26.2%) and phlebotomy (27; 25.2%) (Table 4). However, while most respondents thought that glove use was appropriate, for 23.4% (25/107) of reported activities their use was considered inappropriate. Of the respondents who had been in hospital in the last six months, 29% (23/80) indicated that they had observed inappropriate use of gloves.
Table 4.
Activities where members of the public observed HCWs wearing gloves and their opinion on appropriateness.
| Procedure | Activity where glove use reported |
Glove use considered inappropriate |
Comments | |
|---|---|---|---|---|
| Respondents (n) | n | % | ||
| Administrative task | 5 | 4 | 80 | They had gloves on the whole time they treated me; no need for gloves when writing notes |
| Bed-making | 6 | 4 | 66.6 | The bed wasn’t soiled |
| Handling body fluids | 6 | 1 | 17 | I didn’t see the need as I only need assistance and wasn’t touched |
| Injections/IVs | 8 | 2 | 25 | Not required as a non-needle system just attaching a drip line to the end of a venflon |
| Minor invasive procedure | 28 | 1 | 3.6 | I didn’t see them wash their hands and think it was for their protection not mine |
| Phlebotomy | 27 | 5 | 18.5 | No risk as used safer device; would not appear to be body fluid present |
| Non-invasive care | 6 | 2 | 33.3 | No need for wearing gloves when pushing wheel chair |
| Clinical examination | 12 | 3 | 2.8 | No lesions or open wounds visible; scar was fine, no bodily fluids present |
| Dressings | 6 | 0 | 0 | |
| Washing | 3 | 3 | 100 | I am quite clean; unless the HCW needed protecting from the washing cream or me from them, it made the task more difficult and probably unnecessarily exposed me to latex |
| Total | 107 | 25 | ||
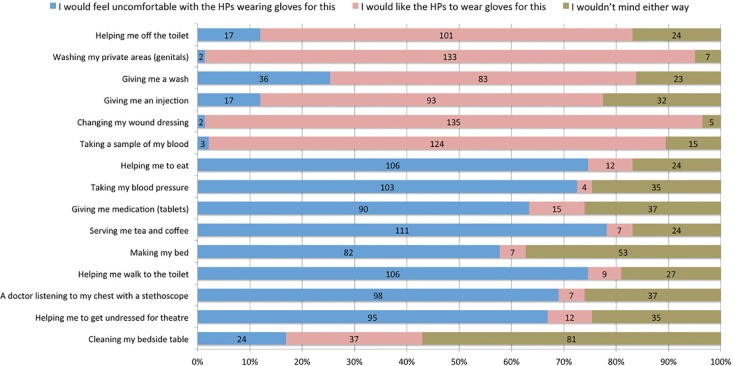
All 142 respondents were asked about procedures that they would like HCWs to wear gloves for (Figure 3 and Table 2). They primarily indicated activities that would be recommended by standard precautions policies, e.g. changing wound dressing (135; 95.1%), taking blood samples (124; 87.3%) and helping off the toilet (101; 71.1%). Respondents reported being uncomfortable with HCWs undertaking personal tasks wearing gloves, such as helping walk to the toilet (107; 74.6%), doctor listening to chest (98; 69%), helping to dress (95; 66.9%), helping to eat (107; 74.6%) or serving tea and coffee (111; 78.2%). For some less personal tasks, such as cleaning a bedside table and making beds, a high proportion of respondents would not mind either way if HCWs used gloves (Figure 3). Although 58.5% (82/142) of respondents said they would prefer HCWs to use gloves to give them a wash, there was stronger support for the use of gloves (133; 93.7%) for washing ‘private parts’. For most comparable procedures, the student nurses’ responses corresponded with those of the public. For some personal tasks, such as assisting to toilet, dressing and cleaning the bed areas, a higher proportion of the public were uncomfortable with HCWs wearing gloves (Table 2), but the student nurses indicated they often did so. The proportion of the public who would prefer HCWs to wear gloves for washing them was less than that reported by student nurses (58.5% versus 88.1%). However, the proportion of both the public and student nurses preferring the glove use for washing genital areas was similar (93.7% versus 95.5%).
Figure 3.
Public views on use of clinical gloves for 15 activities performed by HCWs.
A total of 38 (27%) respondents commented on the observed use of gloves by HCWs. The majority (24; 63%) conveyed a negative opinion of glove use including: a perception that HCWs over-used gloves (n = 8), that they were not changed between tasks or patients (n = 7), were used to protect the HCW rather than the patient (n = 2) and in place of hand hygiene (n = 3). Concerns were also raised about exposure of patients to latex and that patients were never asked if they had a latex allergy. However, 24% (9/38) of comments were positive about HCW glove use, with respondents confident that HCWs knew when to wear gloves and associated their use with the prevention of infection (n = 7), a perception that gloves were important to reduce damage to hands (n = 1) and that routine use prevented attention being drawn to patients with infections (n = 1).
The 25 respondents with recent experience of healthcare also gave examples of inappropriate use of NSCG including: bed-making (n = 8), writing notes/on phone (n = 5), observations (n = 4), walking around ward/to toilet (n = 3), washing (n = 2) and patient examination (n = 1). One respondent commented that ‘they did not change gloves between patients’, another that ‘they were put on way to soon’ and another that ‘they were wearing gloves for the whole of my consultation, they didn’t wash their hands yet touched a large number of items in the room including a keyboard and phone’.
A total of 29 (20.4%) patients recalled occasions where they had challenged a HCW about their glove use. Most of these (11; 37.9%) involved situations where the need to use gloves was questioned or gloves not being changed between procedures/patients was challenged (7; 24.1%). However, on 31% (9/29) of occasions respondents challenged HCWs about the need for them to wear gloves for contact with body fluids or a patient under isolation precautions. The following examples illustrate how such challenges may not be well received by the HCWs:
‘I asked the Dr to change his gloves after he answered the phone in them, adjusted my table to his height, collected the blood bottles and opened doors before he tried to take my blood so I insisted he changed his gloves. I was told by the Dr that the gloves were for his benefit not mine! I politely but firmly insisted he change them and he did… in a very dramatic fashion!’ [R3]
‘A nurse taking a blood sample wasn’t wearing gloves – I had assumed it was standard practice. I didn’t really get an answer when I asked her why not (it wasn’t a challenge just a question).’ [R24]
‘They asked me to talk to the practice manager and made me feel uncomfortable. I didn’t see them wash their hands and I was about to have an injection. The practice manager asked them to take off the gloves and wash their hands. Not a nice experience at all.’ [R22]
Discussion
This study has demonstrated that while almost all student nurses reported using NSCG appropriately for procedures involving a risk of contact with BBF, a significant proportion also routinely used NSCG for a wide range of low-risk tasks and procedures for which they are neither required nor recommended, such as washing patients, helping them onto a commode or helping them to dress (WHO, 2009). Some appear to routinely wear them for almost all tasks. This suggests that the rationale of student nurses for using NSCG is not based on accurate assessment of risk of exposure to BBF. For example, the survey demonstrated that almost all would wear NSCG routinely for washing adult patients, yet only one-quarter would wear them for washing a baby. Not only are NSCG not required for washing patients (in the absence of BBF), but the microbial flora of a baby’s skin closely resembles the denser population of moist sites on adult skin (Oranges et al., 2015). In addition, unlike the skin of an adult patient, a baby’s skin is almost inevitably contaminated with BBF, yet the study suggests that BBF from babies is perceived to have a lower risk than that of adults, with respondents significantly more likely to use gloves to change an incontinence pad than a baby’s nappy. The perception that certain sorts of tasks require the use of gloves regardless of the actual risk of exposure to BBF is also borne out by the factor analysis which demonstrated that a significant proportion of student nurses were likely to consistently wear gloves for delivering ‘personal hygiene’ and other low-risk tasks perceived to be ‘risky’.
The findings in our study are supported by those reported by Radcliffe and Smith (2014) who, in a survey of 89 third-year student nurses, found 88% would use gloves for washing a patient, 98% for washing their genital area and 55% for changing patient clothing and serving food. Another qualitative study based on clinical scenarios also found that student nurses did not use an evidence-based rationale to inform their hand hygiene or glove-use choices, and more worryingly, the attitudes of infection control specialists included in the study were similar (Lee, 2013).
In the case of attaching an intravenous line, for which NSCG would be worn by over 80% of respondents, there may be a perception that gloves are required because this is an ‘aseptic task’. The use of NSCG in this situation is superfluous, given that they are not sterile. Touching of the sterile components of the IV device should be avoided with either hands or NSCG and use of alcohol hand gel immediately prior to undertaking the procedure would be appropriate. The use of NSCG for such procedures may actually increase the risk of contamination, given that they are frequently put on too early and not changed between procedures and therefore at the point of use are likely to be contaminated (Girou et al., 2004; Loveday et al., 2014b; Snyder et al., 2008; Wilson et al., 2015). The assumption that NSCG taken from a box are uncontaminated is not borne out by evidence, with 50% found to be contaminated by skin commensals and 13% by pathogens (Hughes et al., 2013). In the case of taking MRSA swabs, again the rationale for the use of NSCG is obscure, given that the nares are not touched except with the end of a swab; yet 79% of student nurses reported using gloves for this task.
Policy was cited by almost 90% of student nurses as an influence on their decision to wear NSCG. This is interesting given that many of the situations in which they indicated they would routinely use gloves would not be justified by infection control policy. This suggests that either the student nurses were not familiar with the content of policies or the policies do not contain clear recommendations about the use of gloves and underpinning principles of risk assessment. Indeed, Ratcliffe and Smith (2014) found that students are confused about the appropriate use of NSCG and would prefer to be given specific instructions on when and when not to wear them.
The practice of nursing students is often attributed to the instruction from their tutors, yet only half of the respondents cited their tutors as an influence on their practice. Other studies have suggested that mentors are a key influence, with students adopting the practice of others that they work with in order to ‘fit in” (Barrett and Randle, 2008; Lee, 2013; Ratcliffe and Smith, 2013). However, in our study less than 40% of students indicated their decision as influenced by other staff. The most frequently cited influence (94%) on the decision to use NSCG was students’ own judgement. This resonates with other work which has found that HCWs perceive the decision to wear NSCG as a personal one, that others do not have the right to challenge, and NSCG are used in response to an aversion to touching patients (Lee, 2013; Loveday et al., 2014b). This suggests that the improvement strategies such as those used to address hand hygiene, which rely on education and encouraging challenge by peers, are unlikely to be effective in changing glove-use behaviour. Infection control policy needs to be much clearer in directing how and when gloves should be used and not used so that there is less room for ‘personal preference’ and more support for challenging inappropriate use.
Whitby et al. (2006) describes hand hygiene in healthcare settings as a ritualised behaviour that is performed mainly for self-protection and strongly influenced by emotional perceptions about dirtiness and cleanliness that relates to both situations and other people. For example, they found that a family source was considered to be much less harmful than non-family and public sources, and there was a strong intention to perform hand hygiene when hands have been somewhere considered to be ‘emotionally dirty’ such as groins, genitals and axillae. Our findings on the use of NSCG resonates with these findings, in particular the strong intention to use NSCG for contact with genital areas, and suggests that NSCG are used as a ‘protective’ barrier to this emotional response (Lee, 2013; Loveday et al., 2014b; Ratcliffe and Smith, 2013). There are significant dangers associated with widespread use of NSCG in place of hand hygiene. Since they are perceived to protect the hands, they are likely to diminish the usual triggers for hand hygiene, i.e. glove removal, and this may explain the high risk of cross-contamination associated with their use (Loveday et al., 2014b; Wilson et al., 2015).
This study is the first to attempt to establish the views of patients and users of healthcare services about the use of NSCG by HCWs. The members of the public in this survey recognised the need for HCWs to use NSCG for procedures involving contact with BBF, e.g. changing wound dressing and taking blood, and that gloves contributed to reducing the risk of HCAIs. However, the public responders were uncomfortable with their use for some personal tasks for which a high proportion of nursing students would routinely wear NSCG, e.g. helping onto the toilet or to dress. Surprisingly, 58% of respondents in the public survey preferred HCWs to wear gloves for washing, although almost 90% of student nurses would use NSCG for this task, and a very high proportion of both student nurses and the public survey respondents preferred the use of gloves for washing genital areas. This suggests that the psychological barrier perceived by HCW is similarly recognised by their patients and while NSCG may not be indicated for infection control reasons, there is a clear patient preference for HCWs to use them in this situation (Loveday et al., 2014b).
This study has provided evidence that patients notice inappropriate use of gloves by HCWs. One-third of respondents with recent experience of healthcare had observed HCWs use gloves inappropriately. These respondents had a clear sense of situations where NSCG were used but not required, identifying needle-free IV systems and examinations with no contact with BBF as not requiring gloves, as well as less personal tasks such as pushing a wheelchair and bed-making. Comments made by respondents, regardless of whether they had recent experience of healthcare, indicated that many perceived that HCW over-used NSCG and did not change them between tasks or patients.
While patients or their carers might observe care being delivered with potentially contaminated gloves, challenging inappropriate use of NSCG may be difficult. This study has provided some stark examples of how the reasonable concerns of patients are not recognised by the staff members concerned. This is probably hardly surprising given the absence of rationale associated with the use of NSCG and the lack of recognition by HCW, who are primarily using them as a barrier for themselves, that they become contaminated by the things they touch. In addition, there is evidence that patients have concerns about confronting HCWs because of wanting to avoid trouble or fears that it might adversely affect their care (Seale et al., 2015).
Limitations of this study
This was a small sample of nursing students from single university and therefore may not be representative of all students or other HCWs. The sampling procedure for public survey was a convenience method and it is not possible to determine how representative this sample is of patients or the general public. Some respondents were members of service user groups and therefore likely to have an interest in HCAIs and gloves.
Implications of study for infection control practitioners
This study has illustrated that nursing students routinely use NSCG in a wide variety of situations where they are not indicated. Their use as a barrier to protect HCWs from perceived hazards needs to be challenged given that inappropriate use increases the risk of infection to the patient and reduces hand hygiene. However, patient’s preference for the psychological barrier that gloves provide in relation to intimate contact should also be taken into account. As personal judgement appears to strongly influence decisions about glove use, policies should give explicit advice about situations where NSCG are and are not required; the underpinning principles of risk assessment in clinical settings; and the dangers of cross-contamination associated with the misuse of NSCG. These policies should also address the strong desire of patients for HCWs to wear gloves in some situations but communicate this rationale clearly. Mechanisms to support both HCWs and patients to challenge inappropriate use of NSCG need to be developed and embedded across all care settings.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funded by a research grant from the Infection Prevention Society.
Peer review statement: Not commissioned; blind peer-reviewed.
References
- Barrett R, Randle J. (2008) Hand hygiene practices: nursing students’ perceptions. Journal of Clinical Nursing 17: 1851–1857. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Prevention & Control. (1988) Update: universal precautions for prevention of transmission of human immunodeficiency virus, hepatitis B virus and other blood borne pathogens in healthcare settings. Morbidity and Mortality Weekly Report 37: 377–388. [PubMed] [Google Scholar]
- Flores A, Pevalin DJ. (2006) Healthcare workers’ compliance with glove use and the effect of glove use on hand hygiene compliance. British Journal of Infection Control 7: 15–19. [Google Scholar]
- Fuller C, Savage J, Besser S, Hayward A, Cookson B, Cooper B, Stone S. (2011) “The dirty hand in the latex glove”: a study of hand hygiene compliance when gloves are worn. Infection Control and Hospital Epidemiology 32: 1194–1199. [DOI] [PubMed] [Google Scholar]
- Girou E, Chaia SHT, Oppeina F, Legrandb P, Ducelliera D, Cizeaua F, Brun-Buisson C. (2004) Misuse of gloves: the foundation for poor compliance with hand hygiene and potential for microbial transmission? Journal of Hospital Infection 57: 162–169 [DOI] [PubMed] [Google Scholar]
- Hughes KA, Cornwall J, Theis J, Brooks HJL. (2013) Bacterial contamination of unused, disposable non-sterile gloves on a hospital orthopaedic ward. Australasian Medical Journal 6: 331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee K. (2013) Student and infection prevention and control nurses’ hand hygiene decision making in simulated clinical scenarios: a qualitative research study of hand washing, gel and glove use choices. Journal of Infection Prevention 14: 96–103. [Google Scholar]
- Loveday H, Lynam S, Singleton J, Wilson J. (2014. a) Clinical glove use: healthcare workers actions and perceptions. Journal of Hospital Infection 86: 110–116. [DOI] [PubMed] [Google Scholar]
- Loveday H, Wilson J, Pratt R, Golsorkhi M, Tingle A, Bak A, Browne J, Prieto JA, Wilcox M. (2014. b) epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. Journal of Hospital Infection 86 (Suppl. 1): S1–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oranges T, Dini V, Romanelli M. (2015) Skin physiology of the neonate and infant: Clinical implications. Advances in Wound Care 4: 587–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratcliffe S, Smith J. (2014) Factors influencing glove use in student nurses. Nursing Times 110: 18–21. [PubMed] [Google Scholar]
- Royal College of Nursing. (2012) Tools of the trade: RCN guidance for healthcare staff on glove use and the prevention of contact dermatitis. London: Royal College of Nursing. [Google Scholar]
- Seale H, Travaglia J, Chughtai A, Phillipson L, Novytska Y, Kaur R. (2015) ‘I don’t want to cause any trouble’: the attitudes of hospital patients towards patient empowerment strategies to reduce healthcare-acquired infections. Journal of Infection Prevention 16: 167–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel JD, Rhinehart E, Jackson M, Chiarello L. Health Care Infect Control Practices and Health Care Infection Control Practices Advisory Committee. (2007) 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. American Journal of Infection Control 35: S65–S164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder G, Thom K, Furuno J, Perencevich E, Roghmann M, Strauss S, Netzer G, Harris A. (2008) Detection of methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci on the gowns and gloves of healthcare workers. Infection Control and Hospital Epidemiology 29: 583–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitby M, McLaws M, Ross M. (2006) Why healthcare workers don’t wash their hands: a behavioral explanation. Infection Control and Hospital Epidemiology 27: 484–492. [DOI] [PubMed] [Google Scholar]
- Whitfield A. (2015) Different perspectives, same goals. Journal of Infection Prevention 16: 197–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson J, Prieto J, Singleton J, O’Connor V, Lynam S, Loveday H. (2015) The misuse and overuse of non-sterile gloves: application of an audit tool to define the problem. Journal of Infection Prevention 16: 24–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2009) WHO Patient Safety. WHO guidelines on hand hygiene in health care. Geneva: World Health Organization. [Google Scholar]