Abstract
Background:
Healthcare-associated infections (HAIs) are common and harmful to patients. Effective hand hygiene can help prevent HAIs, however, suboptimal healthcare worker hand hygiene remains problematic across the globe. This study analyses the impact of organisational changes on hand hygiene.
Methods:
This observational study assessed hand hygiene by different professions before and after a merger of a recently combined infectious diseases (ID) unit coupled with a qualitative study about barriers to optimal hand hygiene. Direct observations were compared with previous data collected on both units before they merged. We also conducted focus groups with the doctors and nurses about hand hygiene.
Results:
After two ID units merged in 2013, we observed 681 provider–patient interactions. We compared these with a previous observation period in 2012. Hand hygiene adherence among nurses significantly declined after the merger (from 36% to 24%, P <0.001). However, adherence among doctors increased from 51% to 63% after the merger (P = 0.004). Data from the focus groups revealed a gap between doctor and nurses perceptions of education and goal adherence rates.
Conclusions:
Our findings underscore the important role played by effective unit leaders to prevent infection. We found long-term sustainability of hand hygiene practices among doctors. However, adherence among nurses was substantially lower.
Keywords: Patient safety, leadership, infection control
Introduction
Suboptimal adherence to appropriate hand hygiene practice has been a worrisome global trend (Ellingson et al., 2014). In Italy, since 2008, an abrupt and notable increase in the proportion of carbapenem-resistant Klebsiella pneumoniae has been reported corresponding with an endemic situation (Giani et al., 2013; Monaco et al., 2014). In response, a multi-modal intervention was implemented in one of the infectious diseases (ID) units (unit 1) at a hospital in Florence, Italy to improve levels of healthcare worker hand hygiene (Saint et al., 2009).
The intervention was in concordance with the hand hygiene strategy recommendations of the World Health Organization (WHO) (World Health Organization, 2009) and the Society for Healthcare Epidemiology of America (SHEA)/Infectious Disease Society of America (IDSA) (Ellingson et al., 2014). It included education of physicians and nurses about infection and hand hygiene with an emphasis on alcohol-based hand rub.
Additionally, physician and nurse champions were identified to promote hand hygiene (di Martino et al., 2011; Saint et al., 2009). This initial work was followed with a four-year post-intervention assessment of the sustainability in unit 1 (Lieber et al., 2014). Hand hygiene adherence was compared to a second ID unit (unit 2) in the same hospital that did not participate in the original intervention. The findings demonstrated a statistically significant improvement in hand hygiene among doctors in unit 1 (Lieber et al., 2014). However, in unit 2, hand hygiene adherence was low (adherence of 16% for nurses and 18% for doctors for the entire assessment period). Adherence dropped during this assessment from approximately 50% to 7.5% among nurses and 2.6% among doctors after the departure of a physician director who was a hand hygiene leader (Lieber et al., 2014).
Hand hygiene continues to be a priority at the hospital, and therefore an additional post-intervention study was conducted following a significant shift in the ID paradigm. In 2013, the two ID units merged. The doctors and nurses from both units continued in the same capacity in the newly combined unit, but were now under the management of the director of unit 1. The goal of this latest observational study was to determine what, if any, impact these structural shifts had on hand hygiene adherence.
Methods
Observation of hand hygiene adherence
This observational study assessed the current rates of hand hygiene among doctors and nurses in a recently combined ID unit at a hospital in Florence, Italy. These observations were compared with previous data collected one year before the merger (Lieber et al., 2014).
One of the study authors (CP) served as the sole observer to collect data on hand hygiene adherence in the combined ID unit in October 2014. Observations were conducted daily throughout the unit and utilised the same methods as was used in the previous assessment (Lieber et al., 2014).
We again focused on hand hygiene before contact with patients, which corresponds to moment one of the WHO Five Moments for Hand Hygiene (Pittet et al., 2009). Appropriate hand hygiene was defined as either hand washing with soap and water or use of an alcohol-based hand rub immediately prior to patient contact. This included hand hygiene prior to donning gloves, when required. Providers were observed during nursing pre-rounds, vital checks/medication administration and clinical rounds. Providers were informed that the observer was present to conduct a survey in an infection control capacity.
Assessment of barriers
To provide insight into the unit’s hand hygiene adherence, two focus groups were convened with providers from the combined ID unit: one with nurses and the other with doctors. The groups were moderated by the director of the combined unit. Questions focused on how providers felt about hand hygiene and any barriers they perceived to proper hand hygiene adherence.
Statistical analysis
Adherence rates were calculated for doctor and nurse providers in the combined unit. The data were double-entered into a Microsoft Access database and checked for errors. Hand hygiene adherence rates were calculated and compared between provider groups (doctors and nurses) as well as between the combined unit before and after the merger using Pearson χ2 testing. In all cases, two-tailed P ≤0.05 was considered statistically significant.
Results
In October 2014, after the merger in August 2013, 681 provider–patient interactions in the newly combined ID unit were observed (232 doctor encounters and 449 nursing encounters). Before merger observations were conducted between January and November 2012 in both ID units (248 nurse and 249 doctor observations in unit 1; 317 nurse and 230 doctor observations in unit 2). In total there were 565 nurse and 479 doctor observations for both units combined in 2012. The units merged in August 2013. Hand hygiene adherence among doctors increased from 51% before the merger to 63% after the merger, P = 0.004 (Figure 1). However, adherence among nurses significantly declined after the merger (36% before to 24% after, P <0.001).
Figure 1.
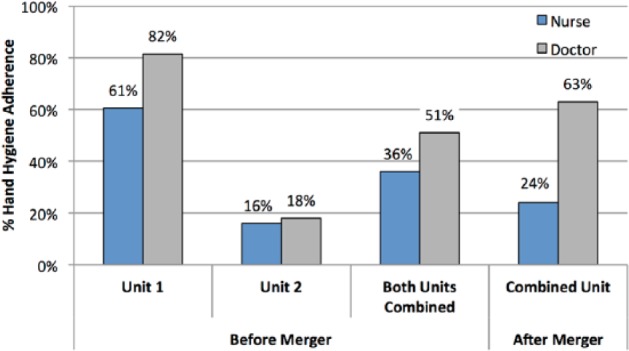
Percentage adherence to appropriate hand hygiene before patient contact by clinician type in two ID units: before and after units merged in August 2013.
Adherence impact: focus group findings
A total of 14 nurses and ten doctors participated in the focus groups. Both doctors and nurses gave positive feedback and valued the relatively recent addition of alcohol-based hand rub dispensers outside every room and portable individual hand sanitiser bottles.
The nurses reported lack of education, increased workload, unclear expectations and unwillingness to enforce or assign peers to enforce the proper hand hygiene protocol. They shared that they were unfamiliar with the WHO’s Five Moments for Hand Hygiene; however, most did request more information and education on appropriate hand hygiene practice.
The doctors were aware of the WHO’s Five Moments for Hand Hygiene, but the details and agreement on adherence of their peers were unclear. They also reported a lack of education. Notably, the doctors’ goal adherence rate was 75–100%, while the nurses thought 50–70% adherence was acceptable.
Discussion
This study assesses the effect of a merger of two ID units on hand hygiene adherence, as well as the long-term sustainability of a prior multi-modal hand hygiene intervention in one of the units. We performed 1725 provider–patient observations through the pre- and post-merger studies. There was an increase in doctors’ adherence, which was consistent with a prior study on unit 1 (Lieber et al., 2014). In both the prior and current study, doctors had a well-defined and motivated champion for hand hygiene practices. However, in the newly combined unit, the nursing staff did not have an analogous hand hygiene counterpart, which may have contributed to the substantial decline in adherence.
Unlike most prior studies, the adherence rate of nurses was notably lower than that of the physicians in this combined unit. A review of 96 studies, among all healthcare workers, found that physicians tend to have lower overall compliance rate (32%) versus nurses at 48% (Erasmus et al., 2010).
One factor that may promote hand hygiene adherence is the presence of a clearly identified leader to motivate the staff. Prior to August 2013, the two ID units had different directors. Unit 1’s director was a champion for hand hygiene. Unit 2, which did not participate in the prior intervention, did not have a physician champion promoting hand hygiene practices. Data from before the merger in 2012 demonstrated doctors’ hand hygiene adherence was 82% in unit 1 compared with 18% in unit 2, while for nurses it was 61% in unit 1 compared with 16% in unit 2 (Lieber et al., 2014).
A second factor could be related to lack of regular feedback mechanisms. The WHO recommends hand hygiene evaluation be performed regularly, at least annually, to monitor improvement in adherence and identify potential targets of additional intervention (World Health Organization, 2009). While neither doctors nor nurses had regular monitoring, this may have contributed to the lack of sustained improvement with nursing.
Our study has several limitations. First, we focused on hand hygiene prior to patient contact, which is only one of the WHO’s Five Moments for Hand Hygiene (Erasmus et al., 2010). The absolute rates that we report can be compared only with those from studies using the same approach. Second, our observations were performed over a relatively short period of one-month. To minimise the likelihood of a Hawthorne effect, the observations were performed during a short period and the focus of observation was not disclosed to the nurses or doctors. Finally, the hospital does not maintain records of healthcare-acquired infections of every patient. Therefore, we were unable to correlate hand hygiene adherence rates with healthcare-associated infection rates.
Conclusions
Our observational study revealed that provider hand hygiene adherence is suboptimal in a recently merged ID unit in Italy (63% for doctors and 24% for nurses). However, improvement of hand hygiene practices was seen among doctors, who had the benefit of a physician leader who championed hand hygiene. The adherence rate among nurses, who did not have an effective champion, was substantially lower. In addition to increased education, accountability and targeted behavioural changes for both groups, a nursing leader to facilitate improved hand hygiene practices appears to be needed. Engaged and effective leadership appears to be important to the sustainable success of hand hygiene improvement initiatives.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Peer review statement: Not commissioned; blind peer-reviewed.
References
- di Martino P, Ban KM, Bartoloni A, Fowler KE, Saint S, Mannelli F. (2011) Assessing the sustainability of hand hygiene adherence prior to patient contact in the emergency department: A 1-year postintervention evaluation. American Journal of Infection Control 39: 14–18. [DOI] [PubMed] [Google Scholar]
- Ellingson K, Haas JP, Aiello AE, Kusek L, Maragakis LL, Olmsted RN, Perencevich E, Polgreen PM, Schweizer ML, Trexler P, VanAmringe M, Yokoe DS. and Society for Healthcare Epidemiology of America (SHEA). (2014) Strategies to prevent healthcare-associated infections through hand hygiene. Infection Control and Hospital Epidemiology 35: 937–960. [DOI] [PubMed] [Google Scholar]
- Erasmus V, Daha TJ, Brug H, Richardus JH, Behrendt MD, Vos MC, van Beeck EF. (2010) Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infection Control and Hospital Epidemiology 31: 283–294. [DOI] [PubMed] [Google Scholar]
- Giani T, Pini B, Arena F, Conte V, Bracco S, Migliavacca R, AMCLI-CRE Survey Participants, Pantosti A, Pagani L, Luzzaro F, Rossolini GM. (2013) Epidemic diffusion of KPC carbapenemase-producing Klebsiella pneumoniae in Italy: results of the first countrywide survey, 15 May to 30 June 2011. Euro Surveillance 18: 20489. [PubMed] [Google Scholar]
- Lieber SR, Mantengoli E, Saint S, Fowler KE, Fumagalli C, Bartolozzi D, Magistri L, Niccolini F, Bartoloni A. (2014) The effect of leadership on hand hygiene: assessing hand hygiene adherence prior to patient contact in 2 infectious disease units in Tuscany. Infection Control and Hospital Epidemiology 35: 313–316. [DOI] [PubMed] [Google Scholar]
- Monaco M, Giani T, Raffone M, Arena F, Garcia-Fernandez A, Pollini S, Network EuSCAPE-Italy, Grundmann H, Pantosti A, Rossolini GM. (2014) Colistin resistance superimposed to endemic carbapenem-resistant Klebsiella pneumoniae: a rapidly evolving problem in Italy, November 2013 to April 2014. Euro Surveillance 19: 20939. [DOI] [PubMed] [Google Scholar]
- Pittet D, Allegranzi B, Boyce J. and World Health Organization World Alliance for Patient Safety First Global Patient Safety Challenge Core Group of Experts. (2009) The World Health Organization Guidelines on Hand Hygiene in Health Care and their consensus recommendations. Infection Control and Hospital Epidemiology 30: 611–622. [DOI] [PubMed] [Google Scholar]
- Saint S, Conti A, Bartoloni A, Virgili G, Mannelli F, Fumagalli S, di Martino P, Conti AA, Kaufman SR, Rogers MA, Gensini GF. (2009) Improving healthcare worker hand hygiene adherence before patient contact: a before-and-after five-unit multimodal intervention in Tuscany. Quality & Safety in Health Care 18: 429–433. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2009) Guide to implementation. A guide to the implementation of the WHO multimodal hand hygiene improvement strategy. Geneva: WHO; Available at: http://www.who.int/gpsc/5may/Guide_to_Implementation.pdf. [Google Scholar]


