Abstract
The peritoneal cavity is subdivided into supracolic and infracolic compartments by transverse colon and its mesocolon. The supracolic compartment contains the liver, spleen, stomach, and lesser omentum. The infracolic compartment contains the coils of small bowel surrounded by ascending, transverse, and descending colon and the paracolic gutters. The imaging of different compartments is possible by various methods such as ultrasound (US) and computerized tomography. The treating physicians should be familiar with the relevant radiological anatomy of different compartments and spaces as accurate localization of fluid collection/lymph node in peritoneal cavity greatly aids in selection of a treatment strategy. The role of endoscopic US (EUS) is emerging for detail evaluation of all parts of peritoneal cavity as it provides an easy access for fine-needle aspiration from different compartments of peritoneal cavity. In this review, we describe the techniques of evaluation of different parts of supracolic compartments of peritoneum by EUS.
Keywords: Endoscopic ultrasound, liver, peritoneal ligaments, peritoneal spaces, retroperitoneum, spleen, stomach
Introduction
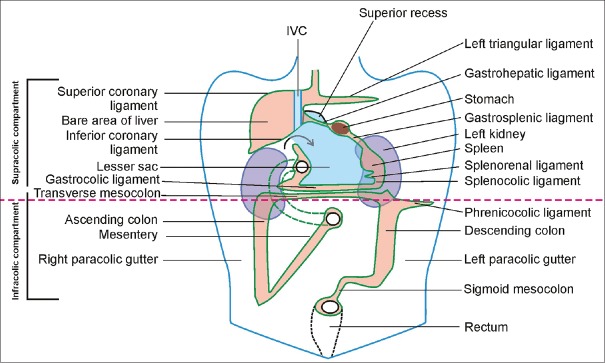
The abdominal cavity contains three potential spaces, i.e., the peritoneal cavity, subperitoneal space, and retroperitoneum.[1] The subperitoneal space, which is enclosed by double-layered peritoneal folds, subdivides the peritoneal cavity into different compartments.[2] These peritoneal folds (known as ligaments, mesentery, or omentum) also connect the intraperitoneal organs to the abdominal wall and act as conduits for the passage of neurovascular structures from the retroperitoneum.[3] The potential space between the peritoneal folds can provide a pathway for subperitoneal spread of disease processes.[4] Slow fluid collection in the retroperitoneal, subperitoneal, or peritoneal space may be localized, but rapid accumulation of fluid, such as occurs in cases of trauma or acute pancreatitis, may overcome the natural boundaries and spill into multiple spaces.[5,6,7] The treating physicians should be familiar with the relevant radiological anatomy of these ligaments and spaces as accurate localization of fluid collection and lymph node in the peritoneal cavity, subperitoneal space, and retroperitoneum greatly aids in the selection of a treatment strategy.[8] The fat, lymph nodes, and blood vessels within ligaments act as radiological landmarks of identification for imaging by ultrasound (US), computerized tomography (CT), and magnetic resonance imaging.[9,10,11,12,13] Endoscopic US (EUS) provides an additional modality for assessment of peritoneal ligaments.[14] The transverse mesocolon, which attaches the transverse colon to the posterior wall of the abdomen, subdivides the peritoneal cavity into supracolic and infracolic compartments located above and below the transverse colon and its mesocolon. The supracolic compartment contains the liver, spleen, stomach, and lesser omentum. The infracolic compartment contains the coils of the small bowel surrounded by the ascending, transverse, and descending colon and the paracolic gutters. In this review, we describe the normal EUS anatomy of the peritoneal spaces and the recesses of the supracolic compartments of the peritoneum with supportive images by US/CT scan. Most of the images have been taken with the presence of fluid in some compartment of the abdominal cavity to facilitate clear description [Figure 1].
Figure 1.
When the intestines are removed as far posteriorly as possible, the cut edges of the peritoneum are exposed as shown in the figure. The attachments of ligaments to the retroperitoneum are shown. Arrow shows the foramen of Winslow
APPLIED EMBRYOLOGY OF THE PERITONEAL LIGAMENTS
Most peritoneal ligaments arise from the ventral or dorsal mesentery of the gut. The liver and its ligaments arise in the ventral mesentery (ventral mesogastrium), whereas the stomach, spleen, pancreatic tail, and their corresponding ligaments develop in the dorsal mesentery of the foregut (dorsal mesogastrium). The ventral part of the ventral mesentery becomes the falciform ligament, and the dorsal part of the ventral mesentery becomes the lesser omentum (hepatogastric and hepatoduodenal parts). At the level of the spleen, the ventral part of the dorsal mesentery becomes the gastrosplenic ligament, and the dorsal part of the dorsal mesentery becomes the splenorenal ligament. Above the level of the spleen, the dorsal mesentery gives rise to the gastrophrenic ligament (GPL), and below the level of the spleen, it gives rise to the gastrocolic ligament.
Applied anatomy of the liver
The ligaments of the liver
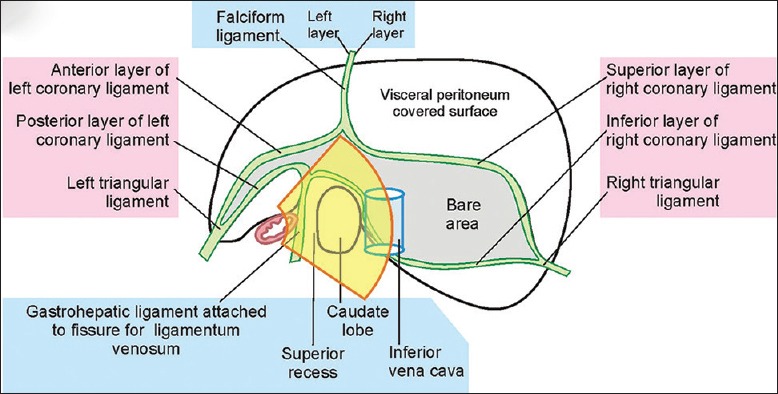
The ligaments of the liver include the suspensory ligaments of the liver (falciform) and the lesser omentum. The falciform ligament and lesser omentum contribute to the formation of the right and left coronary (crown-like) ligaments. The falciform ligament is continuous with the superior layer of the right coronary ligament to the right and with the anterior layer of the left coronary ligament to the left. The gastrohepatic ligament (GHL) (part of the lesser omentum) is continuous with the inferior layer of the right coronary ligament to the right and with the posterior layer of the left coronary ligament to the left. On both sides, the coronary ligaments continue as triangular ligaments. On the right side, the coronary ligament has superior and inferior layers (as it lies more toward the posterior surface of the liver) while on the left side, it has anterior and posterior layers (as it lies more toward the superior surface of the liver). The superior and inferior layers of the right coronary ligament are long, widely separated, and enclose the bare area of the liver. The left triangular ligament is a short ligament [Figure 2].
Figure 2.
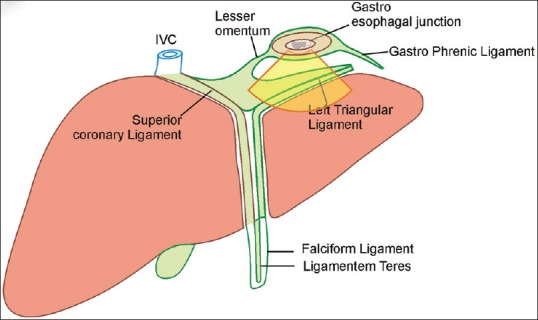
The falciform ligament is continuous with the superior layer of the right coronary ligament to the right and with the anterior layer of the left coronary ligament to the left. The gastrohepatic ligament is continuous with the inferior layer of the right coronary ligament to the right and with the posterior layer of the left coronary ligament to the left. IVC = Inferior vena cava
The perihepatic spaces
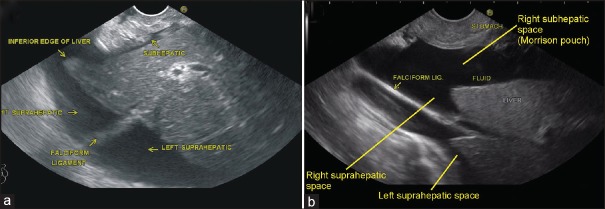
The left and right suprahepatic spaces lie between the diaphragm and the liver and are separated by the falciform ligament [Figures 3, 4 and Video 1]. The left and right infrahepatic spaces lie between the liver, the transverse colon, and the transverse mesocolon and are separated by the ligamentum teres [Figure 5]. The superior coronary ligament separates the bare area from the right suprahepatic space, and the inferior coronary ligament (hepatorenal ligament) separates the bare area from the hepatorenal recess. The inferior coronary ligament has a membranous extension, which reaches up to the inferior vena cava (IVC), and the extended ligament separates the superior recess of the lesser sac from the bare area of the liver on the right side [Figure 6]. The lateral part of the left triangular ligament separates the posterior and anterior left suprahepatic spaces.
Figure 3.
(a) In this case, the falciform ligament is attached to the parietal surface of the liver and divides the suprahepatic space into left and right areas. The right suprahepatic space communicates along the inferior edge of the liver with the right subhepatic space or Morison's pouch. (b) This patient has ascites and the falciform ligament separates the suprahepatic space into left and right areas
Figure 4.
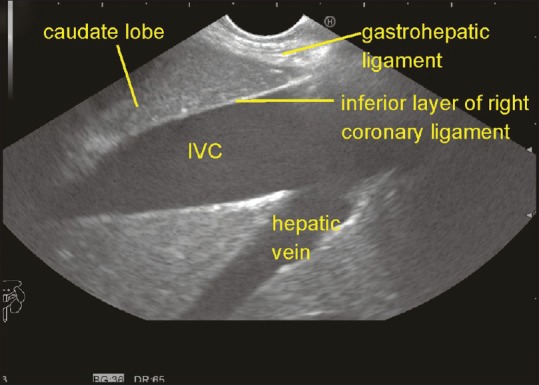
The gastrohepatic ligament is continuous with the inferior layer of the right coronary ligament to the right, which forms the base of the bare area of the liver near the left margin of the inferior vena cava. The caudate lobe is seen between the esophagus and the inferior layer of the right coronary ligament
Figure 5.
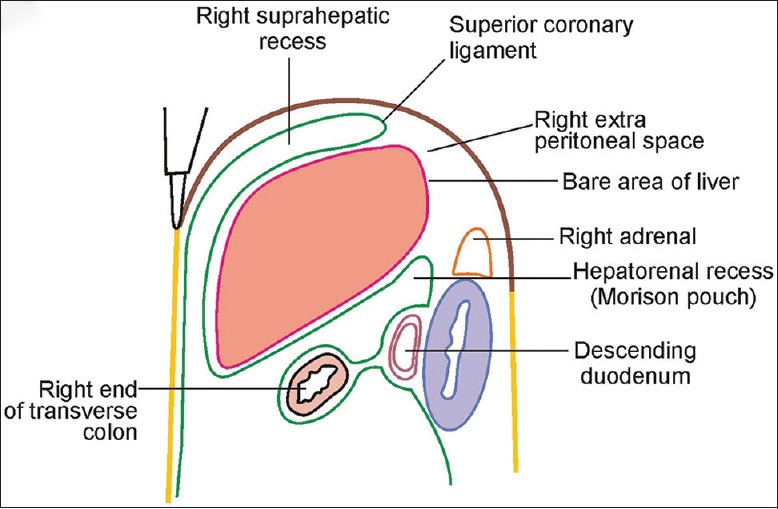
A sagittal section through the right end of the transverse colon shows the suprahepatic and subhepatic spaces on the right side. The adrenal gland is seen in the bare area of the liver
Figure 6.
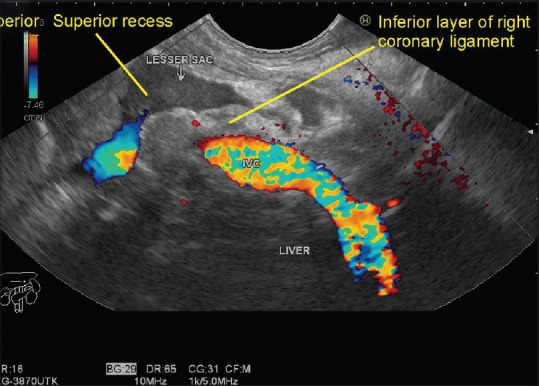
The figure shows the superior recess of the lesser sac. The inferior layer of the right coronary ligament is seen between the superior recess and the inferior vena cava
Communications
The right suprahepatic spaces communicate with the right subhepatic space around the right triangular ligament and the inferior border of the liver [Figures 3–5 and Video 2]. The hepatorenal space communicates medially with the superior recess of the lesser sac through the foramen of Winslow, is limited inferiorly by the right flexure of the colon, and has free lateral communication with the right paracolic gutter [Figures 1, 7 and 8]. The left infrahepatic space is separated from the superior recess of the lesser sac by the GHL and communicates with the left suprahepatic and perisplenic spaces.
Figure 7.

The spaces/recesses around the liver and spleen are shown. The left infrahepatic space is separated from the lesser sac by the gastrohepatic ligament. It communicates with the left suprahepatic and perisplenic recesses. The arrows denote the communication of the peritoneal spaces
Figure 8.
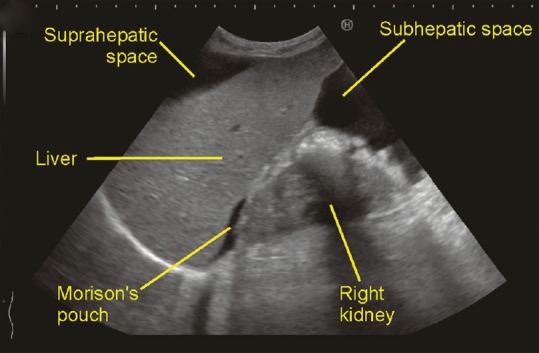
A representative image of an abdominal ultrasound is given to show the location of the suprahepatic and subhepatic spaces. The right subhepatic space between the liver and right kidney is known as Morison's pouch
Applied anatomy of the stomach
The ligaments of the stomach
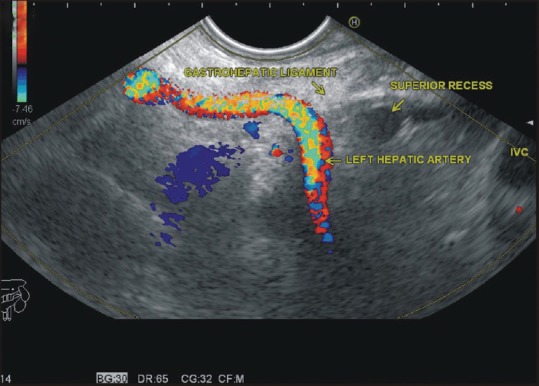
The lesser omentum contains the GHL and the hepatoduodenal ligament (HDL) and extends from the L-shaped (truly a reverse L) attachment on the visceral surface of the liver to the lesser curvature of the stomach. This L-shaped ligament has vertical and horizontal parts [Figures 9 and 10]. The GHL (pars condensa) is the vertical part, which extends from the lesser curvature into the fissure for the ligamentum venosum [Figures 11 and 12]. The superior recess of the lesser sac can extend along the ligament up to the caudate lobe of the liver [Figure 13]. The HDL (pars vasculosa) is the horizontal part, which extends from the porta hepatis to the upper border of the first part of the duodenum [Figure 9]. The three ligaments that are attached to the greater curvature are confluent but described as the gastrophrenic (above the level of spleen) [Figures 9 and 14], gastrosplenic (at the level of spleen) [Figures 9 and 15], and gastrocolic ligaments (below the level of spleen) [Figures 9 and 16]. Strictly speaking, of the three ligaments attached to the greater curvature, only the gastrocolic ligament is referred to as the greater omentum. The GPL forms the boundary of the bare area of the stomach, and the gastrosplenic ligament forms the left boundary of the splenic recess of the lesser sac. The gastrocolic ligament has two anterior layers that fold upon themselves to continue as two posterior layers extending up to the transverse colon. During fetal life, the inferior recess of the lesser sac extends in between the anterior and posterior layers of the gastrocolic ligament. However, the space is usually obliterated in adults. If the layers are not obliterated, fluid collection can occur in the inferior recess of the lesser sac between the anterior and posterior layers.
Figure 9.
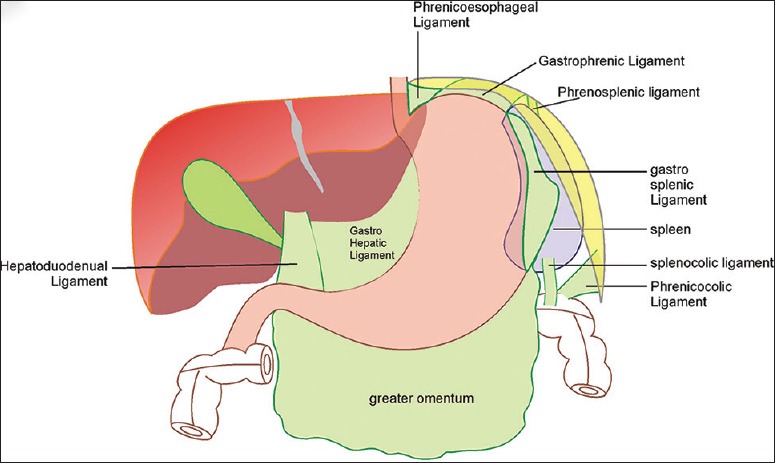
The gastrohepatic ligament is identified in the space between the liver and stomach. The hepatoduodenal ligament is identified in the space between the liver and duodenum. The three ligaments attached to the greater curvature are the gastrophrenic, gastrosplenic, and gastrocolic ligaments. The lateral part of the gastrocolic ligament is in continuity with the attachment between the spleen and colon as the splenocolic ligament. The upper part of the gastrophrenic ligament is in continuity with the attachment between the esophagus and diaphragm as the phrenic-esophageal ligament. A phrenicocolic ligament is seen between the diaphragm and splenic flexure near the lower pole of the spleen, and a phrenosplenic ligament is seen between the diaphragm and splenic flexure near the upper pole of the spleen
Figure 10.
The left gastric artery is seen between the liver and stomach in the upper part of the gastrohepatic ligament
Figure 11.

The gastrohepatic ligament is identified in the triangular space between the liver, pancreas, and stomach. This ligament reaches up to the upper border of the pancreas, and two lymph nodes are seen within the ligament. The dilated pancreatic duct is seen within the pancreas. PD: Pancreatic duct, LN: Lymph node, GHL: Gastrohepatic ligament. Arrows and the dotted black outline show the area of the gastrohepatic ligament
Figure 12.
The accessory or the aberrant, left hepatic artery reaches the liver through the gastrohepatic ligament and is seen entering the liver parenchyma through the ligamentum venosum. The superior recess of the lesser sac is seen extending cranially to the ligamentum venosum in this case. The superior recess is related to the inferior and left sides of the caudate lobe of the liver, and in this figure, it is seen between the esophagus and the caudate lobe of the liver
Figure 13.
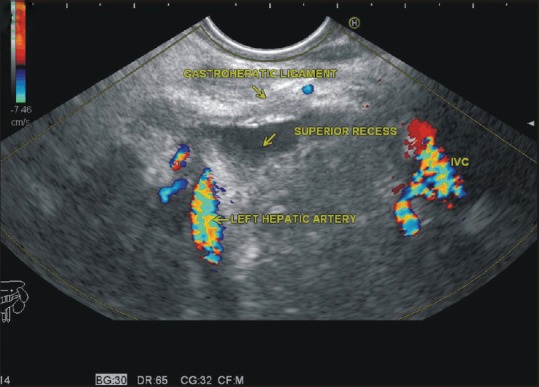
The ligamentum venosum separates the caudate lobe from segment 2 of the liver. The caudate lobe lies between certain vascular structures, namely, the inferior vena cava posteriorly, the hepatic venous confluence superiorly, and the portal triad inferiorly. It embraces the inferior vena cava in a semicircumferential fashion. The caudate lobe lies opposite the tenth and eleventh thoracic vertebrae. It is bound on the left side by the physiological division of the liver called the ligamentum venosum. It is bound below by the porta; on the right, by the fossa for the inferior vena cava; and on the left, by the fossa for the ductus venosus
Figure 14.
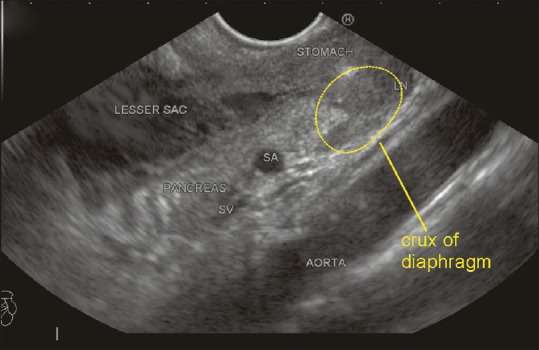
The lesser sac (superior recess) lies behind the stomach anterior to the pancreas. In this case, a lymph node is seen in the bare area of the stomach anterior to the aorta. The lymph node (dotted circle) is seen enclosed within the gastrophrenic ligament, which forms the boundaries of the bare area of the stomach. The gastrophrenic ligament separates the superior recess of the lesser sac from the crux of the diaphragm
Figure 15.
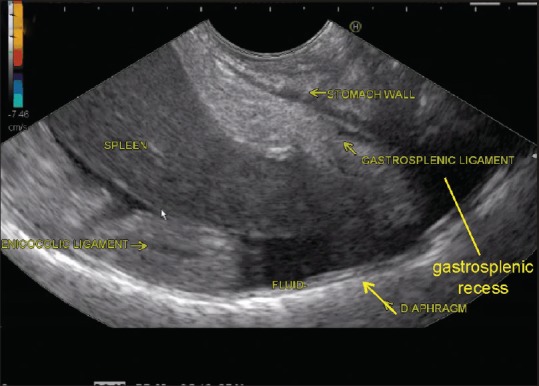
The gastrosplenic ligament is seen between the wall of the stomach and the lower pole of the spleen. The fluid above the gastrosplenic ligament in the left subphrenic space is part of the gastrosplenic recess, which is a part of the greater sac
Figure 16.
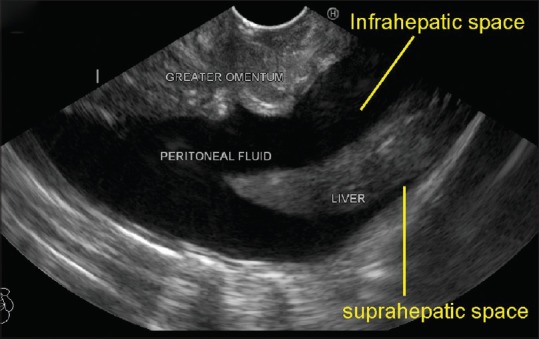
A case of metastasis is in the greater omentum and ascites. The left lobe of the liver is seen, and the infrahepatic and suprahepatic compartments are seen above and below the left lobe of the liver
The perigastric spaces
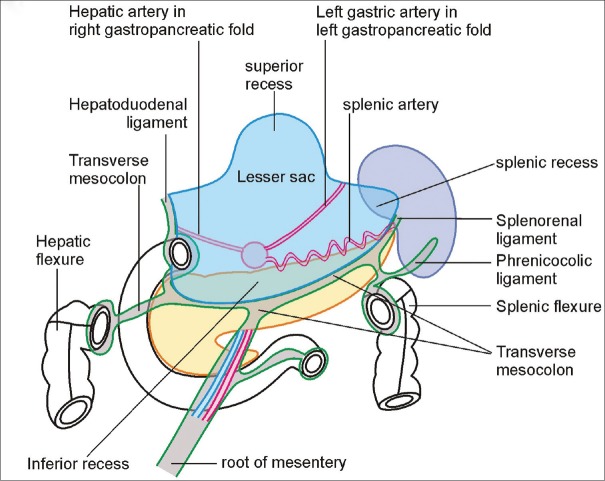
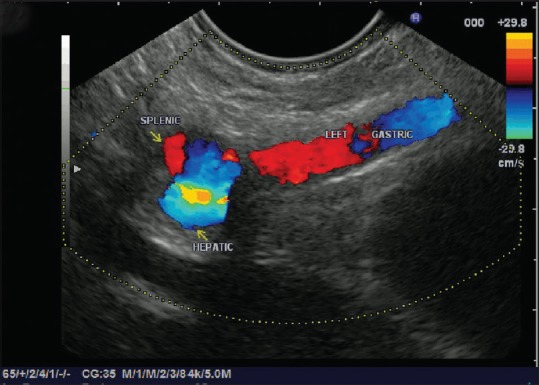
The lesser sac lies posterior to the stomach [Figure 17]. It can be subdivided into superior and inferior compartments, above and below the level of the plane of the pancreas, by the gastropancreatic folds. The left and right folds project into the lesser sac and are raised by the anterior course of the left gastric artery and the common hepatic artery, respectively [Figures 18 and 19]. The superior recess is related to the inferior and left sides of the caudate lobe of the liver [Figures 20 and 21]. The left lateral margin of the superior recess near the fundus of the stomach is related to the GPL, which is contiguous inferiorly with the gastrosplenic and splenorenal ligaments, which form the left lateral boundary of the lesser sac. The space between the anterior margin of the gastropancreatic fold and the posterior layer of the GHL is the only direct pathway between the superior and inferior compartments of the lesser sac. The superior compartment is separated from the splenic recess by the course of the left gastric artery [Figures 22–24 and Video 3]. The splenic recess, which is an extension of the inferior compartment toward the splenic hilum, extends between the gastrosplenic and splenorenal ligaments and lies anterior to the upper part of the left kidney, the left suprarenal gland, and the diaphragm [Video 4]. The inferior recess is significantly larger and mainly located to the left of the midline. It separates the stomach from the body of the pancreas. Generally, the caudal extent of the inferior recess is at the level of the transverse colon and the transverse mesocolon [Figure 25 and Video 5]. The boundaries of the inferior recess include the gastropancreatic folds superiorly and the conjunctive area of the anterior and posterior layers of the greater omentum inferiorly.
Figure 17.
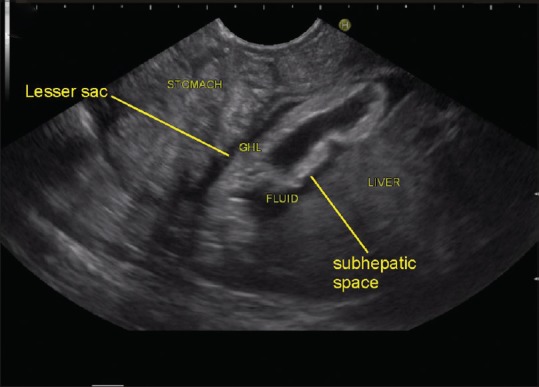
The gastrohepatic ligament is identified in the space between the liver and stomach. The fluid in the area between the stomach and the gastrohepatic ligament is present in the lesser sac, and the fluid between the gastrohepatic ligament and the liver is present in the subhepatic area
Figure 18.
A schematic diagram showing the lesser sac following the removal of the stomach and the transverse colon. The line of attachment of the transverse mesocolon and the mesentery is shown. The left gastric artery and common hepatic artery project into the lesser sac, raising the left and right gastropancreatic folds, which divide the lesser sac into the superior and inferior recesses. The splenic recess of the lesser sac is seen extending toward the splenic hilum
Figure 19.
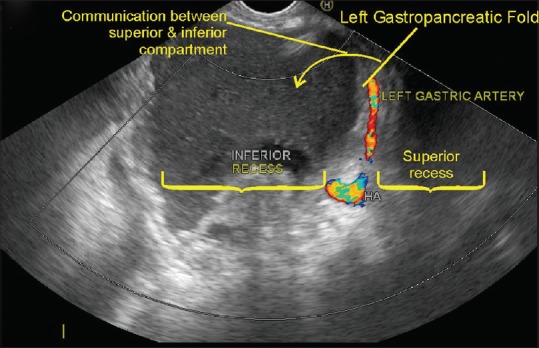
The lesser sac can be subdivided into superior and inferior compartments by the left and right gastropancreatic folds. The left gastropancreatic fold is raised by the anterior course of the left gastric artery. In this case, the communication between the superior and inferior compartments occurs anterior to the gastropancreatic fold, behind the posterior wall of the stomach
Figure 20.
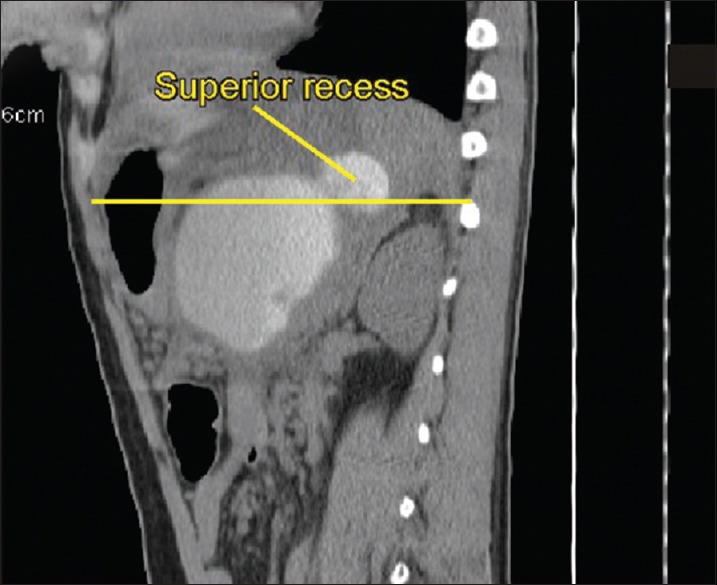
A case of pancreatic duct leak into the lesser sac. The computerized tomography scan was performed after endoscopic retrograde cholangiopancreatography. The contrast is filling the lesser sac. The yellow line demarcates an approximate area above which the superior recess is seen
Figure 21.

The superior recess is separated from the mediastinum by diaphragm and is related to the inferior and left sides of the caudate lobe of the liver. During imaging, the inferior vena cava is seen from the esophagus on the far side of the screen beyond the superior recess. The boundaries of the superior recess include the caudate lobe of the liver and diaphragm superiorly, the lesser omentum anteriorly, and the gastropancreatic folds inferiorly and to the left
Figure 22.

A case of pancreatic duct leak into the lesser sac. Computerized tomography scan was done after endoscopic retrograde cholangiopancreatography. The contrast is filling the lesser sac. The computerized tomography scan shows the splenic recess of the lesser sac
Figure 24.
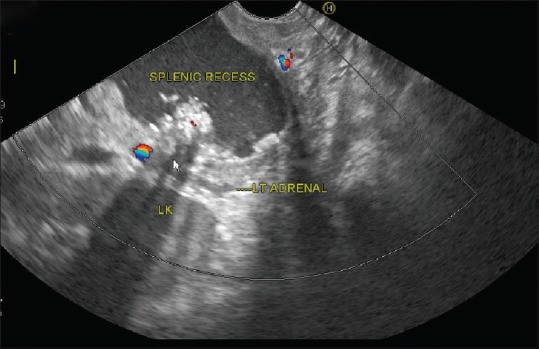
The structures lying retroperitoneally behind the splenic recess are the left suprarenal gland, the upper pole of the left kidney, and the diaphragm. The splenic artery running along the upper border of the pancreas demarcates the splenic and inferior recesses from one another
Figure 25.
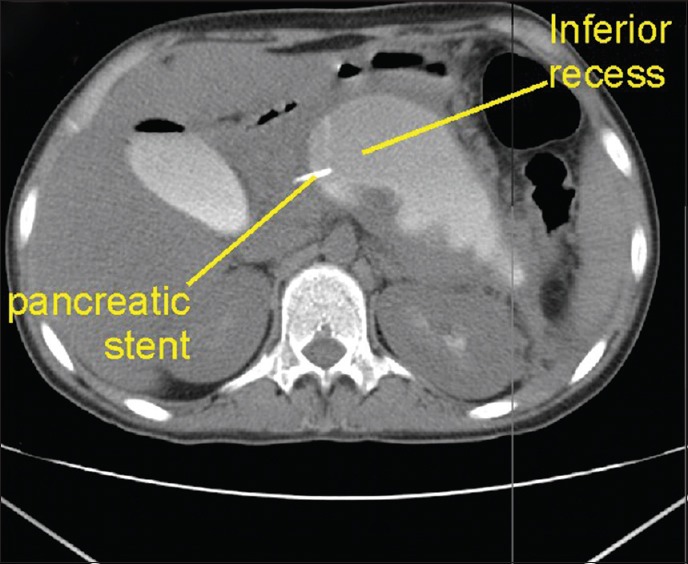
A case of a pancreatic duct leak into the lesser sac. Computerized tomography scan was performed after endoscopic retrograde cholangiopancreatography. The contrast is filling the lesser sac. This patient had pancreatic duct disruption into the lesser sac and a pancreatic duct stenting was done. The stent is seen reaching up to the inferior recess of the lesser sac, which lies anterior to the upper pole of the left kidney. The presence of contrast within the recess is also noted
Figure 23.
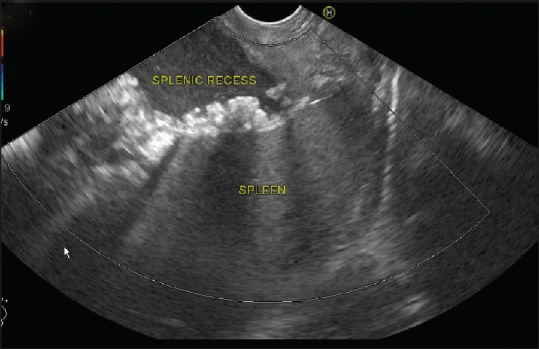
Splenic recess is the part of the inferior compartment of the lesser sac that extends to the hilum of the spleen between the gastrosplenic and splenorenal ligaments
Communications
The gastrosplenic ligament separates the greater sac from the splenic recess of the lesser peritoneal sac [Figures 26 and 27]. The ligaments of the lesser omentum (GHL and HDL) separate the superior recess of the lesser sac from the greater sac [Figures 8 and 9]. The superior recess is separated from the bare area of the liver and the IVC by a membranous continuation of the inferior coronary ligament [Figure 27]. The inferior recess on the right side communicates with the hepatorenal recess through the foramen of Winslow.
Figure 26.
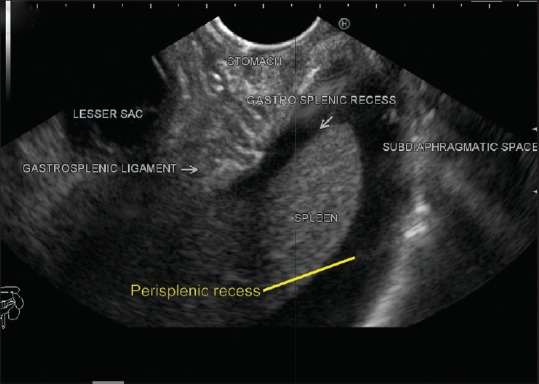
The left subdiaphragmatic recess is seen above the spleen. This recess is in continuity with the gastrosplenic recess, which is a part of greater sac
Figure 27.
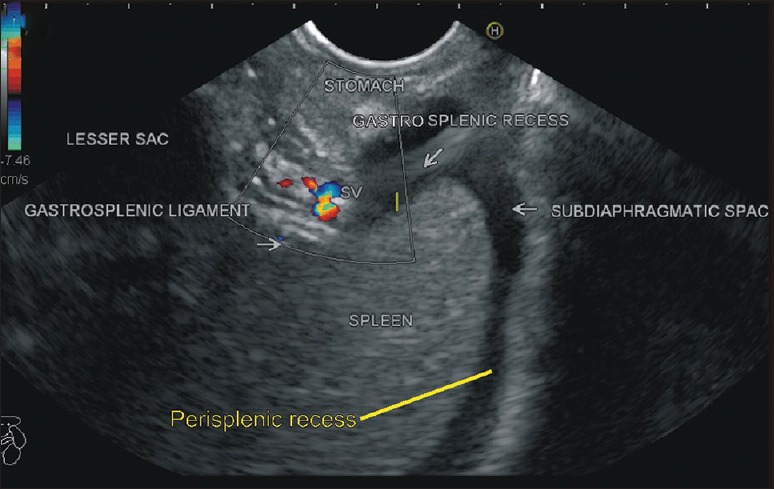
The gastrosplenic recess is separated from the splenic recess of the lesser sac by the gastrosplenic ligament. The color Doppler box is applied to the area of the gastrosplenic ligament and shows short gastric and gastroepiploic vessels, and branches of the splenic artery, which enter the gastrosplenic ligament from the splenorenal ligament
Applied anatomy of the spleen
The ligaments of the spleen
The spleen has five ligaments: one presplenic (the gastrosplenic ligament), three postsplenic (the splenorenal or lienorenal, splenocolic, and pancreaticosplenic ligaments), and one parasplenic (the phrenicosplenic ligament) [Figures 9, 28–31]. The splenocolic, pancreaticosplenic, and phrenicosplenic ligaments are less constant. When present, the phrenicosplenic ligament is identified above the upper pole of the organ, but it does not divide the peritoneal cavity on the left side into two separate subcompartments as does the falciform ligament on the right side. The phrenicocolic ligament, which is not attached to the spleen, is identified near the lower pole and creates a barrier between the perisplenic recess and the left paracolic gutter [Figures 28–30].
Figure 28.
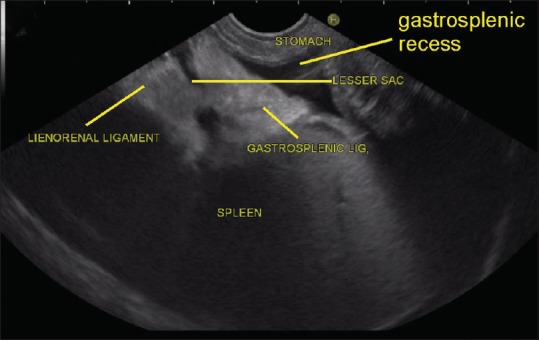
The spleen has two constant attachments: the gastrosplenic ligament and the splenorenal ligament
Figure 31.
A splenic recess derived from the lesser sac appears in relation to the hilum of spleen
Figure 30.
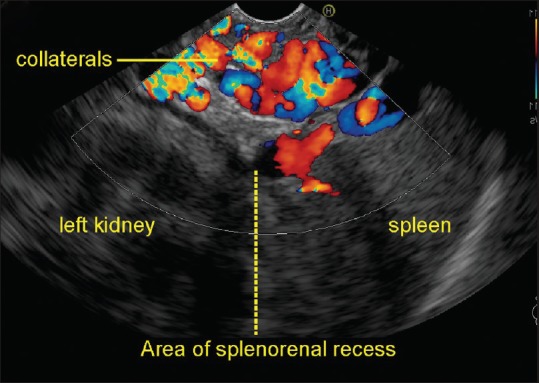
The dotted yellow line shows the area between the kidney and spleen that is analogous to Morison's pouch. The collaterals are present within the splenorenal ligament
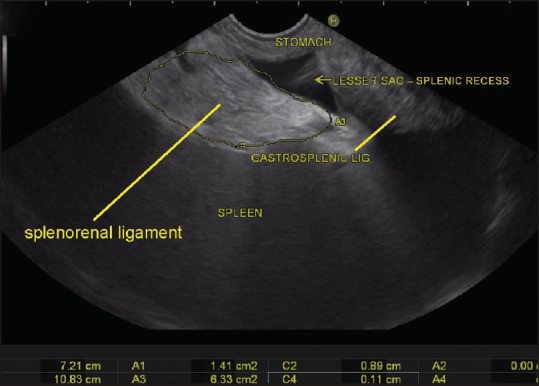
The perisplenic spaces (recesses)
The perisplenic spaces (usually described as recesses) are part of the left subphrenic space. The perisplenic recesses are located around the spleen and include three recesses related to the greater sac, namely, the gastrosplenic, splenorenal, and parasplenic recesses, and one recess related to the lesser sac, namely, the splenic recess. The gastrosplenic recess lies between the stomach and spleen [Figure 28 and Video 6]. The splenorenal recess, which is analogous to Morison's pouch, lies between the spleen and left kidney [Figure 30]. The perisplenic recess lies between the diaphragm and spleen [Figure 32]. The lower part of the perisplenic recess is sometimes defined as the splenocolic recess. All three recesses (the gastrosplenic, splenorenal, and perisplenic) arise from the embryologic left peritoneal space and are related to the greater sac. One splenic recess derived from the embryologic right peritoneal space and related to the lesser sac occurs as a fourth recess (splenic recess of the lesser sac) in relation to the spleen [Figures 28, 29 and 31].
Figure 32.
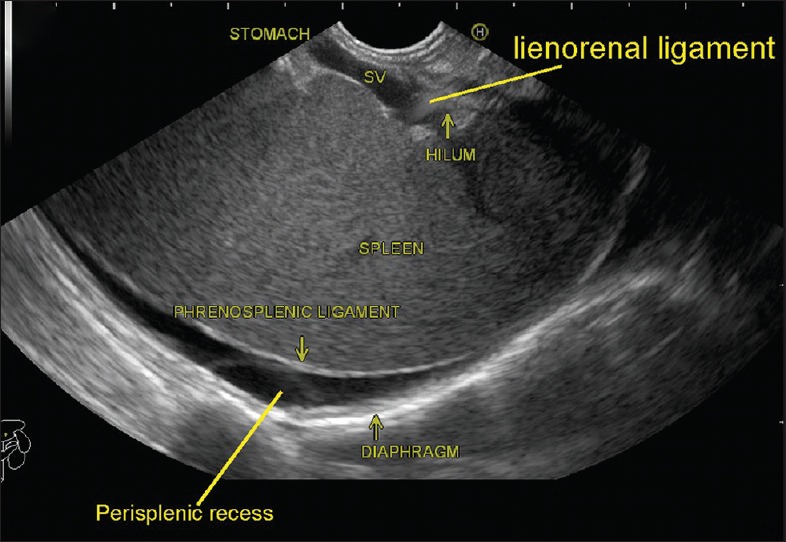
The perisplenic space is a part of the left subphrenic space and is located around the spleen. The phrenosplenic ligament is attached to the outer surface of the spleen. It is only a suspensory ligament and does not divide the perisplenic area into separate compartments. The splenic vein, splenic artery, and tail of the pancreas are enclosed within the lienorenal ligament that comes up to the hilum of the spleen
Figure 29.
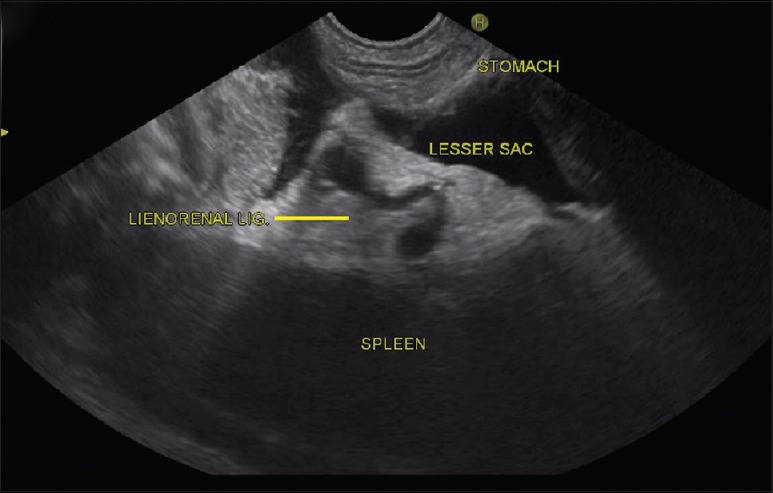
The splenic vein, splenic artery, and tail of the pancreas are enclosed within the lienorenal ligament that comes up to the hilum of the spleen. The gastrosplenic recess lies between the stomach and spleen. The splenorenal recess, which is analogous to Morison's pouch, lies between the spleen and left kidney
Communications
The perisplenic recesses (except for the splenic recess of the lesser sac) are in continuity with each other around the spleen. The gastrosplenic ligament separates the splenic recess of the lesser sac from the gastrosplenic (presplenic) recess, which is a part of the greater sac [Figure 33]. The splenorenal ligament separates the splenic recess of the lesser sac from the splenorenal recess, which is part of the greater sac [Figure 30]. The splenocolic ligament also separates the splenic recess of the lesser sac and the splenocolic recess. The phrenicocolic ligament comes close to the lower pole of the spleen and separates the greater sac from the left paracolic gutter [Figure 33].
Figure 33.
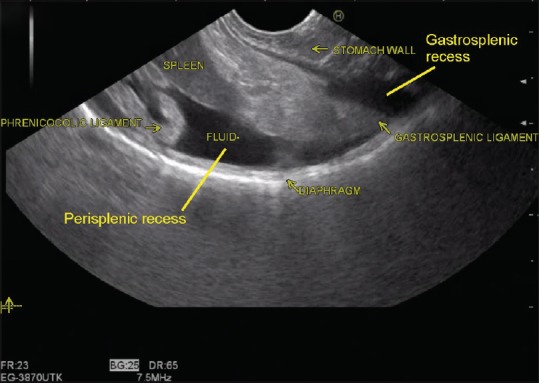
The gastrosplenic ligament is seen between the stomach and spleen. The phrenicocolic ligament is seen beyond the lower pole of the spleen and it separates the left paracolic gutter with the left subphrenic space. The phrenicocolic ligament is not attached to the spleen
The bare areas
The bare area of the liver
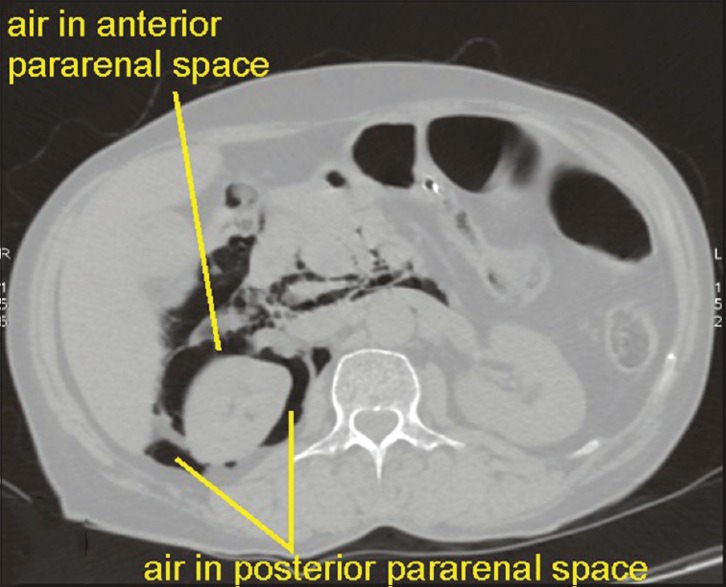
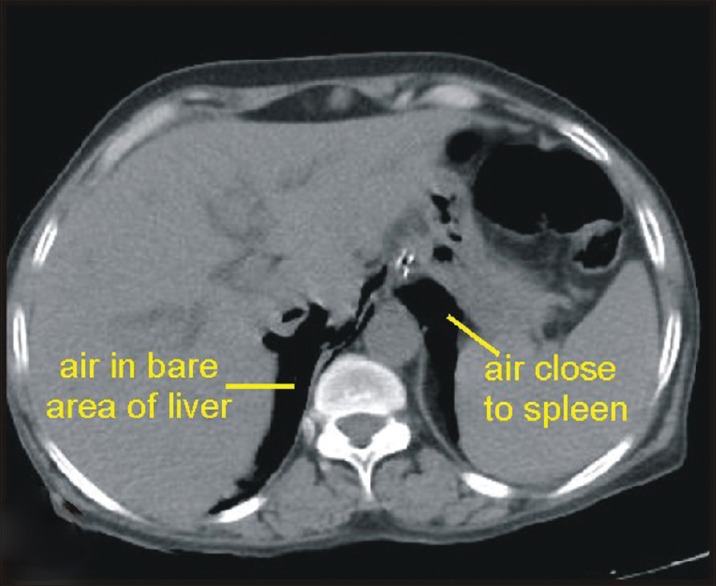
The bare area of the liver is a triangular gap located between the superior and inferior layers of the coronary ligament as well as between the anterior and posterior layers of the left triangular ligament. On the left side, the bare area is almost nonexistent. The base of this triangle lies at the IVC while the apex lies at the tip of the right triangular ligament [Figures 34 and 35]. The superior coronary ligament separates it from the right suprahepatic space and the inferior coronary ligament (hepatorenal ligament) separates it from the hepatorenal recess. A short peritoneal reflection between the IVC and the right border of the caudate lobe of the liver separates it from the superior recess of the lesser sac [Figure 36]. The right suprarenal gland is located in this area [Figure 37]. The bare area of the liver is an extraperitoneal space, which communicates with the right anterior pararenal space of the retroperitoneum, and gas and fluid collection within the perirenal space may communicate directly with the bare area of the liver [Figure 38].
Figure 34.
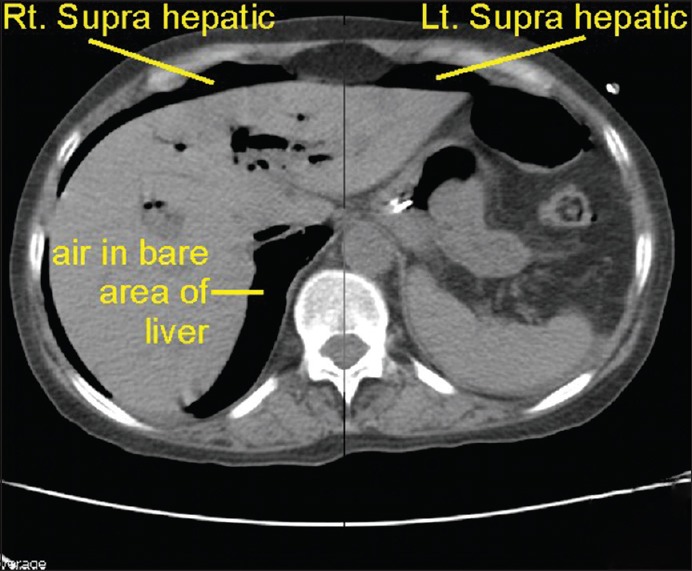
A case of retroduodenal and intraperitoneal perforation after endoscopic retrograde cholangiopancreatography. The computerized tomography scan shows air surrounding the liver in the right and left suprahepatic spaces, which are separated by the attachment of falciform ligament. The presence of air in the bare area of the liver indicates retroduodenal perforation
Figure 35.
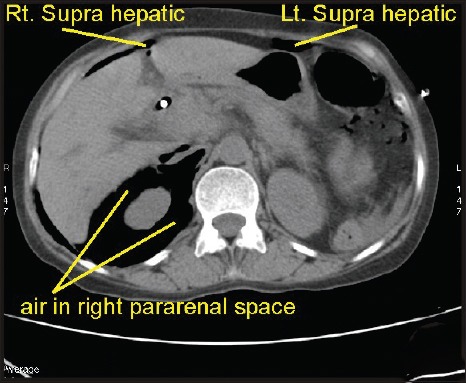
The air is seen surrounding the right kidney. The air is not crossing to the opposite side and is present only in the perirenal area. The presence of air in the right and left suprahepatic spaces is noted
Figure 36.
The beam moves from the esophagogastric junction in an open position. Initially, it shows the left lobe of the liver. On further rotation, the inferior vena cava and ligamentum venosum are seen. Further rotation in a clockwise direction shows the inferior vena cava and the inferior coronary ligament
Figure 37.
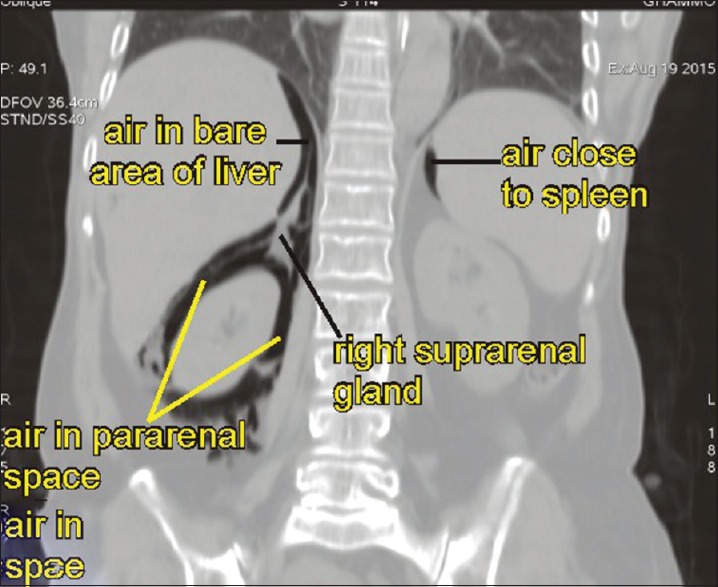
A case of retroduodenal perforation after endoscopic retrograde cholangiopancreatography. Air surrounding the kidney in the anterior and posterior pararenal spaces is noted
Figure 38.
A case of retroduodenal perforation after endoscopic retrograde cholangiopancreatography. The air is seen going up toward the bare area of the liver. A small amount of air is seen close to the spleen also
The bare area of the stomach
The bare area of the stomach is outlined by the GPL and lies on the posterior surface of the stomach. It has a triangular shape with the bottom facing upward and the tip facing downward. It is located in the upper and lower boundaries of the left and right layers of the GPL. The bare area of the stomach is continuous with the bare area of the esophagus, which lies on the posterior surface of the esophagus close to the gastroesophageal junction [Figure 39]. The phrenic-esophageal ligament, which is in continuity with the GPL, encloses the bare area of the esophagus as a fascial expansion extending in a cone-like manner from the margins of the esophageal hiatus of the diaphragm to the esophageal wall. The GPL separates the superior recess from the bare area of the stomach.
Figure 39.
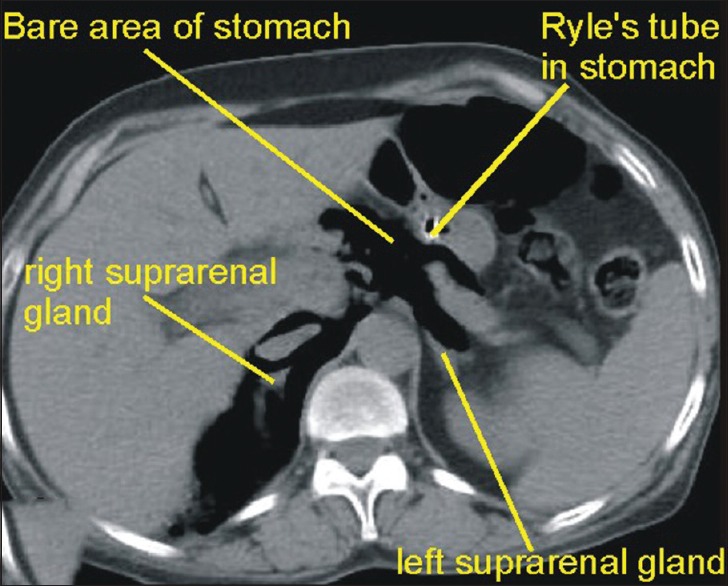
A case of retroduodenal perforation after endoscopic retrograde cholangiopancreatography. The air is seen crossing across the aorta to the opposite side. Both of the adrenal glands are seen. The right adrenal gland is seen surrounded by air on both sides, whereas the left adrenal gland has air only on the anterior surface
The bare area of the spleen
Traditionally, the spleen is considered one of the intraperitoneal viscera, but the bare areas of the spleen exist between numerous ligamentous attachments. The bare areas can be divided into the splenic hilus and the splenorenal parts. The splenorenal part is located between the renal aspect of the spleen and the splenic aspect of the left kidney. The bare area of the spleen and its permanent relationship to the upper pole of the left kidney is helpful for locating the fluid collection in the left upper quadrant on CT, specifically for differentiating between ascites and pleural fluid [Figure 40].
Figure 40.
A case of retroduodenal perforation after endoscopic retrograde cholangiopancreatography. The path of the air crossing from the right side to the left side is seen anterior to the aorta. This potential space is called Kneel and space. The right adrenal gland lies in the bare area of the liver and the left adrenal gland lies close to the bare area of the stomach. The air is seen reaching toward the medial surface of the spleen and corresponds to the area visualized in Figure 37 near the spleen. This will indicate again the bare area of the spleen
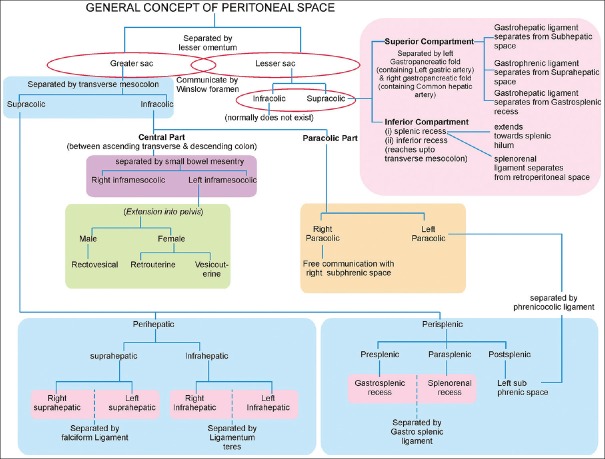
DISCUSSION
The peritoneal spaces and the separations are summarized in the form of a chart [Figure 41]. The ligaments contain fibers and depending on their thickness, they can be seen either as a hyperechoic line or as alternating stripes of hyperechoic lines. Ligaments inhibit the transmission of sound waves and are best seen when they are surrounded by ascitic fluid, i.e., ligamentum teres or parenchymal tissue on either or both sides, i.e. the GHL ligamentum venosum and ligamentum teres.[14] The identification of each ligament is done in its expected location between the organs and is facilitated by the presence of blood vessels that traverse these ligaments.[14] Metastasis within ligaments is of significant clinical importance as peritoneal surface metastases represent Stage III disease and liver metastases suggest Stage IV disease. A systematic examination of ligaments can be a useful modality for imaging and can provide valuable information to the clinician.[15] EUS of ligaments is also useful for group staging of a luminal malignancy, the sampling of station nodes, and decision-making regarding neoadjuvant therapy without laparoscopy or laparotomy.[15] It has become increasingly essential that clinicians and endosonographers thoroughly understand the peritoneal spaces and the ligaments and mesenteries that form their boundaries to localize disease to a particular peritoneal or subperitoneal space and formulate a differential diagnosis on the basis of that location.[8] In this article, we have attempted to describe the normal EUS anatomy of the peritoneal ligaments, which will enable a greater understanding of the spread of disease processes.
Figure 41.
This figure shows the arrangement of the falciform, coronary, triangular, and gastrohepatic ligaments. From the esophagus, the ligamentum venosum, superior recess (if filled with fluid), caudate lobe, and inferior vena cava can be seen in a single plane. The movement of the beam in clockwise and counterclockwise rotation will demonstrate rest of the ligaments
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos Available on: www.eusjournal.com
REFERENCES
- 1.Healy JC, Reznek RH. The peritoneum, mesenteries and omenta: Normal anatomy and pathological processes. Eur Radiol. 1998;8:886–900. doi: 10.1007/s003300050485. [DOI] [PubMed] [Google Scholar]
- 2.Le O. Patterns of peritoneal spread of tumor in the abdomen and pelvis. World J Radiol. 2013;5:106–12. doi: 10.4329/wjr.v5.i3.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yoo E, Kim JH, Kim MJ, et al. Greater and lesser omenta: Normal anatomy and pathologic processes. Radiographics. 2007;27:707–20. doi: 10.1148/rg.273065085. [DOI] [PubMed] [Google Scholar]
- 4.Vikram R, Balachandran A, Bhosale PR, et al. Pancreas: Peritoneal reflections, ligamentous connections, and pathways of disease spread. Radiographics. 2009;29:e34. doi: 10.1148/rg.e34. [DOI] [PubMed] [Google Scholar]
- 5.Coffin A, Boulay-Coletta I, Sebbag-Sfez D, et al. Radioanatomy of the retroperitoneal space. Diagn Interv Imaging. 2015;96:171–86. doi: 10.1016/j.diii.2014.06.015. [DOI] [PubMed] [Google Scholar]
- 6.Mirilas P, Skandalakis JE. Surgical anatomy of the retroperitoneal spaces part II: The architecture of the retroperitoneal space. Am Surg. 2010;76:33–42. [PubMed] [Google Scholar]
- 7.Lee SL, Ku YM, Rha SE. Comprehensive reviews of the interfascial plane of the retroperitoneum: Normal anatomy and pathologic entities. Emerg Radiol. 2010;17:3–11. doi: 10.1007/s10140-009-0809-7. [DOI] [PubMed] [Google Scholar]
- 8.Tirkes T, Sandrasegaran K, Patel AA, et al. Peritoneal and retroperitoneal anatomy and its relevance for cross-sectional imaging. Radiographics. 2012;32:437–51. doi: 10.1148/rg.322115032. [DOI] [PubMed] [Google Scholar]
- 9.Kim S, Kim TU, Lee JW, et al. The perihepatic space: Comprehensive anatomy and CT features of pathologic conditions. Radiographics. 2007;27:129–43. doi: 10.1148/rg.271065050. [DOI] [PubMed] [Google Scholar]
- 10.Auh YH, Lim JH, Kim KW, et al. Loculated fluid collections in hepatic fissures and recesses: CT appearance and potential pitfalls. Radiographics. 1994;14:529–40. doi: 10.1148/radiographics.14.3.8066268. [DOI] [PubMed] [Google Scholar]
- 11.Desai G, Filly RA. Sonographic anatomy of the gastrohepatic ligament. J Ultrasound Med. 2010;29:87–93. doi: 10.7863/jum.2010.29.1.87. [DOI] [PubMed] [Google Scholar]
- 12.Wigham A, Alexander Grant L. Preoperative hepatobiliary imaging: What does the radiologist need to know? Semin Ultrasound CT MR. 2013;34:2–17. doi: 10.1053/j.sult.2012.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Jeon YS, Lee JW, Cho SG. Is it from the mesentery or the omentum? MDCT features of various pathologic conditions in intraperitoneal fat planes. Surg Radiol Anat. 2009;31:3–11. doi: 10.1007/s00276-008-0381-y. [DOI] [PubMed] [Google Scholar]
- 14.Sharma M, Rai P, Rameshbabu CS, et al. Imaging of peritoneal ligaments by endoscopic ultrasound (with videos) Endosc Ultrasound. 2015;4:15–27. doi: 10.4103/2303-9027.151317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma M, Rai P, Rameshbabu CS. Techniques of imaging of nodal stations of gastric cancer by endoscopic ultrasound. Endosc Ultrasound. 2014;3:179–90. doi: 10.4103/2303-9027.138793. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.