Abstract
Patient: Male, 51
Final Diagnosis: ST-segment elevation myocardial infarction with acute stent thrombosis
Symptoms: Chest pain • hiccups
Medication: —
Clinical Procedure: —
Specialty: Cardiology
Objective:
Unusual clinical course
Background:
Acute coronary syndrome (ACS) can present with atypical chest pain or symptoms not attributed to heart disease, such as indigestion. Hiccups, a benign and self-limited condition, can become persistent or intractable with overlooked underlying etiology. There are various causes of protracted hiccups, including metabolic abnormalities, psychogenic disorders, malignancy, central nervous system pathology, medications, pulmonary disorders, or gastrointestinal etiologies. It is rarely attributed to cardiac disease.
Case Report:
We report a case of intractable hiccups in a 51-year-old male with cocaine related myocardial infarction (MI) before and after stent placement. Coronary angiogram showed in-stent thrombosis of the initial intervention. Following thrombectomy, balloon angioplasty, and stent, the patient recovered well without additional episodes of hiccups. Although hiccups are not known to present with a predilection for a particular cause of myocardial ischemia, this case may additionally be explained by the sympathomimetic effects of cocaine, which lead to vasoconstriction of coronary arteries.
Conclusions:
Hiccups associated with cardiac enzyme elevation and EKG ST-segment elevation before and after percutaneous coronary intervention (PCI) maybe a manifestation of acute MI with or without stent. The fact that this patient was a cocaine user may have contributed to the unique presentation.
MeSH Keywords: Cocaine, Coronary Thrombosis, Hiccup, Myocardial Infarction, Percutaneous Coronary Intervention
Background
Hiccups are an infrequently cited symptom of acute myocardial infarction (MI) [1,2]. This unusual presentation appears to be of importance in individuals prone to atypical presentation such as those with diabetes, as well as in females and the elderly [3]. Previous studies have suggested that irritation of the vagus nerve is responsible for this phenomenon [2,4]. Although the occurrence of in-stent thrombosis is rare, risks for platelet activation and thrombus formation can complicate the care of patients after percutaneous coronary intervention (PCI) [5–9]. Cocaine poses a significant risk of acute coronary syndrome (ACS) by enhancing platelet aggregation, forming thrombi, and vasoconstriction. Here we report a case of hiccups in a patient with cocaine associated MI before and after PCI.
Case Report
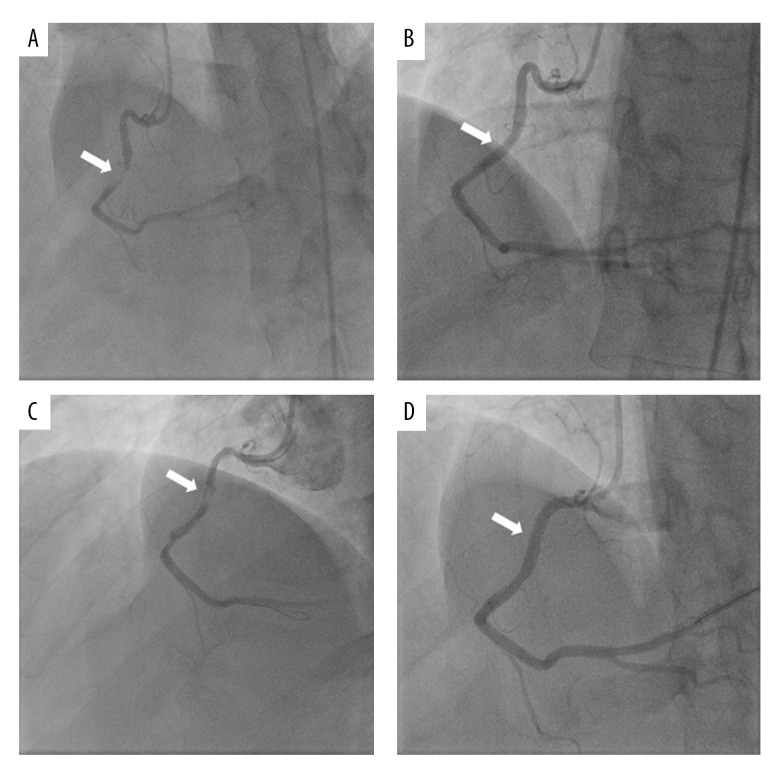
A 51-year-old African American male presented with sudden onset severe non-radiating left sided chest pain, accompanied by nausea, diaphoresis, and two episodes of non-bilious vomiting that partially relieved his pain. His past medical history included hypertension, diabetes mellitus, asthma, and gastritis. The patient additionally admitted to regular use of marijuana, but denied use of cigarettes or other illicit drugs. However, his urine drug screen was positive for cocaine, cannabinoids, and benzodiazepines. The patient was hemodynamically stable and physical examination was unremarkable. A 12-lead electrocardiogram (ECG) revealed ST-segment elevations in the inferior leads (Figure 1). The patient received emergent cardiac catheterization which revealed 99% stenosis of the mid right coronary artery (RCA) with thrombolysis in myocardial infarction (TIMI) grade II flow through the vessel, and 80% stenosis of the left anterior descending artery with TIMI III grade flow (Figure 2). A successful balloon angioplasty with stent was performed on the lesion in the mid RCA. Following intervention, there was no residual stenosis on angiography with TIMI III flow.
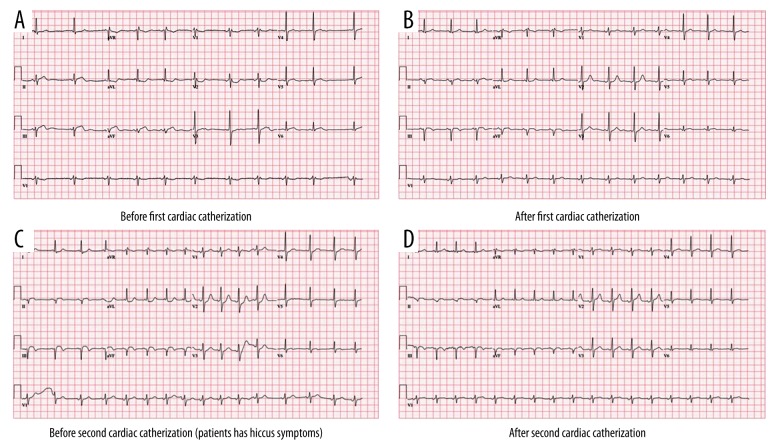
Figure 1.
EKG (A) On admission: sinus rhythm with short PR with marked sinus arrhythmia with blocked PACs. Incomplete right bundle branch block. ST elevation in infero-lateral leads. (B) After first PCI: left anterior fascicular block, T wave abnormality. (C) ECG on the second day (patient developed hiccup): left axis deviation with acute inferior infarct. (D) After second PCI: sinus tachycardia, left axis deviation.
Figure 2.
(A) First coronary angiography: severe stenosis of mid RCA (arrow). (B) Post successful PCI of the RCA with a drug-eluting stent (arrow). (C) Thrombosis formation in mid RCA’s stent (arrow). (D) Post intervention angiogram showing successful PCI of the RCA with a new drug-eluting stent (arrow).
Troponin I peaked at 95.8 ng/mL. The following morning, after PCI, the patient’s troponin I dropped to 16.9 ng/mL and his ECG showed resolved ST elevations. Overnight between hospital day 2 and 3, the patient experienced intractable hiccups and fever without chest pain but with new ST-segment elevation in the inferior leads. Troponin peaked at 80.3 ng/mL (Figure 3). A repeat coronary angiography revealed 100% stenosis of the proximal margin of the stented segment of RCA. A successful balloon angioplasty with thrombectomy and new stent placement were performed. A 50% stenosis was noted in the mid RCA, and an additional balloon angioplasty with stent was placed to restore flow TIMI III through the vessels. There was a concern for clopidogrel resistance, so clopidogrel was switched to prasugrel. Later laboratory tests for the GYP2C19 genotype revealed the patient was negative for clopidogrel resistance.
Figure 3.
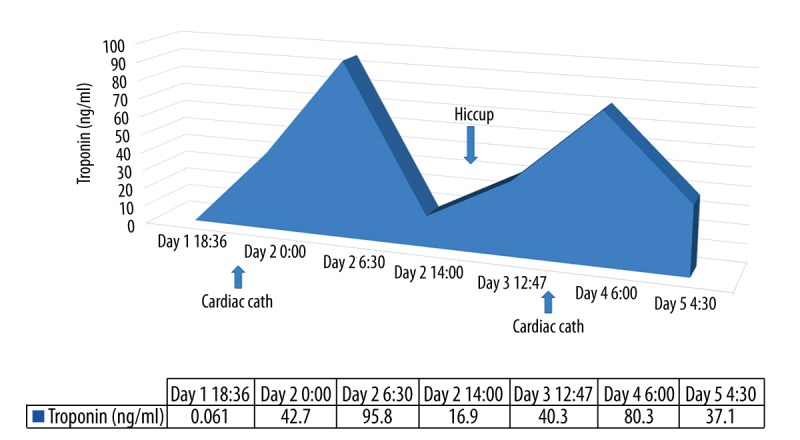
Troponin Level related to rethrombosis MI and hiccup.
Echocardiography revealed features consistent with a pseudo-normal left ventricular filling pattern, with concomitant abnormal relaxation and increased filling pressure (grade 2 diastolic dysfunction). The patient presented no further complications and was discharged home after five days of hospitalization.
Discussion
Persistent hiccups as the sole presenting symptom of myocardial infarction (MI) has previously been rarely reported [1,2]. Unusual presentations are especially important in individuals predisposed to atypical presentation of MI [3]. The pathophysiology of hiccups is mainly neurogenic (with neuro center located in the medulla) and possibly related to the irritation of the vagus or phrenic nerves [4]. It is believed that vagal nerve irritation is responsible for the presentation of hiccups in MI, as it provides parasympathetic innervation to the heart and carries afferent nerve fibers of the hiccup reflex [2,4]. In this patient, non-retractable hiccups associated with new onset ST-segment elevation in the same ECG leads as his initial presentation of ACS and significant elevated troponin prompted a repeat coronary angiography which confirmed involvement of the same artery due to in-stent thrombosis.
Studies have shown that hiccups occurred more frequently in patient with inferior MI and right ventricle infarction. This may be explained by the phrenic nerve forming anastomoses with the major part of the fibers reaching the pericardium from the right side [10]. In one case report, both the RCA and left anterior descending artery (LAD) had been significantly obstructed, but the symptom of hiccups was observed to dissipate after the opening of RCA even though LAD remained obstructed [2]. Our patient’s MI and restenosis occurred in the mid right coronary artery, which further confirmed the preference for right sided coronary vasculature when hiccup is a presenting symptom.
In-stent thrombosis is a rare event that occurs in 0.5% to 1% of patients within one-year of PCI [5]. The rates of thrombosis are comparable between drug eluding stents and bare metal stents [11]. Risk factors for stent thrombosis include, but are not limited to, absence of platelet P2Y12 receptor blocker therapy, presence of GYP2C19 genotype associated with lower efficacy for clopidogrel, premature discontinuation of dual anti-platelet therapy, involvement of the proximal left anterior descending coronary artery, multi-vessel disease, diabetes mellitus, end stage renal disease, malignancy, left ventricular dysfunction, and cocaine use [6,12,13]. In our case, the patient had three important risk factors, including diabetes mellitus, cocaine use, and multi-vessel disease, placing him at a higher risk for stent thrombosis.
Although screening for urine toxicology is not a routine protocol for ACS, it was done for this patient due to his history of regular use of marijuana and the high prevalence of drug use in the local population. The positive result suggested cocaine use within the last 80 hours, which can vary depending on the method used to intake cocaine, the dosage, as well as the use of ethanol which prolongs the clearance [14].
The effects of cocaine on vasoconstriction and enhanced platelet aggregation and thrombus formation have been reported [7,15]. Cocaine is responsible for thrombus formation by causing platelet activation, α granule release, potentiation of thromboxane, and platelet containing micro-aggregate formation [8,9]. Furthermore, cocaine has sympathomimetic activity, which can lead to ischemic events by increasing myocardial demand for oxygen and promoting coronary vasospasm [16]. Retrospective studies have shown that the rate of in-stent thrombosis post-PCI in cocaine users ranges from 5% to 33%, conferring a 10- to 60-fold increase over the general population [7,15]. Previous studies on the temporal relationship between active cocaine abuse and in-stent thrombosis revealed a large time range from 11 days to 91 days post-PCI. One study showed a mean period of 51 days ±40 days (median of 45 days) [15] and another study showed a mean period of 28.5 days ±14 days [7]. Additional data regarding the onset timeframe between the cocaine use and the initial ACS varied from one minute to four days after cocaine use with about two-thirds of infarctions occurring within three hours and one-fourth occurring within one hour [3,4]. Our patient developed in-stent thrombosis within one day post-PCI.
Patients with in-stent thrombosis present with similar symptoms to ACS. Without diagnostic and therapeutic PCI, it is not possible to differentiate between the two [17]. In-stent thrombosis is classified as early (less than 30 days), late (between 31 days and one year), and very late (beyond one year) based on the stent placement. Most incidences of in-stent thrombosis occur in the early stages, and become less likely as time proceeds owing to the effective epithelialization of the stent [18]. In-stent thrombosis should always be part of the differential diagnosis in patients presenting with ACS after PCI, especially within the last year. Management of in-stent thrombosis is similar to that of ACS, but with an even more urgent need for PCI for two reasons: first, time to re-perfusion becomes more critical in these patients as they have poorer outcomes with longer waiting time versus those with de novo coronary thrombosis. Second, there is a higher likelihood of reperfusion failure [19]. Another important factor in management is dual anti-platelet therapy and use of alternative agents in patients with clopidogrel resistance [5].
Clopidogrel resistance is especially important as it predicts high mortality and significantly increases chances of in-stent thrombosis, underlining the benefit of testing patients for GYP2C19 genotype at the cardiac catheterization lab [20]. However, platelet reactivity despite treatment is dependent on the cutoff value used for the GYP2C19 assay. A higher cut-off value will capture fewer positive results. Additionally, the variability in response to clopidogrel is multifactorial. Under dosing, drug-drug interactions, and upregulation of other platelet activating pathways may also be responsible for failure of treatment response [21]. The patient in our case experienced early in-stent re-thrombosis the day after undergoing initial PCI despite adequate anti-platelet coverage and despite not having GYP2C19 genotype associated lower efficacy for clopidogrel.
Conclusions
In summary, we report a rare case of hiccups as manifestation of acute ST-elevation myocardial infarction (STEMI) and early in-stent re-stenosis after PCI. Acute in-stent re-thrombosis should be closely monitored in patients with recent PCI, especially cocaine users, even in patients without the GYP2C19 genotype. Physicians should be alert to the possibility of an atypical presentation and unusual symptomatology in patients with risk factors for coronary artery disease.
Acknowledgments
The authors would like to thank all medical staffs who treated the patient and provided supports.
Footnotes
Conflict of interest
None.
References:
- 1.Davenport J, Duong M, Lanoix R. Hiccups as the only symptom of non-ST-segment elevation myocardial infarction. Am J Emerg Med. 2012;30(1):266e1–2. doi: 10.1016/j.ajem.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 2.Krysiak W, Szabowski S, Stepień M, et al. Hiccups as a myocardial ischemia symptom. Pol Arch Med Wewn. 2008;118(3):148–51. [PubMed] [Google Scholar]
- 3.Swap CJ, Nagurney JT. Value and limitations of chest pain history in the evaluation of patients with suspected acute coronary syndromes. JAMA. 2005;294(20):2623–29. doi: 10.1001/jama.294.20.2623. [DOI] [PubMed] [Google Scholar]
- 4.Howes D. Hiccups: A new explanation for the mysterious reflex. Bioessays. 2012;34(6):451–53. doi: 10.1002/bies.201100194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sommer P, Armstrong EJ. Stent thrombosis: Current management and outcomes. Curr Treat Options Cardiovasc Med. 2015;17(3):365. doi: 10.1007/s11936-015-0365-2. [DOI] [PubMed] [Google Scholar]
- 6.Ibrahim M, Hasan R, Awan M. Cocaine-induced coronary stent thrombosis. Exp Clin Cardiol. 2013;18(1):e57–59. [PMC free article] [PubMed] [Google Scholar]
- 7.Singh S, Arora R, Khraisat A, et al. Increased incidence of in-stent thrombosis related to cocaine use: Case series and review of literature. J Cardiovasc Pharmacol Ther. 2007;12(4):298–303. doi: 10.1177/1074248407306671. [DOI] [PubMed] [Google Scholar]
- 8.Kugelmass AD, Oda A, Monahan K, et al. Activation of human platelets by cocaine. Circulation. 1993;88(3):876–83. doi: 10.1161/01.cir.88.3.876. [DOI] [PubMed] [Google Scholar]
- 9.Togna G, Tempesta E, Togna AR, et al. Platelet responsiveness and biosynthesis of thromboxane and prostacyclin in response to in vitro cocaine treatment. Haemostasis. 1985;15(2):100–7. doi: 10.1159/000215129. [DOI] [PubMed] [Google Scholar]
- 10.Sinha N, Ahuja RC, Saran RK, Jain GC. Clinical correlates of acute right ventricular infarction in acute inferior myocardial infarction. Int J Cardiol. 1989;24(1):55–61. doi: 10.1016/0167-5273(89)90041-7. [DOI] [PubMed] [Google Scholar]
- 11.Spaulding C, Daemen J, Boersma E, et al. A pooled analysis of data comparing sirolimus-eluting stents with bare-metal stents. N Engl J Med. 2007;356(10):989–97. doi: 10.1056/NEJMoa066633. [DOI] [PubMed] [Google Scholar]
- 12.van Werkum JW, Heestermans AA, Zomer AC, et al. Predictors of coronary stent thrombosis: the Dutch Stent Thrombosis Registry. J Am Coll Cardiol. 2009;53(16):1399–409. doi: 10.1016/j.jacc.2008.12.055. [DOI] [PubMed] [Google Scholar]
- 13.Wenaweser P, Daemen J, Zwahlen M, et al. Incidence and correlates of drug-eluting stent thrombosis in routine clinical practice. 4-year results from a large 2-institutional cohort study. J Am Coll Cardiol. 2008;52(14):1134–40. doi: 10.1016/j.jacc.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 14.Huestis MA, Darwin WD, Shimomura E, et al. Cocaine and metabolites urinary excretion after controlled smoked administration. J Anal Toxicol. 2007;31(8):462–68. doi: 10.1093/jat/31.8.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Karlsson G, Rehman J, Kalaria V, Breall JA. Increased incidence of stent thrombosis in patients with cocaine use. Catheter Cardiovasc Interv. 2007;69(7):955–58. doi: 10.1002/ccd.21151. [DOI] [PubMed] [Google Scholar]
- 16.Lange RA, Cigarroa RG, Yancy CW, Jr, et al. Cocaine-induced coronary-artery vasoconstriction. N Engl J Med. 1989;321(23):1557–62. doi: 10.1056/NEJM198912073212301. [DOI] [PubMed] [Google Scholar]
- 17.Holmes DR, Jr, Kereiakes DJ, Garg S, et al. Stent thrombosis. J Am Coll Cardiol. 2010;56(17):1357–65. doi: 10.1016/j.jacc.2010.07.016. [DOI] [PubMed] [Google Scholar]
- 18.Palmerini T, Kirtane AJ, Serruys PW, et al. Stent thrombosis with everolimus-eluting stents: Meta-analysis of comparative randomized controlled trials. Circ Cardiovasc Interv. 2012;5(3):357–64. doi: 10.1161/CIRCINTERVENTIONS.111.967083. [DOI] [PubMed] [Google Scholar]
- 19.Chechi T, Vecchio S, Vittori G, et al. ST-segment elevation myocardial infarction due to early and late stent thrombosis a new group of high-risk patients. J Am Coll Cardiol. 2008;51(25):2396–402. doi: 10.1016/j.jacc.2008.01.070. [DOI] [PubMed] [Google Scholar]
- 20.Sibbing D, Braun S, Morath T, et al. Platelet reactivity after clopidogrel treatment assessed with point-of-care analysis and early drug-eluting stent thrombosis. J Am Coll Cardiol. 2009;53(10):849–56. doi: 10.1016/j.jacc.2008.11.030. [DOI] [PubMed] [Google Scholar]
- 21.Tantry US1, Gesheff M, Liu F, et al. Resistance to antiplatelet drugs: What progress has been made? Expert Opin Pharmacother. 2014;15(17):2553–64. doi: 10.1517/14656566.2014.968126. [DOI] [PubMed] [Google Scholar]