Introduction
KEY TEACHING POINTS
|
Atrial flutter is an uncommonly diagnosed arrhythmia in the neonatal period. The majority of cases can be successfully converted to sinus rhythm by electrical cardioversion or atrial overdrive pacing. Sinus rhythm usually is maintained without the need for ongoing arrhythmic medication.1 Ablation of atrial flutter in neonates for arrhythmia control has yet to be reported.
Case report
The patient was a male infant born at 38 weeks’ gestation. Atrial flutter was diagnosed in utero at 35 weeks of gestation, at which time no hydrops fetalis was present and no treatment was commenced. At 6 hours of life, the infant developed tachycardia. The electrocardiogram (ECG) showed atrial flutter with 2:1 atrioventricular conduction (Figure 1). Initially the rhythm could be reverted to sinus by biphasic direct current (DC) cardioversion. However, atrial flutter recurred despite intravenous amiodarone infusion. The infant developed heart failure on day 3 of life. An echocardiogram demonstrated a structurally normal heart with significant biatrial dilation and moderately impaired biventricular function. No intracardiac thrombus was evident. Transesophageal overdrive pacing was attempted but failed. DC cardioversion (at 1 J/kg) could revert the rhythm to sinus, but atrial flutter recurred within 12 hours. In total, DC cardioversion was attempted 6 times with varying combinations of intravenous amiodarone (15 μg/kg/min), intravenous esmolol (up to 175 μg/kg/min), oral digoxin (8 μg/kg/day), sotalol (4.5 mg/kg/day), and flecainide (4 mg/kg/day), but none of them could maintain the rhythm in sinus, and atrial flutter recurred within 12 hours. In view of the persistent ventricular dysfunction with biatrial dilation, electrophysiologic study with potential radiofrequency ablation of the atrial flutter was performed on day 14 of life.
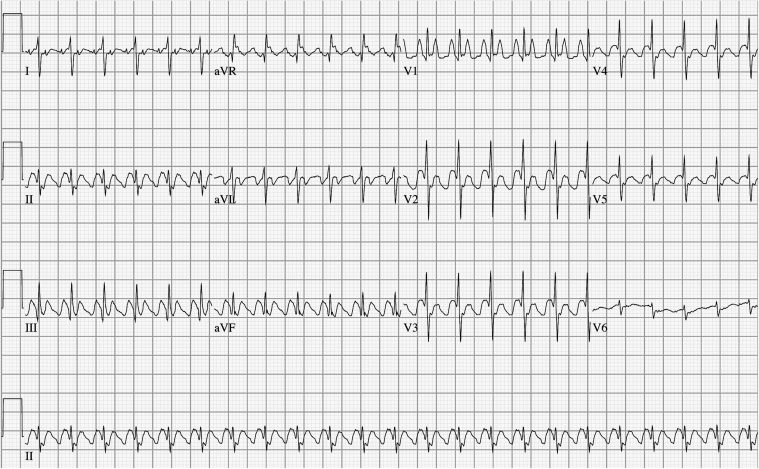
Figure 1.
Electrocardiogram showing atrial flutter with atrioventricular 2:1 block and ventricular rate of 170 bpm.
A 6Fr transesophageal electrode was placed to record left atrial activation and allow pacing. A 5Fr TherapyTM ablation catheter (St. Jude, Saint Paul, MN) (nonirrigated 4-mm tip) was placed via right femoral venous access for mapping in the right atrium. The EnSiteTM 3-dimensional cardiac mapping system (St. Jude, Saint Paul, MN) was used for electroanatomic mapping. Activation sequence confirmed a typical counterclockwise macroreentrant atrial flutter (Figure 2). Entrainment pacing confirmed the cavotricuspid isthmus was in the primary tachycardia circuit. Linear lesions were created using the point-to-point technique through radiofrequency with gradual withdrawal of the catheter from the tricuspid ring to the inferior vena cava. Four applications (mean energy delivery of 8 W, mean temperature 58°C) were given before atrial flutter was terminated (Figure 3). Further ablation was performed to complete the ablation line along the cavotricuspid isthmus. Total ablation time was 3 minutes 49 seconds. Double potentials and unidirectional block along the ablation line were demonstrated (Figure 4).
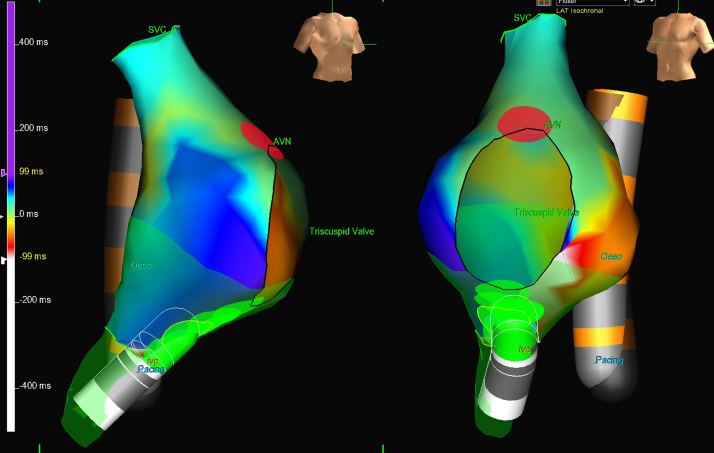
Figure 2.
Three-dimensional electroanatomic mapping of the right atrium in the right anterior oblique (left) and left anterior oblique (right) views showing counterclockwise macroreentry around the cavotricuspid isthmus. Light green spots show the ablation line created over the isthmus. The transesophageal electrode (Oeso) is depicted as the orange catheter. The ablation electrode is depicted as the white catheter. AVN = atrioventricular node; IVC = inferior vena cava; SVC = superior vena cava.
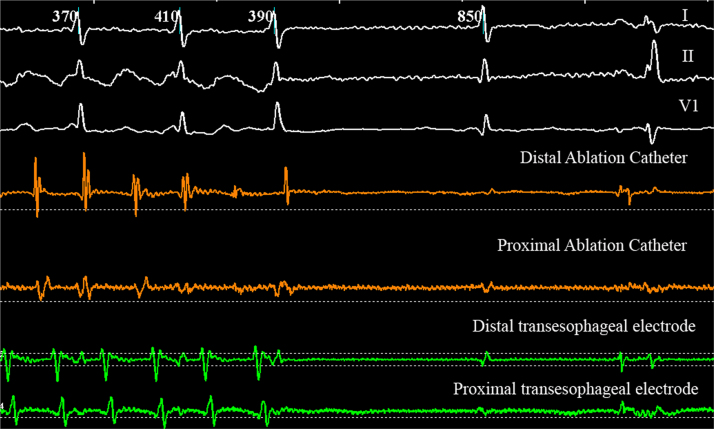
Figure 3.
Prolongation of cycle length before termination of atrial flutter with creation of radiofrequency ablation line at the cavotricuspid isthmus.
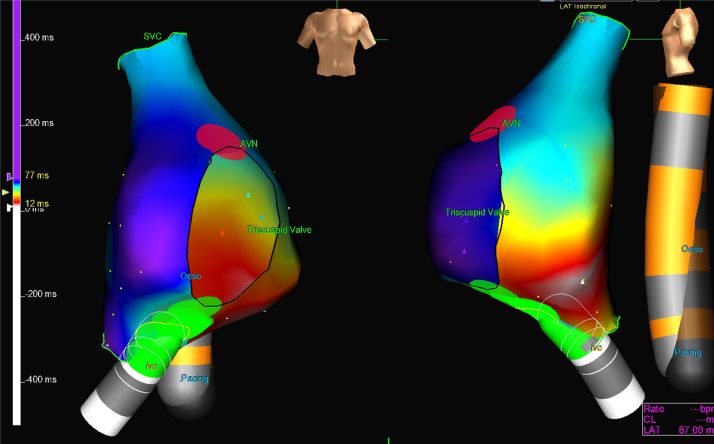
Figure 4.
Anteroposterior (left) and lateral (right) views of 3-dimensional electroanatomic mapping of the right atrium postablation with pacing from the esophageal electrode suggesting conduction block along the cavotricuspid isthmus with 80-ms delay at the lateral atrial wall. AVN = atrioventricular node; IVC = inferior vena cava; SVC = superior vena cava.
Atrial flutter recurred 12 hours after ablation. Electrophysiologic study was repeated on day 16 of life. Reinforcement of the ablation line was performed using a different catheter positioning, and slightly higher energy levels up to 13 W were achieved. Bidirectional isthmus block was confirmed by differential pacing from a 5Fr, 20-pole diagnostic catheter placed along the tricuspid ring from the right lateral atrial wall over the isthmus to the septal wall. There was a greater than 50-ms time difference in both directions. Neither inducible atrial flutter nor recurrence was observed after this ablation. Average radiation dose was 0.7 μGm2 per procedure. Overall radiation time for both procedures was less than 5 minutes of fluoroscopy.
Ventricular function improved significantly within days of conversion to sinus rhythm. A small pericardial effusion developed after the procedure but resolved within 1 week. A 24-hour ambulatory ECG excluded further recurrence of atrial flutter. No further recurrence was evident 6 months after the procedure without antiarrhythmic medication.
Discussion
To our knowledge, this is the first report of successful treatment of neonatal refractory atrial flutter using radiofrequency ablation. There is a single case report of radiofrequency used to ablate the atrioventricular node in a 7-week-old infant who was reported to have refractory atrial flutter requiring extracorporeal membrane oxygenation support.2 A pacemaker was implanted, but atrial flutter could not be reverted.
Most often neonatal atrial flutters can be easily converted to sinus rhythm. Various antiarrhythmic medications, such as digoxin, quinidine, procainamide, flecainide, sotalol, propranolol, and amiodarone, all have been used alone or in combination, with varying reported success rates. DC cardioversion usually is extremely effective, with a success rate greater than 85%, whereas transesophageal pacing seems to have a lower success rate. Sometimes a wait-and-see approach can be adopted until possible spontaneous resolution in hemodynamically stable infants. Recurrence is uncommon.1
The indication for ablation in children weighing less than 15 kg or younger than 4 years should be limited to patients with incessant tachycardia or tachycardia-induced cardiomyopathy unresponsive to a multiagent antiarrhythmic regimen.3 An underlying abnormality causing therapy-refractory flutter was considered, although there was no evidence of channelopathy in any ECG of the child or his family members. Genetic testing has not been performed. Intracardiac signals and conduction time recorded after ablation were normal.
The transesophageal electrode was found to be an effective atrial signal reference as well as a pacing site. Only 1 intracardiac catheter was used for the first procedure. This was advantageous to avoid vessel complications given the child’s small size but sufficient enough to create a good map and provide pacing. The location of the transesophageal probe did not allow determination of a bidirectional block of the ablation line. In hindsight, the recurrence after the first procedure can be best explained by the relatively low energy levels achieved with the first ablation. In the second procedure, placing the multipolar catheter in exchange for the ablation catheter over the isthmus allowed bidirectional block to be achieved.
Ablation of counterclockwise flutter using a 3-dimensional system can be performed safely and effectively in the newborn after all other therapy options have been exhausted. Using a careful and minimalistic approach, we were able to terminate the arrhythmia without significant radiation or side effects and an excellent outcome.
Footnotes
Supplementary material cited in this article is available online at doi:10.1016/j.hrcr.2015.03.010.
Appendix. Supplementary Materials
Supplementary Material
Supplementary Material
Supplementary Material
References
- 1.Texter K.M., Kertesz N.J., Friedman R.A., Fenrich A.L., Jr Atrial flutter in infants. J Am Coll Cardiol. 2006;48:1040–1046. doi: 10.1016/j.jacc.2006.04.091. [DOI] [PubMed] [Google Scholar]
- 2.Cisco MJ1 Asija R, Dubin A.M., Perry S.B., Hanley F.L., Roth S.J. Survival after extreme left atrial hypertension and pulmonary hemorrhage in an infant supported with extracorporeal membrane oxygenation for refractory atrial flutter. Pediatr Crit Care Med. 2011;12:e149–e152. doi: 10.1097/PCC.0b013e3181e8b3e5. [DOI] [PubMed] [Google Scholar]
- 3.Lee S.J., Schueller W.C. Tachycardias in infants, children and adolescents: safety and effectiveness of radiofrequency catheter ablation. Cardiology. 2000;94:44–51. doi: 10.1159/000007045. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Supplementary Material
Supplementary Material