KEY TEACHING POINTS
|
Introduction
Short QT syndrome (SQTS) is a rare hereditary disease that predisposes to life-threatening arrhythmias.1 Prophylactic therapy with hydroquinidine (HQ) has been shown to prolong the QT interval in patients with the p.N588K mutation in the KCNH2 gene2, 3 and reduce the occurrence of ventricular arrhythmias in a long-term follow-up, regardless of genotype.4 In vitro analyses have suggested a possible role for sotalol in the prophylactic treatment of patients with a different mutation (p.T618I) in the KCNH2 gene.5 We report 3 patients from a single family with SQTS thought to be due to the p.T618I-KCNH2 mutation and detail the effects of HQ and sotalol treatment in these patients.
Case report
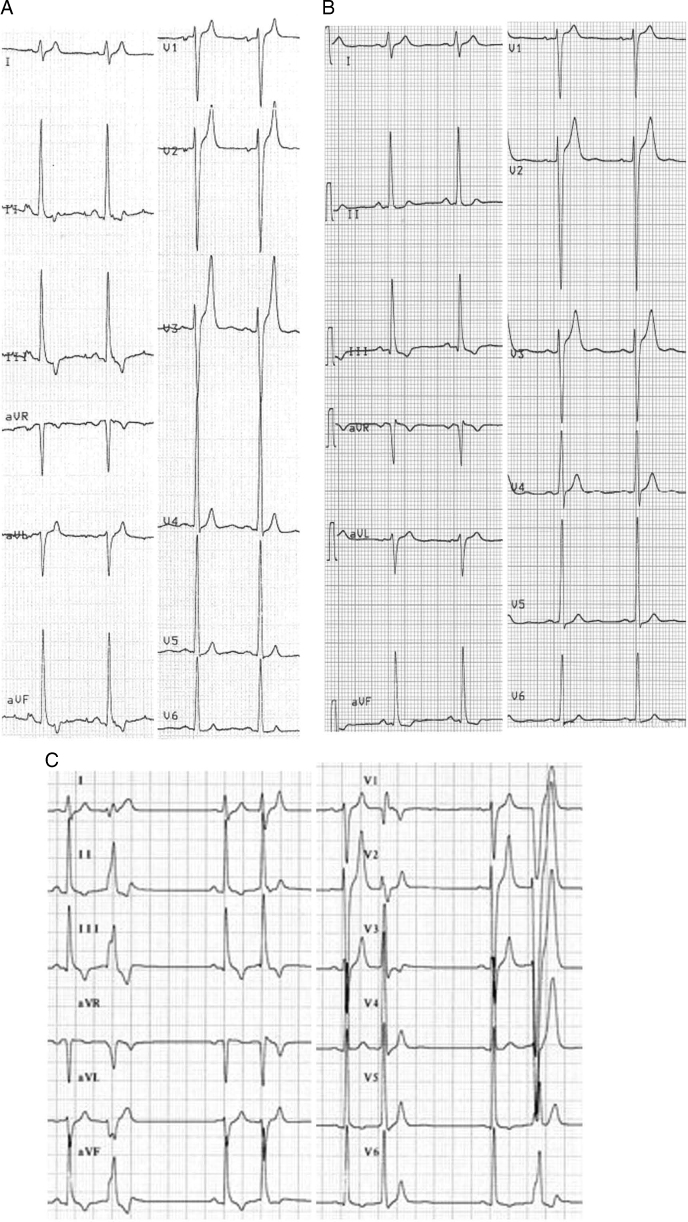
A 16-year-old male patient (patient 1) was referred to our institution after the detection of a short QT interval and frequent ventricular ectopic beats on an electrocardiogram (ECG). He had no history of symptoms suggesting arrhythmias or heart failure. His resting ECG showed a QT interval of 260 milliseconds at a heart rate (HR) of 80 beats per minute, corrected QT (QTc) 300 milliseconds, with tall and peaked T waves in the precordial leads and asymmetric negative T waves in the inferior leads (Figure 1A). Echocardiography results showed a dilated and slightly hypokinetic left ventricle, ejection fraction 48%. Cardiac magnetic resonance excluded myocarditis. Before the patient came to our institution, lamin A/C gene analysis had been performed to exclude a familial dilated cardiomyopathy, and the results were negative. A 24-hour ECG recording showed a QT interval always below the lower limits. Frequent isolated ventricular beats representing 12% of the total heartbeats with coupling intervals of 375–460 milliseconds and occasional bigeminy were recorded. The ectopy occurred mostly at night. There was no ventricular tachycardia. Stress test results revealed a poor shortening of the QT interval with HR increase,6 with an absolute QT value ranging from 240 milliseconds at rest (HR 75 beats per minute) to 200 milliseconds at peak effort (HR 194 beats per minute); no arrhythmias were recorded. An electrophysiological study (EPS) was performed and showed very short atrial and ventricular refractory periods (atrial 130 milliseconds; right ventricular apex 160 milliseconds and right ventricular outflow tract 150 milliseconds at a cycle length of 600 milliseconds); no ventricular arrhythmias were induced with programmed stimulation.
Figure 1.
Patient 1. A: Baseline electrocardiogram (ECG) results: heart rate (HR) 80 beats per minute, QT 260 milliseconds, corrected QT (QTc) 300 milliseconds. B: ECG recorded during treatment with 500 mg of HQ twice daily: HR 65 beats per minute, QT 320 milliseconds, QTc 333 milliseconds. C: ECG recorded during treatment with 80 mg of sotalol twice daily: bigeminy, QT interval 280 milliseconds.
The patient’s family history (Supplement 1) included several unexplained sudden deaths. The patient’s mother had died at the age of 34 during sleep; her ECG showed a QT interval of 270 milliseconds (QTc 300 milliseconds). The proband’s maternal great grandfather had died at the age of 40 shortly after awakening, and a maternal second-degree cousin had died suddenly at the age of 33 at home (no ECGs available).
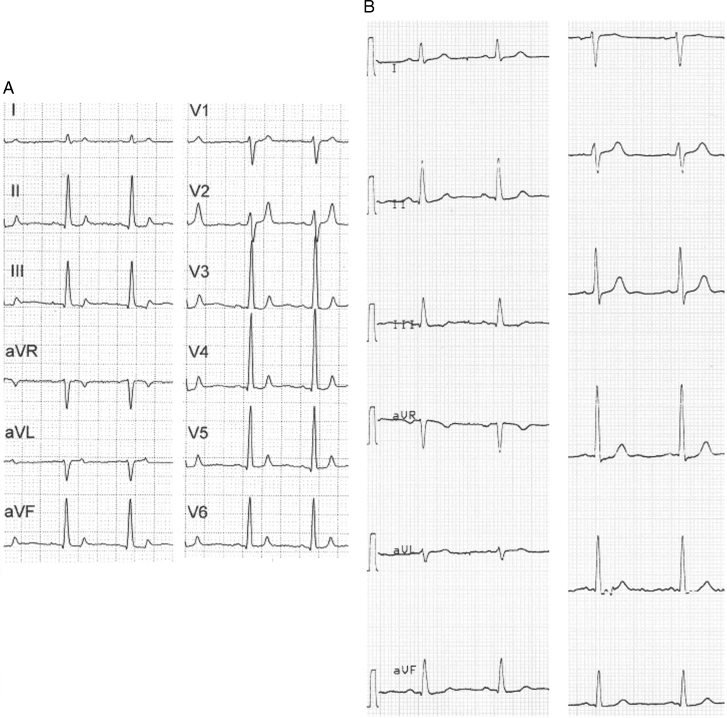
The asymptomatic 21-year-old sister of the index case (patient 2) had an ECG with a QT interval of 280 milliseconds and a QTc of 340 milliseconds (Figure 2A). Her echocardiogram was unremarkable. Poor adaptation of QT interval at different HRs was observed during 24-hour ECG recordings and exercise test; no arrhythmias were recorded. Short atrial and ventricular refractory periods were recorded during an EPS, and no arrhythmias were induced.
Figure 2.
Patient 2. A: Baseline ECG: HR 88 beats per minute, QT 280 milliseconds, QTc 340 milliseconds. B: ECG recorded during treatment with 250 mg of HQ 3 times daily: HR 70 beats per minute, QT 360 milliseconds, QTc 389 milliseconds. Abbreviations as in Figure 1.
These 2 siblings with ECG evidence of short QT intervals and a family history of sudden death in a first-degree relative fit the diagnosis of SQTS. The ventricular ectopy in the proband was of concern. Thus, 2 management strategies were considered: the implantation of an implantable cardioverter-defibrillator or a pharmacologic prophylaxis with HQ. Because of their youth and the absence of symptoms and of induced arrhythmias during EPS, both patients were started on 250 mg of HQ twice daily.
At his 6-month outpatient visit, the ECG of patient 1 showed a QT of 340 milliseconds at an HR of 60 beats per minute (QTc 340 milliseconds), with HQ serum levels at the lower limits (0.6 μg/mL; therapeutic range 0.6–2.2 μg/mL), although his HQ dosage had already been increased to 250 mg 3 times daily, so HQ dosage was further increased to 500 mg twice daily. At 6 months, the ECG of patient 2 showed a QT of 320 milliseconds and a QTc of 376 milliseconds, but her HQ serum levels were very low (0.280 μg/mL), and thus her HQ dosage was increased to 250 mg 3 times daily.
Both patients underwent implantation of a loop recorder to closely monitor for arrhythmias. At their 12-month follow-up visits, the devices had recorded no arrhythmias. The QT interval remained very short in patient 1 (QT 320 milliseconds, QTc 333 milliseconds) (Figure 1B), despite HQ serum level was in the therapeutic range (0.907 μ g/mL). In patient 2 the QTc interval had increased to 389 milliseconds with HQ 250 mg 3 times daily (HQ serum level 0.983 μg/mL, Figure 2B).
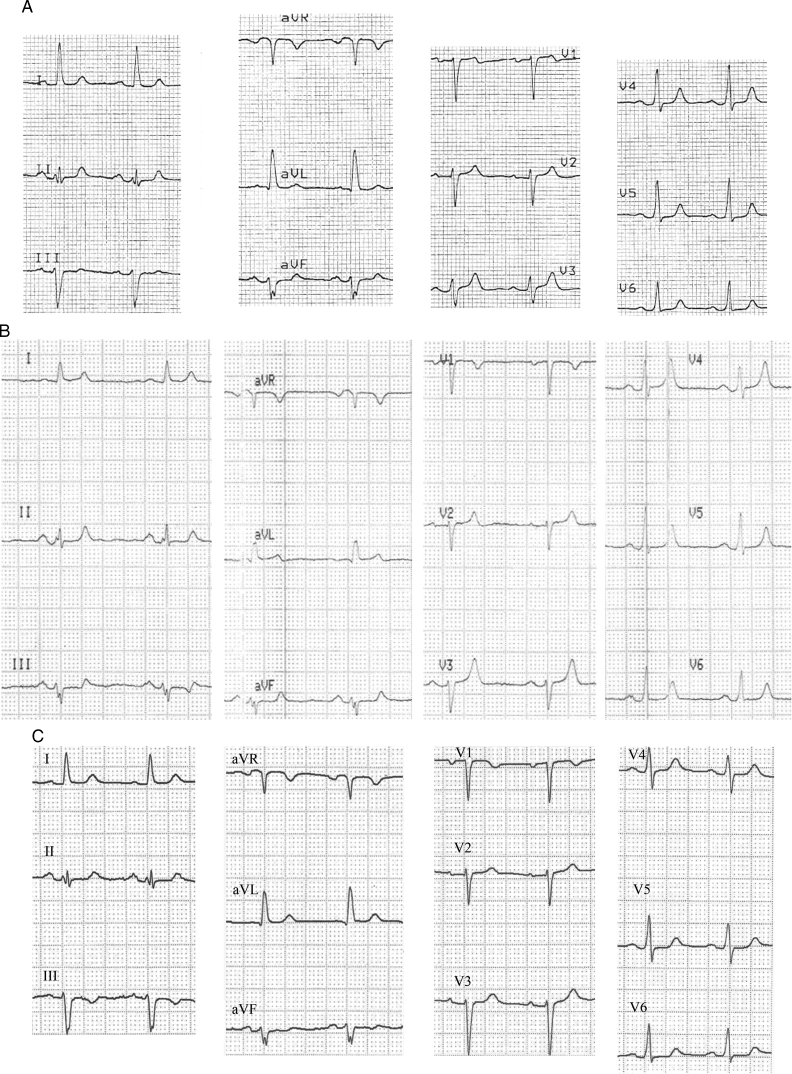
A 47-year-old maternal aunt of the 2 siblings (patient 3) (Supplement 1) experienced a sudden loss of consciousness in a public office. She was promptly resuscitated. Her heart rhythm at the time of arrest was ventricular fibrillation, which was successfully terminated via external defibrillation by emergency medical personnel. The first available ECG on sinus rhythm showed QT and QTc intervals of 260 and 355 milliseconds, respectively, with peaked T waves in the precordial leads. Coronary angiogram, echocardiogram, and magnetic resonance results were normal. A subsequent ECG confirmed the short QT intervals (QT 300 milliseconds, QTc 344 milliseconds at an HR of 79 beats per minute) (Figure 3A). An implantable cardioverter-defibrillator was implanted and therapy with 250 mg of HQ twice daily started. At her 4 month follow-up, the QT and QTc values were unchanged, and the device had recorded 4 episodes of nonsustained ventricular tachycardia (nsVT) up to 3 seconds in duration with subtherapeutic HQ levels (0.552 μg/mL) (Supplement 2A).
Figure 3.
Patient 3. A: Baseline ECG: HR 79 beats per minute, QT 300 milliseconds, QTc 344 milliseconds. B: ECG recorded during treatment with 80 mg of sotalol 3 times daily: HR 65 beats per minute, QT 330 milliseconds, QTc 343 milliseconds. C: ECG recorded during treatment with 250 mg of HQ 3 times daily: HR 78 beats per minute, QT 360 milliseconds, QTc 411 milliseconds. Abbreviations as in Figure 1.
After we obtained written informed consent, a genetic analysis of KCNQ1 and KCNH2 genes was performed. All 3 patients were found to have in heterozygosis the C to T transition at nucleotide 1853 (c.1853C>T) in the KCNH2 gene, which results in the change of the amino acid threonine to isoleucine at position 618 (p.T618I). Patient 1 was also found to have in homozygosis the KCNH2 polymorphism p.K897T, whereas patients 2 and 3 demonstrated this polymorphism in heterozygosis.
Because of the poor effect of HQ in prolonging the QT interval in patients 1 and 3, and in preventing ventricular arrhythmias in patient 3, we decided to evaluate the effect of sotalol in these 2 subjects. They started therapy at the dosage of 40 mg 3 times daily, which was increased after 5 days to 80 mg twice daily because no effect on QT interval was noticed. An ECG performed 10 days later in patient 1 continued to show ventricular bigeminy and a QT interval of 280 milliseconds (Figure 1C). Patient 3 had initial QT and QTc values of 340 milliseconds and similar values after increasing the sotalol dosage up to 80 mg 3 times daily (QT 330, QTc 343 milliseconds) (Figure 3B). We stopped sotalol and restarted HQ in both patients, 500 mg twice daily in patient 1 and 250 mg 3 times daily in patient 3. Two weeks later, patient 3 ECG showed an increase of the QT interval to 360 milliseconds and of the QTc to 411 milliseconds (Figure 3C).
During a mean follow-up of 59 ± 14 months, none of the patients complained of any symptom. Patient 1 still showed QTc values below the normal limits, but with HQ therapy, ventricular ectopy had been suppressed. Patient 2 had a slow nsVT recorded by the loop recorder (Supplement 2B), and patient 3 continued to have runs of nsVT but at slower rates than before (Supplement 2C).
Discussion
This article gives the first report of the in vivo effects of sotalol in SQTS patients carrying the p.T618I mutation in the KCNH2 gene. Our data do not suggest a clinical efficacy in these patients, neither in prolonging the QT interval to normal values nor in preventing ventricular arrhythmias.
Our group first evaluated the clinical effect of various antiarrhythmic drugs, including flecainide, sotalol, ibutilide, and HQ, in 2 SQTS families carrying the p.N588K mutation in the KCNH2 gene,3 and we found that HQ was effective both in prolonging QT interval and ventricular effective refractory periods, and in abolishing the inducibility of ventricular arrhythmias during EPS. The p.N588K mutation was later shown to be responsible for a 5.8-fold decrease in the IKr channel blocking effect of HQ, in contrast to the 20-fold decrease in the effect of sotalol.7 Later, we confirmed the long-term antiarrhythmic efficacy of HQ, despite the fact that a reduced and less homogeneous lengthening of the QTc was recorded in patients with mutations other than the p.N588K in the KCNH2 gene.3, 4 Other drugs, such as dysopiramide8 and amiodarone,4 have been tested in a few subjects. The data for these alternate drugs are limited and the drugs’ efficacy uncertain.
The p.T618I mutation in the pore loop of KCNH2 was described in a Chinese family with a history of sudden death.5 In vitro analysis showed a smaller loss of the inhibitory effect of sotalol on HERG channels compared with that of the p.N588K mutation. However, in this study, the sotalol concentration was 500 μM, whereas plasma concentrations during long-term oral therapy generally range from 1 to 3 mg/mL (88.4–265.2 μM/L).9 This difference may in part explain the drug’s lack of effectiveness in our patients. In the 2013 HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes,10 the authors state that sotalol may be considered in asymptomatic patients with a diagnosis of SQTS and a family history of sudden cardiac death.
Genetic analysis of the family in our study showed, in addition to the p.T618I mutation, the presence of the p.K897T polymorphism in KCNH2. It is well known that in the general population genetic variants have been associated with the variability of the QT interval.11 Although the p.K897T polymorphism has been widely investigated, there is no agreement on its effect on repolarization.12, 13, 14
The presence of genetic modifiers of repolarization may in part explain the familial phenotypic differences and different responses to medications seen in SQTS cases. The reduced efficacy of HQ in patient 1 may be related to his homozygous expression of the p.K897T polymorphism, in contrast to the heterozygous expression in patients 2 and 3. The homozygous expression may confer greater influence on the QT length. Also, after increasing the HQ dosage and with adequate HQ plasma levels, patient 1 still showed a short QT interval; however, he remained asymptomatic and his ventricular ectopy resolved, suggesting that the efficacy of HQ does not rely only on QT prolongation. Left ventricular function, however, did not vary. We observed in some SQTS patients a reduced ejection fraction and a higher mechanical dispersion of contraction compared with those of controls15; our hypothesis is that accelerated repolarization might result in altered calcium loading and therefore in a reduction in contractile activity.
Further studies are needed to evaluate the efficacy of a genotype-guided pharmacologic therapy for SQTS patients.
Acknowledgments
This work was supported by the PRIN Grant (2010BWY8E9_006) of the Ministero Italiano dell’Istruzione, dell’Università e della Ricerca (MIUR). We would like to thank Elisa Pirro, PhD, for her helpful collaboration.
Footnotes
The authors have no conflict of interest to declare.
Supplementary material cited in this article is available online at doi:10.1016/j.hrcr.2015.07.001.
Appendix. Supplementary data
Supplementary Material
References
- 1.Gaita F., Giustetto C., Bianchi F., Wolpert C., Schimpf R., Riccardi R., Grossi S., Richiardi E., Borggrefe M., Short Q.T. syndrome: a familial cause of sudden death. Circulation. 2003;108:965–970. doi: 10.1161/01.CIR.0000085071.28695.C4. [DOI] [PubMed] [Google Scholar]
- 2.Brugada R., Hong K., Dumaine R. Sudden death associated with short-QT syndrome linked to mutations in HERG. Circulation. 2004;109:30–35. doi: 10.1161/01.CIR.0000109482.92774.3A. [DOI] [PubMed] [Google Scholar]
- 3.Gaita F., Giustetto C., Bianchi F., Schimpf R., Haissaguerre M., Calò L., Brugada R., Antzelevitch C., Borggrefe M., Wolpert C., Short Q.T. syndrome: pharmacological treatment. J Am Coll Cardiol. 2004;43:1494–1499. doi: 10.1016/j.jacc.2004.02.034. [DOI] [PubMed] [Google Scholar]
- 4.Giustetto C., Schimpf R., Mazzanti A., Scrocco C., Maury P., Anttonen O., Probst V., Blanc J.J., Sbragia P., Dalmasso P., Borggrefe M., Gaita F. Long-term follow-up of patients with short QT syndrome. J Am Coll Cardiol. 2011;58:587–595. doi: 10.1016/j.jacc.2011.03.038. [DOI] [PubMed] [Google Scholar]
- 5.Sun Y., Quan X.Q., Fromme S., Cox R.H., Zhang P., Zhang L., Guo D., Guo J., Patel C., Kowey P.R., Yan G.X. A novel mutation in the KCNH2 gene associated with short QT syndrome. J Mol Cell Cardiol. 2011;50:433–441. doi: 10.1016/j.yjmcc.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 6.Giustetto C., Scrocco C., Schimpf R. Usefulness of exercise testing in the diagnosis of short QT syndrome. Europace. 2015;17:628–634. doi: 10.1093/europace/euu351. [DOI] [PubMed] [Google Scholar]
- 7.Wolpert C., Schimpf R., Giustetto C., Antzelevitch C., Cordeiro J., Dumaine R., Brugada R., Hong K., Bauersfeld U., Gaita F., Borggrefe M. Further insights into the effect of quinidine in short QT syndrome caused by a mutation in HERG. J Cardiovasc Electrophysiol. 2005;16:54–58. doi: 10.1046/j.1540-8167.2005.04470.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schimpf R., Veltmann C., Giustetto C., Gaita F., Borggrefe M., Wolpert C. In vivo effects of mutant HERG K1 channel inhibition by disopyramide in patients with a short QT-1 syndrome: a pilot study. J Cardiovasc Electrophysiol. 2007;18:1157–1160. doi: 10.1111/j.1540-8167.2007.00925.x. [DOI] [PubMed] [Google Scholar]
- 9.Campbell T.J., Williams K.M. Therapeutic drug monitoring: antiarrhythmic drugs. Br J Clin Pharmacol. 1998;46:307–319. doi: 10.1046/j.1365-2125.1998.t01-1-00768.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Priori S.G., Wilde A.A., Horie M. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013;10:1932–1963. doi: 10.1016/j.hrthm.2013.05.014. [DOI] [PubMed] [Google Scholar]
- 11.Arking D.E., Pfeufer A., Post W. A common genetic variant in the NOS1 regulator NOS1AP modulates cardiac repolarization. Nat Genet. 2006;38:644–651. doi: 10.1038/ng1790. [DOI] [PubMed] [Google Scholar]
- 12.Crotti L., Lundquist A.L., Insolia R., Pedrazzini M., Ferrandi C., De Ferrari G.M., Vicentini A., Yang P., Roden D.M., George A.L., Jr, Schwartz P.J. KCNH2-K897T is a genetic modifier of latent congenital long-QT syndrome. Circulation. 2005;112:1251–1258. doi: 10.1161/CIRCULATIONAHA.105.549071. [DOI] [PubMed] [Google Scholar]
- 13.Pietilä E., Fodstad H., Niskasaari E., Laitinen P.P.J., Swan H., Savolainen M., Kesäniemi Y.A., Kontula K., Huikuri H.V. Association between HERG K897T polymorphism and QT interval in middle-aged Finnish women. J Am Coll Cardiol. 2002;40:511–514. doi: 10.1016/s0735-1097(02)01979-4. [DOI] [PubMed] [Google Scholar]
- 14.Bezzina C.R., Verkerk A.O., Busjahn A. A common polymorphism in KCNH2 (HERG) hastens cardiac repolarization. Cardiovasc Res. 2003;59:27–36. doi: 10.1016/s0008-6363(03)00342-0. [DOI] [PubMed] [Google Scholar]
- 15.Frea S, Giustetto C, Capriolo M, Scrocco C, Fornengo C, Benedetto S, Bianchi F, Pidello S, Morello M, Gaita F. New echocardiographic insights in short QT syndrome: More than a channellopathy? Heart Rhythm 2015: doi: 10.1016/j.hrthm.2015.05.024. [E-pub ahead of print.] [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material