Introduction
Takotsubo cardiomyopathy (TCM) is a form of acute cardiomyopathy showing left ventricular apical ballooning. Whilst the exact mechanism of TCM remains unknown, it is hypothesized that an excess of circulatory catecholamine's to an exaggerated sympathetic from an intense physical or emotional distress as the cause. We report the rare case of a 76-year-old woman who developed TCM after undergoing uncomplicated pacemaker placement. Although rare this emphasizes that TCM, should be considered as a potential complication of pacemaker implantation in post-menopausal women with chest pain or symptoms of left heart failure.
Case Study
KEY TEACHING POINTS
|
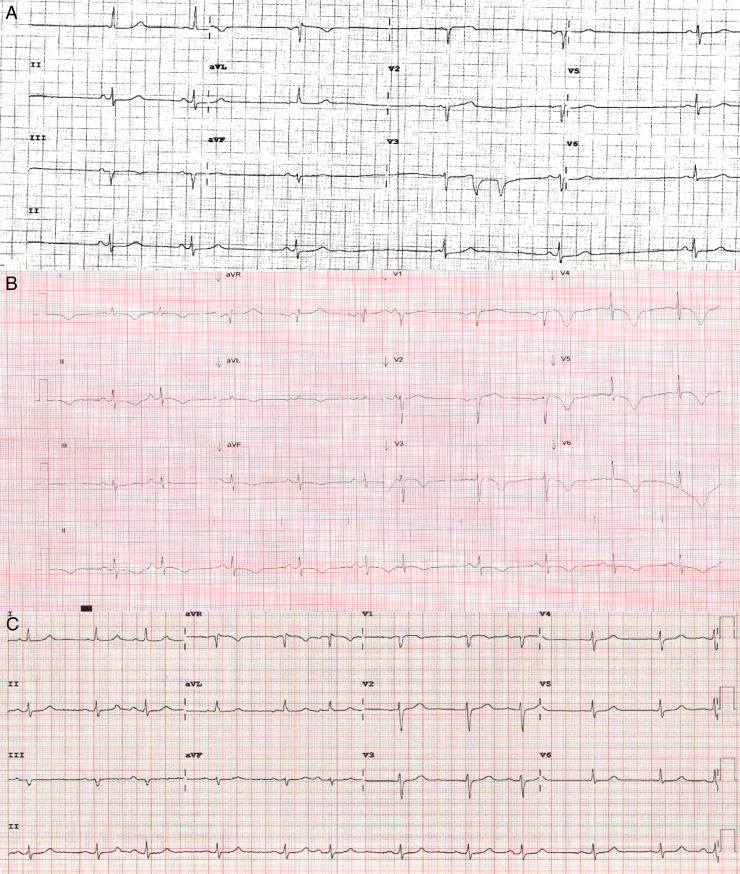
A 76-year-old female patient from Queensland was referred to the Gold Coast Cardiology Department for consideration of permanent pacemaker (PPM) insertion following investigation for syncope. She had a history of symptomatic bradycardia with a recent Holter monitor capturing a 5.5-second pause. She was diagnosed with sinus node dysfunction and was admitted on the day of the planned outpatient procedure; a dual-chamber pacemaker was inserted. She received local anesthetic, lignocaine and 2 mg of midazolam; the procedure was completed without any complications. The following morning she became nauseous and developed severe chest pain radiating to her back. Her vital signs deteriorated, and she became hypoxic and profoundly hypotensive with a systolic blood pressure of 83 mm Hg. An electrocardiogram (ECG) revealed global deep T wave inversions compared with her baseline (Figure 1) and her troponin I concentration was 3.2 μg/L (reference range <0.04 μg/L).
Figure 1.
A: Electrocardiogram (ECG) prior to pacemaker insertion. B: ECG showing deep inferolateral T-wave inversion. C: ECG in follow-up clinic visit showing resolution of T-wave inversion.
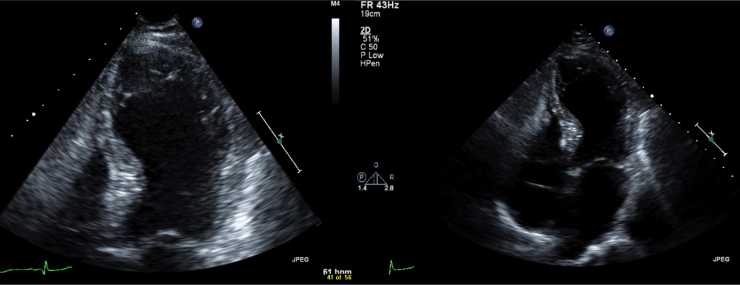
An urgent mobile chest radiograph revealed normal cardiomediastinal borders and no evidence of pneumothorax. A pacemaker check was performed, revealing 73% atrial pacing and <1% ventricular pacing since insertion. A bedside echocardiogram was performed, revealing akinesia in the anteroseptal and apical areas with an left ventricular ejection fraction (LVEF) of 24%. (Figure 2).
Figure 2.
Echocardiogram showing apical left ventricular hypokinesis.
An urgent coronary angiogram was performed. She had no significant coronary artery disease; however, a ventriculogram revealed apical akinesia with hypercontractile basal segments consistent with a diagnosis of TCM (Figure 3).
Figure 3.
Coronary angiogram and ventriculogram revealing left ventricular apical ballooning.
Discussion
Takotsubo cardiomyopathy was first described by Sato et al in 1990. It is named after the Japanese octopus-fishing pot “takotsubo” for the resemblance the “stressed” heart bears to the device. Best seen on a left ventriculogram, such a heart has apical to mid ventricular ballooning with compensatory basal hyperkinesis. This acute change in appearance and function of the left ventricle is usually a reversible and self-limiting form of cardiomyopathy. Patients typically present with symptoms and signs mimicking those of an acute myocardial infarction (AMI) but preceded by a provocative event such as death of a loved one, hence the moniker “broken heart syndrome.” Chest pain and shortness of breath are regularly reported, but syncope can also occur. In contrast to an AMI, takotsubo syndrome usually only modestly elevates the cardiac enzyme levels, a change that is out of proportion to the marked changes seen on the ECG. The most common ECG findings are those of ST segment elevation—which is seen in up to 56% of patients, usually in the anterior precordial leads—and deep T-wave inversion in most leads. Coronary angiogram reveals normal to minimal coronary artery disease, which does not correspond to the area of left ventricular dysfunction, thereby excluding AMI as a diagnosis. Currently no formal consensus has been reached regarding diagnostic criteria, but the proposed Mayo criteria have been adopted by most institutions.1
Whereas the exact mechanism of TCM remains unknown, an excess of circulatory catecholamines to an exaggerated sympathetic response is hypothesized to induce myocardial toxicity leading to myocardial stunning and negative cardiac myocyte inotropy. Beta-adrenoceptors have a higher density in the apex of the heart, explaining the apical ballooning with relative sparing of the ventricle base. It is well recognized that TCM is much more prevalent in postmenopausal women. Estrogen downregulates cardiac adrenoceptors, attenuating their response to activation and providing a plausible reason for this observation.2
What is unique to our case is that it resembles the classical features of TCM following PPM insertion, the sole identifiable stressful event. There have been rare reports of TCM after a PPM insertion; however, TCM remains an unrecognized complication of the procedure.3 Our case and these previous case studies shared common themes. Our patient was an elderly women with a conduction disorder, and there were minimal complications during implantation. Her presenting features were chest pain, dyspnea, and hypotension, symptoms shared with the other case studies. Unlike our case, many of the cases reported before this presented with complete atrioventricular block, and it could be argued that this was the precipitating event. Our case was a routine outpatient PPM insertion for symptomatic bradycardia with a prolonged sinus pause.
The management of patients with TCM is largely supportive and conservative. There are no published randomized control trials, but β-blockers and angiotensin-converting enzyme inhibitors have proven effective. Roughly 20% of patients experience complications; the commonest is the development of left heart failure, which can progress to cardiogenic shock. Another important complication to recognize is left ventricular outflow tract (LVOT) obstruction, which is a result of apical hypokinesis and basal hyperkinesis. The utilization of inotropes may induce further LVOT obstruction and should be avoided. Prognosis is good with the restoration of cardiac function, usually within the month. Recurrence is uncommon, estimated at about 3%, and mortality rates are low, in the range of 1%–3%. Our patient was discharged on once daily 2.5 mg of bisoprolol and once daily 5 mg of ramipril. A follow-up echocardiogram at 4 weeks revealed an LVEF of 45% and resolving wall motion abnormalities.4 At 6 months, her LVEF had improved to 64% with no obvious regional wall motion abnormalities, and her ECG revealed resolution of her T-wave inversion (Figure 1).
Our case report emphasizes that TCM, although rare, should be considered a potential complication of uncomplicated pacemaker implantation in postmenopausal women with chest pain or symptoms of left heart failure.
Footnotes
Conflicts of interest: none
References
- 1.Prasad A., Lerman A., Rihal C.S. Apical ballooning syndrome (tako-tsubo or stress cardiomyopathy): a mimic of acute myocardial infarction. Am Heart J. 2008;155(3):408–417. doi: 10.1016/j.ahj.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 2.Ueyama T., Hano T., Kasamatsu K. Estrogen attenuates the emotional stress induced cardiac responses in the animal model of takotsubo (ampulla) cardiomyopathy. J Cardiovasc Pharmacol. 2003;42(Suppl 1):S117–S119. doi: 10.1097/00005344-200312001-00024. [DOI] [PubMed] [Google Scholar]
- 3.Chun S.G., Kwok V., Pang D.K., Lau T.K. Transient left ventricular apical ballooning syndrome (takotsubo cardiomyopathy) as a complication of permanent pacemaker implantation. Int J Cardiol. 2007;117:e27–e30. doi: 10.1016/j.ijcard.2006.11.125. [DOI] [PubMed] [Google Scholar]
- 4.Donohue D., Movahed M.R. Clinical characteristics, demographics and prognosis of transient left ventricular apical ballooning syndrome. Heart Fail Rev. 2005;10(4):311–316. doi: 10.1007/s10741-005-8555-8. [DOI] [PubMed] [Google Scholar]